NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Center for Substance Abuse Treatment (US). Improving Cultural Competence. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 59.)
John, 27, is an American Indian from a Northern Plains Tribe. He recently entered an outpatient treatment program in a midsized Midwestern city to get help with his drinking and subsequent low mood. John moved to the city 2 years ago and has mixed feelings about living there, but he does not want to return to the reservation because of its lack of job opportunities. Both John and his counselor are concerned that (with the exception of his girlfriend, Sandy, and a few neighbors) most of his current friends and coworkers are “drinking buddies.” John says his friends and family on the reservation would support his recovery—including an uncle and a best friend from school who are both in recovery—but his contact with them is infrequent.
John says he entered treatment mostly because his drinking was interfering with his job as a bus mechanic and with his relationship with his girlfriend. When the counselor asks new group members to tell a story about what has brought them to treatment, John explains the specific event that had motivated him. He describes having been at a party with some friends from work and watching one of his coworkers give a bowl of beer to his dog. The dog kept drinking until he had a seizure, and John was disgusted when people laughed. He says this event was “like a vision;” it showed him that he was being treated in a similar fashion and that alcohol was a poison. When he first began drinking, it was to deal with boredom and to rebel against strict parents whose Pentecostal Christian beliefs forbade alcohol. However, he says this vision showed him that drinking was controlling him for the benefit of others.
Later, in a one-on-one session, John tells his counselor that he is afraid treatment won't help him. He knows plenty of people back home who have been through treatment and still drink or use drugs. Even though he doesn't consider himself particularly traditional, he is especially concerned that there is nothing “Indian” about the program; he dislikes that his treatment plan focuses more on changing his thinking than addressing his spiritual needs or the fact that drinking has been a poison for his whole community.
John's counselor recognizes the importance of connecting John to his community and, if possible, to a source of traditional healing. After much research, his counselor is able to locate and contact an Indian service organization in a larger city nearby. The agency puts him in touch with an older woman from John's Tribe who resides in that city. She, in turn, puts the counselor in touch with another member of the Tribe who is in recovery and had been staying at her house. This man agrees to be John's sponsor at local 12-Step meetings. With John's permission, the counselor arranges an initial family therapy session that includes his new sponsor, the woman who serves as a local “clan mother,” John's girlfriend, and, via telephone, John's uncle in recovery, mother, and brother. With John's permission and the assistance of his new sponsor, the counselor arranges for John and some other members of his treatment group to attend a sweat lodge, which proves valuable in helping John find some inner peace as well as giving his fellow group members some insight into John and his culture.
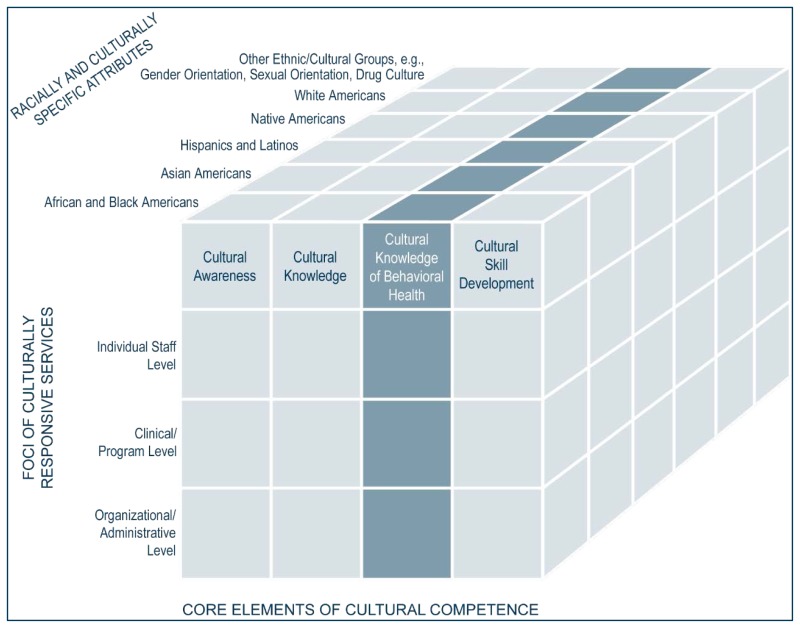
To provide culturally responsive treatment, counselors and organizations must be committed to gaining cultural knowledge and clinical skills that are appropriate for the specific racial and ethnic groups they serve. Treatment providers need to learn how a client's identification with one or more cultural groups influences the client's identity, patterns of substance use, beliefs surrounding health and healing, help-seeking behavior, and treatment expectations and preferences. Adopting Sue's (2001) multidimensional model in developing cultural competence, this chapter identifies cultural knowledge and its relationship to treatment as a domain that requires proficiency in clinical skills, programmatic development, and administrative practices. This chapter focuses on patterns of substance use and co-occurring disorders (CODs), beliefs about and traditions involving substance use, beliefs and attitudes about behavioral health treatment, assessment and treatment considerations, and theoretical approaches and treatment interventions across the major racial and ethnic groups in the United States.
Introduction
Culture is a primary force in the creation of a person's identity. Counselors who are culturally competent are better able to understand and respect their clients' identities and related cultural ways of life. This chapter proposes strategies to engage clients of diverse racial and ethnic groups (who can have very different life experiences, values, and traditions) in treatment. The major racial and ethnic groups in the United States covered in this chapter are African Americans, Asian Americans (including Native Hawaiians and other Pacific Islanders), Latinos, Native Americans (i.e., Alaska Natives and American Indians), and White Americans. In addition to providing epidemiological data on each group, the chapter discusses salient aspects of treatment for these racial/ethnic groups, drawing on clinical and research literature. This information is only a starting point in gaining cultural knowledge as it relates to behavioral health. Understanding the diversity within a specific culture, race, or ethnicity is essential; not all information presented in this chapter will apply to all individuals. The material in this chapter has a scientific basis, yet cultural beliefs, traditions, and practices change with time and are not static factors to consider in providing services for clients, families, or communities.
Although these broad racial/ethnic categories are often used to describe diverse cultural groups, the differences between two members of the same racial/ethnic group can be greater than the differences between two people from different racial/ethnic groups (Lamont and Small 2008; Zuckerman 1998). It is not possible to capture every aspect of diversity within each cultural group. Behavioral health workers should acknowledge that there will be many individual variations in how people interact with their environments, as well as in how environmental context affects behavioral health. However, to provide a framework for understanding many diverse cultural groups, some generalizations are necessary; thus, broad categories are used to organize information in this chapter. Counselors are encouraged to learn as much as possible about the specific populations they serve. Sources listed in Appendix F provide additional information.
Counseling for African and Black Americans
According to the 2010 U.S. Census definition, African Americans or Blacks are people whose origins are “in any of the black racial groups of Africa” (Humes et al. 2011, p. 3). The term includes descendants of African slaves brought to this country against their will and more recent immigrants from Africa, the Caribbean, and South or Central America (many individuals from these latter regions, if they come from Spanish-speaking cultural groups, identify or are identified primarily as Latino). The term “Black” is often used interchangeably with African American, although sometimes the term “African American” is used specifically to describe people whose families have been in this country since at least the 19th century and thus have developed distinct African American cultural groups. “Black” can be a more inclusive term describing African Americans as well as more recent immigrants with distinct cultural backgrounds.
Beliefs About and Traditions Involving Substance Use
In most African American communities, significant alcohol or drug use may be socially unacceptable or seen as a sign of weakness (Wright 2001), even in communities with limited resources, where the sale of such substances may be more acceptable. Overall, African Americans are more likely to believe that drinking and drug use are activities for which one is personally responsible; thus, they may have difficulty accepting alcohol abuse/dependence as a disease (Durant 2005).
Substance Use and Substance Use Disorders
To date, there has not been much research analyzing differences in patterns of substance use and abuse among different groups of Blacks, but there are indications that some gender differences exist. For example, alcohol consumption among African American women increases as they grow older, but Caribbean Black women report consistently low alcohol consumption as they grow older (Center for Substance Abuse Treatment [CSAT] 1999a; Galvan and Caetano 2003). Rates of overall substance use among African Americans vary significantly by age. Several researchers have observed that despite Black youth being less likely than White American youth to use substances, as African Americans get older, they tend to use at rates comparable with those of White Americans (Watt 2008). This increase in substance use with age among Blacks is often referred to as a crossover effect.
However, Watt (2008), in her analysis of 4 years of National Survey on Drug Use and Health (NSDUH) data (1999–2002), found that when controlling for factors such as drug exposure, marriage, employment, education, income, and family/social support, the crossover effect disappeared for Blacks ages 35 and older; patterns for drug and heavy alcohol use among Black and White American adults remained the same as for Black and White American adolescents (i.e., White Americans were significantly more likely to use substances). Watt concludes that systemic issues, such as lower incomes and education levels, and other factors, such as lower marriage rates, contribute to substance use among Black adults. Additional research also suggests that exposure to discrimination increases willingness to use substances in African American youth and their parents (Gibbons et al. 2010).
When comparing African Americans with other racial and ethnic groups, NSDUH data from 2012 suggest that they are somewhat more likely than White Americans to use illicit drugs and less likely than White Americans to use alcohol. They also appear to have an incidence of alcohol and drug use disorders similar to that seen in White Americans (Substance Abuse and Mental Health Services Administration [SAMHSA] 2013d). Crack cocaine use is more prevalent among Blacks than White Americans or Latinos, whereas rates of abuse of methamphetamine, inhalants, most hallucinogens, and prescription drugs are lower (SAMHSA 2011a). Phencyclidine use also appears to be a more serious problem, albeit affecting a relatively small group, among African Americans than among members of other racial/ethnic groups.
There appear to be some other differences in how African Americans use substances compared with members of other racial/ethnic groups. For example, Bourgois and Schonberg (2007) observed that among people who injected heroin in San Francisco, White Americans tended to administer the drug quickly whether or not they could find a vein, which led them to inject into fat or muscle tissue and resulted in a higher rate of abscesses. However, African Americans who injected heroin were more methodical and took the time to find a vein, even if it took multiple attempts. This, in turn, often resulted in using syringes that were already bloodied and increased their chances of contracting HIV/AIDS and other blood-borne diseases. African Americans who injected heroin were significantly more likely to also use crack cocaine than were White Americans who injected heroin (Bourgois et al. 2006).
African American patterns of substance use have changed over time and will likely continue to do so. Based on treatment admission data, admissions of African Americans who injected heroin declined by 44 percent during a 12-year period, whereas admissions declined by only 14 percent among White Americans (Broz and Ouellet 2008). Additionally, during this period, the peak age for African Americans who injected heroin increased by 10 years, yet it decreased by 10 years for White Americans. This suggests that the decrease in injectable heroin use among African Americans was largely due to decreased use among younger individuals.
Some preliminary evidence suggests that African Americans are less likely to develop drug use disorders following initiation of use (Falck et al. 2008), yet more research is needed to identify variables that influence the development of drug use disorders. Even though African Americans seem less likely than White Americans to develop alcohol use disorders, a number of older studies have found that they more frequently experience liver cirrhosis and other alcohol-related health problems (Caetano 2003; Polednak 2008). In tracking 25 years of data, Polednak (2008) found that the magnitude of difference has decreased over time; nonetheless, health disparities continue to exist for African Americans in terms of access to and quality of care, which can affect a number of health problems (Agency for Healthcare Research and Quality 2009; Smedley et al. 2003).
Mental and Co-Occurring Disorders
A number of studies have found biases that result in African Americans being overdiagnosed for some disorders and underdiagnosed for others. African Americans are less likely than White Americans to receive treatment for anxiety and mood disorders, but they are more likely to receive treatment for drug use disorders (Hatzenbuehler et al. 2008). In one study evaluating posttraumatic stress disorder (PTSD) among African Americans in an outpatient mental health clinic, only 11 percent of clients had documentation referring to PTSD, even though 43 percent of the clients showed symptoms of PTSD (Schwartz et al. 2005). Black immigrants are less likely to be diagnosed with mental disorders than are Blacks born in the United States (Burgess et al. 2008; Miranda et al. 2005b).
African Americans are more likely to be diagnosed with schizophrenia and less likely to be diagnosed with affective disorders than White Americans, even though multiple studies have found that rates of both disorders among these populations are comparable (Baker and Bell 1999; Bresnahan et al. 2000; Griffith and Baker 1993; Stockdale et al. 2008; Strakowski et al. 2003). African Americans are about twice as likely to be diagnosed with a psychotic disorder as White Americans and more than three times as likely to be hospitalized for such disorders. These differences in diagnosis are likely the result of clinician bias in evaluating symptoms (Bao et al. 2008; Trierweiler et al. 2000; Trierweiler et al. 2006). Clinicians should be aware of bias in assessment with African Americans and with other racial/ethnic groups and should consider ways to increase diagnostic accuracy by reducing biases. For an overview of mental health across populations, refer to Mental Health United States, 2010 (SAMHSA 2012a).
In some African American communities, incidence and prevalence of trauma exposure and PTSD are high, and substance use appears to increase trauma exposure even further (Alim et al. 2006; Breslau et al. 1995; Curtis-Boles and Jenkins-Monroe 2000; Rich and Grey 2005). Black women who abuse substances report high rates of sexual abuse (Ross-Durow and Boyd 2000). Trauma histories can also have a greater effect on relapse for African American clients than for clients from other ethnic/racial groups (Farley et al. 2004). There are few integrated approaches to trauma and substance abuse that have been evaluated with African American clients, and although some have been found effective at reducing trauma symptoms and substance use, the extent of that effectiveness is not necessarily as great as it is for White Americans (Amaro et al. 2007; Hien et al. 2004; SAMHSA 2006).
African Americans are less likely than White Americans to report lifetime CODs (Mericle et al. 2012). However, limited research indicates that, as with other racial groups, there are differences across African American groups in the screening and symptomatology of CODs. Seventy-four percent of African Americans who had a past-year major depressive episode were identified as also having both alcohol and marijuana use disorders (Pacek et al. 2012). Miranda et al. (2005b) found that American-born Black women were more than twice as likely to be screened as possibly having depression than African- or Caribbean-born Black women, but this could reflect, in part, differences in acculturation (see Chapter 1). However, research findings strongly suggest that cultural responses to some disorders, and possibly the rates of those disorders, do vary among different groups of Blacks. Differences do not appear to be simply reflections of differences in acculturation (Joe et al. 2006). For a review of African American health, see Hampton et al. (2010).
Treatment Patterns
African Americans may be less likely to receive mental health services than White Americans. In the Baltimore Epidemiologic Catchment Services Area study conducted during the 1980s, African Americans were less likely than White Americans to receive mental health services. However, at follow-up in the early 1990s, African American respondents were as likely as White Americans to receive such services, but they were much more likely to receive those services from general practitioners than from mental health specialists (Cooper-Patrick et al. 1999). Stockdale et al. (2008) analyzed 10 years of data from the National Ambulatory Medical Care Survey; they found significant improvements in diagnosis and care for mental disorders among African Americans in psychiatric settings between 1995 and 2005, but they also found that disparities persisted in the diagnosis and treatment of mental disorders in primary care settings. Fortuna et al. (2010) suggest that persistent problems exist in the delivery of behavioral health services, as evidenced by lower retention rates for treating depression.
Even among people who enter substance abuse treatment, African Americans are less likely to receive services for CODs. A study of administrative records from substance abuse and mental health treatment providers in New Jersey found that African Americans were significantly more likely than White Americans to have an undetected co-occurring mental disorder, and, if detected, they were significantly less likely than White Americans or Latinos to receive treatment for that disorder (Hu et al. 2006). Among persons with substance use disorders and co-occurring mood or anxiety disorders, African Americans are significantly less likely than White Americans to receive services (Hatzenbuehler et al. 2008). African Americans who do receive services for CODs are more likely to obtain them through substance abuse treatment programs than mental health programs (Alvidrez and Havassy 2005).
According to the Treatment Episode Data Sets (TEDS) from 2001 to 2011, African American clients entering substance abuse treatment most often reported alcohol as their primary substance of abuse, followed by marijuana. However, gender differences are evident, indicating that women report a broader range of substances as their primary substance of abuse than men do (SAMHSA, Center for Behavioral Health Statistics and Quality [CBHSQ], 2013). Most recent research suggests that African Americans are about as likely to seek and eventually receive substance abuse treatment as are White Americans (Hatzenbuehler et al. 2008; Perron et al. 2009; SAMHSA, CBHSQ 2011; Schmidt et al. 2006). Data analyzed by Perron et al. (2009) indicate that among African Americans with lifetime diagnoses of drug use disorders, 20.8 percent had received some type of treatment, as defined broadly to include resources such as pastoral counseling and mutual-help group attendance. This made them more likely to have received treatment than White Americans (15.5 percent of whom received treatment) or Latinos (17.3 percent of whom received treatment). Although data indicate that African Americans were less likely to receive services from private providers, they also indicate that African Americans were more likely to use more informal services (e.g., pastoral counseling, mutual help).
Although most major studies have found that race is not a significant factor in receiving treatment, African Americans report lengthier waiting periods, less initiation of treatment, more barriers to treatment participation (e.g., lack of childcare, lack of insurance, lack of knowledge about available services), and shorter lengths of stay in treatment than do White Americans (Acevedo et al. 2012; Brower and Carey 2003; Feidler et al. 2001; Grant 1997; Hatzenbuehler et al. 2008; Marsh et al. 2009; SAMHSA 2011c; Schmidt et al. 2006). In SAMHSA's 2010 NSDUH, 33.5 percent of African Americans who had a need for substance abuse treatment but did not receive it in the prior year reported that they lacked money or the insurance coverage to pay for it (SAMHSA, CBHSQ 2011). Economic disadvantage does leave many Africans Americans uninsured; approximately 16.1 percent of non-Latino Blacks had no coverage in 2004 (Schiller et al. 2005).
Likewise, some researchers have found that African Americans are less likely than White Americans to receive needed services or an appropriate level of service (Alegria et al. 2011; Bluthenthal et al. 2007; Marsh et al. 2009). For example, African Americans and Latinos are less likely than White Americans to receive residential treatment and are more likely to receive outpatient treatment, even when they present with more serious substance use problems (Bluthenthal et al. 2007). Other studies have found that African Americans with severe substance use or CODs were less likely to enter or receive treatment than White Americans with equally severe disorders (Schmidt et al. 2006, 2007).
African Americans are overrepresented among people who are incarcerated in prisons and jails (for review, see Fellner 2009), and a substantial number of those who are incarcerated (64.1 percent of jail inmates in 2002) have substance use disorders (Karberg and James 2005) and mental health problems (SAMHSA 2012a). However, according to Karberg and (James 2005), African Americans with substance dependence disorders who were in jail in 2002 were less likely than White Americans or Latinos to participate in substance abuse treatment while under correctional supervision (32 percent of African Americans participated compared with 37 percent of Latinos and 45 percent of White Americans). In the 2010 TEDS survey, African Americans entering treatment were also less likely than Asian Americans, White Americans, Latinos, Native Hawaiians/Pacific Islanders, or American Indians in the same situation to be referred to treatment through the criminal justice system (SAMHSA, CBHSQ 2012). Notwithstanding, African Americans are more likely to be referred to treatment from criminal justice settings rather than self-referred or referred by other sources (Delphin-Rittmon et al. 2012)
Beyond issues related to diagnosis and care that can prevent African Americans from accessing mental health services, research suggests that a lack of familiarity with the value and use of specialized behavioral health services among some African Americans may limit service use. Hines-Martin et al. (2004) found a positive relationship between familiarity and use of mental health services among African Americans. Additionally, factors such as social and familial prejudices (Ayalon and Alvidrez 2007; Mishra et al. 2009; Nadeem et al. 2007) and fears relating to past abuses of African Americans within the mental health system (Jackson 2003) can contribute to the lack of acceptance and subsequent use of these services. An essential step in decreasing disparity in behavioral health services among African Americans involves conducting culturally appropriate mental health screenings and using culturally sensitive instruments and evaluation tools (Baker and Bell 1999).
