1.1. Background
1.1.1. Overview and scope of the guidelines
Over the past 40 years, there have been significant advances in the development of new contraceptive technologies, including changes in formulations and dosing, schedules for administration and novel delivery systems. However, current policies and health-care practices in some countries are based on scientific studies of contraceptive products that are no longer in wide use, on long-standing theoretical concerns that have never been substantiated or on the personal preference or bias of service providers. These outdated policies or practices often result in limitations to both the quality of, and the access to, family planning services for clients.
The goal of this document is to improve access to, and quality of, family planning services by providing policy-makers, decision-makers and the scientific community with recommendations that can be used for developing or revising national guidelines on medical eligibility criteria used in the provision of all hormonal contraceptives, intrauterine devices, barrier methods, fertility awareness-based methods, coitus interruptus, lactational amenorrhoea method, male and female sterilization, and emergency contraception. These evidence-based recommendations do not indicate a “best” method that should be used given a particular medical context; rather, review of the recommendations allows for consideration of multiple methods that could be used safely by people with certain health conditions (e.g. hypertension) or characteristics (e.g. age).
Because country situations and programme environments vary so greatly, it is inappropriate to set firm international guidelines on criteria for contraceptive use. However, it is expected that national programmes will use these recommendations for updating or developing their own contraceptive eligibility guidelines according to national health policies, needs, priorities and resources, while reflecting upon local values and preferences.
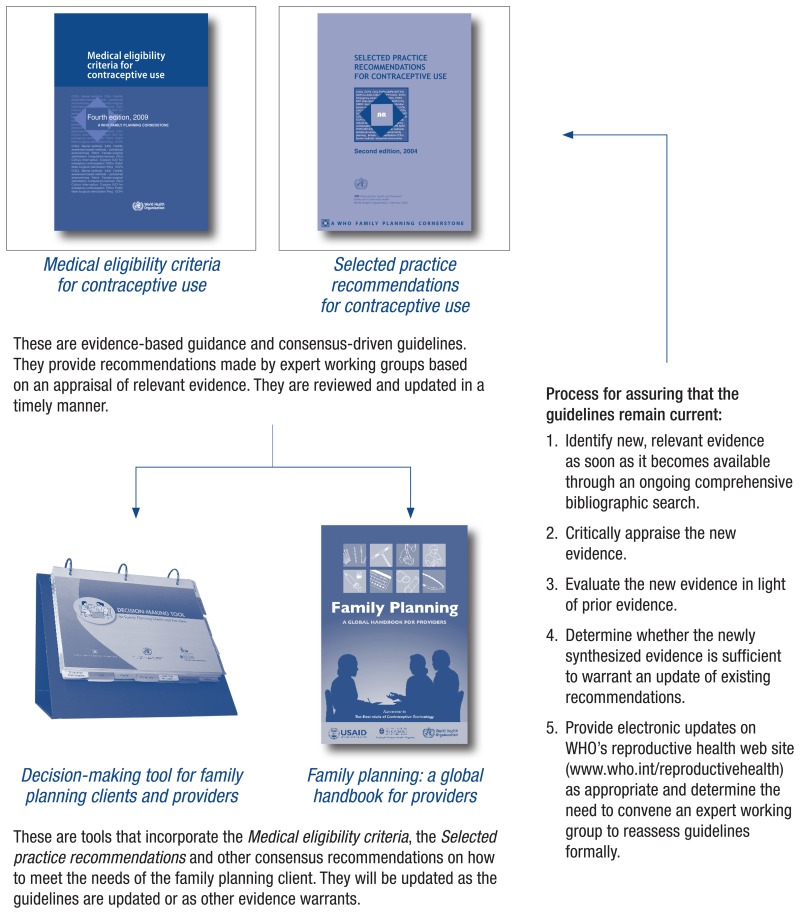
There are a total of four WHO guidance documents (cornerstones) pertaining to contraception; two that focus on evidence-based recommendations (primarily targeted towards policy-makers and programme managers) and two that focus on application of the recommendations (primarily targeted towards health-care providers). All four cornerstones are best interpreted and used in a broader context of reproductive and sexual health care. These four documents, listed below, are updated periodically to reflect changes in the medical and scientific knowledge.
Evidence-based recommendations for provision of contraception:
- Medical eligibility criteria for contraceptive use (MEC) – provides guidance regarding “who” can use contraceptive methods safely; and
- Selected practice recommendations for contraceptive use (SPR) – provides guidance regarding “how” to use contraceptive methods safely and effectively.
Practical tools for front-line providers of contraceptive counselling and services:
- 3.
Decision-making tool for family planning clients and providers – counselling tool that supports both provider and client in the process of choosing a contraceptive method; and
- 4.
Family planning: a global handbook for providers – offers evidence-based information on service delivery, method by method.
1.2. Methods
1.2.1. Development of earlier editions of the Medical eligibility criteria for contraceptive use
This document builds on a process initiated in 1994 to develop the first edition. The initial process involved comparing the eligibility criteria used by different agencies for various contraceptives, preparing summaries of published medical and epidemiological literature relevant to medical eligibility criteria, and preparing a draft classification for review by a larger group of experts and agencies. Two expert Working Group meetings were organized by WHO, in March 1994 and May 1995, to review the background classifications and to formulate recommendations; publication of the document followed in 1996.
Since the publication of the first edition of the MEC, the guideline has been revised and updated three times. With each revision, a Working Group of multidisciplinary experts was assembled to review newly published evidence pertaining to the topics addressed in the guideline. Moreover, with each revision, the Working Group used the opportunity to consider inclusion of new medical conditions and new contraceptive methods, as appropriate.
The second edition of the MEC was based on the recommendations of an expert Working Group meeting held at WHO on 8–10 March 2000, which brought together 32 participants from 17 countries, including representatives of many agencies and organizations. The Working Group reviewed new evidence since the last meetings in 1994 and 1995, primarily obtained from systematic reviews of the most recent literature.
The third edition of the MEC, was based on the recommendations of an expert Working Group meeting held at WHO on 21–24 October 2003, which gathered 36 participants from 18 countries, including representatives of many agencies and organizations. Systematic reviews of the evidence were prepared on topics with newly published evidence since the meeting in 2000; they were presented to the Working Group and provided the basis for their decision-making. A Guideline Steering Group (GSG), comprising seven external members, was established for this edition. The GSG was formed to advise WHO on behalf of the larger expert Working Group on matters related to emerging published evidence on topics covered by the guideline during interim periods between expert Working Group meetings.
The fourth edition of the MEC was based on the recommendations of an expert Working Group meeting held at WHO on 1–4 April 2008, which brought together 43 participants from 23 countries, including nine agency representatives. Eighty-six new recommendations were developed and 165 recommendations were revised for the fourth edition. All members of the expert Working Group were asked to declare any conflict of interest and three of the experts declared conflicts of interest relevant to the subject matter of the meeting. These conflicts of interest were determined not to be sufficient to preclude the experts from participating in the deliberations and development of recommendations and thus they were not asked to withdraw from this process.
The Guidelines Review Committee (GRC) was established by the Director-General of WHO in 2007 to ensure that WHO guidelines are of a high methodological quality and are developed through a transparent, evidence-based decision-making process. The fourth edition of the MEC was reviewed by the newly established GRC and was approved on 16 September 2009.
To assure that the guidelines remain current between guideline meetings, new evidence is identified through an ongoing comprehensive bibiliographic search (the Continuous Identification of Research Evidence, or CIRE system)1. This evidence is synthesized and reviewed. In circumstances where new evidence warrants further evaluation, the GSG is tasked with evaluating such evidence and issuing interim guidance if necessary. Since the release of the fourth edition of the MEC, interim guidance has been issued twice. At the request of the GSG, WHO first convened a technical consultation on 26 January 2010 via teleconference to review new evidence regarding the risk of venous thromboembolism (VTE) in postpartum women. The teleconference brought together members of the GSG and three experts on VTE during the postpartum period. All participants in the consultation were asked to declare any conflict of interest; two participants declared a conflict of interest relevant to the subject matter, but they were not asked to withdraw from the process of recommendation formulation because the WHO Secretariat and GSG did not find these conflicts of interest sufficient to preclude them from participating in the deliberations and development of recommendations. The GRC approved the updated recommendations on 21 April 2010.
Following new findings of epidemiological studies regarding the use of hormonal contraception and HIV acquisition, progression and transmission, a second technical consultation was convened by WHO during 31 January – 1 February 2012. The meeting involved 75 individuals representing a wide range of stakeholders. Through a consensus-driven process, the group considered whether recommendations in the MEC pertaining to hormonal contraceptive use among women at high risk of HIV or women living with HIV should be changed in light of the accumulating evidence. All participants in the consultation were asked to declare any conflict of interest; 13 participants declared an academic conflict of interest relevant to the subject matter of the meeting. These conflicts of interest were determined not to be sufficient to preclude them from participating in the deliberations and development of recommendations and so they were not asked to withdraw from this process. The GRC approved the technical statement presenting the conclusions and updated recommendations of the meeting on 15 February 2012.
1.2.2. Development of the Medical eligibility for criteria for contraceptive use, fifth edition
In preparation for the fifth edition of the document, both approval for the planning and ultimately the final document were obtained from the GRC. Several key aspects of the updating process were adjusted to be in closer alignment with requirements set forth in the WHO handbook for guideline development, authored by the GRC Secretariat.2 Specifically, these alterations included:
- creation of groups with varying roles to undertake the revision;
- convening an additional consultation to define the scope of the revision, giving priority to controversial topics and those for which new evidence had emerged, including topics addressed in interim guidance, clarifying recommendations with a Category 2/3 classification, and drafting questions relating to population, intervention, comparator and outcome (PICO questions) to guide the preparation of systematic reviews; and
- applying the Grading Recommendations, Assessment, Development and Evaluation (GRADE) approach to evidence review and recommendation formulation.3
The groups responsible for the development of the fifth edition of the MEC included: a WHO Secretariat; an Evidence Secretariat including a GRADE methodologist; a Guideline Steering Group (GSG); and a Guideline Development Group (GDG), which was formerly called the expert Working Group for the earlier MEC editions. The GSG, which has served as an external advisory group to WHO on family planning guidelines since 2003, was part of the larger GDG, to be compliant with WHO requirements for guideline development and to gain input from a larger advisory group. For a summary of the members of the WHO Secretariat, the Evidence Secretariat and the GDG, see the Acknowledgements at the beginning of this document.
1.2.3. Prioritization of topics for the revision process
On 14–15 May 2013, the first GDG meeting convened in Ferney Voltaire, France, to initiate the revision process for the development of the fifth edition of the MEC. Prior to the meeting, the CIRE system1 was used to identify recommendations from the fourth edition of the MEC for which new evidence was available.
To further inform decision-making with respect to clinical questions and priorities, the WHO Secretariat reached out to a broad group of stakeholders with expertise in family planning and familiarity with the guideline, including individuals from a number of implementing agencies, professional societies, and WHO regional and country offices, as well as the Ministry of Health in each of the Member States. They were asked to voluntarily complete an electronic 24-question anonymous survey available in English, French and Spanish, and to forward the link for the survey to others in their professional communities familiar with family planning and the MEC during the period 2 March – 2 May 2013. The respondents were asked to rank the importance of various outcomes pertaining to topics that had been identified as priority questions for the current revision, as well as to suggest other outcomes and clinical questions of importance, and to give input regarding the format of the guidance. More than 250 individuals submitted completed surveys; these results were presented to the GDG during the meeting to inform the prioritization process.
At the meeting, the WHO Secretariat presented brief summaries of new evidence to the GDG to determine whether the existing recommendation remained consistent or had become inconsistent with the updated body of evidence. Recommendations considered to be possibly inconsistent with the updated body of evidence were selected for presentation and discussion at a larger meeting convened in March 2014. Recommendations considered to be consistent with the updated body of evidence, and recommendations for which no new evidence had been identified through CIRE were determined by the GDG to need no further review during the revision process.
Also at this first GDG meeting, the members were asked to consider whether WHO should include several new conditions, contraceptive methods and/or formulations of methods, based upon their global relevance and availability in multiple countries. Participants were also asked to review the two interim guidance documents released since the fourth edition. Further, during this meeting the GDG was asked to address current recommendations which were classified as category “2/3” in the fourth edition, as earlier reviews by the GRC noted that these recommendations may be confusing to users of the document.
Thus, topics were prioritized for review and consideration by the GDG at the second meeting in March 2014 based on meeting one or more of the following criteria: topics identified as controversial or of particular importance to the field; topics with new evidence, for which the existing recommendation was potentially inconsistent with the updated body of evidence; topics with interim guidance issued by WHO since the MEC fourth edition; newly introduced contraceptive methods; or recommendations from the MEC fourth edition that were determined to lack clarity by the GRC. All existing recommendations that did not fall into one of these categories were reaffirmed by the GRC and thus were not reviewed.
For the topics outlined in Table 1.1, the GDG developed questions using the PICO format (i.e. questions with specified populations, interventions, comparators and outcomes) to serve as the framework for the systematic reviews and GRADE evidence tables. In order to inform the MEC recommendations, PICO questions generally guide the systematic review to focus on studies of populations with the condition or characteristic of interest using a specific contraceptive method compared with the same population not using the method, reporting on critical safety outcomes. PICO questions were also crafted to also identify relevant indirect evidence that may have included comparator populations without the condition or characteristic of interest using the same method, or reporting on surrogate outcomes. These systematic reviews, therefore, assessed the safety risks of using a given method among women with a particular medical condition or characteristic. The remainder of the existing recommendations were determined to be consistent with the body of published evidence and did not need to be formally reviewed for this revision.
Table 1.1
Medical eligibility criteria for contraceptive use, fifth edition: selection of topics for 2014 revision.
1.2.4. Evidence identification and synthesis
For each of the priority topics listed in Table 1.1, systematic reviews were conducted in accordance with PRISMA guidelines to answer PICO-formatted questions regarding safety outcomes.4 The systematic reviews may be accessed in Annex 2. In general, the PubMed and Cochrane databases were searched for studies published in any language in a peer-reviewed journal up to 15 January 2014, to inform the systematic reviews. Reference lists and direct contact with experts in the field were also used to identify other studies, including those in press; neither grey literature nor conference abstracts were included in these reviews. Due to heterogeneity of study designs, contraceptive formulations and outcome measures, meta-analyses were generally not performed. The quality of evidence presented in individual studies within a systematic review was assessed by review authors using the United States Preventive Services Task Force system.5 GRADE evidence profiles were then prepared by a GRADE methodologist to assess the quality of the summarized evidence and include the range of the estimates of effect for each clinical outcome assessed. GRADE evidence profiles were prepared for each PICO question for which evidence was found and clinical outcomes were reported. The systematic reviews that resulted from this process were peer-reviewed by selected members of the GDG, and final drafts were made electronically available to all GDG members prior to the consultations. Printed copies of GRADE evidence profiles for each topic were also given to each GDG member during the March 2014 GDG meeting. The written and orally presented systematic reviews and GRADE evidence profiles served as the basis for the GDG's deliberations.
1.2.5. Decision-making during the Guideline Development Group meetings
During 9–12 March 2014 and 24–25 September 2014, WHO convened a series of GDG meetings to review the evidence for the priority topics and, where appropriate, revise specific recommendations in the MEC. Members of the GDG and members of the External Peer Review Group (who did not participate in the GDG meeting) submitted Declaration of Interest forms to the WHO Secretariat: 14 individuals declared an academic conflict of interest relevant to the MEC guidance. The WHO Secretariat and the GDG reviewed all declarations of interest and, with the exception of two members (Dr Glasier and Dr Sitruk-Ware), found no conflicts of interest sufficient to preclude anyone from participating in the deliberations or development of recommendations. In the case of the two exceptions, the WHO Secretariat and the GDG agreed that their disclosed academic conflicts of interest were sufficient to preclude them from participating in the deliberations and development of recommendations relevant to ulipristal acetate (Dr Glasier) and the progesterone-releasing vaginal ring (Dr Sitruk-Ware). For details of the declared academic interests see Annex 1.
The GDG considered the overall quality of the safety evidence, paying particular attention to the strength and consistency of the data, according to the GRADE approach to evidence review. In most cases, the quality of evidence pertaining to each recommendation was low or very low and only addressed potential harms related to contraceptive use. To arrive at a category designation, within the range 1–4, the GDG considered these potential harms, the GRADE evidence profiles, the benefits of preventing unintended pregnancy, as well as the other GRADE constructs of values and preferences.
The GDG endorsed an approach to patient preferences and values that prioritized the availability of a wide range of contraceptive options, as women vary in their preferences regarding contraceptive selection and in the value they place on different beneficial and harmful outcomes.6 7 In addition, the availability of a range of contraceptive options is critical because a woman's contraceptive choices are made at a particular time and in a particular societal and cultural context, and these choices are complex, multifactorial and subject to change.8 9 Decision-making for contraceptive methods usually requires making trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Owing to the focus of this guidance on the safety of specific contraceptive methods for women with medical conditions or personal characteristics, opportunity costs were not formally assessed during the formulation of these recommendations since costs may vary widely throughout different regions.10
Since publication of the first edition of the MEC in 1996, the 1–4 scale has been used to categorize medical eligibility for contraceptive use. These categories are well known by health-care providers, professional organizations, training institutions and ministries of health as the basis for determining contraceptive eligibility for women with medical conditions or characteristics. As a result, to avoid confusion and retain consistency, it was determined that recommendations would not be defined as “strong” or “weak” according to GRADE methodology and would instead retain the 1–4 scale reflecting eligibility for contraceptive use.
Through consensus, the GDG arrived at new and revised recommendations, as well as upholding the majority of the existing recommendations using the categories 1–4. For the topics they reviewed in 2014 (see Box 1.1), the GDG considered the potential benefits and risks of contraceptive method use with respect to each of the medical conditions or personal characteristics assessed.
Owing to the public health importance of recommendations on hormonal contraceptive use for women at risk of HIV and women living with HIV, and based on encouragement from the GDG, WHO issued its contraceptive eligibility guidance for women living with HIV or at high risk of acquiring the infection in advance of the entire guideline revision. The document, Hormonal contraceptive methods for women at high risk of HIV and living with HIV: 2014 guidance statement was approved by the WHO Guidelines Review Committee (GRC) on 7 July 2014. The statement was released on 24 July 2014, at the 20th International AIDS Conference.
A draft version of the entire MEC document was sent to the External Peer Review Group, comprising eight experts who did not participate in the GDG meeting. Comments received from these reviewers were addressed and incorporated into this guidance by the WHO Secretariat as appropriate. The final version of this document was approved by the GRC on 18 March 2015.
1.3. Dissemination and evaluation of the Medical eligibility criteria for contraceptive use, fifth edition
The recommendations in the Medical eligibility criteria for contraceptive use, fifth edition guidance were released during a global live Facebook Chat on 1 June 2015. A comprehensive dissemination and evaluation plan will be implemented, which will include widespread dissemination through the WHO regional and country offices, WHO Member States, the United Nations (UN) agency cosponsors of the Special Programme of Research, Development and Research Training in Human Reproduction (HRP) within the WHO Department of Reproductive Health and Research (i.e. UNDP, UNFPA, UNICEF, WHO and the World Bank), WHO collaborating centres, professional organizations, governmental and nongovernmental partner organizations working in the area of sexual and reproductive health, and civil society groups engaged in sexual and reproductive health projects The WHO Secretariat will work closely with sexual and reproductive health points of contact in the WHO regional offices to conduct a series of regional events during 2015–2016. In addition, special panel sessions will be organized during the summer and autumn of 2015 at international conferences convened by the International Society of Obstetricians and Gynaecologists (FIGO), the International Council of Nurses (ICN) and the International Confederation of Midwives (ICM) to update the membership of these societies about the revised recommendations. Once translations of the document in other official languages of the UN become available, opportunities to ensure effective dissemination will be actively sought. An evaluation survey targeting ministries of health, WHO offices and partners, professional organizations and civil society will be fielded to assess the extent and effectiveness of the dissemination, evaluate the level of implementation of the guidance into national policies, and identify areas for further refinement and research gaps in contraceptive eligibility criteria.
1.4. Reviewed recommendations
The Guideline Development Group (GDG) determined priority topics to be addressed as part of the revision process for the fifth edition (see Table 1.1).
Information on using the recommendations in practice, as well as recommendations in the fifth edition (new, revised and confirmed) are presented in Part II, sections 2.3 and 2.7, starting on p. 91. A summary of changes between the fourth edition of the MEC and the updated fifth edition is available in Part II (see section 2.6 and Tables 2.4–2.6, pp. 93–96).
1. Recommendations for combined hormonal contraceptives by age group
Question 1: Are women who use combined hormonal contraceptives (CHCs) at increased risk for fracture compared with women who do not use CHCs? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Are women who use combined hormonal contraceptives (CHCs) at increased risk for decreased bone mineral density compared with women who do not use CHCs, with a specific focus on adolescents? (Indirect evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Women from menarche to < 40 years of age can use combined hormonal contraceptives (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) without restriction (MEC Category 1).
- Women 40 years and older can generally use combined hormonal contraceptive methods (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 2).
Remarks
- In 2014, the GDG focused specifically on the evidence pertaining to fracture risk among women of all ages, and the evidence for combined hormonal contraceptives (CHCs) and potential for decreased bone mineral density (BMD) among adolescents. BMD is a surrogate marker for fracture risk that may not be valid for premenopausal women, and therefore may not accurately predict current or future (postmenopausal) fracture risk (1–3). The risk of cardiovascular disease increases with age and may also increase with CHC use. In the absence of other adverse clinical conditions, CHC can be used until menopause.
- Due to heterogeneity of study designs, contraceptive formulations and outcome measures a meta-analysis was not performed.
- CHCs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms, male or female, is recommended.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Evidence is inconsistent on the question of whether CHC use affects fracture risk (4–15), although three recent studies show no effect (4, 5, 15). CHC use may decrease BMD in adolescents, especially in those choosing very-low-dose formulations (< 30 μg ethinylestradiol-containing combined oral contraceptives) (16–29). CHC use has little to no effect on BMD in premenopausal women (30–44), and may preserve bone mass in those who are perimenopausal (45-54).
Quality of the evidence
(intervention versus comparator; outcome)
GRADE table 1
(Question 1): Are women who use combined hormonal contraceptives (CHCs) at increased risk for fracture compared with women who do not use CHCs? (Direct evidence).
GRADE table 2
(Question 2): Are women who use combined hormonal contraceptives (CHCs) at increased risk for decreased bone mineral density compared with women who do not use CHCs, with a specific focus on adolescents? (Indirect evidence).
References
- 1.
- Grimes D, Schulz K. Surrogate end points in clinical research: hazardous to your health. Obstet Gynecol. 2005;105:1114–8. [PubMed: 15863552]
- 2.
- Schonau E. The peak bone mass concept: is it still relevant? Pediatric Nephrology. 2004;19:825–31. [PubMed: 15197638]
- 3.
- Cohen A, Shane E. Treatment of premenopausal women with low bone mineral density. Curr Osteoporosis Rep. 2008;6(1):39–46. [PMC free article: PMC4414067] [PubMed: 18430399]
- 4.
- Memon S, Iversen L, Hannaford PC. Is the oral contraceptive pill associated with fracture in later life? New evidence from the Royal College of General Practitioners Oral Contraception Study. Contraception. 2011;84(1):40–7. [PubMed: 21664509]
- 5.
- Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk in very young women using combined oral contraceptives. Contraception. 2008;78(5):358–64. [PubMed: 18929731]
- 6.
- Vestergaard P, Rejnmark L, Mosekilde L. Oral contraceptive use and risk of fractures. Contraception. 2006;73(6):571–6. [PubMed: 16730486]
- 7.
- Barad D, Kooperberg C, Wactawsi-Wende J, Liu J, Hendrix S, Watts N. Prior oral contraception and postmenopausal fracture: a Women's Health Initiative observational cohort study. Fertil Steril. 2005;84(2):374–83. [PubMed: 16084878]
- 8.
- Michaelsson K, Baron JA, Farahmand BY, Ljunghall S. Influence of parity and lactation on hip fracture risk. Am J Epidemiol. 2001;153(12):1166–72. [PubMed: 11415951]
- 9.
- Michaelsson K, Baron JA, Farahmand BY, Persson I, Ljunghall S. Oral-contraceptive use and risk of hip fracture: a case-control study. Lancet. 1999;353(9163):1481–4. [PubMed: 10232314]
- 10.
- La Vecchia C, Tavani A, Gallus S. Oral contraceptives and risk of hip fractures. Lancet. 1999;354(9175):335–6. [PubMed: 10440332]
- 11.
- Vessey M, Mant J, Painter R. Oral contraception and other factors in relation to hospital referral for fracture. Findings in a large cohort study. Contraception. 1998;57(4):231–5. [PubMed: 9649913]
- 12.
- O'Neill TW, Marsden D, Adams JE, Silman AJ. Risk factors, falls, and fracture of the distal forearm in Manchester, UK. J Epidemiol Community Health. 1996;50(3):282–92. [PMC free article: PMC1060285] [PubMed: 8935460]
- 13.
- Mallmin H, Ljunghall S, Persson I, Bergstrom R. Risk factors for fractures of the distal forearm: a population-based case-control study. Osteoporosis Int. 1994;4(6):298–304. [PubMed: 7696821]
- 14.
- Cooper C, Hannaford P, Croft P, Kay CR. Oral contraceptive pill use and fractures in women: a prospective study. Bone. 1993;14(1):41–5. [PubMed: 8443001]
- 15.
- Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot medroxyprogesterone acetate and fracture risk. J Clin Endocrinol Metab. 2010;95(11):4909–16. [PubMed: 20685865]
- 16.
- Cibula D, Skrenkova J, Hill M, Stepan JJ. Low-dose estrogen combined oral contraceptives may negatively influence physiological bone mineral density acquisition during adolescence. Eur J Endocrinol. 2012;166(6):1003–11. [PubMed: 22436400]
- 17.
- Gai L, Jia Y, Zhang M, Gai P, Wang S, Shi H, et al. Effect of two kinds of different combined oral contraceptives use on bone mineral density in adolescent women. Contraception. 2012;86(4):332–6. [PubMed: 22364818]
- 18.
- Scholes D, Hubbard RA, Ichikawa LE, LaCroix AZ, Spangler L, Beasley JM, et al. Oral contraceptive use and bone density change in adolescent and young adult women: a prospective study of age, hormone dose, and discontinuation. J Clin Endocrinol Metab. 2011;96(9):E1380–E7. [PMC free article: PMC3167673] [PubMed: 21752879]
- 19.
- Lattakova M, Borovsky M, Payer J, Killinger Z. Oral contraception usage in relation to bone mineral density and bone turnover in adolescent girls. Eur J Contracept Reprod Health Care. 2009;14(3):207–14. [PubMed: 19565418]
- 20.
- Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral density in a cohort of adolescents during use of norethisterone enanthate, depot-medroxyprogesterone acetate or combined oral contraceptives and after discontinuation of norethisterone enanthate. Contraception. 2009;79(5):345–9. [PMC free article: PMC3833049] [PubMed: 19341845]
- 21.