Beliefs and Attitudes About Treatment
According to 2011 NSDUH data, African Americans were, next to Asian Americans, the least likely of all major ethnic and racial groups to state a need for specialized substance abuse treatment (SAMHSA, CBHSQ 2013a). Still, logistical barriers may pose a greater challenge for African Americans than for members of other major racial and ethnic groups. For example, 2010 NSDUH data regarding individuals who expressed a need for substance abuse treatment but did not receive it in the prior year indicate that African Americans were more likely than members of other major ethnic/racial groups to state that they lacked transportation to the program or that their insurance did not cover the cost of such treatment (SAMHSA 2011a). African Americans experience several challenges in accessing behavioral health treatment, including fears about the therapist or therapeutic process and concerns about discrimination and costs (Holden et al. 2012; Holden and Xanthos 2009; Williams et al. 2012).
Longstanding suspicions regarding established healthcare institutions can also affect African Americans' participation in, attitudes toward, and outcomes after treatment (for review, see Pieterse et al. 2012). Historically, the mental health system has shown bias against African Americans, having been used in times past to control and punish them (Boyd-Franklin and Karger 2012; Jackson 2003). After controlling for socioeconomic factors, African Americans are significantly more likely to perceive the healthcare system as poor or fair and significantly more likely to believe that they have been discriminated against in healthcare settings (Blendon et al. 2007). Attitudes toward psychological services appear to become more negative as psychological distress increases (Obasi and Leong 2009). In many African American communities, there is a persistent belief that social and treatment services try to impose White American values, adding to their distrust of the treatment system (Larkin 2003; Solomon 1990).
African Americans, even when receiving the same amount of services as White Americans, are less likely to be satisfied with those services (Tonigan 2003). However, recent evidence suggests that, once engaged, African American clients are at least as likely to continue participation as members of other ethnic/racial groups (Harris et al. 2006). Because distrust of the healthcare system can make it more difficult to engage African American clients initially in treatment, Longshore and Grills (2000) recommend culturally congruent motivational enhancement strategies to address African American clients' ambivalence about treatment services. Providers also need to craft culturally responsive health-related messages for African Americans to improve treatment engagement and effectiveness (Larkin 2003).
Most importantly, providers need to demonstrate multicultural experience. In a study comparing outcomes among Black and White clients at community mental health centers, the only clinician factor that predicted more favorable outcomes was clinicians' general experiences and relationships with people from racial/ethnic and cultural groups other than their own (Larrison et al. 2011).
Treatment Issues and Considerations
African American clients generally respond better to an egalitarian and authentic relationship with counselors (Sue 2001). Paniagua (1998) suggests that in the initial sessions with African American clients, counselors should develop a collaborative client–counselor relationship. Counselors should request personal information gradually rather than attempting to gain information as quickly as possible, avoid information-gathering methods that clients could perceive as an interrogation, pace the session, and not force a data-gathering agenda (Paniagua 1998; Wright 2001). Counselors must also establish credibility with clients (Boyd-Franklin 2003).
Next, counselors should establish trust. Self-disclosure can be very difficult for some clients because of their histories of experiencing racism and discrimination. These issues can be exacerbated in African American men whose experience of racism has been more severe or who have had fewer positive relationships with White Americans (Reid 2000; Sue 2001). Counselors, therefore, need to be willing to address the issue of race and to validate African American clients' experiences of racism and its reality in their lives, even if it differs from their own experiences (Boyd-Franklin 2003; Kelly and Parsons 2008). Moreover, racism and discrimination can lead to feelings of anger, anxiety, or depression. Often, these feelings are not specific to any given event; rather, they are pervasive (Boyd-Franklin et al. 2008). Counselors should explore with clients the psychological effects of racism and develop approaches to challenge internal negative messages that have been received or generated through discrimination and prejudice (Gooding 2002).
Additional methods that may enhance engagement and promote participation include peer-supported interventions and strategies that promote empowerment by emphasizing strengths rather than deficits (Paniagua 1998; Tondora et al. 2010; Wright 2001). It is important to explore with clients the strengths that have brought them this far. What personal, community, or family strengths have helped them through difficult times? What strengths will support their recovery efforts? Exhibit 5-1 gives an overview of core guiding principles in working with African American clients.
Exhibit 5-1
Core Culturally Responsive Principles in Counseling African Americans.
Theoretical Approaches and Treatment Interventions
Research suggests that culturally congruent interventions are effective in treating African Americans (Longshore and Grills 2000; Longshore et al. 1998a; Longshore et al. 1998b 1999). Although there are conflicting results on the effectiveness of motivational interviewing among African American clients (Montgomery et al. 2011), some motivational interventions have been found to reduce substance use among African Americans (Bernstein et al. 2005; Longshore and Grills 2000). Longshore and Grills (2000) describe a culturally specific motivational intervention for African Americans involving both peer and professional counseling that makes use of the core African American value of communalism by addressing the ways in which the individual's substance abuse affects his or her whole community. The motivational program affirms “the heritage, rights, and responsibilities of African Americans…using interaction styles, symbols and values shared by members of the group” (Longshore et al. 1998b, p. 319). So too, African American music, artwork, and food can help programs create a welcoming and familiar atmosphere, as is the case for other racial and ethnic groups when familiar cultural symbols appear in the clinical setting.
Many of the interventions developed for substance abuse treatment services in general have been evaluated with populations that were at least partly composed of African Americans; many of these interventions are as effective for African Americans as they are for White Americans (Milligan et al. 2004; Tonigan 2003). One intervention that appears to work better for African American (and Latino) clients than for White American clients—perhaps because it focuses on improving client–counselor communication—is node-link mapping (visual representation using information diagrams, fill-in-the-blank graphic tools, and client-generated diagrams or visual maps). This approach was associated with lower rates of substance use, better treatment attendance, and better counselor ratings of motivation and confidence among African Americans than among White Americans (Dansereau et al. 1996; Dansereau and Simpson 2009).
In addition, cognitive–behavioral therapy (CBT) has certain distinct advantages for African American clients; it fosters a collaborative relationship and recognizes that clients are experts on their own problems (Kelly and Parsons 2008). Maude-Griffin et al. (1998) compared CBT and 12-Step facilitation for a group of mostly African American (80 percent) men who were homeless and found that CBT achieved significantly better abstinence outcomes, except among those who considered themselves very religious (these individuals had better outcomes with 12-Step facilitation).
Other interventions that use CBT principles have also been effective with African American populations. For example, a number of studies have evaluated contingency management approaches with predominantly African American client populations, finding that this model was effective at reducing cocaine and illicit opioid use, improving employment outcomes for clients in methadone maintenance (Silverman et al. 2002; Silverman et al. 2007), reducing substance use during and after treatment, and improving self-reported quality of life (Petry et al. 2004; Petry et al. 2005; Petry et al. 2007). The Living in the Balance intervention, which uses psychoeducation and CBT techniques, has also been evaluated with a mostly African American sample and has been shown to improve treatment retention and reduce substance use (Hoffman et al. 1996).
Another therapy that has been evaluated with African American clients and found effective is supportive–expressive psychotherapy, which reduces substance use and improves psychological functioning for individuals in methadone maintenance (Woody et al. 1987; Woody et al. 1995). Medications for substance abuse can also work well with African American clients. In one large study, African Americans were more likely than Latinos or White Americans to indicate that they found methadone helpful (Gerstein et al. 1997), and in another study, they reported greater perceived quality of life as a result of participation in a methadone program (Geisz 2007). Schroeder et al. (2005) also reported that African Americans in a methadone program had significantly fewer adverse medical events (e.g., infections, gastrointestinal complaints) than did White American participants. African Americans who were being treated for cocaine dependence remained in treatment significantly longer than did other African Americans if they received disulfiram (Milligan et al. 2004).
A review of cultural adaptations of evidence-based practices is given by Bernal and Domenech Rodriguez (2012). For an overview of gender-specific treatment considerations for mental and substance use disorders among African American men and women, see Shorter-Gooden (2009).
Family therapy
African American clients appear more likely to stay connected with their families throughout the course of their addiction. For instance, Bourgois et al. (2006) reported that in comparing African American and White American individuals who injected heroin, African Americans appeared to be more likely to maintain contact with their extended families. Some research also suggests that African Americans with substance use disorders are more likely to have family members with histories of substance abuse, suggesting an even greater need to address substance abuse within the family (Brower and Carey 2003).
Strong family bonds are important in African American cultural groups. African American families are embedded in a complex kinship network of biologically related and unrelated persons. Hence, counselors should be willing to expand the definition of family to a more extended kinship system (Boyd-Franklin 2003; Hines and Boyd-Franklin 2005). Clients need to be asked how they define family, whom they would identify as family or “like family,” who resides with them in their homes, and whom they rely on for help. Hines and Boyd-Franklin (2005) discuss the importance of both blood and nonblood kinship networks for African American families. To build a support network for African American clients, counselors should start by asking clients to identify people (whether biological kin or not) who would be willing and able to support their recovery and then ask clients for permission to contact those people and include them in the treatment process.
Family therapy is often a productive approach to treatment with African Americans (Boyd-Franklin 2003; Hines and Boyd-Franklin 2005; Larkin 2003). However, the extended family can be large and have many ties with other families in a community; therefore, the family therapist sometimes needs to take on other roles to assist with case management or other activities, including involvement in community-wide interventions (Sue 2001). In reviewing specific family therapy approaches for African Americans, Boyd-Franklin (2003) discusses the use of a multisystem family therapy approach, which incorporates an extended network of relationships that play a part in clients' lives. Using this model, social service and other community agencies can be considered a significant part of the family system. Network therapy, which involves clients' extended social networks, has also been found to improve substance use outcomes for African American clients when added to standard treatment (Keller and Galanter 1999). Likewise, the family team conference model can be a useful approach, given that it also engages both families and communities in the helping process by attempting to stimulate extensive mobilization of activity in the formal and informal relationships in and around clients' families (State of New Jersey Department of Human Services 2004).
Advice to Counselors: Strengths of African American Families
African American kinship bonds have historically been sources of strength. Although substance abuse lessens the strength of the family and can erode relationships, counselors can use the inherent strengths of the family to benefit clients and their families (Boyd-Franklin and Karger 2012; Larkin 2003; Reid 2000). Bell-Tolliver et al. (2009) and Hill (1972) suggest that strengths of African American family life include:
- Strong bonds and extensive kinship.
- Adaptability of family roles.
- A strong family hierarchy.
- A strong work orientation.
- A high achievement orientation.
- A strong religious orientation.
Brief structural family therapy and strategic family therapy reduce substance use as well, but research has primarily focused on African American youth (Santisteban et al. 1997; Santisteban et al. 2003; Szapocznik and Williams 2000). Multidimensional family therapy has increased abstinence from substance use among African American adolescents and produced more lasting effects than CBT, but it also has not been evaluated with adult clients (Liddle et al. 2008). In reviewing specific family programs, Larkin (2003) reports promising preliminary data on a family therapy intervention among African Americans in public housing that addresses substance abuse.
The program initially engages families via psychoeducation on substance abuse and its effects on the family, followed by a strength-based family therapy intervention. Despite the small sample size, all 10 families admitted to the program completed treatment, and 7 of 10 family members with substance abuse problems entered recovery and continuing care. Participant surveys indicated that 60 percent of families preferred multiple-family therapy over single-family therapy, and 80 percent preferred services delivered in the housing project community center to other venues.
Engaging Moms is another family-oriented program and intervention developed specifically for African American mothers that has been shown to significantly improve treatment engagement (Dakof et al. 2003). The intervention is designed for women who have children and have been identified as cocaine users. The program focuses on mobilizing family members who would be likely to motivate the mothers to enroll and remain in substance abuse treatment. Research has shown no long-term impact, yet women who received the intervention were significantly more likely to enter treatment (88 percent of women involved in the program versus 46 percent of the control group) and remain for at least 2 weeks.
Group therapy
Because of the communal, cooperative values held by many African Americans, group therapy can be a particularly valuable component of the treatment process (Sue and Sue 2013b). A strong oral tradition is one of many forms of continuity with African tradition maintained in the African American experience; therefore, speaking in groups is generally acceptable to African American clients. However, Bibb and Casimer (2000) note that Black Caribbean Americans can be less comfortable with the group process, particularly the requirement that they self-disclose personal problems to people who are relative strangers. African Americans seem less likely to self-disclose about the past in group settings that include non-Hispanic Whites (Johnson et al. 2011; Richardson and Williams 1990). Consequently, groups composed only of African Americans can be more beneficial. Homogenous African American groups can also be good venues for clients to deal with systemic problems, such as racism and lack of economic opportunities in the African American community (Jones et al. 2000).
Mutual-help groups
A variety of mutual-help groups are available for African Americans entering recovery from substance use and mental disorders. However, most of the literature focuses on 12-Step groups, including Alcoholics Anonymous (AA) and Narcotics Anonymous. Some find that the 12-Step approach warrants careful consideration with African Americans, who can find the concept of powerlessness over substances of abuse to be too similar to experiences of powerlessness via discrimination. Additionally, the disease concept of addiction presented in 12-Step meetings can be difficult for many African Americans (Durant 2005). In some instances, the Black community has changed the mutual-help model for substance use and mental health to make it more empowering and relevant to African American participants. For additional information on the 12 Steps for African Americans, visit Alcoholics Anonymous World Services (AAWS), AA for the Black and African American Alcoholic, available online (http://www.aa.org/pdf/products/p-51_CanAAHelpMeToo.pdf).
Despite their emphasis on the concept of powerlessness, 12-Step programs are significant support systems for many African Americans. In AA's 2011 membership survey, 4 percent of members identified their race as Black (AAWS 2012). Analysis of 2006–2007 NSDUH data showed that African Americans were less likely to use mutual-help groups in the past year for substance use (about 11 percent did) than White Americans (about 67 percent did) or Latinos (about 16 percent did; SAMHSA 2013d). However, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) survey did find that African Americans who had a lifetime drug use disorder diagnosis and had sought help were more than three times as likely to have attended mutual-help meetings as were White Americans or Latinos (Perron et al. 2009). Several other surveys suggest that African Americans with alcohol-related problems are at least as likely to participate in AA as White Americans and that greater problem severity is associated with increased likelihood of participation (Kingree and Sullivan 2002). Of the participants who attended mutual-help group sessions for mental health in the past year, approximately 10 percent were Black or African American, 75 percent were White American, and 11.4 percent were Latino (SAMHSA 2010).
Durant (2005) observes that African American 12-Step participants tend to participate differently in meetings where participants are mostly White Americans than in meetings where most participants are African American. I n some areas, there are 12-Step meetings that are largely or entirely composed of African American members, and some African American clients feel more comfortable participating in these meetings. Mutual-help groups can be particularly helpful for African Americans who consider themselves religious. Maude-Griffin et al. (1998) found that individuals who identified as highly religious did significantly better when receiving 12-Step facilitation than when receiving C B T, but that pattern was reversed for those who did not consider themselves highly religious. Other studies have found that African Americans express a greater degree of comfort with sharing in meetings, and they are more likely to engage in AA services and state that they had a spiritual awakening as a result of AA participation (Bibb and Casimer 2000; Kaskutas et al. 1999; Kingree 1997).
Research suggests that African Americans who attend 12-Step programs have higher levels of affiliation than White Americans in the same programs (Kingree and Sullivan 2002). However, they are less likely to have a sponsor or to read program materials (Kaskutas et al. 1999), and their abstinence appears to be less affected by meeting attendance (Timko et al. 2006). Other research has found that African Americans who participate in 12-Step groups report an increase in the number of people within their social networks who support their recovery efforts (Flynn et al. 2006). Other mutual-help groups for African Americans are available, particularly faith-based programs to support recovery from mental illness and substance use disorders and to aid individuals in the process of transitioning from correctional institutions. For example, the Nation of Islam has been involved in successful substance abuse recovery efforts, especially for incarcerated persons (Sanders 2002; White and Sanders 2004).
Traditional healing and complementary methods
In general, African Americans are less likely to make use of popular alternative or complementary healing methods than White Americans or Latinos (Graham et al. 2005). However, the African American culture and history is steeped in healing traditions passed down through generations, including herbal remedies, root medicines, and so forth (Lynch and Hanson 2011). The acceptance of traditional practices by African American clients and their families does not necessarily indicate that they oppose or reject the use of modern therapeutic approaches or other alternative approaches. They can accept and use all forms of treatment selectively, depending on the perceived nature of their health problems. That said, psychological and substance abuse problems can be seen as having spiritual causes that need to be addressed by traditional healers or religious practices (Boyd-Franklin 2003). Moreover, African Americans are much more likely to use religion or spirituality as a response to physical or psychological problems (Cooper et al. 2003; Dessio et al. 2004; Graham et al. 2005; Nadeem et al. 2008).
African American cultural and religious institutions (see advice box below) play an important role in treatment and recovery, and African Americans who use spirituality or religion to cope with health problems are nearly twice as likely as other African Americans to also make use of complementary or alternative medicine (Dessio et al. 2004). Likewise, African American churches and mosques play a central role in education, politics, recreation, and social welfare in African American communities. To date, African Americans report the highest percentage (87 percent) of religious affiliation of any major racial/ethnic group (Kosmin and Keysar 2009; Pew Forum on Religion and Public Life 2008). Even though most are committed to various Christian denominations (with the Baptist and African Methodist Episcopal churches accounting for the largest percentages), a growing number of African Americans are converts to Islam, and many recent immigrants from Africa to the United States are also Muslims (Boyd-Franklin 2003; Pew Forum on Religion and Public Life 2008).
Advice to Counselors: The Role of African American Religious Institutions in Treatment and Recovery
Within African American communities, religious institutions and clergy often function as service providers as well as counselors (Boyd-Franklin 2003; Reid 2000; Taylor et al. 2000). It is not uncommon for African Americans to approach clergy first when faced with their own or family members' mental health or substance abuse problems, but many African American clergy members believe they are not well-prepared to address those problems (Neighbors et al. 1998; Sexton et al. 2006). According to NESARC data, African Americans are twice as likely as Latinos and nearly three times as likely as White Americans to receive pastoral counseling for their drug use (Perron et al. 2009).
For many African Americans in recovery, churches play a significant role in helping them maintain abstinence (Perron et al. 2009). Beyond pastoral counseling, research suggests that other means of engagement within the church can lead to recovery. For example, participation in religious services has been associated with significantly better outcomes for African American men in continuing care following court-mandated treatment (Brown et al. 2004). Stahler et al. (2007) also report successful use of peer mentors drawn from churches for African American women in treatment, marked by significantly fewer drug-positive urine samples in the 6 months following treatment.