- Pikkarainen E, Lehtonen-Veromaa M, Mottonen T, Kautiainen H, Viikari J. Estrogen-progestin contraceptive use during adolescence prevents bone mass acquisition: a 4-year follow-up study. Contraception. 2008;78(3):226–31. [PubMed: 18692613]
- 22.
- Cromer BA, Bonny AE, Stager M, Lazebnik R, Rome E, Ziegler J, et al. Bone mineral density in adolescent females using injectable or oral contraceptives: a 2–month prospective study. Fertil Steril. 2008;90(6):2060–7. [PMC free article: PMC2652861] [PubMed: 18222431]
- 23.
- Berenson AB, Rahman M, Breitkopf CR, Bi LX. Effects of depot medroxyprogesterone acetate and 20-microgram oral contraceptives on bone mineral density. Obstet Gynecol. 2008;112(4):788–99. [PMC free article: PMC2745348] [PubMed: 18827121]
- 24.
- Harel Z, Riggs S, Vaz R, Flanagan P, Harel D, Machan JT. Bone accretion in adolescents using the combined estrogen and progestin transdermal contraceptive method Ortho Evra: a pilot study. J Pediatr Adolesc Gynecol. 2010;23(1):23–31. [PubMed: 19647454]
- 25.
- Cobb KL, Bachrach LK, Sowers M, Nieves J, Greendale GA, Kent KK, et al. The effect of oral contraceptives on bone mass and stress fractures in female runners. Med Sci Sports Exerc. 2007;39(9):1464–73. [PubMed: 17805075]
- 26.
- Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral density in adolescents using norethisterone enanthate, depot-medroxyprogesterone acetate or combined oral contraceptives for contraception. Contraception. 2007;75(6):438–43. [PubMed: 17519149]
- 27.
- Lara-Torre E, Edwards CP, Perlman S, Hertweck SP. Bone mineral density in adolescent females using depot medroxyprogesterone acetate. J Pediatr Adolesc Gynecol. 2004;17(1):17–21. [PubMed: 15010034]
- 28.
- Cromer BA, Blair JM, Mahan JD, Zibners L, Naumovski Z. A prospective comparison of bone density in adolescent girls receiving depot medroxyprogesterone acetate (Depo-Provera), levonorgestrel (Norplant), or oral contraceptives. J Pediatr. 1996;129(5):671–6. [PubMed: 8917232]
- 29.
- Polatti F, Perotti F, Filippa N, Gallina D, Nappi RE. Bone mass and long-term monophasic oral contraceptive treatment in young women. Contraception. 1995;51(4):221–4. [PubMed: 7796586]
- 30.
- Sordal T, Grob P, Verhoeven C. Effects on bone mineral density of a monophasic combined oral contraceptive containing nomegestrol acetate/17beta-estradiol in comparison to levonorgestrel/ethinylestradiol. Acta Obstet Gynecol Scand. 2012;91(11):1279–85. [PubMed: 22762147]
- 31.
- Gargano V, Massaro M, Morra I, Formisano C, Di CC, Nappi C. Effects of two low-dose combined oral contraceptives containing drospirenone on bone turnover and bone mineral density in young fertile women: a prospective controlled randomized study. Contraception. 2008;78(1):10–5. [PubMed: 18555812]
- 32.
- Nappi C, Di Spiezio SA, Greco E, Tommaselli GA, Giordano E, Guida M. Effects of an oral contraceptive containing drospirenone on bone turnover and bone mineral density. Obstet Gynecol. 2005;105(1):53–60. [PubMed: 15625142]
- 33.
- Berenson AB, Radecki CM, Grady JJ, Rickert VI, Thomas A. A prospective, controlled study of the effects of hormonal contraception on bone mineral density. Obstet Gynecol. 2001;98(4):576–82. [PubMed: 11576570]
- 34.
- Berenson AB, Breitkopf CR, Grady JJ, Rickert VI, Thomas A. Effects of hormonal contraception on bone mineral density after 24 months of use. Obstet Gynecol. 2004;103(5 Pt 1):899–906. [PubMed: 15121563]
- 35.
- Elgan C, Samsioe G, Dykes AK. Influence of smoking and oral contraceptives on bone mineral density and bone remodeling in young women: a 2-year study. Contraception. 2003;67(6):439–47. [PubMed: 12814812]
- 36.
- Elgan C, Dykes AK, Samsioe G. Bone mineral density changes in young women: a two year study. Gynecol Endocrinol. 2004;19(4):169–77. [PubMed: 15724798]
- 37.
- Endrikat J, Mih E, Dusterberg B, Land K, Gerlinger C, Schmidt W, et al. A 3-year double-blind, randomized, controlled study on the influence of two oral contraceptives containing either 20 microg or 30 microg ethinylestradiol in combination with levonorgestrel on bone mineral density. Contraception. 2004;69(3):179–87. [PubMed: 14969664]
- 38.
- Paoletti AM, Orru M, Lello S, Floris S, Ranuzzi F, Etzi R, et al. Short-term variations in bone remodeling markers of an oral contraception formulation containing 3 mg of drospirenone plus 30 microg of ethinyl estradiol: observational study in young postadolescent women. Contraception. 2004;70(4):293–8. [PubMed: 15451333]
- 39.
- Nappi C, Di Spiezio SA, Acunzo G, Bifulco G, Tommaselli GA, Guida M, et al. Effects of a low-dose and ultra-low-dose combined oral contraceptive use on bone turnover and bone mineral density in young fertile women: a prospective controlled randomized study. Contraception. 2003;67(5):355–9. [PubMed: 12742557]
- 40.
- Reed SD, Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Longitudinal changes in bone density in relation to oral contraceptive use. Contraception. 2003;68(3):177–82. [PubMed: 14561537]
- 41.
- Cobb KL, Kelsey JL, Sidney S, Ettinger B, Lewis CE. Oral contraceptives and bone mineral density in white and black women in CARDIA. Coronary Risk Development in Young Adults. Osteoporosis Int. 2002;13(11):893–900. [PubMed: 12415437]
- 42.
- Burr DB, Yoshikawa T, Teegarden D, Lyle R, McCabe G, McCabe LD, et al. Exercise and oral contraceptive use suppress the normal age-related increase in bone mass and strength of the femoral neck in women 18–31 years of age. Bone. 2000;27(6):855–63. [PubMed: 11113398]
- 43.
- Recker RR, Davies KM, Hinders SM, Heaney RP, Stegman MR, Kimmel DB. Bone gain in young adult women. JAMA. 1992;268(17):2403–8. [PubMed: 1404797]
- 44.
- Mazess RB, Barden HS. Bone density in premenopausal women: effects of age, dietary intake, physical activity, smoking, and birth-control pills. Am J Clin Nutr. 1991;53(1):132–42. [PubMed: 1984338]
- 45.
- Gambacciani M, Cappagli B, Lazzarini V, Ciaponi M, Fruzzetti F, Genazzani AR. Longitudinal evaluation of perimenopausal bone loss: effects of different low dose oral contraceptive preparations on bone mineral density. Maturitas. 2006;54(2):176–80. [PubMed: 16332417]
- 46.
- Gambacciani M, Spinetti A, Taponeco F, Cappagli B, Piaggesi L, Fioretti P. Longitudinal evaluation of perimenopausal vertebral bone loss: effects of a low-dose oral contraceptive preparation on bone mineral density and metabolism. Obstet Gynecol. 1994;83(3):392–6. [PubMed: 8127531]
- 47.
- Gambacciani M, Spinetti A, Cappagli B, Taponeco F, Maffei S, Piaggesi L, et al. Hormone replacement therapy in perimenopausal women with a low dose oral contraceptive preparation: effects on bone mineral density and metabolism. Maturitas. 1994;19(2) [PubMed: 7968645]
- 48.
- Gambacciani M, Cappagli B, Ciaponi M, Benussi C, Genazzani AR. Hormone replacement therapy in perimenopause: effect of a low dose oral contraceptive preparation on bone quantitative ultrasound characteristics. Menopause. 1999;6(1):43–8. [PubMed: 10100179]
- 49.
- Gambacciani M, Ciaponi M, Cappagli B, Benussi C, Genazzani AR. Longitudinal evaluation of perimenopausal femoral bone loss: effects of a low-dose oral contraceptive preparation on bone mineral density and metabolism. Osteoporosis Int. 2000;11(6):544–8. [PubMed: 10982172]
- 50.
- Volpe A, Malmusi S, Zanni AL, Landi S, Cagnacci A. Oral contraceptives and bone metabolism. Eur J Contracept Reprod Health Care. 1997;2(4):225–8. [PubMed: 9678077]
- 51.
- Hansen M, Overgaard K, Riis B, Christiansen C. Potential risk factors for development of postmenopausal osteoporosis – examined over a 12-year period. Osteoporosis Int. 1991;1(2):95–102. [PubMed: 1790399]
- 52.
- Shargil AA. Hormone replacement therapy in perimenopausal women with a triphasic contraceptive compound: a three-year prospective study. Int J Fertil. 1985;30(1) [PubMed: 2862116]
- 53.
- Taechakraichana N, Limpaphayom K, Ninlagarn T, Panyakhamlerd K, Chaikittisilpa S, Dusitsin N. A randomized trial of oral contraceptive and hormone replacement therapy on bone mineral density and coronary heart disease risk factors in postmenopausal women. Obstet Gynecol. 2000;95(1):87–94. [PubMed: 10636509]
- 54.
- Taechakraichana N, Jaisamrarn U, Panyakhamlerd K, Chaikittisilpa S, Limpaphayom K. Difference in bone acquisition among hormonally treated postmenopausal women with normal and low bone mass. J Med Assoc Thailand. 2001 84 Suppl 2:S586–S92. [PubMed: 11853286]
2. Recommendations for combined hormonal contraceptives among breastfeeding women
Question 1: Among breastfeeding women, does initiation of combined hormonal contraceptives (CHCs) at < 6 weeks postpartum have negative effects on breastfeeding outcomes or infant outcomes, compared with no contraception or non-hormonal contraception? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among breastfeeding women, does initiation of combined hormonal contraceptives (CHCs) at ≥ 6 weeks postpartum have negative effects on breastfeeding outcomes or infant outcomes, compared with no contraception or non-hormonal contraception? (Direct evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Breastfeeding women < 6 weeks postpartum should not use combined hormonal contraceptives (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 4).
- Breastfeeding women ≥ 6 weeks to < 6 months postpartum (primarily breastfeeding) generally should not use CHCs (MEC Category 3).
- Breastfeeding women ≥ 6 months postpartum can generally use CHCs (MEC Category 2).
Remarks
- Due to heterogeneity of study designs, contraceptive formulations and outcome measures, a meta-analysis was not performed.
- Combined hormonal contraceptives (CHCs) do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Clinical studies demonstrate conflicting results regarding effects on breastfeeding continuation or exclusivity in women exposed to combined oral contraceptives (COCs) during lactation. No consistent effects on infant growth or illness have been reported (1–6). Adverse health outcomes or manifestations of exogenous estrogen in infants exposed to CHCs through breast-milk have not been demonstrated; however, studies have been inadequately designed to determine whether a risk of either serious or subtle long-term effects exists.
Quality of the evidence
< 6 weeks postpartum:
(method; outcome)
≥ 6 weeks postpartum:
(method; outcome)
GRADE table 1
(Question 1): Among breastfeeding women, does initiation of combined hormonal contraceptives (CHCs) at < 6 weeks postpartum have negative effects on breastfeeding outcomes or infant outcomes, compared with no contraception or non-hormonal contraception? (more...)
GRADE table 2
(Questions 2): Among breastfeeding women, does initiation of combined hormonal contraceptives (CHCs) at > 6 weeks postpartum have negative effects on breastfeeding outcomes or infant outcomes, compared with no contraception or non-hormonal contraception? (more...)
References
- 1.
- Bahamondes L, Bahamondes MV, Modesto W, Tilley IB, Magalhaes A, Pinto e Silva JL, et al. Effect of hormonal contraceptives during breastfeeding on infant's milk ingestion and growth. Fertil Steril. 2013;100(2):445–50. [PubMed: 23623474]
- 2.
- Espey E, Ogburn T, Leeman L, Singh R, Ostrom K, Schrader R. Effect of progestin compared with combined oral contraceptive pills on lactation: a randomized controlled trial. Obstet Gynecol. 2012;119(1):5–13. [PMC free article: PMC3586805] [PubMed: 22143258]
- 3.
- Kamal I, Hefnawi F, Ghoneim M, Abdallah M, Abdel Razek S. Clinical, biochemical, and experimental studies on lactation. V. Clinical effects of steroids on the initiation of lactation. Am J Obstet Gynecol. 1970;108(4):655–8. [PubMed: 4918514]
- 4.
- Kamal I, Hefnawi F, Ghoneim M, Talaat M, Younis N, Tagui A, et al. Clinical, biochemical, and experimental studies on lactation. II. Clinical effects of gestagens on lactation. Am J Obstet Gynecol. 1969;105(3):324–34. [PubMed: 5810783]
- 5.
- Kapp N, Curtis K. Combined oral contraceptive use among breastfeeding women: a systematic review. Contraception. 2010;82(1):10–16. [PubMed: 20682139]
- 6.
- Koetsawang S, Bhiraleus P, Chiemprajert T. Effects of oral contraceptives on lactation. Fertil Steril. 1972;23(1):24–8. [PubMed: 4109500]
3. Recommendations for combined hormonal contraceptives among postpartum women
Question 1: Among postpartum women, does combined hormonal contraceptive (CHC) use increase risk of venous thromboembolism (VTE) compared with no CHC use? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among women of reproductive age, do postpartum women have increased risk of venous thromboembolism (VTE) compared with non-postpartum, non-pregnant women? (Indirect evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Women who are < 21 days postpartum and do not have other risk factors for venous thromboembolism (VTE) generally should not use combined hormonal contraceptives (CHCs) (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 3).