Counselors working with African American clients should prepare to include churches, mosques, or other faith communities in the therapeutic process, and they should develop a list of appropriate spiritual resources in the community. Treatment providers may consider involving African American clergy in treatment programs to improve clergy members' understanding of behavioral health problems and treatments and to better engage clients and their families. Programs can conduct outreach with local faith-based institutions and clergy to facilitate treatment referrals (Taylor et al. 2000).
Relapse prevention and recovery
African Americans appear to be responsive to continuing care participation and recovery activities associated with substance use and mental disorders, yet research is very limited. According to NESARC data (Dawson et al. 2005), African Americans in recovery from alcohol dependence were more than twice as likely as White Americans to maintain abstinence rather than just limiting alcohol consumption or changing drinking patterns. In another study analyzing the use of continuing care following residential treatment in the U.S. Department of Veterans Affairs care system, African American men were significantly more likely than White Americans to participate in continuing care (Harris et al. 2006). Other research evaluating continuing care for African American men who had been mandated to outpatient treatment by a parole or probation office found that participants assigned to a continuing care intervention were almost three times as likely to be abstinent and five times less likely to be using any drugs on a weekly basis during the 6-month follow-up period compared with those who did not receive continuing care (Brown et al. 2004).
In evaluating appropriate relapse prevention strategies for African American clients, Walton et al. (2001) found that African American clients leaving substance abuse treatment reported fewer cravings, greater use of coping strategies, and a greater belief in their self-efficacy. However, they also expected to be involved in fewer sober leisure activities, to be exposed to greater amounts of substance use, and to have a greater need for continuing care services (e.g., housing, medical care, assistance with employment). Walton notes that these findings could reflect a tendency of African American clients to underestimate the difficulties they will face after treatment; they report a greater need for resources and greater exposure to substance use, but they still have a greater belief in their ability to remain free of substances. Although an individual's belief in coping can have a positive effect on initially managing high-risk situations, it also can lead to a failure to recognize the level of risk in a given situation, anticipate the consequences, secure resources and appropriate support when needed, or engage in coping behaviors conducive to maintaining recovery. Counselors can help clients practice coping skills by role-playing, even if clients are confident that they can manage difficult or high-risk situations.
Counseling for Asian Americans, Native Hawaiians, and Other Pacific Islanders
Asian Americans, per the U.S. Census Bureau definition, are people whose origins are in the Far East, Southeast Asia, or the Indian subcontinent (Humes et al. 2011). The term includes East Asians (e.g., Chinese, Japanese, and Korean Americans), Southeast Asians (e.g., Cambodian, Laotian, and Vietnamese Americans), Filipinos, Asian Indians, and Central Asians (e.g., Mongolian and Uzbek Americans). In the 2010 Census, people who identified solely as Asian American made up 4.8 percent of the population, and those who identified as Asian American along with one or more other races made up an additional 0.9 percent. Census data includes specific information on people who identify as Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, and “other Asians.” The largest Asian populations in the United States are Chinese Americans, Filipino Americans, Asian Indian Americans, Korean Americans, and Vietnamese Americans. Asian Americans overwhelmingly live in urban areas, and more than half (51 percent) live in just three states (NY, CA, and HI; Hoeffel et al. 2012).
Not all people with origins in Asia belong to what is commonly conceived of as the Asian race. Some Asian Indians, for example, self-identify as White American. For this reason, among others, counselors should be careful to learn from their Asian American clients how they identify themselves and which national heritages they claim. Counselors should recognize that clients who appear to be Asian may not necessarily think of themselves primarily as persons of Asian ancestry or have a deep awareness of the traditions and values of their countries of origin. For example, Asian orphans who have been adopted in the United States and raised as Americans in White American families may have very little connection with the cultural groups of their biological parents (St. Martin 2005). Counselors should not make generalizations across Asian cultures; each culture is quite distinct.
Little literature on substance use and mental disorders, rates of co-occurrence, and treatment among Asian Americans focuses on behavioral health treatment for Native Hawaiians and Pacific Islanders; thus, a text box at the end of this section summarizes available information.
Beliefs About and Traditions Involving Substance Use
Within many Asian societies, the use of intoxicants is tolerated within specific contexts. For example, in some Asian cultural groups, alcohol is believed to have curative, ceremonial, or beneficial value. Among pregnant Cambodian women, small amounts of herbal medicines with an alcohol base are sometimes used to ensure an easier delivery. Following childbirth, similar medicines are generally used to increase blood circulation (Amodeo et al. 1997). Some Chinese people believe that alcohol restores the flow of qi (i.e., the life force). The written Chinese character for “doctor” contains the character for alcohol, which implies the use of alcohol for medicinal purposes.
Some Asian American cultural groups make allowances for the use of other substances. Marijuana, for instance, has been used medicinally in parts of Southeast Asia for many years (Iversen 2000; Martin 1975). However, some Asian Americans tend to view illicit substance use and abuse as a serious breach of acceptable behavior that cannot readily be discussed. Nonetheless, there are broad differences in Asian cultures' perspectives on substance use, thus requiring counselors to obtain more specific information during intake and subsequent encounters.
Acknowledging a substance abuse problem often leads to shame for Asian American clients and their families. Families may deny the problem and inadvertently, or even intentionally, isolate members who abuse substances (Chang 2000). For example, some Cambodian and Korean Americans perceive alcohol abuse and dependence as the result of moral weakness, which brings shame to the family (Amodeo et al. 2004; Kwon-Ahn 2001).
Substance Use and Substance Use Disorders
According to the 2012 NSDUH, Asian Americans use alcohol, cigarettes, and illicit substances less frequently and less heavily than members of any other major racial/ethnic group (SAMHSA 2013d). However, large surveys may undercount Asian American substance use and abuse, as they are typically conducted in English and Spanish only (Wong et al. 2007b). Despite the limitations of research, data suggest that although Asian Americans use illicit substances and alcohol less frequently than other Americans, substance abuse problems have been increasing among Asian Americans. The longer Asian Americans reside in the United States, the more their substance use resembles that of other Americans. Excessive alcohol use, intoxication, and substance use disorders are more prevalent among Asians born in the United States than among foreign-born Asians living in the United States (Szaflarski et al. 2011).
Among Asian Americans who entered substance abuse treatment between 2000 and 2010, methamphetamine and marijuana were the most commonly reported illicit drugs (SAMHSA, CBHSQ 2012). Methamphetamine abuse among Asian Americans is particularly high in Hawaii and on the West Coast (OAS 2005a). As with other racial and ethnic groups, numerous factors—such as age, birth country, immigration history, acculturation, employment, geographic location, and income—add complexity to any conclusions about prevalence among specific Asian cultural groups. Asian Americans who are recent immigrants, highly acculturated, unemployed, or living in Western states are generally more likely than other Asian Americans to abuse drugs or alcohol (Makimoto 1998). For example, according to the National Latino and Asian American Study (NLAAS), Asians who are more acculturated are at greater risk for prescription drug abuse (Watkins and Ford 2011).
There are variations among particular groups of Asians; some Asian cultural groups have different attitudes toward substance use than others, and these differences tend to be obscured in large-scale surveys. Researchers have found that Korean American college students drank more frequently and drank greater quantities than did Chinese American students at the same schools and were more likely to consider drinking socially acceptable (Chang et al. 2008). Another study in the District of Columbia and surrounding metropolitan area compared substance use among different groups of Southeast Asians (i.e., Cambodian, Laotian, and Vietnamese Americans); Vietnamese Americans had the highest rates of alcohol use, but Cambodian Americans had the highest rates of illicit drug use (Wong et al. 2007b). Research in San Francisco found Chinese Americans to be less likely than Vietnamese or Filipino Americans to use illicit drugs, whereas Filipino Americans had the highest rate of illicit drug use (Nemoto et al. 1999). In that same study, Filipino American immigrants were also significantly more likely to have begun using substances prior to immigrating than were Chinese or Vietnamese immigrants. Other studies have found that Filipino Americans are more likely to use illicit drugs and to inject drugs than other Asian American populations (see review in Nemoto et al. 2002).
To date, the largest national study to assess substance use and mental disorders across Asian American groups is the NLAAS (Takeuchi et al. 2007). This study found that Filipino American men were 2.38 times more likely to have a lifetime substance use disorder than were Chinese American men, whereas the differences among women of diverse Asian ethnicities were much smaller. Other research suggests that Korean Americans are more likely to have family histories of alcohol dependence than are Chinese Americans (Ebberhart et al. 2003).
Besides the variations across different cultures, substance use and abuse among Asian Americans is also influenced by age. Substance abuse appears higher for young Asian Americans than for those who are older (possibly reflecting differences in acculturation). A study conducted in New York City showed that Asian American junior and senior high school students had the lowest percentage of heavy drinkers of any ethnic group, but those who were heavy drinkers drank twice as much daily as those who did not drink heavily (Makimoto 1998). Asian American youth, especially immigrants, tend to start using substances at a later age than members of other ethnic groups, which could be a factor in the lower levels of abuse seen among Asian Americans.
Despite rates of substance use disorders among Asian Americans having increased over time, research has regularly found that, of all major racial/ethnic groups in United States, Asian Americans have the lowest rates of alcohol use disorders (Grant et al. 2004; SAMHSA 2012b). This phenomenon has typically been explained in part by the fact that some Asians lack the enzyme aldehyde dehydrogenase, which chemically breaks down alcohol (McKim 2003). Thus, high levels of acetaldehyde, a byproduct of alcohol metabolism, accumulate and cause an unpleasant flushing response (Yang 2002). The alcohol flushing response primarily manifests as flushing of the neck and face but can also include nausea, headaches, dizziness, and other symptoms.
Additional factors that could play a part in increasing the likelihood of substance use disorders among Asian Americans include experiences of racism and the absence of ethnic identification. Compared with Asian Americans who do not have alcohol use disorders, Asian Americans who have alcohol use disorders are more than five times as likely to report unfair treatment because of their race and are more than twice as likely to deny strong ethnic identification (Chae et al. 2008). Compared with other racial and ethnic groups, Asian Americans who drink heavily are more likely to have friends or peers who also drink heavily (Chi et al. 1989).
Mental and Co-Occurring Disorders
Overall, health and mental health are not seen as two distinct entities by Asian American cultural groups. Most Asian American views focus on the importance of virtue, maturity, and self-control and find full emotional expression indicative of a lack of maturity and self-discipline (Cheung 2009). Given the potential shame they often associate with mental disorders and their typically holistic worldview of health and illness, Asian Americans are more likely to present with somatic complaints and less likely to present with symptoms of psychological distress and impairment (Hsu and Folstein 1997; Kim et al. 2004; Room et al. 2001; U.S. Department of Health and Human Services [HHS] 2001; Zhang et al. 1998), even though mental illness appears to be nearly as common among Asian Americans as it is in other ethnic/racial groups. In 2009, approximately 15.5 percent of Asians reported a mental illness in the past y e a r, but only 2 percent reported past-year occurrence of serious mental illness (SAMHSA 2012a). Asian Americans have a lower incidence of CODs than other racial/ethnic groups because the prevalence of substance use disorders in this population is lower. In the 2012 NSDUH, 0.3 percent of Asian Americans indicated co-occurring serious psychological distress and substance use disorders, and 1.1 percent had some symptoms of mental distress along with a substance use disorder—the lowest rates of any major racial/ethnic group in the survey (SAMHSA 2013c).
Considerable variation in the types of mental disorders diagnosed among diverse Asian American communities is evident, although it is unclear to what extent this reflects diagnostic and/or self-selection biases. For example, Barreto and Segal (2005) found that Southeast Asians were more likely to be treated for major depression than other Asians or members of other ethnic/racial groups; East Asians were the most likely of all Asian American groups to be treated for schizophrenia (nearly twice as likely as White Americans). Traumatic experiences and PTSD can be particularly difficult to uncover in some Asian American clients. Although Asian Americans are as likely to experience traumatic events (e.g., wars experienced by first-generation immigrants from countries such as Vietnam and Cambodia) in their lives, their cultural responses to trauma can conceal its psychological effects. For instance, some Asian cultural groups believe that stoic acceptance is the most appropriate response to adversity (Lee and Mock 2005a, b).
Treatment Patterns
Treatment-seeking rates for mental illness are low among most Asian populations, with rates varying by specific ethnic/cultural heritage and, possibly, level of acculturation (Abe-Kim et al. 2007; Barreto and Segal 2005; Lee and Mock 2005a, b). Asian Americans who seek help for psychological problems will most likely consult family members, clergy, or traditional healers before mental health professionals, in part because of a lack of culturally and linguistically appropriate mental health services available to them (HHS 2001; Spencer and Chen 2004). However, among those Asian Americans who seek behavioral health treatment, the amount of services used is relatively high (Barreto and Segal 2005).
Asian Americans tend to enter treatment with less severe substance abuse problems than members of other ethnic/racial groups and have more stable living situations and fewer criminal justice problems upon leaving treatment (Niv et al. 2007). However, for Asian Americans involved in the criminal justice system, there is a more pronounced relationship between crime and drug abuse than for other ethnic and racial groups. In the early 1990s, an estimated 95 percent of Asian Americans in California prisons were there because of drug-related crimes (Kuramoto 1994). According to SAMHSA's 2010 TEDS data, 48.5 percent of Asian Americans in treatment were referred by the criminal justice system in that year, compared with 36.4 percent of African Americans and 36.6 percent of White Americans (SAMHSA, CBHSQ 2012). According to 2010 NSDUH data regarding individuals who reported a need for treatment but did not receive it in the prior year, Asian Americans were also the most likely of all major racial/ethnic groups to report that they could not afford or had no insurance coverage for substance abuse treatment (SAMHSA, CBHSQ 2011).
Beliefs and Attitudes About Treatment
Compared with the general population, Asian Americans are less likely to have confidence in their medical practitioners, feel respected by their doctors, or believe that they are involved in healthcare decisions. Many also believe that their doctors do not have a sufficient understanding of their backgrounds and values; this is particularly true for Korean Americans (Hughes 2002). Even so, Asian Americans, especially more recent immigrants, seem more likely to seek help for mental and substance use disorders from general medical providers than from specialized treatment providers (Abe-Kim et al. 2007). Many Asian American immigrants underuse healthcare services due to confusion about eligibility and fears of jeopardizing their residency status (HHS 2001).
As with other groups, discrimination, acculturation stress, and immigration and generational status, along with language needs, have a large influence on behavioral health and treatment-seeking for Asian Americans (Meyer et al. 2012; Miller et al. 2011). The NLAAS found that although rates of behavioral health service use were lower for Asian Americans who immigrated recently than for the general population, those rates increased significantly fo r U.S.-born Asian Americans; third-generation U.S.-born individuals' rates of service use also were relatively high (Abe-Kim et al. 2007). Of those Asian Americans who had any mental disorder diagnosis in the prior year, 62.6 percent of third-generation Americans sought help for it in the prior year compared with 30.4 percent of first-generation Americans.
Overall, Asian Americans place less value on substance abuse treatment than other population groups and are less likely to use such services (Yu and Warner 2012). Niv et al. (2007) found that Asian and Pacific Islanders entering substance abuse treatment programs in California expressed significantly more negative attitudes toward treatment and rated it as significantly less important than did others entering treatment. Seeking help for substance abuse can be seen, in some Asian American cultural groups, as an admission of weakness that is shameful in itself or as an interference with family obligations (Masson et al. 2013). Among 2010 NSDUH respondents who stated a need for substance abuse treatment in the prior year but did not receive it, Asian Americans were more likely than members of all other major racial/ethnic groups to say that they could handle the problem without treatment or that they did not believe treatment would help (SAMHSA 2011c). Combining NSDUH data from 2003 to 2011 NSDUH, Asian Americans who needed but did not receive treatment in the past year were the least likely of all major ethnic/racial groups to express a need for such treatment (SAMHSA, CBHSQ 2013c).
Treatment Issues and Considerations
It is important for counselors to approach presenting problems through clients' culturally based explanations of their own issues rather than imposing views that could alter their acceptance of treatment. In Asian cultural groups, the physical and emotional aspects of an individual's life are undifferentiated (e.g., the physical rather than emotional or psychological aspect of a problem can be the focus for many Asian Americans); thus, problems as well as remedies are typically handled holistically. Some Asian Americans with traditional backgrounds do not readily accept Western biopsychosocial explanations for substance use and mental disorders. Counselors should promote discussions focused on clients' understanding of their presenting problems as well as any approaches the clients have used to address them. Subsequently, presenting problems need to be reconceptualized in language that embraces the clients' perspectives (e.g., an imbalance in yin and yang, a disruption in chi; Lee and Mock 2005a,b). It is advisable to educate Asian American clients on the role of the counselor/therapist, the purpose of therapeutic interventions, and how particular aspects of the treatment process (e.g., assessment) can help clients with their presenting problems (Lee and Mock 2005a,b; Sue 2001). Asian American clients who receive such education participate in treatment longer and express greater satisfaction with it (Wong et al. 2007a).
As with other racial/ethnic groups, Asian American clients are responsive to a warm and empathic approach. Counselors should realize, though, that building a strong, trusting relationship takes time. Among Asian American clients, humiliation and shame can permeate the treatment process and derail engagement with services. Thus, it is essential to assess and discuss client beliefs about shame (see the “Assessing Shame in Asian American Clients” advice box on the next page). In some cases, self-disclosure can be helpful, but the counselor should be careful not to self-disclose in a way that will threaten his or her position of respect with Asian American clients.
Asian American clients may look to counselors for expertise and authority. Counselors should attempt to build client confidence in the first session by introducing themselves by title, displaying diplomas, and mentioning his or her experience with other clients who have similar problems (Kim 1985; Lee and Mock 2005a,b). Asian American clients may expect and be most comfortable with formalism on the part of counselors, especially at the beginning of treatment and prior to assessment of clients' needs (Paniagua 1998). Many Asian American clients expect counselors to be directive (Leong and Lee 2008). Passivity on the part of the counselor can be misinterpreted as a lack of concern or confidence.
Advice to Counselors: Assessing Shame in Asian American Clients
Shame and humiliation can be significant barriers to treatment engagement for Asian Americans. Gaw (1993) suggests that the presence of the following factors may indicate that a client has shame about seeking treatment:
- The client or a family member is extremely concerned about the qualifications of the counselor.
- The client is hesitant to involve others in the treatment process.
- The client is excessively worried about confidentiality.
- The client refuses to cover expenses with private insurance.
- The client frequently misses or arrives late for treatment.
- Family members refuse to support treatment.
- The client insists on having a White American counselor to avoid opening up to another Asian.
- The client refuses treatment even when severe problems are evident.
Counselors who are unaccustomed to working with Asian populations will likely encounter conflict between their theoretical worldview of counseling and the deference to authority and avoidance of confrontation that is common among more traditional Asian American clients. Some clients can be hesitant to contradict the counselor or even to voice their own opinions. Confrontation can be seen as something to avoid whenever possible. Furthermore, many Asian cultural groups have high-context styles of communication, meaning that members often place greater importance on nonverbal cues and the context of verbal messages than on the explicit content of messages (Hall 1976). Asian Americans often use indirect communication, relying on subtle gestures, expressions, or word choices to convey meaning without being openly confrontational. Counselors must not only be observant of nuances in meaning, but also learn about verbal and nonverbal communication styles specific to Asian cultural groups (for a review of guidelines to use when working with Asian Americans, see Gallardo et al. 2012).
Asian American clients appear to respond more favorably to treatment in programs that provide services to other Asian clients. Takeuchi et al. (1995) found that Asian Americans were much more likely to return to mental health clinics where most clients were Asian American than to programs where that was not the case (98 percent and 64 percent returned, respectively). When demographic differences were controlled for, those who attended programs that had predominantly Asian clients were 15 times more likely to return after the initial visit. Asian Americans were also more likely to stay in treatment when matched with an Asian American counselor regardless of the type of program they attended. Sue et al. (1991) also found that Asian American clients attended significantly more treatment sessions if matched with an Asian American counselor.
Among Asian American women, crucial strategies include reducing the shame of substance abuse and focusing on the promotion of overall health rather than just addressing substance abuse. Such strategies reduce the chance of a woman and her family seeing substance abuse as an individual flaw. Home visits, when agreed in advance with the client, can be appropriate in some cases as a way to gain the trust of, and show respect for, Asian American women. Asian American women may not be as successful in mixed-gender groups if strict gender roles exist whereby communication is constricted within and outside the family; women will likely remain silent or defer to the men in the group (Chang 2000). For more information on treating women, see Treatment Improvement Protocol (TIP) 51, Substance Abuse Treatment: Addressing the Specific Needs of Women (CSAT 2009c).
Advice to Administrators: Culturally Responsive Program Development
Behavioral health service program administrators can improve engagement and retention of Asian clients by making culturally appropriate accommodations in their programs. The accommodations required will vary according to the specific cultural groups, language preferences, and levels of acculturation in question. The following culturally responsive program suggestions were initially identified for Cambodian clients but can be adapted to match the unique needs of other Asian clients from different ethnic and cultural backgrounds:
- Create an advisory committee using representatives from the community.
- Incorporate cultural knowledge and maintain flexible attitudes as a counselor.
- Use cotherapist teams in which one member is Asian and bilingual.
- Provide services in the clients' primary language.
- Develop culturally specific questionnaires for intake to capture information that may be missed by standard questionnaires.
- Conduct culturally appropriate assessments of trauma that ask about the traumatic experiences common to the population in question.
- Visit client homes to improve family involvement in treatment.
- Provide support to families during transitions from and to professional care.
- Emphasize traditional values.
- Explore client coping mechanisms that draw upon cultural strengths.
- Use acupuncture or other traditional practices for detoxification.
- Integrate Buddhist ideas, values, and practices into treatment when appropriate.
- Emphasize relationship-building; help clients with life problems beyond behavioral health concerns.
- Provide concrete services, such as housing assistance and legal help.
Sources: Amodeo et al. 2004; Park et al. 2011.
Theoretical Approaches and Treatment Interventions
Some Asian cultural groups emphasize cognitions. For instance, Asian cultural groups that have a Buddhist tradition, such as the Chinese, view behavior as controlled by thought. Thus, they accept that addressing cognitive patterns will affect behaviors (Chen 1995). Some Asian cultural groups encourage a stoic attitude toward problems, teaching emotional suppression as a coping response to strong feelings (Amodeo et al. 2004; Castro et al. 1999b; Lee and Mock 2005a,b; Sue 2001). Treatment can be more effective if providers avoid approaches that target emotional responses and instead use strategies that are more indirect in discussing feelings (e.g., saying “that might make some people feel angry” rather than asking directly what the client is feeling; Sue 2001).
Asian Americans often prefer a solution-focused approach to treatment that provides them with concrete strategies for addressing specific problems (Sue 2001). Even though little research is available in evaluating specific interventions with Asian Americans, clinicians tend to recommend cognitive–behavioral, solution-focused, family, and acceptance commitment therapies (Chang 2000; Hall et al. 2011; Iwamasa et al. 2006; Rastogi and Wadhwa 2006; Sue 2001). Asian American clients are likely to expect that their counselors take an active role in structuring the therapy session and provide clear guidelines about what they expect from clients. CBT has the advantages of being problem focused and time limited, which will likely increase its appeal for many Asian Americans who might see other types of therapy as failing to achieve real goals (Iwamasa et al. 2006). Although specific data on the effectiveness of CBT among Asian Americans is not available, there is some research indicating that CBT is effective for treating depressive symptoms in Asians (Dai et al. 1999; Fujisawa et al. 2010). In China, a Chinese Taoist version of CBT has been developed to treat anxiety disorders and was found to be effective, especially in conjunction with medication (Zhang et al. 2002).
Family therapy
Some Asian Americans, particularly those who are less acculturated, prefer individual therapy to group or family interventions because it better enables them to save face and keep their privacy (Kuramoto 1994). Some clients may wish to enter treatment secretly so that they can keep their families and friends from knowing about their problems. Once treatment is initiated, counselors should strongly reinforce the wisdom of seeking help through statements such as “you show concern for your husband by seeking help” or “you are obviously a caring father to seek this help.”
The norm in Asian families is that “all problems (including physical and mental problems) must be shared only among family members”; sharing with others can cause shame and guilt, exacerbating problems (Paniagua 1998, pp. 59–60). Counselors should expect to take more time than usual to learn about clients' situations, anticipate client needs for reassurance in divulging sensitive information, and frame discussions in a culturally competent way. For example, counselors can assure clients that discussing problems is a step toward resuming their full share of responsibility in their families and removing some of the stress their families have been feeling.
For most Asian Americans, particularly those who are less acculturated, successful treatment involves the client's family (Chang 2000; Kim et al. 2004; Rastogi and Wadhwa 2006). Even in individual treatment, it is important to understand the client's family and his or her relationship with its members, the dynamics and style of the family, and the family's role in the client's substance abuse (Meyer et al. 2012). Particularly among Asian American women, family involvement can be essential due to the client's concern about being responsive to her family's needs. Nonetheless, involving the family can be quite difficult, as both male and female clients may wish to conceal their substance abuse from their families because of the shame that it brings.
Advice to Counselors: Culturally Responsive Family Therapy Guidelines for Asian Families
Kim et al. (2004) reviewed references that provide guidelines for family therapy with Korean Americans. They established 11 essential ingredients applicable to Korean and other Asian American groups and families. To provide culturally responsive therapy to Asian Americans, counselors should:
- Assess support from community and extended family systems.
- Assess immigration history, if appropriate.
- Establish credibility as a professional in the initial meeting with the family.
- Explain the key principles and expectations of family therapy and the family roles (especially elders/decisionmakers) in the process.
- Enable clients, particularly male elders or decisionmakers, to save face.
- Validate and address somatic complaints.
- Be both problem focused and present focused.
- Be directive in guiding therapy.
- Respect the family's hierarchy.
- Avoid being confrontational and facilitate interactions that are nonconfrontational.
- Reframe problems in positive terms.
Source: Kim et al. 2004.
To engage family members in the client's treatment, the counselor first needs to be familiar with the way the family functions. Different acculturation levels among individual family members and across generations can affect how the family functions, producing significant stress and internal conflict. Also, the counselor must be aware of how gender roles and generational status influence the communication patterns and rules within each family (e.g., expectations of how a child addresses a parent, the potential relegation of authority among female family members). Even more than for other clients, it is critical for Asian Americans to “avoid embarrassing the family members in front of each other. The counselor should always protect the dignity and self-respect of the client and his or her family” (Paniagua 1998, p. 71).
Group therapy
Group therapy may not be a good choice for Asian Americans, as many prefer individual therapy (Lai 2001; Sandhu and Malik 2001). Paniagua (1998, p. 73) suggests that “group therapy…would be appropriate in those cases in which the client's support system (relatives and close friends) is not available and an alternative support system is quickly needed.” Some Asian Americans participating in group therapy will find it difficult to be assertive in a group setting, preferring to let others talk. They can also abide by more traditional roles in this context; men might not want to divulge their problems in front of women, women can feel uncomfortable speaking in front of men, and both men and women might avoid contradicting another person in group (especially an older person). It may not make sense to Asian American clients to hear about the problems of strangers who are not part of their community.
Asian Americans are likely to be motivated to work for the good of the group; presenting group goals in this framework can garner active participation. Still, in group settings and in other instances, Asian American clients may expect a fair amount of direction from the group leader. Chen (1995) described leadership of a culturally specific therapy group for Chinese Americans, noting that clients expect a group leader to act with authority and give more credence to his or her expertise than to other group members. If members of the group belong to the same Asian American community, the issue of confidentiality will loom large, because the community is often small. Asian cultural groups generally appreciate education in more formal settings, so psychoeducation groups can work well for Asian Americans. It is possible for a psychoeducational group with Asian American participants to evolve comfortably into group therapy.
Mutual-help groups
According to 2012 NSDUH data, Asian Americans were less likely than other racial and ethnic groups to report the use of mutual-help groups in the past year (SAMHSA 2013d). Mutual-help groups can be challenging for Asian Americans who find it difficult and shaming to self-disclose publicly. The degree of emotion and candor within these groups can further alienate traditional Asian American clients. Furthermore, linguistically appropriate mutual-help groups are not always available for people who do not speak English. Highly acculturated Asian Americans may perceive participation in mutual-help groups as less of a problem, but nevertheless, Asian Americans can benefit from culture-specific mutual-help groups where norms of interpersonal interaction are shared. Asian American 12-Step groups are available in some locales. It is important for counselors to assess client attitudes toward mutual-help participation and find alternative strategies and resources, including encouragement to attend without sharing (Sandhu and Malik 2001).
Although they are not mutual-help groups in the traditional sense, mutual aid societies and associations are important in some Asian American communities. Some mutual aid societies have long histories and have provided assistance ranging from financial loans to help with childcare and funerals. The Chinese have family associations for people with the same last name who share celebrations and offer each other help. Japanese, Chinese, and South Asians have specific associations for people from the same province or village. For some Asian American groups, such as Koreans, churches are the primary organizational vehicles for assistance. These social support groups can be important resources for Asian American clients, their families, and the behavioral health agencies that provide services to them.
Traditional healing and complementary methods
Asian Americans are twice as likely as other Americans to report making use of acupuncture and traditional healers. Even though there is considerable variation in their use of complementary and traditional medicine (Hughes 2002), many Asian Americans highly regard traditional healers, herbal preparations, and other culturally specific interventions as a means of restoring harmony and balance. However, Asian American clients do not always readily disclose the use of traditional medicine to Western treatment providers. Ahn et al. (2006) found that about two-thirds of Chinese and Vietnamese Americans who spoke no or limited English had used traditional medicine, but only 7.6 percent had discussed the use of these therapies with their Western medical providers.
Traditional treatment to restore physical and emotional balance for Asian Americans occurs through a variety of culture-specific interventions. For example, some Southeast Asian cultural groups practice cao gio—massaging the skin with ointment and hot coins (Chan and Chen 2011). The Chinese have developed enormously complex systems of medical treatment over centuries of pragmatic experimentation. Traditional herbal medicine combines plant substances according to precise formulas to have the desired influence on the affected organs of the body. Acupuncture techniques involve regulating the flow of energy (qi) through the body by inserting needles at precise locations called acupuncture points. In traditional Chinese medicine, which has influenced traditional medical practices in other Asian cultural groups, illness is seen as an imbalance of yin and yang; a return to physical wellness can require introducing elements such as herbs to increase yin or yang as needed (Torsch and Ma 2000).
Among less acculturated Asian Americans, Western medicine, including Western behavioral health services, can be insufficient to deal with a problem such as substance abuse and its effects on clients and their families. For example, all health problems for the Hmong (whether physical or psychological) are considered spiritual in nature; if providers ignore the clients' understanding of their problems as spiritual maladies, they are unlikely to effect positive change (Fadiman 1997). Even for more acculturated Asian Americans, the use of traditional healing methods and spirituality can be a very important aspect of treatment (see Chan and Chen 2011 for an overview of health beliefs and practices). Such use can provide a spiritual connection that helps manage feelings that are especially difficult to express to others. Many practices associated with meditation, yoga, and Eastern religious traditions can help disperse the stress and anxiety experienced during treatment and recovery. In the United States, there are few examples of culturally specific treatment programs that focus on Asian religious or spiritual treatment; however, there are programs overseas, such as the Thai Buddhist treatment center described by Barrett (1997).
Behavioral Health Counseling for Native Hawaiians and Other Pacific Islanders
The ancestors of Native Hawaiians and other Pacific Islanders were the original inhabitants of Hawaii, Guam, Samoa, and other Pacific islands. The population of Native Hawaiians and other Pacific Islanders grew more than three times faster than the total U.S. population from 2000 to 2010. More than half of Native Hawaiian and other Pacific Islanders live in Hawaii and California. The largest Pacific Islander populations in the United States comprise Hawaiians, Samoans, and Chamorros—the indigenous people of the Mariana Islands, of which Guam is the largest (Hixson et al. 2012).
Native Hawaiians and other Pacific Islanders make up a relatively small proportion of the total United States population. In the 2010 Census, 540,000 people, or 0.2 percent of the population, reported their race as Native Hawaiian or other Pacific Islander, and another 685,000 people (0.2 percent of the population) stated that they were Native Hawaiian or other Pacific Islander in addition to one or more other races (Hixson et al. 2012). The largest concentration of Native Hawaiians and other Pacific Islanders is in Hawaii, where individuals with at least some of this ancestry made up 23.3 percent of the population.
In 2012, according to NSDUH data, 5.4 percent of Native Hawaiians and other Pacific Islanders interviewed had a substance use disorder in the prior year, and 7.8 percent engaged in current illicit drug use (SAMHSA 2013d). Binge and heavy drinking appear to be relatively high, especially among Native Hawaiian/Pacific Islander women. Data from the 2001–2011 TEDS surveys indicate that the most common primary substances of abuse among Native Hawaiians and other Pacific Islanders entering substance abuse treatment are alcohol, cannabis, and methamphetamine (SAMHSA 2013c). Because of its relatively small size, many studies have either ignored or been unable to make conclusions about substance use and abuse in this population; other research has grouped Native Hawaiians and other Pacific Islanders together with Asians (more for the sake of convenience than for underlying cultural similarities).
According to NSDUH data, 1.8 percent of adult Native Hawaiians and other Pacific Islanders reported serious mental illness. Insufficient data were available to analyze past-year mental illness rates (SAMHSA 2013c). Similar to substance use data, specific mental health data are limited across national studies, primarily because the population has been grouped with Asians. However, the evidence that is available suggests that Native Hawaiians are less likely than other racial/ethnic groups in Hawaii to access treatment services even though they experience higher rates of mental health problems (for a review of health beliefs and practices, see Mokuau and Tauili'ili 2011).
A few examples of culturally specific interventions for Native Hawaiians have been presented in the literature. For example, the Rural Hawai'i Behavioral Health Program, which provides substance abuse and mental health services to Native Hawaiians living in rural areas, incorporates Native Hawaiian beliefs and practices into all areas of the program, emphasizing the value of 'ohana (family) relations, including the importance of respecting and honoring ancestors and elders and passing on cultural ways to the next generation. Program staff members are trained in Native Hawaiian culture and beliefs, including spirituality and the essential value of graciousness, the honoring of mana (life energy), healing rituals such as pule (prayer), the use of healing herbs, and Native Hawaiian beliefs about the causes of illness, such as wrongdoing and physical disruption (Oliveira et al. 2006).
Ho'oponopono is a form of group therapy used by Native Hawaiians; it involves family members and is facilitated by a Küpuna (elder). A qualitative study by Morelli and Fong (2000) of Ho'oponopono with pregnant or postpartum women with substance use disorders (primarily methamphetamine abuse) reported high client satisfaction and positive outcomes (80 percent were abstinent 2 years after treatment). The Na Wahine Makalapua Project, sponsored by the Hawaii Department of Health's Alcohol and Drug Abuse Division and SAMHSA's Center for Substance Abuse Prevention, uses elements of Hawaiian culture to treat women with substance use disorders, such as by having Küpuna counsel younger generations.
Asian Americans are much more likely than members of other racial/ethnic groups to label themselves as secular, agnostic, or atheist (Kosmin and Keysar 2009; Pew Forum on Religion and Public Life 2008). That said, a substantial number of Asian Americans still have religious affiliations. About 45 percent are Protestant; 17 percent, Catholic; 14 percent, Hindu; 9 percent, Buddhist; and 4 percent, Muslim (Pew Forum on Religion and Public Life 2008). More acculturated Asian Americans are likely to enter treatment through medical settings and to be comfortable with a medical model for treatment, but those who are less acculturated or are foreign-born can prefer the use of traditional healing and/or religious traditions and beliefs as part of their treatment (Ja and Yuen 1997). Religious institutions can play an important part in the treatment of some groups of Asian Americans. For example, Kwon-Ahn (2001) notes that many Korean Americans, particularly more recent immigrants, turn to Christian clergy or church groups for assistance with family and personal problems, such as substance abuse, before seeking professional help. Amodeo et al. (2004) suggest that, in working with Cambodian immigrants, providers integrate Buddhist philosophy and practices into treatment, and, if possible, partner with Buddhist temples to facilitate treatment entry or to provide services for clients who choose to reside in Buddhist temples.
Relapse prevention and recovery
Little research has evaluated relapse prevention and recovery promotion strategies specifically for Asian Americans. However, issues involving shame can make the adjustment to abstinence difficult for Asian clients. Counselors should take this into account and address difficulties that can arise for clients with families who have shame about mental illness or substance use disorders. To date, there are no indications that standard approaches are unsuitable for Asian American clients. For more information on these approaches, see the planned TIP, Relapse Prevention and Recovery Promotion in Behavioral Health Services (SAMHSA planned e).
Counseling for Hispanics and Latinos
The terms “Hispanic” and “Latino” refer to people whose cultural origins are in Spain and Portugal or the countries of the Western Hemisphere whose culture is significantly influenced by Spanish or Portuguese colonization. Technically, a distinction can be drawn between Hispanic (literally meaning people from Spain or its former colonies) and Latino (which refers to persons from countries ranging from Mexico to Central and South America and the Caribbean that were colonized by Spain, and also including Portugal and its former colonies); this TIP uses the more inclusive term (Latino), except when research specifically indicates the other. The term “Latina” refers to a woman of Latino descent.
Latinos are an ethnic rather than a racial group; Latinos can be of any race. According to 2010 Census data, Latinos made up 16 percent of the total United States population; they are its fastest growing ethnic group (Ennis et al. 2011). Latinos include more than 30 national and cultural subgroups that vary by national origin, race, generational status in the United States, and socioeconomic status (Padilla and Salgado de Snyder 1992; Rodriguez-Andrew 1998). According to Ennis et al. (2011), of Latinos currently living in the United States (excluding Puerto Rico and other territories), Mexican Americans are the largest group (63 percent), followed by Central and South Americans (13.4 percent), Puerto Ricans (9.2 percent), and Cubans (3.5 percent).