- Women who are < 21 days postpartum with other risk factors for VTE should not use CHCs (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 4). For women ≤ 42 days postpartum with other risk factors for VTE, such as immobility, transfusion at delivery, BMI > 30 kg/m2, postpartum haemorrhage, immediately post-caesarean delivery, pre-eclampsia or smoking, use of CHCs may pose an additional increased risk for VTE.
- Women who are 21–42 days postpartum and do not have other risk factors for VTE can generally use CHCs (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 2). Women who are 21–42 days postpartum with other risk factors for VTE generally should not use CHC methods (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 3). For women ≤ 42 days postpartum with other risk factors for VTE, such as immobility, transfusion at delivery, BMI > 30 kg/m2, postpartum haemorrhage, immediately post-caesarean delivery, pre-eclampsia or smoking, use of CHCs may pose an additional increased risk for VTE.
- Women who are > 42 days postpartum can use CHC methods (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) without restriction (MEC Category 1).
Remarks
- The Guideline Development Group (GDG) considered the balance of benefits and harms for CHC use among postpartum women, at different time points postpartum, and with and without other risk factors for VTE, including the risk of VTE in the postpartum period, the risks associated with rapid repeat pregnancy, the benefits of preventing rapid repeat pregnancy, and the availability of other contraceptive methods that are safe for use by postpartum women. The GDG also considered that risk of pregnancy during the first 21 days postpartum is very low, but increases after that time in non-breastfeeding women; ovulation before first menses is common (1).
- Due to heterogeneity of study designs, contraceptive formulations and outcome measures, a meta-analysis was not performed.
- CHCs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
One study examined use of CHCs during the postpartum period and found that VTE rates were higher for CHC users compared with non-users at all time points postpartum. Rates were significantly different only after 13 weeks postpartum, but the numbers needed to harm were lowest in the first 6 weeks postpartum (2). VTE risk is elevated during pregnancy and the postpartum period; this risk is most pronounced in the first 3 weeks after delivery, declining to near baseline levels by 42 days postpartum (3–7).
Quality of the evidence
(intervention versus comparator; outcome)
GRADE table 1
(Question 1): Among postpartum women, does combined hormonal contraceptive (CHC) use increase risk of venous thromboembolism (VTE) compared with no CHC use? (Direct evidence).
GRADE table 2
(Question 2): Among women of reproductive age, do postpartum women have increased risk of venous thromboembolism (VTE) compared with non-postpartum, non-pregnant women? (Indirect evidence).
References
- 1.
- Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactating women: a systematic review. Obstet Gynecol. 2011;117(3):657–62. [PubMed: 21343770]
- 2.
- Petersen JF, Bergholt T, Nielsen AK, Paidas MJ, Lokkegaard EC. Combined hormonal contraception and risk of venous thromboembolism within the first year following pregnancy. Danish nationwide historical cohort 1995–2009. Thromb Haemost. 2014;112(1):73–8. [PubMed: 24499991]
- 3.
- Kamel H, Navi BB, Sriram N, Hovsepian DA, Devereux RB, Elkind MS. Risk of a thrombotic event after the 6-week postpartum period. N Engl J Med. 2014;370(14):1307–15. [PMC free article: PMC4035479] [PubMed: 24524551]
- 4.
- Sultan AA, Tata LJ, West J, Fiaschi L, Fleming KM, Nelson-Piercy C, et al. Risk factors for first venous thromboembolism around pregnancy: a population-based cohort study from the United Kingdom. Blood. 2013;121(19):3953–61. [PubMed: 23550034]
- 5.
- Sultan AA, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ. Risk of first venous thromboembolism in and around pregnancy: a population-based cohort study. Br J Haematol. 2012;156(3):366–73. [PubMed: 22145820]
- 6.
- Tepper NK, Boulet SL, Whiteman MK, Monsour M, Marchbanks PA, Hooper WC, et al. Postpartum venous thromboembolism: incidence and risk factors. Obstet Gynecol. 2014;123(5):987–96. [PubMed: 24785851]
- 7.
- Jackson E, Curtis KM, Gaffield ME. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691–703. [PubMed: 21343773]
4. Recommendations for combined hormonal contraceptives among women with superficial venous disorders
The disease nomenclature has been updated to reflect current recognized standard terminology and more accurately describe the condition and sub-conditions. The overall name of the condition has been changed to “superficial venous disorders”. The subcondition “superficial thrombophlebitis” has been changed to “superficial venous thrombosis” (SVT).
Question 1: Among women with varicose veins, does use of combined hormonal contraceptives (CHCs) increase the risk of venous thromboembolism (VTE) or superficial venous thrombosis (SVT) compared with non-use of CHCs? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among women with superficial venous thrombosis (SVT), does use of combined hormonal contraceptives (CHCs) increase the risk of venous thromboembolism (VTE) compared with non-use of CHCs? (Direct evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Women with varicose veins can use combined hormonal contraceptives (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) without restriction (MEC Category 1).
- Women with superficial venous thrombosis (SVT) can generally use combined hormonal contraceptives (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 2). SVT may be associated with an increased risk of venous thromboembolism (VTE).
Remarks
- Due to heterogeneity of study designs, contraceptive formulations and outcome measures, a meta-analysis was not performed.
- CHCs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
One study suggested that among women with varicose veins, the rate of VTE and SVT was higher in oral contraceptive users compared with non-users; however, statistical significance was not reported and the number of events was small (1). One study demonstrated that among women with SVT, the risk of VTE was higher in oral contraceptive users compared with non-users (2).
Quality of the evidence
Women with varicose veins:
(intervention versus comparator; outcome)
Women with superficial venous thrombosis:
(intervention versus comparator; outcome)
GRADE table 1
(Question 1): Among women with varicose veins, does use of combined hormonal contraceptives (CHCs) increase the risk of venous thromboembolism (VTE) or superficial venous thrombosis (SVT) compared with non-use of CHCs? (Direct evidence).
GRADE table 2
(Question 2): Among women with superficial venous thrombosis (SVT), does use of combined hormonal contraceptives (CHCs) increase the risk of venous thromboembolism (VTE) compared with non-use of CHCs? (Direct evidence).
References
- 1.
- Oral contraceptives, venous thrombosis, and varicose veins. Royal College of General Practitioners' Oral Contraception Study. J R Coll Gen Pract. 1978;28(192):393–9. [PMC free article: PMC2158790] [PubMed: 702453]
- 2.
- Roach RE, Lijfering WM, van Hylckama Vlieg A, Helmerhorst FM, Rosendaal FR, Cannegieter SC. The risk of venous thrombosis in individuals with a history of superficial vein thrombosis and acquired venous thrombotic risk factors. Blood. 2013;122(26):4264–9. [PubMed: 24184685]
5. Recommendations for combined hormonal contraceptives among women with dyslipidaemias
Question 1: Among women with known dyslipidaemias, without other known cardiovascular risk factors, does combined hormonal contraceptive (CHC) use increase risk of arterial thromboembolism (ATE), venous thromboembolism (VTE) or pancreatitis compared with no CHC use? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among women of reproductive age using combined hormonal contraception (CHC), are women with known dyslipidaemias without other known cardiovascular risk factors at increased risk for ATE, VTE or pancreatitis compared to women without known dyslipidaemias? (Indirect evidence)
Table
Selection criteria for the systematic review.
Question 3: Among women with known dyslipidaemias without other known cardiovascular risk factors, does combined hormonal contraceptive (CHC) use increase risk for worsening of lipid abnormalities compared with no CHC use? (Indirect evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Women with known dyslipidaemias without other known cardiovascular risk factors can generally use combined hormonal contraceptive methods (combined oral contraceptives, combined contraceptive patch, combined contraceptive vaginal ring, combined injectable contraceptives) (MEC Category 2). Routine screening is not appropriate because of the rarity of the conditions and the high cost of screening. Increased levels of total cholesterol, low-density lipoprotein (LDL) and triglycerides, as well as decreased levels of high-density lipoprotein (HDL), are known risk factors for cardiovascular disease. Women with known severe genetic lipid disorders at much higher lifetime risk for cardiovascular disease may warrant further clinical consideration.
Remarks
- The Guideline Development Group (GDG) determined that the existing condition name, “known hyperlipidaemias”, should be changed to “known dyslipidaemias” to better describe the spectrum of clinically important lipid abnormalities. They also specified that the condition should include only women “without other known cardiovascular risk factors” for better clarity.
- The GDG noted that the baseline absolute risk for cardiovascular disease among women of reproductive age is very low. Using available cardiovascular risk prediction models, even among healthy perimenopausal women with high total cholesterol and normal HDL, 10-year risks for cardiovascular disease remain low. The most recent guidelines from the Fifth Joint Task Force of the European Society of Cardiology, published in 2012, predict that a healthy woman aged 45–49 years with total cholesterol levels greater than 280 mg/dL has < 1% 10-year risk for fatal myocardial infarction (MI) or stroke; similarly, recent guidelines released by the American College of Cardiology and the American Heart Association predict a 1.9% 10-year risk for a non-fatal or fatal first MI or stroke. Further, it was concluded that even if combined oral contraceptive (COC) use increases risk for MI or stroke among women of reproductive age with known dyslipidaemias and no other risk factors for cardiovascular disease, the absolute risk for these serious adverse events remains low.
- Use of combined hormonal contraception (CHC) among women with severe genetic lipid disorders may warrant further clinical consideration given that these women are at much higher lifetime risk for cardiovascular disease.
- The GDG determined that risk for arterial thrombotic events was the main safety concern for women with known dyslipidaemias without other cardiovascular risk factors. Independent of COC use, there does not appear to be a clear association between dyslipidaemia and risk for VTE among women of reproductive age, and indirect evidence from one study identified in our systematic review noted only a slight increased risk for VTE among COC users with the condition compared to users without the condition. No comparative data were available to assess the risk of pancreatitis among women with known dyslipidaemias, and while it is well established that elevated triglyceride levels are associated with acute pancreatitis, severe hypertriglyceridemia is a very rare condition with a risk for pancreatitis associated with triglyceride levels ≥ 1000 mg/dL estimated at approximately 5%.
- Due to heterogeneity of study designs, contraceptive formulations and outcome measures, a meta-analysis was not performed.
- CHCs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
One case-control study suggested an increased risk for MI among COC users with hypercholesterolemia compared to non-users without hypercholesterolemia (1). One retrospective cohort study suggested an increased risk for stroke and VTE among COC users with dyslipidaemia compared to COC users without dyslipidaemia (2). One prospective cohort study suggested no worsening of lipid abnormalities among CHC users with dyslipidaemia compared to non-users with dyslipidaemia (3).
Quality of the evidence
GRADE table 1
(Question 1): Among women with known dyslipidaemias without other known cardiovascular risk factors, does combined hormonal contraceptive (CHC) use increase risk of arterial thromboembolism (ATE), venous thromboembolism (VTE) or pancreatitis compared (more...)
GRADE table 2
(Question 2): Among women of reproductive age using combined hormonal contraception (CHC), are women with known dyslipidaemias without other known cardiovascular risk factors at increased risk for ATE, VTE or pancreatitis compared to women without known (more...)
GRADE table 3
(Question 3): Among women with known dyslipidaemias without other known cardiovascular risk factors, does combined hormonal contraception (CHC) use increase risk of worsening lipid abnormalities compared with no CHC use? (Indirect evidence).
References
- 1.
- Tanis BC, van den Bosch MA, Kemmeren JM, Cats VM, Helmerhorst FM, Algra A, et al. Oral contraceptives and the risk of myocardial infarction. N Engl J Med. 2001;345(25):1787–93. [PubMed: 11752354]
- 2.
- Gronich N, Lavi I, Rennert G. Higher risk of venous thrombosis associated with drospirenone-containing oral contraceptives: a population-based cohort study. CMAJ. 2011;183(18):E1319–25. [PMC free article: PMC3255137] [PubMed: 22065352]
- 3.
- Runnebaum B, Grunwald K, Rabe T. The efficacy and tolerability of norgestimate/ethinyl estradiol (250 micrograms of norgestimate/35 micrograms of ethinyl estradiol): results of an open, multicenter study of 59,701 women. Am J Obstet Gynecol. 1992;166(6 Pt 2):1963–8. [PubMed: 1605286]
6. Recommendations for progestogen-only contraceptives and levonorgestrel-releasing intrauterine devices among breastfeeding women
Question 1: Among breastfeeding women (and their infants), does the use of progestogen-only contraceptives (POCs) and levonorgestrel-releasing intrauterine devices (LNG-IUDs) have an impact on breastfeeding or infant health outcomes compared with those not using POCs? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among breastfeeding women (and their infants), does the use of progestogen-only contraceptives (POCs) and levonorgestrel-releasing intrauterine devices (LNG-IUDs) initiated up to 6 weeks postpartum have an impact on breastfeeding or infant health outcomes compared with initiation after 6 weeks postpartum? (Direct evidence)
Table
Selection criteria for the systematic review.
6a. Recommendations for use of progestogen-only contraceptives (pills, injectables, implants)
< 6 weeks postpartum
- Breastfeeding women who are < 6 weeks postpartum can generally use progestogen-only pills (POPs), and levonorgestrel (LNG) and etonogestrel (ETG) implants (MEC Category 2).
- Breastfeeding women who are < 6 weeks postpartum generally should not use progestogen-only injectables (DMPA/NET-EN) (MEC Category 3). There is theoretical concern about the potential exposure of the neonate to DMPA/NET-EN during the first 6 weeks postpartum. However, in many settings pregnancy-related morbidity and mortality risks are high, and access to services is limited. In such settings, DMPA/NET-EN may be one of the few types of methods widely available and accessible to breastfeeding women immediately postpartum.