Beliefs About and Traditions Involving Substance Use
Attitudes toward substance use vary among Latino cultural groups, but Latinos are more likely to see substance use in negative terms than are White Americans. Marin (1998) found that Mexican Americans were significantly more likely to expect negative consequences and less likely to expect positive outcomes as a result of drinking than were White Americans. Similarly, Hadjicostandi and Cheurprakobkit (2002) note that most Latinos believe that prescription drug abuse could have dangerous effects (85.7 percent), that individuals who abuse substances cause their whole families to suffer (81.4 percent), and that people who use illicit drugs will participate in violent crime (74.9 percent) and act violently toward family members (78.9 percent). Driving under the influence of alcohol is one of the most serious substance use problems in the Latino community.
Other research suggests that some Latinos hold different alcohol expectancies. When comparing drinking patterns and alcohol expectancies among college students, Velez-Blasini (1997) found that Puerto Rican participants were more likely than other students to see increased sociability as a positive expectancy related to drinking and sexual impairment as a negative expectancy. Puerto Rican participants were also significantly more likely to report abstinence from alcohol. In another study comparing Puerto Ricans and Irish Americans, Puerto Rican participants who expected a loss of control when drinking had fewer alcohol-related problems, whereas Irish Americans who expected a loss of control had a greater number of such problems (Johnson and Glassman 1999). The authors concluded that “losing control” has a different cultural meaning for these two groups, which in turn affects how they use alcohol.
For many Latino men, drinking alcohol is a part of social occasions and celebrations. By contrast, solitary drinking is discouraged and seen as deviant. Social norms for Latinas are often quite different, and those who have substance abuse problems are judged much more harshly than men. Women can be perceived as promiscuous or delinquent in meeting their family duties because of their substance use (Hernandez 2000). Amaro and Aguiar (1995) note that the heavy emphasis on the idealization of motherhood contributes to the level of denial about the prevalence of substance use among Latinas. Women who use injection drugs feel the need to maintain their roles as daughters, mothers, partners, and community members by separating their drug use from the rest of their lives (Andrade and Estrada 2003), yet research suggests that substance abuse among women does not go unrecognized within the Latino community (Hadjicostandi and Cheurprakobkit 2002).
Among families, Latino adults generally show strong disapproval of alcohol use in adolescents of either gender (Flores-Ortiz 1994). Adults of both genders generally disapprove of the initiation of alcohol use for youth 16 years of age and under (Rodriguez-Andrew 1998). Long (1990) also found that even among Latino families in which there has been multi-generational drug abuse, young people were rarely initiated into drug abuse by family members. However, evidence regarding parental substance use and its influence on youth has been mixed; most studies show some correlation between parental attitudes toward alcohol use and youth drinking (Rodriguez-Andrew 1998). For instance, research with college students found that family influences had a significant effect on drinking in Latinos but not White Americans; the magnitude of this effect was greater for Latinas than for Latino men (Corbin et al. 2008).
Substance Use and Substance Use Disorders
According to 2012 NSDUH data, rates of past-month illicit substance use, heavy drinking, and binge drinking among Latinos were lower than for White Americans, Blacks, and Native Americans, but not significantly so (SAMHSA 2013d). The same data showed that 8.3 percent of Latinos reported past-month illicit drug use compared with 9.2 percent of White Americans and 11.3 percent of African Americans.
Although data are available from a number of studies regarding Latino drinking and drug use patterns, more targeted research efforts are needed to unravel the complexities of substance use and the many factors that affect use, abuse, and dependence among subgroups of Latino origin (Rodriguez-Andrew 1998). For example, some studies show that Latino men are more likely to have an alcohol use disorder than are White American men (Caetano 2003), whereas others have found the reverse to be true (Schmidt et al. 2007). Disparities in survey results may reflect varying efforts to develop culturally responsive criteria (Carle 2009; Hasin et al. 2007). The table in Exhibit 5-2 shows lifetime prevalence of substance use disorders among Latinos based on immigration status and ethnic subgroup (Alegria et al. 2008a).
Exhibit 5-2
Lifetime Prevalence of Substance Use Disorders According to Ethnic Subgroup and Immigration Status.
Among diverse Latino cultural groups, different patterns of alcohol use exist. For example, some older research suggests that Mexican American men are more likely to engage in binge drinking (having five or more drinks at one time; drinking less frequently, but in higher quantities) than other Latinos but use alcohol less frequently (Caetano and Clark 1998). There are also differences regarding the abuse of other substances. Among Latinos entering substance abuse treatment in 2006, heroin and methamphetamine use were especially high among Puerto Ricans and Mexican Americans, respectively. Other research has found that Puerto Ricans are more likely to inject drugs and tend to inject more often during the course of a day than do other Latinos (Singer 1999).
Patterns of substance use are also linked to gender, age, socioeconomic status, and acculturation in complex ways (Castro et al. 1999a; Wahl and Eitle 2010). For instance, increased frequency of drinking is associated with greater acculturation for Latino men and women, yet the drinking patterns of Latinas are affected significantly more than those of Latino men (Markides et al. 2012; Zemore 2005).
Age appears to influence Latino drinking patterns somewhat differently than it does for other racial/ethnic groups. Research indicates that White Americans often “age out” of heavy drinking after frequent and heavy alcohol use in their 20s, but for many Latinos, drinking peaks between the ages 30 and 39. Latinos in this age range have the lowest abstention rates and the highest proportions of frequent and heavy drinkers of any age group (Caetano and Clark 1998). In the same study, Latino men between 40 and 60 years of age had higher rates of substance use disorders than men in the same age group across other racial/ethnic populations.
Latino youth appear to start using illicit drugs at an earlier age than do members of other major ethnic/racial groups. Cumulative data from 28 years of the Monitoring the Future Study show Latino eighth graders as having higher rates of heavy drinking, marijuana use, cocaine use, and heroin use than African or White Americans in the same grade. Among youth in grade 12, the rates of use among Latino and White American students are more similar, but Latinos still had the highest rates of crack cocaine and injected heroin use (Johnston et al. 2003).
Patterns of substance use and abuse vary based on Latinos' specific cultural backgrounds. Among Latinos, rates of past-year alcohol dependence were higher among Puerto Rican and Mexican American men (15.3 percent and 15.1 percent, respectively) than among South/Central American or Cuban American men (9 percent and 5.3 percent, respectively). Among Latinas, past-year alcohol dependence rates were significantly higher for Puerto Rican women (6.4 percent) than for Mexican American (2.1 percent), Cuban American (1.6 percent), or South/Central American (0.8 percent) women (Caetano et al. 2008).
Mental and Co-Occurring Disorders
As with other populations, it is important to address CODs in Latino clients, as CODs have been associated with higher rates of treatment dropout (Amodeo et al. 2008). There are also reports of diagnostic bias, suggesting that some disorders are underreported and others are overreported. Minsky et al. (2003) found that, at one large mental health treatment site in New Jersey, major depression was overdiagnosed among Latinos, especially Latinas, whereas psychotic symptoms were sometimes ignored. Among Latinos with CODs, other mental disorders preceded the development of a substance use disorder 70 percent of the time (Vega et al. 2009).
Overall, research indicates fewer mental disorders and CODs among Latinos than among White Americans (Alegria et al. 2008a; Vega et al. 2009). However, data from the 2012 NSDUH indicate that the magnitude of the difference may be decreasing; 1.2 percent of Latinos had both serious mental illness and substance use disorders in the prior year, as did White Americans, similar to the rate seen among African Americans (0.9 percent; SAMHSA 2013c). When any mental disorder symptoms co-occurring with a substance use disorder diagnosis were evaluated, Latinos had a slightly higher rate of co-occurrence (3.4 percent) than did African Americans (3.3 percent; SAMHSA 2013c). Rates of mental disorders and CODs also vary by Latino subgroup (Alegria et al. 2008a), and acculturation can play a confounding, but inconsistent, role in the identification and development of CODs in Latino populations (Alegria et al. 2008a; Vega et al. 2009).
Treatment Patterns
Barriers to treatment entry for Latinos include, but are not limited to, lack of Spanish-speaking service providers, limited English proficiency, financial constraints, lack of culturally responsive services, fears about immigration status and losing custody of children while in treatment, negative attitudes toward providers, and discrimination (Alegria et al. 2012; Mora 2002). Among all ethnic/racial groups included in the 2010 NSDUH, Latinos were the most likely to report that they had a need for treatment but did not receive it because they could not find a program with the appropriate type of treatment or because there were no openings in programs that they wished to attend, which may reflect a lack of linguistically and/or culturally appropriate services (SAMHSA 2011c). They were about twice as likely to state the former and four times as likely to state the latter as members of the group that was the next most likely to make such statements.
A significant problem prohibiting participation in substance abuse treatment among Latinos is the lack of insurance coverage to pay for treatment. In SAMHSA's 2010 NSDUH, 32 percent of Latinos who needed but did not receive substance abuse treatment in the past year reported that they lacked money or insurance coverage to pay for it compared with 29.5 percent of White Americans and 33.5 percent of African Americans (SAMHSA 2011c). Other national surveys also found that Latinos with self-identified drinking problems were significantly more likely than either White Americans or African Americans to indicate that they did not seek treatment because of logistical barriers, such as a lack of funds or being unable to obtain childcare (Schmidt et al. 2007).
Latinos with substance use disorders are about as likely to enter substance abuse treatment programs as White Americans (Hser et al. 1998; Perron et al. 2009; Schmidt et al. 2006). Latinos tend to enter treatment at a younger age than either African Americans or White Americans (Marsh et al. 2009). There are also significant differences in treatment-seeking patterns among Latino cultural groups. For example, Puerto Ricans who inject heroin are much more likely to participate in methadone maintenance and less likely to enter other less-effective detoxification programs than are Dominicans, Central Americans, and other Latinos (Reynoso-Vallejo et al. 2008). The researchers note, however, that this could be due partially to the fact that Puerto Ricans, compared with other Latinos, have a greater awareness of treatment options.
Beliefs and Attitudes About Treatment
In general, Latino attitudes toward health care are shaped by a lack of access to regular quality care, including inability to afford it (see review of health beliefs and help-seeking behaviors among Mexican Americans and Mexicans dwelling in the United States in Rogers 2010). DeNavas-Walt et al. (2006) found that Latinos are less likely to have health insurance (32.7 percent were uninsured in 2005) than either non-Latino White Americans (11.3 percent were uninsured) or African Americans (19.6 percent were uninsured). They are also less likely to have had a regular place to go for conventional medical care (Schiller et al. 2005). Lack of knowledge about available services can be a major obstacle to seeking services (Vega et al. 2001). In their review, Murguia et al. (2000) identified several factors that influence the use of medical services, including cultural health beliefs, demographic barriers, level of acculturation, English proficiency, accessibility of service providers, and flexibility of intake procedures; they found that many Latinos only seek medical care for serious illnesses.
Research on substance abuse indicates that Latinos who use illicit drugs appear to have relatively unfavorable attitudes toward treatment and perceive less need for treatment than do illicit drug users among every other major ethnic and racial group but Native Americans (Brower and Carey 2003). However, in the 2011 NSDUH, Latinos were more likely than White Americans, African Americans, or Asian Americans to indicate that they had a need for substance abuse treatment in the prior year but did not receive it (SAMHSA 2012b). Other studies have found that Latinos with substance use disorders are about as likely to enter substance abuse treatment programs as other racial and ethnic groups (Hser et al. 1998; Perron et al. 2009; Schmidt et al. 2006). Latinos who receive substance abuse treatment also report less satisfaction with the services they receive than White or African Americans (Wells et al. 2001). Even when receiving a level of substance abuse treatment services comparable to those received by White and African Americans, Latinos are more likely to be dissatisfied with treatment (Tonigan 2003).
Treatment Issues and Considerations
Latino clients' responsiveness to therapy is influenced not only by counselor and program characteristics, but also by individual characteristics, including worldview, degree of acculturation, gender orientation, religious beliefs, and personality traits. As with other cultural groups, efforts to establish clear communication and a strong therapeutic alliance are essential to positive treatment outcomes among Latino clients. Foremost, counselors should recognize the importance of—and integrate into their counseling style and approach—expressions of concern, interest in clients' families, and personal warmth (personalismo; Ishikawa et al. 2010).
Counselors and clinical supervisors need to be educated about culturally specific attributes that can influence participation and clinical interpretation of client behavior in treatment. For instance, some Latino cultural groups view time as more flexible and less structured; thus, rather than negatively interpreting the client's behavior regarding the keeping of strict schedules or appointment times, counselors should adopt scheduling strategies that provide more flexibility (Alvarez and Ruiz 2001; Sue 2001). However, counselors should also advise Latino clients of the need to take relevant actions with the aim of arriving on time for each appointment or group session. Counselors should try to avoid framing noncompliance in Latino clients as resistance or anger. It is often, instead, a pelea nonga (relaxed fight) showing both a sense of being misunderstood and respeto (respect that also encompasses a sense of duty) for the counselor's authority (Barón 2000; Medina 2001).
Unfortunately, many providers who work with Latino cultural groups continue to have misperceptions and can even see culture as a hindrance to effective treatment rather than as a source of potential strength (Quintero et al. 2007). For instance, in treating the alcohol problems of Latinas, many counselors believe that they should not incorporate endorsement of traditional and possibly harmful cultural patterns into the services they provide (Mora 2002). However, other counselors note that the transformative value of the most positive aspects of Latino cultural groups can be emphasized: strength, perseverance, flexibility, and an ability to survive (Gloria and Peregoy 1996). Respecting women's choices can mean supporting empowerment to pursue new roles and make new choices free of alcohol, guilt, and discrimination (Mora 2002). For others, it can mean reinvigorating the positivity of Latina culture to promote abstinence while respecting and maintaining traditional family roles for women (Gloria and Peregoy 1996).
Because some research has found that Latinos have higher rates of treatment dropout than other populations (Amaro et al. 2006), programs working with this population should consider ways to improve retention and outcomes. Treatment retention issues for Latinos can be similar to those found for other populations (Amodeo et al. 2008), but culturally specific treatment has been associated with better retention for Latinos (Hohman and Galt 2001). Research evaluating ethnic matching with brief motivational interventions also found more favorable substance abuse treatment outcomes at 12-month follow-up when clients and providers were ethnically matched (Field and Caetano 2010). Available literature and research highlight four main themes surrounding general counseling issues and programmatic strategies for Latinos, as follows.
Socializing the client to treatment: Latino clients are likely to benefit from orientation sessions that review treatment and counseling processes, treatment goals and expectations, and other components of services (Organista 2006).
Reassurance of confidentiality: Regardless of the particular mode of therapy, counselors should explain confidentiality. Many Latinos, especially undocumented workers or recent immigrants, are fearful of being discovered by authorities like the United States Citizenship and Immigration Services and subsequently deported back to their countries of origin (Ramos-Sanchez 2009).
Client–counselor matching based on gender: To date, research does not provide consistent findings on client–counselor matching based on similarity of Latino ethnicity. However, client–counselor matching based on gender alone appears to have a greater effect on improving engagement and abstinence among Latinos than it does for clients of other ethnicities (Fiorentine and Hillhouse 1999).
Client–program matching: Matching clients to ethnicity-specific programs appears to improve outcomes for Latinos. Takeuchi et al. (1995) found that only 68 percent of Mexican American clients in programs that had a majority of White American clients returned after the first session compared with 97 percent in those programs where the majority of clients were Mexican American.
Theoretical Approaches and Treatment Interventions
Overall, research evaluating cultural adoption of promising or evidence-based practices in treatment specifically for Latinos is scarce (Carvajal and Young 2009). For instance, empirical literature evaluating CBT specifically for substance abuse and substance use disorders in Latinos is quite limited. Still, a number of authors recommend CBT for Latinos in mental health and substance abuse treatment settings because it is action oriented, problem focused, and didactic (Alvarez and Ruiz 2001; Organista 2006; Organista and Muñoz 1998). CBT's didactic component can educate Latinos about disorders and frame therapy as an educational (and hence less shameful) experience. However, Organista's (2006) review of available research on CBT for mental disorders among Latinos suggests that this approach is not always as effective with Latinos as it is with other populations.
Other effective interventions include contingency management and motivational interviewing; see the review by Amaro et al. (2006) for more on these interventions. Methadone maintenance, too, has been associated with long-term reductions in the use of alcohol as well as heroin and other illicit drugs among Mexican Americans with opioid use disorders, although 33 percent of the original cohort died before the 22-year longitudinal study concluded (Goldstein and Herrera 1995). Another therapeutic intervention that can improve outcomes for Latino clients is node-link mapping (visual representation using information diagrams, fill-in-the blank graphic tools, and client-generated diagrams or visual maps), which has been associated with lower levels of opioid and cocaine use, better treatment attendance, and higher counselor ratings of motivation and confidence for Latinos in methadone maintenance treatment (Dansereau et al. 1996; Dansereau and Simpson 2009). For a review of Latino outcome studies in health, substance abuse, and mental health in social work, refer to Jani and colleagues (2009).
Family therapy
Family therapy is often recommended for treating Latinos with substance use disorders (Amaro et al. 2006; Barón 2000; Hernandez 2000). Although there is little research evaluating the effectiveness of family therapy for adults, both multidimensional family therapy (Liddle 2010) and brief strategic family therapy (Santisteban et al. 1997; Santisteban et al. 2003; Szapocznik and Williams 2000) have been found to reduce substance use and improve psychological functioning among Latino youth. The term familismo refers to the centrality of the family in Latino culture and can include valuing and protecting children, respecting the elderly, preserving the family name, and consulting with one another before making important decisions. As highlighted in the case study of a Puerto Rican client on the next page, counselors must consider the potentially pivotal roles families can play in supporting treatment and recovery. Latino families are likely to have a strong sense of obligation and commitment to helping their members, including those who have substance use disorders. Even so, the level of family support for people who have substance use or mental disorders varies among Latinos depending on country of origin, level of acculturation, degree of family cohesion, socioeconomic status, and factors related to substance use (Alegria et al. 2012). For example, Reynoso-Vallejo et al. (2008) concluded that significantly higher rates of homelessness found among people from Central American countries who injected heroin compared with other Latinos could stem from lower levels of tolerance for injection drug use among their families.
For counselors who lack cultural understanding, it can be easy to simply label and judge families' behavior as enabling or codependent. Instead, counselors should move away from labeling the behavior and focus more on helping families recognize how their behavior can affect one member's substance abuse and how best to handle it. The advice box on the next page provides general therapeutic guidelines for working with Latino families.
Case Study: A Puerto Rican Client
Anna is a 27-year-old woman who was born in New York and self-identifies as Puerto Rican. She has a 12th-grade education, is unemployed, and lives with her parents, her 4-year-old daughter, and a nephew. Anna is separated from her partner, who is also her daughter's father. She entered treatment as a result of feeling depressed ever since her partner physically assaulted her because she refused to use heroin (the event that sparked their separation). She states, “I want to be clean and take care of my family.” At intake, she had just undergone detoxification and had stopped using alcohol, crack cocaine, and heroin.
Anna states that she feels guilty about her drug use and the way it caused her to neglect her family. She has been having serious problems with her mother, who is critical of her substance use, but believes that her mother is important in her recovery because of the structure she provides at home. She describes her father as a very important figure with whom she enjoys spending time. Her father had stopped drinking 9 years before and is very supportive of her abstinence. He is willing to help in any way he can but has been very sick lately and was diagnosed with prostate cancer. Her father had never received treatment for his drinking problem, and her mother believes that Anna should be able to stop just like her father did. As she describes her situation in treatment, Anna's vergüenza (shame) and sense of hopelessness is very evident. She fears her father's death and her mother's subsequent rejection of her for not helping out.
Anna's treatment includes family therapy to restructure communication patterns, rules, expectations, and roles. For family sessions, either her mother or both parents participate, depending on her father's physical condition. Initially, her parents displayed a tendency to focus on the problems of the past, but the counselor directed them to focus on changes needed to help Anna's recovery. The counselor has also worked with other family members to rally support and use their strengths while also clarifying perceptions, feelings, and behaviors that will help them function as a family unit. Anna's counselor recognizes that, within the context of her culture, her reliance on her family can be used to aid her recovery and that her family, as defined by Anna, can be used as a support system.
Source: Medina 2001. Adapted with permission.
Group therapy
Little information is available concerning Latinos' preferences in behavioral health services, but a study evaluating mental health treatment preferences for women in the United States found that Latinas were significantly more likely to prefer group treatment (Nadeem et al. 2008). According to Paniagua (1998), the use of group therapy with Latino clients should emphasize a problem-focused approach. Group leaders should allow members to learn from each other and resist functioning as a content expert or a representative of the rules of the system. Otherwise, members could see group therapy as oppressive. Facilitators in groups consisting mostly of Latino clients must establish trust, responsibility, and loyalty among members. In addition, acculturation levels and language preferences should be assessed when forming groups so that culturally specific or Spanish-speaking groups can be made available if needed.
Mutual-help groups
Findings on the usefulness of 12-Step groups for Latino clients are inconsistent. Membership surveys of AA indicate that Latinos comprise about 5 percent of AA membership (AAWS 2012). Latinos who received inpatient treatment were less likely to attend AA than White Americans (Arroyo et al. 1998). Rates of mutual-help participation among people with drug use disorders are also lower for Latinos (Perron et al. 2009). Language can present a barrier to mutual-help group participation for Spanish-speaking Latinos; however, Spanish-language meetings are held in some locations. Counselors should consider the appropriateness of 12-Step participation on a case-by-case basis (Alvarez and Ruiz 2001). For example, Mexican American men who identify with attitudes of machismo can feel uncomfortable with the 12-Step approach. Concern about divulging family issues in public can cause hesitation to address substance-related problems in public meetings.
Advice to Counselors: Family Therapy Guidelines for Latino Families
- Provide bilingual services.
- Use family therapy as a primary method of treatment.
- Assess cultural identity and acculturation level for each family member.
- Determine the family's level of belief in traditional and complementary healing practices; integrate these as appropriate.
- Discuss the family's beliefs, history, and experiences with standard American behavioral health services.
- Explore migration and immigration experiences, if appropriate.
- Provide additional respect to the father or father figure in the family.
- Interview family members or groups of family members (e.g., children) separately to allow them to voice concerns.
- Generate solutions with the family. Do not force changes in family relationships.
- Provide specific, concrete suggestions for change that can be quickly implemented.
- Focus on engaging the family in the first session using warmth and personalismo.
Sources: Bean et al. 2001; Hernandez 2005; Lynch and Hanson 2011.
For Latinos who do participate in 12-Step programs, findings suggest higher rates of abstinence, degree of commitment, and level of engagement than for White American participants (Hoffman 1994; Tonigan et al. 1998). For some Latinos, 12-Step groups can appeal to religious and spiritual beliefs. Hernandez (2000) suggests that mutual-help groups composed solely of Latinos make it easier for participants to address the cultural context of substance abuse. Some Latino 12-Step groups do not hold that substance abuse is a biopsychosocial problem, instead conceptualizing the disorder as a weakness of character that must be corrected. Hoffman (1994) studied Latino 12-Step groups in Los Angeles and observed that, in addition to a more traditional form of AA, there were groups that practiced terapia dura (i.e., rough therapy), which often uses a confrontational approach and endorses family values related to machismo (e.g., by reinforcing that overcoming substance abuse rather than drinking is manly). However, these groups were not overly welcoming of female members and gay men. In such cases, gay Latino men and Latinas can benefit from attending 12-Step groups that are not culturally specific or that do not use terapia dura.
Traditional healing and complementary methods
In a study of the use of alternative and complementary medical therapies, Latinos were less likely to use medical alternatives than were White Americans (Graham et al. 2005). However, those who did use such approaches were more likely to do so because they could not afford standard medical care (Alegria et al. 2012). As in other areas, the use of complementary and traditional medicine likely varies according to acculturation level and country of origin. For instance, the use of faith and religious practices to cope with mental and emotional problems is significantly more common among foreign-born Latinos than among those born in the United States (Nadeem et al. 2008; Vega et al. 2001).
Many Latinos place great importance on the practice of Roman Catholicism. Yamamoto and Acosta (1982) describe the central tenets of Latino Catholicism as sacrifice, charity, and forgiveness. These beliefs can hinder assertiveness in some Latinos, but they can also be a source of strength and recovery. Traditionally, Latinos have been Catholic, although several Protestant and evangelical groups have converted millions of Latinos to their religions since the 1970s. Some Latinos also believe in syncretistic religions (e.g., Santería or Curanderismo) or practices derived from them and make use of a variety of traditional healing practices and rituals to heal mental and spiritual ailments (Lefley et al. 1998; Sandoval 1979). Among Puerto Ricans, espiritismo (spiritualism) is a popular traditional healing system successfully used to address mental health issues (Lynch and Hanson 2011; Molina 2001). Some Mexican Americans rely on curanderos, folk healers who address problems that might be framed as psychological (Falicov 2005, 2012). For a review of culturally responsive interventions with Latinos, refer to Gallardo and Curry (2009).
Relapse prevention and recovery
There are no substantial studies evaluating the use of relapse prevention and recovery promotion with Latinos, yet literature suggests that they would be appropriate and effective for this population (Blume et al. 2005; Castro et al. 2007). Overall, Latinos can face somewhat different triggers for relapse relating to acculturative stress or the need to uphold particular cultural values (e.g., personalismo, machismo; Castro et al. 2007), which can lead to higher rates of relapse among some Latino clients. For example, in a study of relapse patterns among White American and Latino individuals who used methamphetamine, Brecht et al. (2000) found that Latino participants relapsed more quickly than White American participants.
Data are lacking on long-term recovery for Latinos. Given the many obstacles that block accessibility to treatment for Latinos, continuing care planning can benefit from greater use of informal or peer supports. For example, White and Sanders (2004) recommend the use of a recovery management approach with Latinos. They point to an early example of the East Harlem Protestant Parish's work, which helped Puerto Rican individuals recovering from heroin dependence connect to social clubs and religious communities that supported recovery. Latinos use community and family support in addition to spirituality to address mental disorders (Lynch and Hanson 2011; Molina 2001). Castro et al. (2007) also note that family support systems can be especially important for Latinos in recovery.
Counseling for Native Americans
There are 566 federally recognized American Indian Tribes, and their members speak more than 150 languages (U.S. Department of the Interior, Indian Affairs 2013a); there are numerous other Tribes recognized only by states and others that still go unrecognized by government agencies of any sort. According to the 2010 U.S. Census (Norris et al. 2012), the majority (78 percent) of people who identified as American Indian or Alaska Native, either alone or in combination with one or more other races, lived outside of American Indian and Alaska Native areas. Approximately 60 percent of the 5.2 million people who identified as American Indian or Alaska Native, alone or in combination with one or more other races, reside in urban areas (Norris et al. 2012). The category of Alaska Natives includes four recognized Tribal groups—Alaskan Athabascan, Aleut, Eskimo, and Tingit-Haida—along with many other independent communities (Ogunwole 2006).
Native Americans who belong to federally recognized Tribes and communities are members of sovereign Indian nations that exist within the United States. On lands belonging to these Tribes and communities, Native Americans are able to govern themselves to a large extent and are not subject to most state laws—only to federal legislation that is specifically designated as applying to them (Henson 2008). Although health care (including substance abuse treatment) is provided to many Native Americans by Indian Health Services (IHS), Tribal governments do have the option of taking over those services. Counselors working with these populations should remember that Native Americans, by virtue of their membership in sovereign Tribal entities, have rights that are different from those of other Americans; this distinguishes them from members of other ethnic/racial groups.
American Indians live in all 50 states; the states with the largest populations of American Indians are Oklahoma, California, and Arizona. The 2000 Census allowed people to identify, for the first time, as a member of more than one race. Of persons who checked two or more races, nearly one in five indicated that they were part American Indian or Alaska Native (U.S. Census Bureau 2001a,b).
Behavioral health service providers should recognize that Native American Tribes represent a wide variety of cultural groups that differ from one another in many ways (Duran et al. 2007). Alaska Natives who live in coastal areas have very different customs from those inhabiting interior areas (Attneave 1982). The diversity of Native American Tribes notwithstanding, they also share a common bond of respect for their cultural heritages, histories, and spiritual beliefs, which are different from those of mainstream American culture. For more information on the treatment and prevention of substance abuse and mental illness among Native Americans, see the planned TIP, Behavioral Health Services for American Indians and Alaska Natives (SAMHSA planned a).
Beliefs About and Traditions Involving Substance Use
Few American Indian Tribes and no Alaska Natives consumed alcoholic beverages prior to contact with non-Native people, and those who did used alcohol primarily for special occasions and ceremonies. Most Tribes first encountered the use of alcohol when they encountered European settlers and traders. Because of this lack of experience with alcohol, few Native Americans had a context for drinking besides what they learned from these non-Natives, who at the time drank in large quantities and often engaged in binge drinking. Although patterns of alcohol consumption in the mainstream population of the United States changed over time, they remained relatively the same in the more isolated Native American communities. According to an NSDUH report on American Indian and Alaska Native adults, binge drinking continues to be a significant problem for these populations. Both binge drinking and illicit drug use is higher among Native Americans than the national average (30.2 percent versus 23 percent and 12.7 percent versus 9.2 percent, respectively; SAMHSA 2013d).
American Indian drinking patterns vary a great deal by Tribe. Tribal attitudes toward alcohol influence consumption in complicated ways. For example, in Navajo communities, excessive drinking was acceptable if done in a group or during a social activity. However, solitary drinking (even in lesser amounts) was considered to be deviant (Kunitz et al. 1994). Kunitz et al. (1994) observed that during the 1960s, binge drinking was acceptable among the Navajo during public celebrations, whereas any drinking was considered unacceptable among the neighboring Hopi population, wherein regular drinkers were shunned or, in some cases, expelled from the community. Hopi individuals who did drink tended to do so alone or moved off the reservation to border towns where heavy alcohol use was common. The ostracism of Hopi drinkers seemed to lead to even greater levels of abuse, given that there were much higher death rates from alcoholic cirrhosis among the Hopi than among the Navajo.
Native American recovery movements have often viewed substance abuse as a result of cultural conflict between Native and Western cultures, seeing substances of abuse as weapons that have caused further loss of traditions (Coyhis and White 2006). To best treat this population, substance abuse treatment providers need to expand their perspectives regarding substance abuse and dependence and must embrace a broader view that explores the spiritual, cultural, and social ramifications of substance abuse (Brady 1995; Duran 2006; Jilek 1994).
Substance Use and Substance Use Disorders
According to 2012 NSDUH data, American Indian and Alaska Native peoples have the highest rates of substance use disorders and binge drinking (SAMHSA 2013d). Although rates of substance abuse are high among Native Americans, so too are rates of abstinence. American Indians and Alaska Natives are more likely to report no alcohol use in the past year than are members of all other major racial and ethnic groups (OAS 2007). The American Indian Services Utilization and Psychiatric Epidemiology Risk and Protective Factors Project (AI-SUPER PFP) also found that rates of lifetime abstinence from alcohol for American Indians in the study were significantly higher than lifetime abstinence rates among the general population (Beals et al. 2003). Data on alcohol consumption also show that Alaska Natives are significantly more likely to abstain than are other Alaskans (Wells 2004).
The most common pattern of abusive drinking among American Indians appears to be binge drinking followed by long periods of abstinence (French 2000; May and Gossage 2001). A similar pattern is seen among Alaska Natives (Seale et al. 2006; Wells 2004). As an example, the Urban Indian Health Institute (2008) found that binge drinking was significantly more common among the Native American population (with 21.3 percent engaging in binge drinking in the prior 30 days compared with 15.8 percent of non-Native Americans) and that, among those who drank, 40.7 percent of Native American participants engaged in binge drinking compared with 26.9 percent of non-Natives.
There are a number of historical reasons for the development of binge drinking among Native Americans. The existence of dry reservations (which can limit the times when individuals are able to get alcohol), high levels of poverty, lack of availability (e.g., in remote Alaska Native villages), a history of trauma, and the loss of cultural traditions can all contribute to the development and continuation of this pattern of drinking. Native Americans are also more likely than members of other major racial/ethnic groups to have had their first drink before the age of 21 or before the age of 16, which also may shape drinking patterns (SAMHSA 2011c).
However, data on heavy and binge drinking do not reflect the same pattern of alcohol consumption for all Native American Tribes. One analysis of alcohol dependence among members of seven different Tribes found rates of dependence varying from 56 percent of men and 30 percent of women in one Tribe to 1 percent of men and 2 percent of women in another (Koss et al. 2003). Other research confirms significant differences in alcohol use among diverse Native American communities (O'Connell et al. 2005; Whitesell et al. 2006).
In addition to alcohol, methamphetamine and inhalant abuse are major concerns for a number of Native American communities. Nonetheless, there are considerable regional differences in patterns and prevalence of drug use (Miller et al. 2012). According to the National Congress of American Indians (2006), 74 percent of Tribal police forces ranked methamphetamine as the drug causing the most problems in their communities. Methamphetamine abuse can be even more serious for Native Americans living in rural areas than for those in urban areas, but it is also a serious problem for growing numbers of American Indians, especially women, entering treatment in urban areas (Spear et al. 2007).
American Indians and Alaska Natives are more likely to report having used inhalants at some time during their lives, but use tends to peak in 8th grade and then decrease (Miller et al. 2012). In some Native American communities (e.g., on the Kickapoo reservation in Texas), inhalants have been a major drug of abuse for adults as well as youth. During the early 1990s, about 46 percent of the adult population on that reservation were thought to abuse inhalants (Fredlund 1994). Although more recent data are not available, reports from the area suggest that inhalant abuse remains a significant problem (Morning Star 2005).
Rates of substance use disorders appear to be higher in individuals who consider themselves exclusively Native American than for those who identify as more than one race/ethnicity, but even when surveys ask whether people are of mixed race, those who report themselves to be partially Native American still have high rates of substance use disorders (OAS 2007). Native Americans are about 1.4 times more likely than White Americans to have a lifetime diagnosis of an alcohol use disorder (Gilman et al. 2008). Illicit drug use is also more common for Native Americans than for members of other major racial/ethnic groups.
Among Native Americans entering treatment in 2010, alcohol use disorders alone or in conjunction with drug use disorders were the most pressing substance-related problem, with cannabis and opioids other than heroin being the next most common primary substances of abuse. One of the largest studies on American Indian substance use and abuse to date, the AI-SUPER PFP, found that 31.2 percent of American Indians met criteria for a lifetime diagnosis of a substance use disorder, and 13.4 percent met criteria for a past-year diagnosis (Beals et al. 2003). The study found that rates of alcohol use disorders were high among men from the three Tribes represented but varied to a greater degree among women across Tribes (Mitchell et al. 2003).
American Indians have high rates of certain diseases and conditions. In particular, the incidence of diabetes is increasing among Native Americans, and approximately 38 percent of elder Native Americans have diabetes (Moulton et al 2005). Diabetes is also associated with both substance use disorders and depression in this population (Tann et al. 2007). Other health problems associated with alcohol use include fetal alcohol syndrome, cirrhosis, and depression.
Mental and Co-Occurring Disorders
According to the 2012 NSDUH, 28.3 percent of American Indians and Alaska Natives report having a mental illness, with approximately 8.5 percent indicating serious mental illness in the past year (SAMHSA 2013c). Native Americans were nearly twice as likely to have serious thoughts of suicide as members of other racial/ethnic populations, and more than 10 percent reported a major depressive episode in the past year. Common disorders include depression, anxiety, and substance use.
As with other groups, substance use disorders among Native Americans have been associated with increased rates of a variety of different mental disorders (Beals et al. 2002; Tann et al. 2007; Westermeyer 2001). The 2012 NSDUH revealed that 14 percent of Native Americans reported both past-year substance use disorders and mental illness. Among those who reported mental illness, nearly 5 percent reported several mental illnesses co-occurring with substance use disorders (SAMHSA 2013c).
Native American communities have experienced severe historical trauma and discrimination (Brave Heart and DeBruyn 1998; Burgess et al. 2008). Studies suggest that many Native Americans suffer from elevated exposure to specific traumas (Beals et al. 2005; Ehlers et al. 2006; Manson 1996; Manson et al. 2005), and they may be more likely to develop PTSD as a result of this exposure than members of other ethnic/racial groups. PTSD comparison rates taken from the AI-SUPER PFP study and the National Comorbidity Study show that 12.8 percent of the Southwest Tribe sample and 11.5 percent of the Northern Plains Tribe sample met criteria for a lifetime diagnosis of PTSD compared with 4.3 percent of the general population (Beals et al. 2005). Trauma histories and PTSD are so prevalent among Native Americans in substance abuse treatment that Edwards (2003) recommends that assessment and treatment of trauma should be a standard procedure for behavioral health programs serving this population. For example, Native American veterans with substance use disorders are significantly more likely to have co-occurring PTSD than the general population of veterans with substance use disorders (Friedman et al. 1997).
Treatment Patterns
Despite a number of potential barriers to treatment (Venner et al. 2012), Native Americans are about as likely as members of other racial/ethnic groups to enter behavioral health programs. According to data from the 2003 and 2011 NSDUH (SAMHSA, CBHSQ 2012), Native Americans were more likely to have received substance use treatment in the past year than persons from other racial/ethnic groups (15.0 percent versus 10.2 percent). Other studies indicate that about one-third of Native Americans with a current substance use disorder had received treatment in the prior year (Beals et al. 2006; Herman-Stahl and Chong 2002). The 2012 NSDUH reported that approximately 15 percent of Native Americans received mental health treatment (SAMHSA 2013c).
Native Americans were least likely of all major ethnic/racial groups to state that they could not find the type of program they needed and were the next least likely after Native Hawaiians and other Pacific Islanders to state that they did not know where to go or that their insurance did not cover needed treatment. Among Native Americans who identified a need for treatment in the prior year but did not enter treatment, the most commonly cited reasons for not attending were lack of transportation, lack of time, and concerns about what one's neighbors might think (SAMHSA 2011c).
Many Native Americans, especially those residing on reservations or other Tribal lands, seek mental health and substance abuse treatment through Tribal service providers or IHS (Jones-Saumty 2002; McFarland et al. 2006). However, an analysis using multiple sources found that 67 percent of Native Americans entering substance abuse treatment over the course of a year did so in urban areas, and the majority of those urban-based programs were not operated by IHS (McFarland et al. 2006). The same research also found that Native Americans were somewhat more likely than the general treatment-seeking population to enter residential programs.