≥ 6 weeks to < 6 months postpartum
- Breastfeeding women who are 6 weeks to < 6 months postpartum can use without restriction the following contraceptive methods: POPs, progestogen-only injectables (DMPA and NET-EN), and LNG and ETG implants (MEC Category 1).
≥ 6 months postpartum
- Breastfeeding women who are ≥ 6 months postpartum can use without restriction the following contraceptive methods: POPs, progestogen-only injectables (DMPA and NET-EN), and LNG and ETG implants (MEC Category 1).
6b. Recommendations for use of levonorgestrel-releasing intrauterine devices (LNG-IUDs)
< 48 hours postpartum
- Breastfeeding women who are < 48 hours postpartum can generally use LNG-IUDs (MEC Category 2).
≥ 48 hours to < 4 weeks postpartum
- Breastfeeding (and non-breastfeeding) women generally should not have an LNG-IUD inserted from 48 hours to < 4 weeks postpartum (MEC Category 3).
≥ 4 weeks postpartum
- Breastfeeding (and non-breastfeeding) women can use an LNG-IUD without restriction at ≥ 4 weeks postpartum (MEC Category 1).
Puerperal sepsis
- Breastfeeding (and non-breastfeeding) women with puerperal sepsis should not have an LNG-IUD inserted (MEC Category 4).
Remarks
- Animal data suggest an effect of progesterone on the developing brain; whether similar effects occur following progestogen exposure in humans is unclear (1–3). Available data from clinical and observational trials do not suggest an increased risk for either breastfeeding performance or infant health outcomes with use of progestogen-only injectables compared to outcomes in studies using other progestogen-only methods (4–8). However, the Guideline Development Group felt that, as infants in the first 6 weeks of life may be exposed to higher hormone levels with use of progestogen-only injectables, as compared to the exposure using other methods of progestogen-only contraceptives (POCs), the theoretical risks of progestogen-only injectables may outweigh the benefits, particularly in settings with access to a wide variety of contraceptive methods.
- Due to heterogeneity of study designs, contraceptive methods/formulations and outcome measures, a meta-analysis was not performed.
- POCs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Forty-seven articles reporting on 45 different studies were identified in the systematic review that investigated the use of POCs in breastfeeding women and reported clinically relevant outcomes of infant growth, health or breastfeeding performance. Direct evidence demonstrates no effect of POCs on breastfeeding performance (4–51), and generally demonstrates no harmful effects on infant growth, health or development (6, 7, 28, 42). However, these studies have been inadequately designed to determine whether a risk of long-term effects exists.
One randomized trial found that immediate insertion of the LNG-IUD was associated with decreased breastfeeding duration compared with delayed insertion (5). Two other randomized controlled trials assessing early versus delayed initiation of POCs failed to show a difference in breastfeeding outcomes (4, 16). In other studies, initiation of LNG-IUD after 4 weeks postpartum demonstrated no detrimental effect on breastfeeding outcomes (11, 13, 45).
Quality of the evidence
< 6 weeks postpartum:
Breastfeeding outcomes
Table
Progestogen-only pills (POPs).
Table
Progestogen-only injectables (DMPA/NET-EN).
Table
Progestogen-containing implants.
Table
LNG-IUD.
Infant outcomes
Table
POPs.
Table
Progestogen-only injectables (DMPA/NET-EN).
Table
Progestogen-containing implants.
Table
LNG-IUD.
≥ 6 weeks postpartum:
Breastfeeding outcomes
Table
POPs.
Table
Progestogen-only injectables (DMPA/NET-EN).
Table
Progestogen-containing implants.
Table
LNG-IUD.
Infant outcomes
Table
POPs.
Table
Progestogen-only injectables (DMPA/NET-EN).
Table
Progestogen-containing implants.
Table
LNG-IUD.
GRADE table 1
(Question 1): Among breastfeeding women (and their infants), does the use of progestogen-only contraceptives (POCs) and levonorgestrel-releasing intrauterine devices (IUDs) have an impact on breastfeeding or infant health outcomes compared with those (more...)
References
- 1.
- Quadros PS, Pfau JL, Wagner CK. Distribution of progesterone receptor immunoreactivity in the fetal and neonatal rat forebrain. J Comp Neurol. 2007;504(1):42–56. [PubMed: 17614295]
- 2.
- Wagner CK. The many faces of progesterone: a role in adult and developing male brain. Front Neuroendocrinol. 2006;27(3):340–59. [PubMed: 17014900]
- 3.
- Wagner CK. Progesterone receptors and neural development: a gap between bench and bedside? Endocrinology. 2008;149(6):2743–9. [PMC free article: PMC2408811] [PubMed: 18308849]
- 4.
- Brito MB, Ferriani RA, Quintana SM, Yazlle ME, Silva de S MF, Vieira CS. Safety of the etonogestrel-releasing implant during the immediate postpartum period: a pilot study. Contraception. 2009;80(6):519–26. [PubMed: 19913145]
- 5.
- Chen BA, Reeves MF, Creinin MD, Schwarz EB. Postplacental or delayed levonorgestrel intrauterine device insertion and breast-feeding duration. Contraception. 2011;84(5):499–504. [PMC free article: PMC3202348] [PubMed: 22018124]
- 6.
- Dahlberg K. Some effects of depo-medroxyprogesterone acetate (DMPA): observations in the nursing infant and in the long-term user. Int J Gynaecol Obstet. 1982;20(1):43–8. [PubMed: 6126406]
- 7.
- Karim M, Ammar R, el-Mahgoub S, el-Ganzoury B, Fikri F, Abdou I. Injected progestogen and lactation. Br Med J. 1971;1(5742):200–3. [PMC free article: PMC1794828] [PubMed: 5099971]
- 8.
- Matias SL, Nommsen-Rivers LA, Dewey KG. Determinants of exclusive breastfeeding in a cohort of primiparous periurban peruvian mothers. J Hum Lact. 2012;28(1):45–54. [PubMed: 22058120]
- 9.
- Progestogen-only contraceptives during lactation: I. Infant growth. World Health Organization Task force for Epidemiological Research on Reproductive Health; Special Programme of Research, Development and Research Training in Human Reproduction. Contraception. 1994;50(1):35–53. [PubMed: 7924321]
- 10.
- McEwan JA, Joyce DN, Tothill AU, Hawkins DF. Early experience in contraception with a new progestogen. Contraception. 1977;16(4):339–50. [PubMed: 923246]
- 11.
- Bahamondes L, Bahamondes MV, Modesto W, Tilley IB, Magalhaes A, Pinto e Silva JL, et al. Effect of hormonal contraceptives during breastfeeding on infant's milk ingestion and growth. Fertil Steril. 2013;100(2):445–50. [PubMed: 23623474]
- 12.
- Brownell EA, Fernandez ID, Fisher SG, Howard CR, Ternullo SR, Lawrence RA, et al. The effect of immediate postpartum depot medroxyprogesterone on early breastfeeding cessation. Contraception. 2013;87(6):836–43. [PMC free article: PMC4038903] [PubMed: 23153897]
- 13.
- Costa ML, Cecatti JG, Krupa FG, Rehder PM, Sousa MH, Costa-Paiva L. Progestin-only contraception prevents bone loss in postpartum breastfeeding women. Contraception. 2012;85(4):374–80. [PubMed: 22036473]
- 14.
- Diaz S, Reyes MV, Zepeda A, Gonzalez GB, Lopez JM, Campino C, et al. Norplant((R)) implants and progesterone vaginal rings do not affect maternal bone turnover and density during lactation and after weaning. Hum Reprod. 1999;14(10):2499–505. [PubMed: 10527977]
- 15.
- Espey E, Ogburn T, Leeman L, Singh R, Ostrom K, Schrader R. Effect of progestin compared with combined oral contraceptive pills on lactation: a randomized controlled trial. Obstet Gynecol. 2012;119(1):5–13. [PMC free article: PMC3586805] [PubMed: 22143258]
- 16.
- Gurtcheff SE, Turok DK, Stoddard G, Murphy PA, Gibson M, Jones KP. Lactogenesis after early postpartum use of the contraceptive implant: a randomized controlled trial. Obstet Gynecol. 2011;117(5):1114–21. [PubMed: 21508750]
- 17.
- Kamal I, Hefnawi F, Ghoneim M, Talaat M, Younis N, Tagui A, et al. Clinical, biochemical, and experimental studies on lactation. II. Clinical effects of gestagens on lactation. Am J Obstet Gynecol. 1969;105(3):324–34. [PubMed: 5810783]
- 18.
- Pardthaisong T, Yenchit C, Gray R. The long-term growth and development of children exposed to Depo-Provera during pregnancy or lactation. Contraception. 1992;45(4):313–24. [PubMed: 1387602]
- 19.
- Zanartu J, Aguilera E, Munoz G, Peliowsky H. Effect of a long-acting contraceptive progestogen on lactation. Obstet Gynecol. 1976;47(2):174–6. [PubMed: 943074]
- 20.
- Abdel-Aleem H, Abol-Oyoun el SM, Shaaban MM, el-Saeed M, Shoukry M, Makhlouf A, et al. The use of nomegestrol acetate subdermal contraceptive implant, uniplant, during lactation. Contraception. 1996;54(5):281–6. [PubMed: 8934061]
- 21.
- Abdulla KA, Elwan SI, Salem HS, Shaaban MM. Effect of early postpartum use of the contraceptive implants, NORPLANT, on the serum levels of immunoglobulins of the mothers and their breastfed infants. Contraception. 1985;32(3):261–6. [PubMed: 3936675]
- 22.
- Affandi B, Karmadibrata S, Prihartono J, Lubis F, Samil RS. Effect of Norplant on mothers and infants in the postpartum period. Adv Contracept. 1986;2(4):371–80. [PubMed: 3105266]
- 23.
- Baheiraei A, Ardsetani N, Ghazizadeh S. Effects of progestogen-only contraceptives on breast-feeding and infant growth. Int J Gynaecol Obstet. 2001;74(2):203–5. [PubMed: 11502302]
- 24.
- Bjarnadottir RI, Gottfredsdottir H, Sigurdardottir K, Geirsson RT, Dieben TO. Comparative study of the effects of a progestogen-only pill containing desogestrel and an intrauterine contraceptive device in lactating women. BJOG. 2001;108(11):1174–80. [PubMed: 11762658]
- 25.
- Coutinho EM, Athayde C, Dantas C, Hirsch C, Barbosa I. Use of a single implant of elcometrine (ST-1435), a nonorally active progestin, as a long acting contraceptive for postpartum nursing women. Contraception. 1999;59(2):115–22. [PubMed: 10361626]
- 26.
- Croxatto HB, Dìaz S, Peralta O, Juez G, Casado ME, Salvatierra AM, et al. Fertility regulation in nursing women. II. Comparative performance of progesterone implants versus placebo and copper T. Am J Obstet Gynecol. 1982;144(2):201–8. [PubMed: 7114130]
- 27.
- Diaz S, Herreros C, Juez G, Casado ME, Salvatierra AM, Miranda P, et al. Fertility regulation in nursing women: VII. Influence of NORPLANT levonorgestrel implants upon lactation and infant growth. Contraception. 1985;32(1):53–74. [PubMed: 3931973]
- 28.
- Dìaz S, Peralta O, Juez G, Herreros C, Casado ME, Salvatierra AM, et al. Fertility regulation in nursing women. VI. Contraceptive effectiveness of a subdermal progesterone implant. Contraception. 1984;30(4):311–25. [PubMed: 6509984]
- 29.
- Diaz S, Zepeda A, Maturana X, Reyes MV, Miranda P, Casado ME, et al. Fertility regulation in nursing women. IX. Contraceptive performance, duration of lactation, infant growth, and bleeding patterns during use of progesterone vaginal rings, progestin-only pills, Norplant implants, and Copper T 380-A intrauterine devices. Contraception. 1997;56(4):223–32. [PubMed: 9408703]
- 30.
- Giner Velazquez J, Cortes Gallegos V, Sotelo Lopez A, Bondani G. [Effect of daily oral administration of 0.350 mg of norethindrone on lactation and on the composition of milk]. Ginecol Obstet Mex. 1976;40(237):31–9. [PubMed: 780215]
- 31.
- Guiloff E, Ibarra-Polo A, ZaÒartu J, Toscanini C, Mischler TW, GÛmez-Rogers C. Effect of contraception on lactation. Am J Obstet Gynecol. 1974;118(1):42–5. [PubMed: 4128673]
- 32.
- Halderman LD, Nelson AL. Impact of early postpartum administration of progestin-only hormonal contraceptives compared with nonhormonal contraceptives on short-term breast-feeding patterns. Am J Obstet Gynecol. 2002;186(6):1250–6. discussion 6–8. [PubMed: 12066106]
- 33.
- Hannon PR, Duggan AK, Serwint JR, Vogelhut JW, Witter F, DeAngelis C. The influence of medroxyprogesterone on the duration of breast-feeding in mothers in an urban community. Arch Pediatr Adolesc Med. 1997;151(5):490–6. [PubMed: 9158442]
- 34.
- Heikkila M, Luukkainen T. Duration of breast-feeding and development of children after insertion of a levonorgestrel-releasing intrauterine contraceptive device. Contraception. 1982;25(3):279–92. [PubMed: 6804164]
- 35.
- Jimenez J, Ochoa M, Soler MP, Portales P. Long-term follow-up of children breast-fed by mothers receiving depot-medroxyprogesterone acetate. Contraception. 1984;30(6):523–33. [PubMed: 6241560]
- 36.
- Kamal I, Hefnawi F, Ghoneim M, Abdallah M, Abdel Razek S. Clinical, biochemical, and experimental studies on lactation. V. Clinical effects of steroids on the initiation of lactation. Am J Obstet Gynecol. 1970;108(4):655–8. [PubMed: 4918514]
- 37.