Native Americans were more likely to enter treatment as a result of criminal justice referrals than were White Americans or African Americans: 47.9 percent of American Indians and Alaska Natives entering public treatment programs in 2010 were court-ordered to treatment compared with 36.6 percent of White Americans and 36.4 percent of African Americans (SAMHSA, CBHSQ 2012). The lack of recognition of special needs and knowledge of Native American cultures within behavioral health programs may be the main reasons for low treatment retention and underuse of help-seeking behaviors among Native Americans (LaFromboise 1993; Sue and Sue 2013e).
Beliefs and Attitudes About Treatment
Duran et al. (2005) evaluated obstacles to treatment entry among American Indians on three different reservations; most frequently mentioned were the perception that good-quality or suitable services were unavailable and the perceived need for individuals to be self-reliant. They also found social relationships to be extremely important in overcoming these barriers. Jumper-Thurman and Plested (1998) reported that focus groups of American Indian women listed mistrust as one of the primary barriers for seeking treatment. This is due, in part, to the women's belief that they would encounter people they knew among treatment agency staff; they also doubted the confidentiality of the treatment program.
Treatment Issues and Considerations
Each Tribe and community will likely have different customs, healing traditions, and beliefs about treatment providers that can influence not only willingness to participate in treatment services, but also the level of trust clients have for providers. Counselors and other behavioral health workers must develop ongoing relationships within local Native American communities to gain knowledge of the unique attributes of each community, to show investment in the community, and to learn about community resources (Exhibit 5-3). Identifying and developing resources within Native communities can help promote culturally congruent relationships.
Exhibit 5-3
Native Americans and Community.
To provide culturally responsive treatment, providers need to understand the Native American client's Tribe; its history, traditions, worldview, and beliefs; the dimensions of its substance abuse problem and other community problems; the incidence of trauma and abuse among its members; its traditional healing practices; and its intrinsic strengths. Providers who work with Native Americans but do not have an understanding of their cultural identity and acculturation patterns are at a distinct disadvantage (Ponterotto et al. 2000). Before beginning any treatment, providers should routinely seek consultation with knowledgeable professionals who are experienced in working with the specific Tribal group in question (Duran 2006; Edwards and Egbert-Edwards 1998; Straits et al. 2012) and should conduct thorough client assessments that evaluate cultural identity (see Appendix F and Chapter 2 for resources). Some Native American persons have a strong connection to their cultures and others do not; some identify with a blend of American Indian cultural groups called pan-Indianism or inter-Tribal identity. Still others are comfortable with a dual identity that embraces both Native and non-Native cultural groups.
Native Americans often approach the beginning of a relationship in a calm, unhurried manner, and they may need more time to develop trust with providers. Concerns about confidentiality can be an important issue to address with Native American clients, especially for those in small, tightly-knit communities. For providers, it is very important to make clear to clients that what they say to the counselor will be held in confidence, except when there is an ethical duty to report.
Native American cultural groups generally believe that health is nurtured through balance and living in harmony with nature and the community (Duran 2006; Garrett et al. 2012). They also, for the most part, have a holistic view of health that incorporates physical, emotional, and spiritual elements (Calabrese 2008), individual and community healing (Duran 2006; McDonald and Gonzalez 2006), and prevention and treatment activities (Johnston 2002). For many, culture is the path to prevention and treatment.
However, not all Native Americans have a need to develop stronger connections to their communities and cultural groups. As Brady (1995) cautions, culture is complex and changing, and a return to the values of a traditional culture is not always desired. An initial inquiry into each client's connection with his or her culture, cultural identity, and desire to incorporate cultural beliefs and practices into treatment is an essential step in culturally competent practice. When appropriate, providers can help facilitate the client's reconnection with his or her community and cultural values as an integral part of the treatment plan. In addition, treatment providers need to adapt services to be culturally responsive. In doing so, outcomes are likely to improve not only for Native American clients, but for all clients within the program. Fisher et al. (1996) modified a therapeutic community in Alaska to incorporate Alaska Native spiritual and cultural practices and found that retention rates improved for White and African American clients as well as Alaska Native clients participating in the program.
In working with Native American clients, providers should be prepared to address spirituality and to help clients access traditional healing practices. Culturally responsive treatment should involve community events, group activities, and the ability to participate in ceremonies to help clients achieve balance and find new insight (Calabrese 2008). Stronger attachment to Native American cultural groups protects against substance use and abuse; therefore, strengthening this connection is important in substance abuse treatment (Duran 2006; Moss et al. 2003; Spicer 2001; Stone et al. 2006).
Theoretical Approaches and Treatment Interventions
Some clinicians caution that a model of counseling that requires self-disclosure to relative strangers can be counterproductive with Native American clients. Other authors recommend CBT and social learning approaches for Native American clients, as such approaches typically have less cultural bias, focus on problem-solving and skill development, emphasize client strengths and empowerment, recognize the need to accept personal responsibility for change, and make use of learning styles that many Native Americans find culturally appropriate (Heilbron and Guttman 2000; McDonald and Gonzalez 2006). Motivational interviewing is also recommended for Native American clients. In a small study, Villanueva et al. (2007) found that all treatment modalities resulted in improvements at 15-month follow-up, but clients who received motivational enhancement therapy reported significantly fewer drinks per drinking day during the 10- to 15-month posttreatment follow-up period. Venner et al. (2006) wrote a manual for motivational interviewing with Native American clients.
Advice to Counselors: Counseling Native Americans
When working with Native American clients, providers should:
- Use active listening and reflective responses.
- Avoid interrupting the client.
- Refrain from asking about family or personal matters unrelated to substance abuse without first asking the client's permission to inquire about these areas.
- Avoid extensive note-taking or excessive questioning.
- Pay attention to the client's stories, experiences, dreams, and rituals and their relevance to the client.
- Recognize the importance of listening and focus on this skill during sessions.
- Accept extended periods of silence during sessions.
- Allow time during sessions for the client to process information.
- Greet the client with a gentle (rather than firm) handshake and show hospitality (e.g., by offering food and/or beverages).
- Give the client ample time to adjust to the setting at the beginning of each session.
- Keep promises.
- Offer suggestions instead of directions (preferably more than one to allow for client choice).
Sources: Aragon 2006; Trimble et al. 2012.
Family therapy
Family involvement in treatment leads to better outcomes for Native Americans at the time of discharge from treatment (Chong and Lopez 2005). Research also suggests that family and community support can have a significant effect on recovery from substance use disorders for this population (Jones-Saumty 2002; Paniagua 1998). Family therapy can be quite helpful and perhaps even essential for American Indian clients (Coyhis 2000), especially when other social supports are lacking (Jones-Saumty 2002).
American Indians place high value on family and extended family networks; restoring or healing family bonds can be therapeutic for clients with substance use disorders. Moreover, Native American clients are sometimes less motivated to engage in “talk therapy” and more willing to participate in therapeutic activities that involve social and family relationships (Joe and Malach 2011). Treatment approaches should remain flexible and include clients' families when appropriate. Counselors should be able to recognize what constitutes family, family constellations, and family characteristics. The Native American concept of family can include elders, others from the same clan, or individuals who are not biologically related. In many Tribes, all members are considered relatives. Families can be matrilineal (i.e., kinship is traced through the female line) and/or matrilocal (i.e., married couples live with wife's parents).
When families do enter treatment, they may initially prefer to focus on a concrete problem, but not necessarily on the most significant family issue. Discussion of a clearly defined presenting problem enables families to assess the therapeutic process and better understand what is expected of them in treatment. Providers should be aware that the entire clan and/or Tribe could know about a given client's treatment and progress. Family therapy models such as network therapy, which makes use of support structures outside the immediate family and which were originally developed for Native American families living in urban communities, can be particularly effective with Native clients, especially when they have been cut off from their home communities because of substance abuse or other issues. For more information on network therapy and similar approaches, see TIP 39, Substance Abuse Treatment and Family Therapy (CSAT 2004b).
Group therapy
Although researchers and providers once viewed group therapy as ineffective for American Indian clients (Paniagua 1998), opinion has shifted to recognize that, when appropriately structured, group therapy can be a powerful treatment component (Garrett 2004; Garrett et al. 2001; Trimble and Jumper-Thurman 2002). Garrett (2004) notes that many Native American Tribes have traditional healing practices that involve groups; for many of these cultural groups, healing needs to occur within the context of the group or community (e.g., in talking circles). Thus, if properly adapted, group therapy can be very beneficial and culturally congruent. It is important, however, to determine Native American clients' level of acculturation before recommending Western models of group therapy, as less acculturated Native clients are likely to be less comfortable with group talk therapy (Mail and Shelton 2002). Group therapy for Alaska Natives should also be nonconfrontational and focus on clients' strengths.
Group therapy can incorporate Native American traditions and rituals to make it more culturally suitable. For example, the talking circle is a Native tradition easily adapted for behavioral health treatment. In this tradition, the members of the group sit in a circle. An eagle feather, stone, or other symbolic item is passed around, and each person speaks when he or she is handed the item. Based on a review of the literature, Paniagua (1998) recommends that providers using group therapy with Native American clients:
- Earn support or permission from Tribal authorities before organizing group therapy.
- Consult with Native professionals.
- If group members consent, invite respected Tribal members (e.g., traditional healers or elders) to participate in sessions.
Mutual-help groups
Native American peoples have a long history of involvement in mutual-help activities that predates the 12-Step movement (Coyhis and White 2006). Depending on acculturation, availability of a community support network, and the nature of their presenting problems, Native American clients may be more likely to solicit help from significant others, extended family members, and community members. Contemporary manifestations of Native American mutual-help efforts include adaptations of the 12 Steps (Exhibit 5-4) and of 12-Step meeting rituals and practices (Coyhis and White 2006). Another modified element of the 12 Steps is use of a circular, rather than a linear, path to healing. The circle is important to American Indian philosophy, which sees the great forces of life and nature as circular (Coyhis 2000). In addition, staff members of the White Bison program have also rewritten the AA “Big Book” from a Native American perspective (Coyhis and Simonelli 2005). The principles of the 12 Steps, which involve using the group or community to provide support and motivation while emphasizing spiritual reconnection, appeal to many Native Americans who see treatment as social in nature and who view addiction as a spiritual problem.
Exhibit 5-4
The Lakota Version of the 12 Steps.
The Native American Wellbriety movement is a modern, indigenous mutual-help program that has its roots in 12-Step groups but incorporates Native American spiritual beliefs and cultural practices (Coyhis and Simonelli 2005; Coyhis and White 2006; White Bison, Inc. 2002; also see http://www.whitebison.org). Although the Wellbriety movement is popular with many Native Americans in recovery, a considerable number also continue to participate in traditional 12-Step groups. In the AI-SUPER-PFP, 47 percent of Northern Plains Tribe respondents and 28.8 percent of Southwest Tribe respondents with a past-year substance use disorder reported 12-Step group attendance in the prior year (Beals et al. 2006). Mohatt et al. (2008b) found that more Alaska Natives in recovery reported participation in 12-Step groups than in substance abuse treatment. In Venner and Feldstein's (2006) research with American Indians in recovery, 84 percent of respondents had attended some mutual-help meetings.
Traditional healing and complementary methods
Native American peoples have a range of beliefs about health care—from traditional beliefs to strong support for modern science—and may use a number of strategies when addressing health problems. Traditional healing practices are often used in conjunction with modern medicine. For example, American Indians traditionally view all things as deeply interconnected. Disruption of the physical, mental, spiritual, or emotional sides of a person can result in illness. A Native American client may consult a medical doctor to address part of the problem and a traditional healer to help regain balance and harmony.
The use of traditional healing for substance abuse and mental health problems is fairly common among Native Americans (Herman-Stahl and Chong 2002; Herman-Stahl et al. 2003). For example, among Native American individuals who reported a substance use disorder in the past year, 57.4 percent of those from a Southwest Tribe and 31.7 percent from a Northern Plains Tribe used traditional healers or healing practices (Beals et al. 2006). In a survey of American Indians from three different Arizona Tribes, 27.4 percent stated that they had used traditional healers and/or healing practices to help with mental health problems (Herman-Stahl and Chong 2002). Overall, many Native Americans believe that culture is the primary avenue of healing and that connecting with one's culture is not only a means of prevention, but also a healing treatment (Bassett et al. 2012)
Each Native American culture has its own specific healing practices, and not all of those practices are necessarily appropriate to adapt to behavioral health treatment settings. However, many traditional healing activities and ceremonies have been made accessible during treatment or effectively integrated into treatment settings (Castro et al. 1999b; Coyhis 2000; Coyhis and White 2006; Mail and Shelton 2002; Sue 2001; White 2000). These practices include sacred dances (such as the Plains Indians' sun dance and the Kiowa's gourd dance), the four circles (a model for conceptualizing a harmonious life), the talking circle, sweat lodges, and other purification practices (Cohen 2003; Mail and Shelton 2002; White 2000). The sweat lodge, in particular, is frequently used in substance abuse treatment settings (Bezdek and Spicer 2006; Schiff and Moore 2006).
Alaskan behavioral health programs have developed recovery camps to provide a treatment setting that incorporates Native beliefs and seasonal practices (e.g., Old Minto Family Recovery Camp: http://www.tananachiefs.org/health-services/old-minto-family-recovery-camp-new/). Recovery camps are based on the model of traditional Native Alaskan fishing camps and provide a context in which clients can learn about traditional practices, such as sustenance activities. Another program, the Village Sobriety Project, incorporates traditional Yup'ik and Cup'ik Eskimo traditions of hunting, chopping wood, berry picking, and taking tundra walks (Mills 2003). See Niven (2010) for a review of client-centered, culturally responsive behavioral health techniques for use with Alaska Natives.
It is difficult to measure the effectiveness of Native American healing practices using Western standards and practices. Limited or inconsistent funding, migration patterns, culturally incompetent or incongruent evaluation practices, and abuses incurred during or after data collection are major confounding variables that have limited knowledge on the effectiveness of incorporating traditional practices into Western approaches to the treatment of substance abuse and mental illness. Nonetheless, Mail and Shelton (2002) reviewed earlier literature on the use of “indigenous therapeutic interventions” for alcohol abuse and dependence and suggest that a number of these interventions have been of value to Native Americans with substance use disorders. Other authors have concurred (Coyhis and White 2006; Sabin et al. 2004).
There are a number of potential pitfalls that can occur when trying to integrate Native spiritual and cultural practices into treatment. Cultural groups are complex systems; removing pieces of them for implementation as part of a treatment program can be a disservice to the culture as well as the clients (Kunitz et al. 1994; Moss et al. 2003); a breach of customs and traditions; and a sign of disrespect for the community and Tribe, Tribal leadership, and Native American practices. It is important to take the time to build relationships and seek consultation with Tribal elders, and other Tribal leaders to ensure that the best and most appropriate steps are taken in creating a culturally relevant and responsive treatment model and program.
Regardless of whether a program adapts specific Native American healing practices, providers working with this population should recognize that spirituality is central to its values and is perceived as an integral part of life itself. It is through spiritual experiences that Native Americans believe they will find meaning in life. Some Native languages have words that refer to spirituality as “walking around” or “living the path.” In many cases, the spiritual traditions of Native Americans are not (and have never been) conceived of as a religion, but rather as a set of beliefs and practices that pervades every aspect of daily life (Deloria 1973).
Despite religion and spirituality often playing important roles in recovery from mental and substance use disorders for Native Americans, providers should not assume that only indigenous spirituality is relevant. The majority of Native Americans do not practice their traditional spirituality exclusively, and Christian religious institutions like the Native American Church and Pentecostal churches have been instrumental in helping many Native Americans overcome substance use disorders (Garrity 2000). In 2001, roughly 20 percent of American Indians identified as Baptist, 17 percent as Catholic, 17 percent as having no religious preference, and 3 percent as following a Tribal religion (Kosmin et al. 2001).
The relative importance of religion can also vary among diverse Native American communities. Before pursuing traditional methods, assessment of clients' spiritual orientation is important. Spirituality is a personal issue that treatment providers must respect; clients should choose which spiritual and cultural methods to incorporate into treatment. Providers should also be wary of an obsession with their clients' cultural activities, which may be considered intrusive (LaFromboise et al. 1993). Checking with community resources on the subject and asking the client “What feels right for you?” are appropriate steps to take in identifying whether traditional healing practices will have therapeutic value. Providers should consult with Native healers or Tribal leaders about the appropriateness of using a particular practice as part of behavioral health services. Rather than using traditional healing methods themselves, counselors may wish to refer clients to a Native American healer in the community or in the treatment program.
Relapse prevention and recovery
Despite limited data on long-term recovery for Native Americans who have substance use disorders, a few studies have found high rates of relapse following substance abuse treatment (see review in Chong and Herman-Stahl 2003). White and Sanders (2004) recommend that long-term recovery plans for Native Americans make use of a recovery management rather than a traditional continuing care approach. Such an approach emphasizes the use of informal recovery communities and traditional healing approaches to provide extended monitoring and support for Native Americans leaving treatment.
Researchers have conducted interviews with both American Indians (Bezdek and Spicer 2006) and Alaska Natives (Hazel and Mohatt 2001; Mohatt et al. 2008; People Awakening Project 2004) who have achieved extended periods of recovery. Bezdek and Spicer (2006) identified two key tasks for American Indians entering recovery. First, they need to learn how to respond to family and friends who drank with them and to those who supported their recovery. Next, they have to find new ways to deal with boredom and negative feelings. By accomplishing these tasks, Native clients can build new social support systems, develop effective coping strategies for negative feelings, and achieve long-term recovery. The People Awakening Project found that, among Alaska Natives who had a substantial period of recovery, t he development of active, culturally appropriate coping strategies was essential (e.g., distancing themselves from friends or family who drank heavily, getting involved in church, doing community service, praying; Hazel and Mohatt 2001; Mohatt et al. 2008; People Awakening Project 2004).
Counseling for White Americans
According to the 2010 U.S. Census definition, White Americans are people whose ancestors are among those ethnic groups believed to be the original peoples of Europe, the Middle East, or North Africa (Humes et al. 2011). The racial category of White Americans includes people of various ethnicities, such as Arab Americans, Italian Americans, Polish Americans, and Anglo Americans (i.e., people with origins in England), among others. Many Latinos will also identify racially (if not ethnically) as White American. Non-Latino White Americans constitute the largest racial group in the United States (making up 63.7 percent of the population in the 2010 Census; Mather et al. 2011).
White Americans, like other large ethnic and cultural groups, are extremely heterogeneous in historical, social, economic, and personal features, with many (often subtle) distinctions among subgroups. Perhaps because White Americans have been the majority in the United States, it is sometimes forgotten how historically important certain distinctions between diverse White American ethnic heritages have been (and continue to be, for some). Conversely, many White American people prefer not to see themselves as such and instead identify according to their specific ethnic background (e.g., as Irish American). For similar reasons, certain cross-cutting cultural issues (see Chapter 1) like geographic location, sexual orientation, and religious affiliation are important in defining the cultural orientations of many White Americans.