- Massai MR, Dìaz S, Quinteros E, Reyes MV, Herreros C, Zepeda A, et al. Contraceptive efficacy and clinical performance of Nestorone implants in postpartum women. Contraception. 2001;64(6):369–76. [PubMed: 11834236]
- 38.
- McCann MF, Moggia AV, Higgins JE, Potts M, Becker C. The effects of a progestin-only oral contraceptive (levonorgestrel 0.03 mg) on breast-feeding. Contraception. 1989;40(6):635–48. [PubMed: 2515939]
- 39.
- Moggia AV, Harris GS, Dunson TR, Diaz R, Moggia MS, Ferrer MA, et al. A comparative study of a progestin-only oral contraceptive versus non-hormonal methods in lactating women in Buenos Aires, Argentina. Contraception. 1991;44(1):31–43. [PubMed: 1893700]
- 40.
- Reinprayoon D, Taneepanichskul S, Bunyavejchevin S, Thaithumyanon P, Punnahitananda S, Tosukhowong P, et al. Effects of the etonogestrel-releasing contraceptive implant (Implanon on parameters of breastfeeding compared to those of an intrauterine device. Contraception. 2000;62(5):239–46. [PubMed: 11172794]
- 41.
- Schiappacasse V, Diaz S, Zepeda A, Alvarado R, Herreros C. Health and growth of infants breastfed by Norplant contraceptive implants users: a six-year follow-up study. Contraception. 2002;66(1):57–65. [PubMed: 12169382]
- 42.
- Seth U, Yadava HS, Agarwal N, Laumas KR, Hingorani V. Effect of a subdermal silastic implant containing norethindrone acetate on human lactation. Contraception. 1977;16(4):383–98. [PubMed: 923249]
- 43.
- Shaaban MM. Contraception with progestogens and progesterone during lactation. J Steroid Biochem Mol Biol. 1991;40(4–6):705–10. [PubMed: 1835650]
- 44.
- Shaaban MM, Salem HT, Abdullah KA. Influence of levonorgestrel contraceptive implants, NORPLANT, initiated early postpartum upon lactation and infant growth. Contraception. 1985;32(6):623–35. [PubMed: 3937665]
- 45.
- Shaamash AH, Sayed GH, Hussien MM, Shaaban MM. A comparative study of the levonorgestrel-releasing intrauterine system Mirena versus the Copper T380A intrauterine device during lactation: breast-feeding performance, infant growth and infant development. Contraception. 2005;72(5):346–51. [PubMed: 16246660]
- 46.
- Shikary ZK, Betrabet SS, Toddywala WS, Patel DM, Datey S, Saxena BN. Pharmacodynamic effects of levonorgestrel (LNG) administered either orally or subdermally to early postpartum lactating mothers on the urinary levels of follicle stimulating hormone (FSH), luteinizing hormone (LH) and testosterone (T) in their breast-fed male infants. Contraception. 1986;34(4):403–12. [PubMed: 3096635]
- 47.
- Taneepanichskul S, Reinprayoon D, Thaithumyanon P, Praisuwanna P, Tosukhowong P, Dieben T. Effects of the etonogestrel-releasing implant Implanon and a nonmedicated intrauterine device on the growth of breast-fed infants. Contraception. 2006;73(4):368–71. [PubMed: 16531169]
- 48.
- Tankeyoon M, Dusitsin N, Chalapati S, Koetsawang S, Saibiang S, Sas M, et al. Effects of hormonal contraceptives on milk volume and infant growth. WHO Special Programme of Research, Development and Research Training in Human Reproduction Task force on oral contraceptives. Contraception. 1984;30(6):505–22. [PubMed: 6241559]
- 49.
- West CP. The acceptability of a progestagen-only contraceptive during breast-feeding. Contraception. 1983;27(6):563–9. [PubMed: 6617204]
- 50.
- Zacharias S, Aguilera E, Assenzo JR, Zanartu J. Effects of hormonal and nonhormonal contraceptives on lactation and incidence of pregnancy. Contraception. 1986;33(3):203–13. [PubMed: 2941236]
- 51.
- Zanartu J, Aguilera E, Munoz-Pinto G. Maintenance of lactation by means of continuous low-dose progestogen given post-partum as a contraceptive. Contraception. 1976;13(3):313–8. [PubMed: 55332]
7. Recommendations for safety of depot medroxyprogesterone acetate delivered subcutaneously
Question 1: What is the safety of depot medroxyprogesterone acetate (104 mg/0.65 mL) delivered subcutaneously (DMPA-SC) for women with medical conditions or other specific characteristics established within the World Health Organization's eligibility criteria for contraceptive use? (Direct evidence)
A
Selection criteria for the systematic review.
B
Selection criteria for the systematic review.
Question 2: Among healthy women or among a general population of women of reproductive age, do those who use depot medroxyprogesterone acetate (104 mg/0.65 mL) delivered subcutaneously (DMPA-SC) have an increased risk for serious adverse events or other relevant outcomes compared with those who use DMPA delivered intramuscularly (DMPA-IM)? (Indirect evidence)
Table
Selection criteria for the systematic review.
Recommendations
Age
- Young women (menarche to < 18 years) can generally use DMPA (MEC Category 2).
- Women between the ages of 18 and 45 years can use DMPA without restriction (MEC Category 1)
- Women > 45 years old can generally use DMPA (MEC Category 2).
Endometriosis
- Women with endometriosis can use DMPA without restriction (MEC Category 1).
HIV
- Women living with HIV who have asymptomatic or mild clinical disease (WHO stage 1 or 2) can use DMPA without restriction (MEC Category 1).
- Women living with HIV who have severe or advanced HIV clinical disease (WHO stage 3 or 4) can use DMPA without restriction (MEC Category 1).
Obesity
- Women with a body mass index (BMI) ≥ 30 kg/m2 can use DMPA without restriction (MEC Category 1).
- Young women (menarche to < 18 years) with a BMI ≥ 30 kg/m2 can generally use DMPA (MEC Category 2).
- There is evidence for differential weight gain among normal-weight and obese adolescents who use DMPA, but not those using norethisterone enanthate (NET-EN). However, NET-EN is MEC Category 2 due to evidence regarding potential effects of NET-EN on bone mineral density among adolescents.
Remarks
- The Guideline Development Group determined that no change to the existing recommendations for DMPA was warranted with inclusion of DMPA-SC as a new method.
- The body of evidence evaluating use of DMPA-SC and DMPA-IM among healthy women of reproductive age suggests a similar safety profile. Due to heterogeneity of study designs and outcome measures, a meta-analysis was not performed.
- DMPA-SC does not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
A randomized trial evaluating changes in bone mineral density (BMD) among adult DMPA-SC and IM users demonstrated no differences at two years of follow-up (1). Limited evidence from three Phase 3 contraceptive trials reported no consistent differences in weight change or bleeding patterns according to age; adolescents aged < 18 years were not included in any studies (1–3). Two prospective, non-comparative studies demonstrated that women with endometriosis treated with DMPA-SC for six months experienced minimal weight gain and decreases in BMD; serious adverse events were rare and DMPA-SC improved pain symptoms associated with the condition (4, 5). A randomized cross-over study reported that women living with HIV tolerated injection of DMPA-SC and that experiences of serious adverse events were rare and occurred at similar rates as in users of DMPA-IM (6). Evidence from three Phase 3 contraceptive trials and four reports from a small prospective cohort study reported similar contraceptive efficacy, weight change, bleeding patterns and other adverse effects, including variations in a number of biomarkers, among obese and non-obese DMPA-SC users (1, 3, 7–12).
DMPA-IM and DMPA-SC appear to be therapeutically equivalent; the two formulations demonstrate similar pharmacokinetics, effects on serum estradiol levels and high contraceptive efficacy (1). In addition, similar effects on weight change, bleeding patterns and experience of other adverse effects have been reported among healthy reproductive age users (1, 3, 13).
Quality of the evidence
GRADE table 1
(Question 1): What is the safety of depot medroxyprogesterone acetate (104 mg/0.65 mL) delivered subcutaneously (DMPA-SC) for women with medical conditions or other specific characteristics established within the World Health Organization's eligibility (more...)
GRADE table 2
(Question 2): Among healthy women or among a general population of women of reproductive age, do those who use depot medroxyprogesterone acetate (104 mg/0.65 mL) delivered subcutaneously (DMPA-SC) have an increased risk for serious adverse events or other (more...)
References
- 1.
- Kaunitz AM, Darney PD, Ross D, Wolter KD, Speroff L. Subcutaneous DMPA vs. intramuscular DMPA: a 2-year randomized study of contraceptive efficacy and bone mineral density. Contraception. 2009;80(1):7–17. [PubMed: 19501210]
- 2.
- Arias RD, Jain JK, Brucker C, Ross D, Ray A. Changes in bleeding patterns with depot medroxyprogesterone acetate subcutaneous injection 104 mg. Contraception. 2006;74(3):234–8. [PubMed: 16904417]
- 3.
- Westhoff C, Jain JK, Milsom I, Ray A. Changes in weight with depot medroxyprogesterone acetate subcutaneous injection 104 mg/0.65 mL. Contraception. 2007;75(4):261–7. [PubMed: 17362703]
- 4.
- Crosignani PG, Luciano A, Ray A, Bergqvist A. Subcutaneous depot medroxyprogesterone acetate versus leuprolide acetate in the treatment of endometriosis-associated pain. Hum Reprod. 2006;21(1):248–56. [PubMed: 16176939]
- 5.
- Schlaff WD, Carson SA, Luciano A, Ross D, Bergqvist A. Subcutaneous injection of depot medroxyprogesterone acetate compared with leuprolide acetate in the treatment of endometriosis-associated pain. Fertil Steril. 2006;85(2):314–25. [PubMed: 16595206]
- 6.
- Polis CB, Nakigozi GF, Nakawooya H, Mondo G, Makumbi F, Gray RH, et al. Preference for Sayana® Press versus intramuscular Depo-Provera among HIV-positive women in Rakai, Uganda: a randomized crossover trial. Contraception. 2014;89(5):385–95. [PubMed: 24332432]
- 7.
- Jain J, Dutton C, Nicosia A, Wajszczuk C, Bode FR, Mishell DR Jr. Pharmacokinetics, ovulation suppression and return to ovulation following a lower dose subcutaneous formulation of Depo-Provera. Contraception. 2004;70(1):11–8. [PubMed: 15208047]
- 8.
- Jain J, Jakimiuk AJ, Bode FR, Ross D, Kaunitz AM. Contraceptive efficacy and safety of DMPA-SC. Contraception. 2004;70(4):269–75. [PubMed: 15451329]
- 9.
- Segall-Gutierrez P, Taylor D, Liu X, Stanzcyk F, Azen S, Mishell DR Jr. Follicular development and ovulation in extremely obese women receiving depomedroxyprogesterone acetate subcutaneously. Contraception. 2010;81(6):487–95. [PubMed: 20472115]
- 10.
- Segall-Gutierrez P, Du J, Niu C, Ge M, Tilley I, Mizraji K, et al. Effect of subcutaneous depo-medroxyprogesterone acetate (DMPA-SC) on serum androgen markers in normal-weight, obese, and extremely obese women. Contraception. 2012;86(6):739–45. [PubMed: 22959905]
- 11.
- Segall-Gutierrez P, Xiang AH, Watanabe RM, Trigo E, Stanczyk FZ, Liu X, et al. Deterioration in cardiometabolic risk markers in obese women during depot medroxyprogesterone acetate use. Contraception. 2012;85(1):36–41. [PubMed: 22067800]
- 12.
- Segall-Gutierrez P, Agarwal R, Ge M, Lopez C, Hernandez G, Stanczyk FZ. A pilot study examining short-term changes in bone mineral density among class 3 obese users of depot-medroxyprogesterone acetate. Eur J Contracept Reprod Health Care. 2013;18(3):199–205. [PubMed: 23530919]
- 13.
- Goldstein J, Cushman M, Badger GJ, Johnson JV. Effect of depomedroxyprogesterone acetate on coagulation parameter: a pilot study. Fertil Steril. 2007;87(6):1267–70. [PubMed: 17336967]
8. Recommendations for safety of Sino-implant (II)
Question 1: What is the safety of the contraceptive implant Sino-implant (II) for women with medical conditions established within the World Health Organization's eligibility criteria for contraceptive use? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among healthy women or among a general population of women of reproductive age, do those who use Sino-implant (II) have an increased risk for serious adverse events or other relevant outcomes compared with those who do not use Sino-implant (II)? (Indirect evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Recommendations for Sino-implant (II) will be the same recommendations as for other levonorgestrel implants (see p. 143–158).
Remarks
- Although there was no direct evidence regarding Sino-implant (II) among women with medical conditions, studies were identified that looked at safety of the implant among healthy women compared to those who do not use the SI (II). In addition, the safety data from studies of other levonorgestrel (LNG) implants among women with medical conditions is used due to the similarity of SI (II) and other LNG implants in hormone formulation, quality profile and daily release rates. Given this, the panel decided to make the same recommendations for SI (II) as the other LNG implants. Due to heterogeneity of study designs and outcome measures, a meta-analysis was not performed.
- The Sino-implant (II) does not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
No studies were identified that provided direct evidence on the use of the Sino-implant (II) among women with medical conditions in the MEC that included a comparison group. When looking at the studies on healthy women, evidence from four studies comparing SI (II) users with users of other LNG-containing implants demonstrates that SI (II) has a similar safety profile with no significant differences in serious adverse events such as ectopic pregnancy or discontinuation due to medical problems (1–3).