Beliefs About and Traditions Involving Substance Use
Historically, use of alcohol was accepted among White/European cultural groups because it provided an easy way to preserve fruit and grains and did not contain bacteria that might be found in water. Over time, the production and consumption of alcohol became an often-integral part of cultural activities, which can be seen in the way some White cultural groups take particular pride in national brands of alcoholic beverages (e.g., Scotch whisky, French wine; Abbott 2001; Hudak 2000). A number of European cultural groups (e.g., French, Italian) traditionally believed that daily alcohol use was healthy for both mind and body (Abbott 2001; Marinangeli 2001), and for others (e.g., English, Irish), the bar or pub was the traditional center of community life (O'Dwyer 2001). Despite some variations in cultural attitudes toward appropriate drinking practices, alcohol has been and remains the primary recreational substance for Whites in the United States. Predominant attitudes toward drinking in the United States more closely reflect those of Northern Europe; alcohol use is generally accepted during celebrations and recreational events, and, at such times, excessive consumption is more likely to be acceptable.
Typically, White European cultural groups accept alcohol use as long as it does not interfere with responsibilities, such as work or family, or result in public drunkenness (Hamid 1998). However, among certain groups of White Americans (usually defined by religious beliefs), the use of alcohol or any other intoxicant is considered immoral (van Wormer 2001). These religious beliefs, combined with concerns about the effects of problematic drinking patterns (especially among men in the frontier; White 1998), became the impetus for the early 19th-century creation of the Temperance Movement and culminated in the passing of the 18th Amendment to the United States Constitution, which enacted Prohibition. Although the Temperance Movement is no longer a major political force, belief in the moral and social value of abstinence continues to be strong among some segments of the White American population.
Illicit drug use, on the other hand, has historically been demonized by White American cultural groups and seen as an activity engaged in by people of color or undesirable subcultures (Bonnie and Whitebread 1970; Hamid 1998; Whitebread 1995). For example, White Americans typically link drug use to perceived threat of crime—particularly crimes perpetrated by people of color (Hamid 1998; Whitebread 1995). Attitudes have changed over time, but White American cultural groups continue to enforce strong cultural prohibitions against most types of illicit drug use. At the same time, White Americans are often more accepting of prescription medication abuse and less likely to perceive prescription medications as potentially harmful (Hadjicostandi and Cheurprakobkit 2002).
Despite illicit drug use now being as common among White Americans as people of color, White Americans still tend to perceive drug use as an activity that occurs outside their families and communities. In a 2001 survey, only 54 percent of White Americans expressed concern that someone in their family might develop a drug abuse problem compared with 81 percent of African Americans (Pew Research Center for the People and the Press 2001). In the same survey, White Americans expressed less concern about drug abuse in their neighborhoods than did other racial and ethnic groups. However, in terms of seeing drugs as a national problem, White Americans and other racial and ethnic groups are in closer agreement. Perhaps as a result of this misperception about the prevalence of drug use in their homes and communities, White American parents are less likely to convey disapproval of drug use to their children than African American parents (National Center on Addiction and Substance Abuse 2005) and much more likely than Latino or African American parents to think that their children have enough information about drugs (Pew Research Center for the People and the Press 2001).
There are also differences in how White Americans, Latinos, and African Americans perceive drug and alcohol addictions. White Americans are less likely than African Americans, but more likely than Latinos, to state that they believe a person can recover fully from addiction (Office of Communications 2008). However, White Americans are more likely than African Americans to indicate that substance use disorders should be treated as diseases (Durant 2005).
Substance Use and Substance Use Disorders
According to 2012 NSDUH data, rates of past-year substance use disorders were higher for White Americans than for Native Hawaiians, other Pacific Islanders, and Asian Americans; rates of current alcohol use were higher than for every other major ethnic/racial group (SAMHSA 2013d). Alcohol has traditionally been the drug of choice among White Americans of European descent; however, not all European cultural groups have the same drinking patterns. Researchers typically contrast a Northern/Eastern European pattern, in which alcohol is consumed mostly on weekends or during celebrations, with that of Southern Europe, in which alcohol is consumed daily or almost daily but in smaller quantities and almost always with food. The Southern European pattern involves more regular use of alcohol, but it is also associated with less alcohol-related harm overall (after controlling for total consumption; Room et al. 2003). The pattern of White Americans typically follows that of Northern and Eastern Europe, but individuals from some ethnic groups maintain the Southern European pattern.
White Americans, on average, begin drinking and develop alcohol use disorders at a younger age than African Americans and Latinos (Reardon and Buka 2002). White Americans are more likely to have their first drink before the age of 21 and to have their first drink before the age of 16 than members of any other major racial/ethnic group except Native Americans (SAMHSA 2011c). Some data suggest that White Americans begin using illicit drugs at an earlier age than African Americans (Watt 2008) and that the mean age for White Americans who inject heroin has decreased (Broz and Ouellet 2008).
White Americans who use heroin are less likely than people who use heroin from all other major racial/ethnic groups except African Americans to have injected the drug (SAMHSA 2011c). White Americans are also more likely than members of other major racial/ethnic groups, except Native Hawaiians and other Pacific Islanders (for whom estimates may not be accurate), to have tried ecstasy. Except for Native Americans (some of whom may use the hallucinogen peyote for religious purposes), they are also more likely than other racial/ethnic groups to have tried hallucinogens (SAMHSA 2011c). Research confirms that prescription drug misuse is more common among White Americans than African Americans or Latinos (Ford and Arrastia 2008; SAMHSA 2011c), and they are more likely to have used prescription opioids in the past year and to use them on a regular basis.
Comparative studies indicate that White Americans are more likely than all other major racial/ethnic groups except Native Americans to have an alcohol use disorder (Hasin et al. 2007; Perron et al. 2009; Schmidt et al. 2007). White Americans are at a greater risk of having severe alcohol withdrawal symptoms (such as delirium tremens) than are African Americans or Latinos with alcohol use disorders (Chan et al. 2009). So too, White Americans are more likely than African Americans or Latinos to meet diagnostic criteria for a drug use disorder at some point during their lives (Perron et al. 2009). Overall, substance use disorders vary considerably across and within non-European White American cultural groups. For example, rates of substance abuse treatment admissions in Michigan from 2005 suggest that substance use disorders may be considerably lower for Arab Americans than other White Americans (Arfken et al. 2007).
Mental and Co-Occurring Disorders
About 20 percent of White Americans reported some form of mental illness in the past year, and they were more likely to have past-year serious psychological distress than other population groups excluding Native Americans (SAMHSA 2012a).
White Americans appear to be more likely than Latinos or Asian Americans to have CODs (Alegria et al. 2008a; Vega et al. 2009) and more likely to have concurrent serious psychological distress and substance use disorders (SAMHSA 2011c). White Americans with CODs are also more likely to receive treatment for both their substance use and mental disorders than are African Americans with CODs (Alvidrez and Havassy 2005; Hatzenbuehler et al. 2008), but they are perhaps less likely to receive treatment for their substance use disorder alone (Alvidrez and Havassy 2005). White Americans are more likely to receive family counseling and mental health services while in substance abuse treatment and less likely to have unmet treatment needs (Marsh et al. 2009; Wells et al. 2001). In addition, White Americans are significantly less likely than Latinos or African Americans to believe that antidepressants are addictive (Cooper et al. 2003).
The most common mental disorders among White Americans are mood disorders (particularly major depression and bipolar I disorder) and anxiety disorders (specifically phobias, including social phobia, and generalized anxiety disorder; Grant et al. 2004b). Among White Americans, these disorders are more prevalent than in any other ethnic/racial groups save Native Americans (Grant et al. 2005; Hasin et al. 2005). For example, rates of a lifetime diagnosis of generalized anxiety disorder are about 40 percent lower for African Americans and Latinos than for White Americans and about 60 percent lower for Asian Americans (Grant et al. 2005). A similar pattern exists for major depressive disorder (Hasin et al. 2005).
Treatment Patterns
White Americans are more likely to receive mental health treatment or counseling than other racial/ethnic groups (SAMHSA 2012b). White Americans are more likely than African Americans to receive substance abuse treatment services from a private physician or other behavioral health or primary care professional (Perron et al. 2009). Among White American clients entering substance abuse treatment programs in 2010, alcohol (alone or in conjunction with illicit drugs) was most often the primary substance of abuse, followed by heroin and cannabis. However, findings are inconsistent concerning the relative frequency with which White Americans enter substance abuse treatment. Some studies have found that White Americans are more likely to receive needed behavioral health services than both African Americans and Latinos (Marsh et al. 2009; Wells et al. 2001). In contrast, other studies have found that African Americans with an identified need are somewhat more likely to enter treatment for drug use disorders and about as likely to receive treatment for alcohol use disorders when compared with White Americans (Hatzenbuehler et al. 2008; Perron et al. 2009; SAMHSA, CBHSQ 2012; Schmidt et al. 2006).
Beliefs and Attitudes About Treatment
White Americans appear to be generally accepting of behavioral health services. They have better access to health care and are more likely to use services than people of color, but this varies widely based on socioeconomic status and cultural affiliation. Most treatment services have historically been developed for White American populations, so it is not surprising that White Americans are more likely than other racial/ethnic groups to be satisfied with treatment services (Tonigan 2003).
Still, attitudes differ among certain cultural subgroups of White Americans. For example, Russian immigrants from the former Soviet Union have a longstanding distrust of mental health systems and hence may avoid substance abuse treatment (Kagan and Shafer 2001). Other groups who have a strong family orientation, such as Italian Americans or Scotch-Irish Americans, might avoid treatment that asks them to reveal family secrets (Giordano and McGoldrick 2005; Hudak 2000).
According to 2010 NSDUH data regarding people who recognized a need for substance abuse treatment in the prior year but did not receive it, White Americans were more likely than members of other major racial/ethnic groups to state that it was because they had no time for treatment, that they were concerned what their neighbors might think, that they did not want others to know, and/or that they were concerned about how it might affect their jobs (SAMHSA 2011c). Other research confirms that White Americans are significantly more likely to avoid treatment due to fear of what others might think or because they are in denial (Grant 1997). White Americans may also have different attitudes toward recovery, at least regarding alcohol use disorders, than do members of other ethnic/racial groups. According to NESARC data on people who met criteria for a diagnosis of alcohol dependence at some point during their lives, White Americans were more likely than African Americans, Latinos, or other non-Latinos to have achieved remission from that disorder but were also less likely than African Americans or other non-Latinos (but not Latinos) to currently abstain from drinking, as opposed to being in partial remission or drinking without symptoms of alcohol dependence (Dawson et al. 2005).
Treatment Issues and Considerations
Most major treatment interventions have been evaluated with a population that is largely or entirely White American, although the role of White American cultural groups is rarely considered in evaluating those interventions. For example, as Straussner (2001) notes, “the paradox of writing about substance abusers of European background is that they are a group that is believed to be the group for whom the traditional alcohol and other drug treatment models have been developed, and yet they are a group whose unique treatment needs and treatment approaches have rarely been explored” (p. 165). Very few evaluations of treatment strategies and interventions (whether based on research or clinical observation) have taken into account ethnic and cultural differences among White American clients, and therefore it is generally not possible to make culturally responsive recommendations for specific subgroups of White Americans.
Culturally responsive treatment for many White Americans will involve helping them rediscover their cultural backgrounds, which sometimes have been lost through acculturation and can be an important part of their long-term recovery. Giordano and McGoldrick (2005) note that ethnic identity and culture can be more important for some White Americans “in times of stress or personal crisis,” when they may want to “return to familiar sources of comfort and help, which may differ from the dominant society's norms” (p. 503). Appendix B provides information on instruments for assessing cultural identification. For an overview of challenges in maintaining mental health, access to health care, and help-seeking among White Americans, see Downey and D'Andrea (2012).
Theoretical Approaches and Treatment Interventions
Overall, the optimum treatment approach with White Americans is a comprehensive one; the more tools in the toolkit, the greater the chance of success (McCaul et al. 2001). Within-group differences arise regarding education level, socioeconomic status, gender, and other factors, which must be considered. Providers can, however, assume that most well-accepted treatment approaches and interventions (e.g., CBT, motivational interviewing, 12-Step facilitation, contingency management, pharmacotherapies) have been tested and evaluated with White American clients.
Still, treatment is not uniformly appropriate even for White Americans. Approaches may need modification to suit class, ethnic, religious, and other client traits. Providers should establish not only the client's ethnic background, but also how strongly the person identifies with that background. Few clinicians have made observations on best therapeutic approaches for members of particular White American cultural/ethnic subgroups.
Family therapy
In White American families, individuals are generally expected to be independent and self-reliant; as a result, families in therapy can have trouble adjusting to work that focuses more on communication processes than specific problems or content (McGill and Pearce 2005). Van Wormer (2001) notes that many White Americans need help addressing communication issues. In family therapy, useful approaches include those that encourage open, direct, and nonthreatening communication.
There is no singular description that fits White American families within or across ethnic heritages, and there is no approach that is effective for all White Americans in family therapy (Hanson 2011). Hierarchical families, such as German American families, may expect the counselor to be authoritative, at least in the initial sessions (Winawer and Wetzel 2005), although a more egalitarian German American family might not respond well to such imperatives. In the same vein, one client of French background could readily accept direct and clear therapeutic assignments that contain measurable goals (Abbot 2001), whereas another French American client may value counseling that is more process oriented. Thus, it is imperative to assess the cultural identification of clients and their families, along with the treatment needs that best match their cultural worldviews.
In some White American families, there is a longstanding culture of drinking. Attempts at abstinence can be perceived by family members as culturally inappropriate. In other families, there is deep denial about alcohol abuse or dependence, especially when talking about substance use to those outside the family. For example, some Polish American families can be resistant to the idea that drinking is the cause of family problems (Folwarski and Smolinski 2005) and sometimes believe that to admit an alcohol problem, especially to someone outside the family, signals weakness.
Group therapy
Standard group therapies developed for mental health and substance abuse treatment programs have generally been used and evaluated with White American populations. For details on group therapy in substance abuse treatment, see TIP 41, Substance Abuse Treatment: Group Therapy (CSAT 2005c).
Mutual-help groups
Mutual-help groups, of which AA is the most prevalent, have a largely White American membership (AAWS 2008; Atkins and Hawdon 2007). In a 2011 survey, 87 percent of AA members indicated their race as White (AAWS 2012). In research with largely White populations, AA participation has been found to be an effective strategy for promoting recovery from alcohol use disorders (Dawson et al. 2006; McCrady et al. 2004; Moos and Moos 2006; Ritsher et al. 2002; Weisner et al. 2003). Other mutual-help groups, such as Self-Management and Recovery Training, Secular Organizations for Sobriety/Save Our Selves, and Women for Sobriety, also have predominately White American membership and are based on Western ideas drawn from psychology (Atkins and Hawdon 2007; White 1998).
The appeal of mutual-help groups among White Americans rests on the historical origins of this model. The 12-Step model was originally developed by White Americans based on European ideas of spirituality, faith, and group interaction. Although the model has been adopted worldwide by different cultural groups (White 1998), the 12-Step model works especially well for White ethnic groups, including Irish Americans, Polish Americans, French Americans, and Scotch-Irish Americans, because it incorporates Western cultural traditions involving spiritual practice, public confession, and the use of anonymity to protect against humiliation (Abbott 2001; Gilbert and Langrod 2001; Hudak 2000; McGoldrick et al. 2005; Taggart 2005).
In addition to mutual-help groups for substance abuse, numerous recovery support groups, Internet resources, Web-based communities, and peer support programs are available to promote mental health recovery. Many resources are available through the National Alliance on Mental Illness (http://www.nami.org).
Traditional healing and complementary methods
Only 12 percent of White Americans consider themselves atheist, agnostic, or secular without a religious affiliation, meaning that, as a group, White Americans are more religious than Asian Americans but less so than Latinos or African Americans (Pew Forum on Religion and Public Life 2008). As with other groups, White Americans belong to many different religions, although the vast majority belong to various Christian denominations, with approximately 57 percent identifying as Protestant and 25.9 percent as Catholic (National Center on Addiction and Substance Abuse, 2001). White Americans also make up 91 percent of practitioners of Judaism in the United States, 14 percent of followers of Islam, and 32 percent of the American Buddhist population (Kosmin et al. 2001). For more religious White Americans, pastoral counseling or prayer can be useful aids in the treatment of substance use disorders. However, White Americans are significantly less likely to use prayer as a method of coping (Graham et al. 2005). White Americans are more likely than members of other major racial/ethnic groups to use complementary or alternative medical therapies, such as herbal medicine, acupuncture, chiropractors, massage therapy, yoga, and special diets (Graham et al. 2005).
Relapse prevention and recovery
Factors that promote recovery for White Americans include the learning and use of coping skills (Litt et al. 2003; Litt et al. 2005; Maisto et al. 2006). Even though some research suggests that White Americans are less likely to use coping skills than African Americans (Walton 2001) and have lower levels of self-efficacy upon leaving treatment (Warren et al. 2007), the development of these skills and of self-efficacy is important in managing relapse risks and in maintaining recovery. Counselors may offer psychoeducation on the value of coping strategies, specific skills to manage stressful situations or environments, and opportunities to practice these skills during treatment. Some coping skills or strategies may be more important than others in managing high-risk situations, but research suggests that greater use of a variety of coping strategies is more important than the use of any one specific skill (Gossop et al. 2002).
Social and family supports are also important in maintaining recovery and preventing relapse among White Americans (Laudet et al. 2002; McIntosh and McKeganey 2000; Rumpf et al. 2002). Other important factors include continuing care, the development of substitute behaviors (i.e., reliance on healthy or positive activities in lieu of substance use), the creation of new caring relationships that do not involve substance use, and increased spirituality (Valliant 1983). Valliant (1983) and others (e.g., Laudet et al. 2002; McCrady et al. 2004; Moos and Moos 2006) conclude, based on research with mostly White participants, that mutual-help groups often play an important role in maintaining recovery.
TIPs That Provide Supplemental Information on Topics in This Chapter
TIP 34: Brief Interventions and Brief Therapies for Substance Abuse (CSAT 1999a)
TIP 35: Enhancing Motivation for Change in Substance Abuse Treatment (CSAT 1999c)
TIP 39: Substance Abuse Treatment and Family Therapy (CSAT 2004b)
TIP 41: Substance Abuse Treatment: Group Therapy (CSAT 2005c)
TIP 42: Substance Abuse Treatment for Persons With Co-Occurring Disorders (CSAT 2005d)
TIP 44: Substance Abuse Treatment for Adults in the Criminal Justice System (CSAT 2005b)
TIP 47: Substance Abuse: Clinical Issues in Intensive Outpatient Treatment (CSAT 2006c)
TIP 51: Substance Abuse Treatment: Addressing the Specific Needs of Women (CSAT 2009c)
TIP 57: Trauma-Informed Care in Behavioral Health Services (SAMHSA 2014)
Planned TIP: Relapse Prevention and Recovery Promotion in Behavioral Health Services (SAMHSA planned e)
- Behavioral Health Treatment for Major Racial and Ethnic Groups - Improving Cultu...Behavioral Health Treatment for Major Racial and Ethnic Groups - Improving Cultural Competence
Your browsing activity is empty.
Activity recording is turned off.
See more...