When investigating serious adverse events in healthy women using SI (II), three articles were identified (1–3). These three articles reported on four randomized controlled trials (RCTs) and found no difference between users of SI (II) and users of SI (I) or Norplant with respect to incidence of serious adverse events. Similar effects on selected markers of disease in healthy women were seen for healthy women using SI (II) compared to women using SI (I) or Norplant. These markers of disease were liver function (3), weight (1, 4–6), blood pressure (1, 6), bone mineral density (7), ovarian cysts and benign myomas (6). Two studies provided limited evidence regarding menorrhagia (1, 8). The studies suggest that SI (II) is not harmful and may be beneficial for women with menorrhagia. One RCT found an increased pregnancy rate among women weighing 70 kg or over using SI (II) (9), while another RCT failed to find this association and also reported no association between duration of use, weight and pregnancy (3).
Quality of the evidence
Table
Women with medical conditions or other specific characteristics. (intervention versus comparator; outcome)
Table
Healthy women or general population of reproductive age women. (intervention versus comparator; outcome)
GRADE table 1
(Question 2): Among healthy women or among a general population of women of reproductive age, do those who use Sino-implant (II) have an increased risk for serious adverse events or other relevant outcomes compared with those who do not use Sino-implant (more...)
References
- 1.
- Qi L, Liu J, Yu L, Ye L, Sun L, Liu K. Multicenter clinical study of two Sino-subdermal implants. Chinese J Fam Plann. 2002;79:87–95.
- 2.
- Fang K, Guan Y, Fan H, Gao E, Yang D, Xue L, et al. A multicentre study of CLa Implant and Sino-implant: expanded application (two-year follow-up). J Reproduc Contracep. 1997;8:101–10.
- 3.
- Fan H, Han L, Jiang J, Wu M, Chen B, Meng F, et al. A multicenter comparative clinical study of Sino-Levonorgestrel-Releasing Implants – No. I and No. II with Norplant. J Reprod Contracept. 2004;15:101–7.
- 4.
- Zhang G, Li Y, Ren L. A comparative study on the acceptability of China-made subdermal implants. J Reprod Med. 1998;7(2):12–16.
- 5.
- Ni F, Mei F, Bian C, Chai Y, Wang G, Li Y, et al. Effect of three types of subdermal implants on female body weight. Chinese J Fam Plann. 1998;5:210–1.
- 6.
- Liu X, Mao J, Li Y, Chen X, Wang Z, Jin Y, et al. The safety of Sino-implant II – 3 years clinical observation. Reprod Contracept. 2000;20:92–7.
- 7.
- Shen H, Han L, Fan H, Gong Q, Zhao J, Tan J, et al. The effects of long-acting contraceptive implants on bones of reproductive women. Chinese J Fam Plann. 1998;6:539–42.
- 8.
- Han L, Fan H, Gong Q, Xie Z, Meng F, Hong Y, et al. The effects of three types of long-acting subcutaneous implants on menstrual blood loss. Chinese J Fam Plann. 1998;6:250–3.
- 9.
- Xing Q, Guan Y, Yang D, Yang Z, Guan F, Li W, et al. A multicenter comparative clinical study of two types of Sino-implant. Chinese J Fam Plann. 2002;79:282–6.
9. Recommendations for use of emergency contraceptive pills, including adding the condition of obesity and the new method, ulipristal acetate
Question 1: Among women with certain characteristics or medical conditions, are those who use levonorgestrel (LNG), ulipristal acetate (UPA) or combined oral contraceptive (COC) regimens for emergency contraceptive pills (ECPs) at increased risk for adverse events compared with those who do not use these forms of emergency contraception? (Direct evidence)
Table
Selection criteria for the systematic review.
Question 2: Among women who use levonorgestrel (LNG), ulipristal acetate (UPA) or combined oral contraceptive (COC) regimens for emergency contraceptive pills (ECPs), are those with obesity at increased risk for adverse events or pregnancy compared with those who do not have obesity? (Direct evidence)
Table
Selection criteria for the systematic review.
Recommendations
- For pregnant women, emergency contraceptive pill (ECP) use is not applicable. Although this method is not indicated for a woman with a known or suspected pregnancy, there is no known harm to the woman, the course of her pregnancy, or the fetus if ECPs are accidentally used.
- Women who are breastfeeding can use COCs or LNG regimens for ECPs without restriction (MEC Category 1). Women who are breastfeeding can generally use UPA (MEC Category 2). Breastfeeding is not recommended for one week after taking UPA since it is excreted in breast-milk. Breast-milk should be expressed and discarded during that time (1).
- Women who have experienced past ectopic pregnancies can use COCs, LNG or UPA for ECPs without restriction (MEC Category 1).
- Women with history of severe cardiovascular disease, including ischaemic heart disease, cerebrovascular attack, or other thromboembolic conditions, can generally use COCs, LNG or UPA for ECPs (MEC Category 2).
- Women with migraines can generally use COCs, LNG or UPA for ECPs (MEC Category 2).
- Women with severe liver disease, including jaundice, can generally use COCs, LNG or UPA for ECPs (MEC Category 2).
- Women using CYP3A4 inducers (e.g. rifampicin, phenytoin, phenobarbital, carbamazepine, efavirenz, fosphenytoine, nevirapine, oxcarbazepine, primidone, rifabutin, St John's wort/Hypericum perforatum) can use COCs, LNG or UPA for ECPs without restriction (MEC Category 1). Strong CYP3A4 inducers may reduce the effectiveness of ECPs.
- There are no restrictions on repeated ECP use for COCs, LNG or UPA (MEC Category 1). Recurrent ECP use is an indication that the woman requires further counselling on other contraceptive options. Frequently repeated ECP use may be harmful for women with conditions classified as Category 2, 3 or 4 for use of combined hormonal contraceptives (CHCs) or progestogen-only contraceptives (POCs).
- There are no restrictions for use of COCs, LNG or UPA for ECPs in cases of rape (MEC Category 1).
- Women who are obese can use COCs, LNG or UPA for ECPs without restriction (MEC Category 1). ECPs may be less effective among women with BMI ≥ 30 kg/m2 than among women with BMI < 25 kg/m2. Despite this, there are no safety concerns.
Remarks
- Ulipristal acetate (UPA) was added as a new method to the MEC.
- The duration of use of ECPs is less than the duration of regular use of COCs or POPs and thus would be expected to have less clinical impact for women with history of severe cardiovascular complications, migraine or severe liver disease (including jaundice). There are no restrictions for the use of ECPs in cases of rape.
- The Guideline Development Group (GDG) decided to remove the condition “angina pectoris” from the MEC recommendations for ECPs. This condition does not appear elsewhere in the MEC and there was no evidence suggesting safety concerns for ECP use among women with angina pectoris.
- The GDG decided to change the term “history of severe cardiovascular complications” to “history of severe cardiovascular disease” to be more consistent with terminology used elsewhere in the MEC.
- According to labelling information, rifampicin markedly decreases UPA levels by 90% or more, which may decrease its efficacy (1). Theoretical concerns, therefore, extend to use of other CYP3A4 inducers as well as LNG and COCs, which have similar metabolic pathways to UPA.
- Due to heterogeneity of study designs and outcome measures, a meta-analysis was not performed.
- ECPs do not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Four direct studies examined LNG-ECP use among pregnant or breastfeeding women (2–5). No studies were identified that examined UPA- or COC-ECP use among women with medical conditions or characteristics. One cohort study and one randomized controlled trial analysed outcomes among breastfeeding women (3–4), and two cohort studies analysed outcomes among breastfeeding women (2, 5). Poor pregnancy outcomes appear rare among pregnant women who used ECPs during conception cycle or early in pregnancy. Breastfeeding outcomes do not seem to differ between women exposed to LNG and those unexposed. One pharmacokinetic study demonstrates that LNG does pass to breast-milk but is found in minimal quantities (6).
A small pharmacokinetic study found that concomitant efavirenz use decreased LNG levels in women taking LNG-ECP (0.75 mg) by 56% compared with LNG-ECP alone (7).
There is limited evidence from one study that suggests obese women with BMI ≥ 30 kg/m2 experience an increased risk of pregnancy after use of LNG compared with women with BMI < 25 kg/m2 (8). Evidence from two studies suggests that obese women may also experience an increased risk of pregnancy after use of UPA compared with non-obese women, though this increase was not significant in one of the studies (8, 9).
Quality of the evidence
Women with certain characteristics or medical conditions:
(intervention versus comparator; outcome)
Table
Breastfeeding women.
Table
Currently pregnant women.
GRADE methodology was not used to assess quality of evidence for studies that did not report clinical outcomes, including pharmacokinetic studies.
Women using LNG-, UPA- or COC-ECPs:
(intervention versus comparator: outome)
GRADE tables 1
(Question 1): Among women with certain characteristics or medical conditions, are those who use levonorgestrel (LNG), ulipristal acetate (UPA) or combined oral contraceptive (COC) regimens for emergency contraceptive pills (ECPs) at increased risk for (more...)
GRADE table 2
(Question 2): Among women who use levonorgestrel (LNG), ulipristal acetate (UPA) or combined oral contraceptive (COC) regimens for emergency contraceptive pills (ECPs), are those with obesity at increased risk for adverse events or pregnancy compared (more...)
References
- 1.
- ellaOne® ulipristal acetate. Abbreviated prescribing information (UK). London: HRA Pharma UK & Ireland Ltd; 2013. [23 October 2014]. http://www
.ellaone.co .uk/hcp/abbreviated-prescribing-information-uk. - 2.
- De Santis M, Cavaliere AF, Straface G, Carducci B, Caruso A. Failure of the emergency contraceptive levonorgestrel and the risk of adverse effects in pregnancy and on fetal development: an observational cohort study. Fertil Steril. 2005;84(2):296–9. [PubMed: 16084867]
- 3.
- Polakow-Farkash S, Gilad O, Merlob P, Stahl B, Yogev Y, Klinger G. Levonorgestrel used for emergency contraception during lactation-a prospective observational cohort study on maternal and infant safety. J Matern Fetal Neonatal Med. 2013;26(3):219–21. [PubMed: 22928541]
- 4.
- Shaaban OM, Hassen SG, Nour SA, Kames MA, Yones EM. Emergency contraceptive pills as a backup for lactational amenorrhea method (LAM) of contraception: a randomized controlled trial. Contraception. 2013;87(3):363–9. [PubMed: 22935323]
- 5.
- Zhang L, Chen J, Wang Y, Ren F, Yu W, Cheng L. Pregnancy outcome after levonorgestrel-only emergency contraception failure: a prospective cohort study. Hum Reprod. 2009;24(7):1605–11. [PubMed: 19336440]
- 6.
- Gainer E, Massai R, Lillo S, Reyes V, Forcelledo Ml, Caviedes R, et al. Levonorgestrel pharmacokinetics in plasma and milk of lactating women who take 1.5 mg for emergency contraception. Hum Reprod. 2007;22(6):1578–84. [PubMed: 17337471]
- 7.
- Carten ML, Kiser JJ, Kwara A, Mawhinney S, Cu-Uvin S. Pharmacokinetic interactions between the hormonal emergency contraception, levonorgestrel (Plan B), and Efavirenz. Infect Dis Obstet Gynecol. 2012;2012:1–4. [PMC free article: PMC3299227] [PubMed: 22536010]
- 8.
- Glasier A, Cameron ST, Blithe D, Scherrer B, Mathe H, Levy D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel. Contraception. 2011;84(4):363–7. [PubMed: 21920190]
- 9.
- Moreau C, Trussell J. Results from pooled Phase III studies of ulipristal acetate for emergency contraception. Contraception. 2012;86(6):673–80. [PMC free article: PMC3766836] [PubMed: 22770793]
10. Recommendations for intrauterine devices among women with increased risk for sexually transmitted infections
Question 1: Among women with an increased risk of sexually transmitted infections (STIs), does intrauterine device (IUD) insertion increase risk for pelvic inflammatory disease (PID) compared with women with an increased risk of STIs that do not undergo IUD insertion?
Table
Selection criteria for the systematic review.
Recommendations
- Many women with increased risk of sexually transmitted infections (STIs) can generally undergo either Cu-IUD or LNG-IUD initiation (MEC Category 2). Some women at increased risk (very high individual likelihood) of STIs generally should not have an IUD inserted until appropriate testing and treatment occur (MEC Category 3). IUD insertion may further increase the risk of PID among women at increased risk of STIs, although limited evidence suggests that this risk is low. Current algorithms for determining increased risk of STIs have poor predictive value. Risk of STIs varies by individual behaviour and local STI prevalence. Therefore, while many women at increased risk of STIs can generally have an IUD inserted, some women at increased risk (very high individual likelihood) of STIs should generally not have an IUD inserted until appropriate testing and treatment occur.
- Women at increased risk of STIs can generally continue use of either Cu-IUD or LNG-IUD (MEC Category 2).
Remarks
- The Guideline Review Committee advised that this recommendation be revised to clarify the Category 2/3 recommendation in the MEC fourth edition. However, as no new evidence was identified to update this recommendation, there was no evidence to take through the GRADE process. This was addressed by the Guideline Development Group (GDG), who decided that the best course of action was to revise the clarification. The GDG highlighted the universal recommendation for dual protection with condoms, especially for women at increased risk of STIs.
- IUDs do not protect against STIs, including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Using an algorithm to classify STI risk status among IUD users, one study reported that 11% of women at high risk of STI experienced IUD-related complications compared with 5% of those not classified as high risk (1). In another small study, the incidence of PID after IUD insertion was low (2.2%) in a cohort of women considered to be at high risk based on high background rates of STIs in the general population (2).
Quality of the evidence
References
- 1.
- Morrison CS, Sekadde-Kigondu C, Miller WC, Weiner DH, Sinei SK. Use of sexually transmitted disease risk assessment algorithms for selection of intrauterine device candidates. Contraception. 1999;59(2):97–106. [PubMed: 10361624]
- 2.
- Cropsey KL, Matthews C, Campbel S, Ivey S, Adawadkar S. Long-term, reversible contraception use among high-risk women treated in a university-based gynecology clinic: comparison between IUD and depo-provera. J Womens Health. 2010;19(2):349–53. [PubMed: 20109106]
11. Recommendations for use of progesterone-releasing vaginal ring
Question 1: Among breastfeeding women and their infants, does the use of the progesterone-releasing contraceptive vaginal ring (PVR), compared with non-use of progestogen-only contraceptive (POC) methods, affect maternal health, breastfeeding performance, infant growth or infant health? (Direct evidence)
Table
Selection criteria for the systematic review.
Recommendations
- Women who breastfeed and are ≥ 4 weeks postpartum, can use without restrictions the progesterone-releasing vaginal ring (PVR) (MEC Category 1). A woman who uses the PVR must be actively breastfeeding (e.g. at least four breastfeeding episodes per day) to maintain the efficacy of the method.
Remarks
- If the progesterone-releasing vaginal ring (PVR) is accidentally used during pregnancy, there is no known harm to the woman, the course of her pregnancy, or the fetus.
- Due to heterogeneity of study designs and outcome measures, a meta-analysis was not performed.
- The PVR does not protect against sexually transmitted infections (STIs), including HIV. If there is a risk of STI/HIV, the correct and consistent use of condoms is recommended. When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women is critical for upholding their reproductive rights. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence
Seven prospective cohort studies examined the effect of using the progesterone-releasing vaginal ring (PVR) on maternal health, breastfeeding performance, infant health and infant growth, compared with other hormonal and non-hormonal contraceptive methods, during the first year postpartum or longer (1–7).
Of the six studies that evaluated various measures of breastfeeding performance, neither duration of lactation (1, 4, 7), the proportion of women fully breastfeeding (2), the number of breastfeeding episodes (2, 5), nor the timing of supplementary food introduction (6) significantly differed among PVR users compared with users of non-hormonal or progestogen-only contraceptives (POCs) during 12 months of observation.
No statistically significant differences in infant weight gain were observed among PVR users compared with women using non-hormonal or POCs (3, 4, 6) and similar patterns of infant weight gain were observed in another study that compared PVR and IUD users (5). One study reported no significant difference in infant health (5).
Quality of the evidence
Table
Among breastfeeding women, use of PVR versus non-PVR contraceptive; various outcomes.
GRADE table 1
(Question 1): Among breastfeeding women and their infants, does the use of the progesterone-releasing contraceptive vaginal ring (PVR), compared with non-use of progestogen-only contraceptive (POC) methods, affect maternal health, breastfeeding performance, (more...)
References
- 1.
- Diaz S, Reyes MV, Zepeda A, Gonzalez GB, Lopez JM, Campino C, et al. Norplant® implants and progesterone vaginal rings do not affect maternal bone turnover and density during lactation and after weaning. Hum Reprod. 1999;14:2499–505. [PubMed: 10527977]
- 2.
- Massai R, Miranda P, Valdes P, Lavin P, Zepeda A, Casado ME, et al. Preregistration study on the safety and contraceptive efficacy of a progesterone-releasing vaginal ring in Chilean nursing women. Contraception. 1999;60:9–14. [PubMed: 10549447]
- 3.
- Chen JH, Wu SC, Shao WQ, MH Zou, J Hu, J Cong, et al. The comparative trial of TCu 380A IUD and progesterone-releasing vaginal ring used by lactating women. Contraception. 1998;57:371–9. [PubMed: 9693396]
- 4.
- Diaz S, Zepeda A, Maturana X, Reyes MV, Miranda P, Casado ME, et al. Fertility regulation in nursing women. IX. Contraceptive performance, duration of lactation, infant growth, and bleeding patterns during use of progesterone vaginal rings, progestin-only pills, Norplant® implants, and copper T380-A intrauterine devices. Contraception. 1997;56:223–32. [PubMed: 9408703]
- 5.
- Sivin I, Diaz S, Croxatto HB, Miranda P, Shaaban M, Sayed EH, et al. Contraceptives for lactationg women: A comparative trial of a progesterone-releasing vaginal ring and the copper T380A IUD. Contraception. 1997;55:225–32. [PubMed: 9179454]
- 6.
- Shaaban MM. Contraception with progestogens and progesterone during lactation. J Steriod Biochem Mol Biol. 1991;40:705–10. [PubMed: 1835650]
- 7.
- Diaz S, Jackanicz TM, Herreros C, Juez G, Peralta O, Miranda P, et al. Fertility regulation in nursing women: VIII. Progeseterone plasma levels and contraceptive efficacy of a progesterone-releasing vaginal ring. Contraception. 1985;32:603–22. [PubMed: 3912105]
12. Recommendations for use of hormonal contraception among women at high risk of HIV, women living with HIV, and women living with HIV using antiretroviral therapy
Background
Owing to the public health importance of recommendations on hormonal contraceptive use for women at risk of HIV and women living with HIV, the following recommendations were issued ahead of this fifth edition of the MEC in the document entitled Hormonal contraceptive methods for women at high risk of HIV and living with HIV: 2014 guidance statement, which was approved by the WHO Guidelines Review Committee (GRC) on 7 July 2014 (1).
Question 1: Does the use of a particular method of hormonal contraception directly increase the risk of HIV acquisition in women?
Table
Selection criteria for the systematic review.
Question 2: Does the use of various hormonal contraceptive methods accelerate HIV disease progression in women living with HIV?
Table
Selection criteria for the systematic review.
Question 3: Does the use of various hormonal contraceptive methods increase the risk of female-to-male HIV sexual transmission?
Table
Selection criteria for the systematic review.
Question 4: Are there any possible interactions between hormonal contraceptive methods and antiretroviral (ARV) medications?
Table
Selection criteria for the systematic review.
12a. Recommendations among women at high risk of HIV infection
- Women at high risk of acquiring HIV can use the following hormonal contraceptive methods without restriction: combined oral contraceptive pills (COCs), combined injectable contraceptives (CICs), contraceptive patches and rings, progestogen-only pills (POPs), progestogen-only injectables (DMPA and NET-EN), and levonorgestrel (LNG) and etonogestrel (ETG) implants (MEC Category 1).
- Women at high risk of HIV who are using progestogen-only injectables (POIs) should be informed that available studies on the association between POI contraception and HIV acquisition have important methodological limitations hindering interpretation. Some studies suggest that women using POI contraception may be at increased risk of HIV acquisition; other studies have not found this association. The public health impact of any such association would depend upon the local context, including rates of injectable contraceptive use, maternal mortality and HIV prevalence. This must be considered when adapting guidelines to local contexts. WHO expert groups continue to actively monitor any emerging evidence. At the meeting in 2014, as at the 2012 technical consultation, it was agreed that the epidemiological data did not warrant a change to the MEC. Given the importance of this issue, women at high risk of HIV infection should be informed that POIs may or may not increase their risk of HIV acquisition. Women and couples at high risk of HIV acquisition considering POIs should also be informed about and have access to HIV preventive measures, including male and female condoms.
- Women at high risk of acquiring HIV can generally use LNG-releasing IUDs (LNG-IUDs) (MEC Category 2).
Remarks
- It is critically important that women and couples at risk of HIV infection be informed about and have access to male and female condoms, and other measures to prevent and reduce their risk of HIV infection and sexually transmitted infections (STIs), regardless of which form of contraception they choose.
- Hormonal contraceptives, including COCs, CICs, POPs, POIs, progestogen-only implants, and LNG-IUDs do not protect against STIs/HIV.
Summary of the evidence (Question 1: HIV acquisition)
Twenty-two prospective observational studies have assessed the risk of HIV acquisition among women using a method of hormonal contraception versus the risk of HIV acquisition in women using a non-hormonal contraceptive method (i.e. condoms, Cu-IUD, withdrawal) or no contraceptive method (2–27).
Combined hormonal contraceptives
Eight studies assessed the use of COCs and were considered to be “informative but with important limitations” (28). Seven of these studies found no statistically significant association between use of COCs and HIV acquisition (3, 5-11), although one study among sex workers in Kenya did (12).
Progestogen-only contraceptives
Five studies assessed the use of NET-EN injectables and were considered to be “informative but with important limitations” (28). Four of them reported no statistically significant association with HIV acquisition (3, 8, 9, 13), while one did (11).
Nine studies assessed DMPA, or, if a DMPA-specific result was unavailable, assessed non-specified injectables; these studies were considered to be “informative but with important limitations” (28). The results were mixed: three of the studies showed a significant increase in risk (5, 11, 12), one showed a significant increase in risk using one statistical model but this association was not statistically significant using another statistical model (6, 7), and five showed no significant increase in risk (3, 8–10, 13).
Two studies assessed implants, one of which was classified as “unlikely to inform the primary question” (4, 28). Neither of these studies reported a statistically significant increased risk of HIV acquisition, but confidence intervals were wide (4, 21).
Quality of the evidence (Question 1: HIV acquisition)
12b. Recommendations among women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2)
- Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) can use the following hormonal contraceptive methods without restriction: combined oral contraceptive pills (COCs), combined injectable contraceptives (CICs), contraceptive patches and rings, progestogen-only pills (POPs), progestogen-only injectables (DMPA and NET-EN), and levonorgestrel (LNG) and etonogestrel (ETG) implants (MEC Category 1).
- Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) can generally use the LNG-IUD (MEC Category 2).
- Because there may be interactions between certain methods of hormonal contraception and certain antiretroviral medications (ARVs), refer to the recommendations on ART medication interactions (see p. 72).
Remarks
- Hormonal contraceptives do not protect against sexually transmitted infections (STIs), including HIV. Consistent and correct use of condoms, male or female, is critical for prevention of HIV transmission to non-infected sexual partners, and for protection against other STIs. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women living with HIV who wish to prevent pregnancy is critical for upholding their reproductive rights and continues to be an important strategy for reducing vertical HIV transmission. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence (Question 2: disease progression; Question 3: female-to-male transmission)
Two systematic reviews investigating Questions 2 and 3 informed the contraceptive eligibility recommendations for women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2).
Combined hormonal contraceptives (CHCs)
Out of eight available studies, seven suggested no association between use of COCs and progression of HIV, as measured by CD4 count < 200 cells/mm3, initiation of ART, or mortality (29–35). One randomized controlled trial found an increased risk of a composite outcome of declining CD4 count or death among COC users when compared with users of copper-bearing IUDs (Cu-IUDs) (36, 37).
Two prospective observational studies directly assessed the effects of different hormonal contraceptive methods on female-to-male HIV transmission by measuring seroconversions in male partners of women known to be using hormonal contraceptives. One of these studies reported an elevated, but not statistically significant, point estimate for COCs (5). The other study also did not find a statistically significant association for COCs (4).
Studies indirectly assessing the effect of various hormonal contraceptive methods on female-to-male HIV transmission by measuring genital viral shedding as a proxy for infectivity have had mixed results. The majority of indirect studies measuring whether various hormonal contraceptive methods affect plasma HIV viral load have found no effect (38–53).
Progestogen-only contraceptives (POCs)
Out of six available studies, five suggested no association between use of progestogen-only injectable (POI) contraceptives and progression of HIV, as measured by CD4 count < 200 cells/mm3, initiation of ART, or mortality (31–35). One randomized trial found an increased risk of a composite outcome of declining CD4 count or death among oral contraceptive (OC) users (COCs and POPs) when compared with users of Cu-IUDs; this study, however, had significant loss to follow-up and method-switching among groups, limiting its interpretation (36, 37). One study found no difference in ART initiation or CD4 count between users and non-users of the LNG-IUD (54).
Two prospective observational studies directly assessed the effects of different hormonal contraceptive methods on female-to-male HIV transmission by measuring seroconversions in male partners of women known to be using hormonal contraceptives. One study reported a statistically significant association between POI contraception and female-to-male transmission of HIV (5), while another study did not find a statistically significant association between use of DMPA and female-to-male HIV transmission (4). The findings of studies indirectly assessing the effect of various hormonal contraceptive methods on female-to-male HIV transmission by measuring genital viral shedding as a proxy for infectivity have been mixed. The majority of indirect studies measuring whether various hormonal contraceptive methods affect plasma HIV viral load have found no effect (38–53).
Quality of the evidence
12c. Recommendations among women living with severe or advanced HIV clinical disease (WHO stage 3 or 4)
- Women living with severe or advanced HIV clinical disease (WHO stage 3 or 4) can use the following hormonal contraceptive methods without restriction: combined oral contraceptive pills (COCs), combined injectable contraceptives (CICs), contraceptive patches and rings, preogestogen-only pills (POPs), progestogen-only injectables (DMPA and NET-EN), and levonorgestrel (LNG) and etonogestrel (ETG) implants (MEC Category 1).
- Women living with severe or advanced HIV clinical disease (WHO stage 3 or 4) should generally not initiate use of the LNG-IUD (MEC Category 3 for initiation) until their illness has improved to asymptomatic or mild HIV clinical disease (WHO stage 1 or 2). However, women who already have an LNG-IUD inserted and who develop severe or advanced HIV clinical disease need not have their IUD removed (MEC Category 2 for continuation). LNG-IUD users with severe or advanced HIV clinical disease should be closely monitored for pelvic infection.
- Because there may be interactions between certain methods of hormonal contraception and certain antiretroviral medications (ARVs), refer to the recommendations on ART medication interactions (see p. 72).
Remarks
- Hormonal contraceptives do not protect against sexually transmitted infections (STIs), including HIV. Consistent and correct use of condoms, male or female, is critical for prevention of HIV transmission to non-infected sexual partners, and for protection against other STIs. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women living with HIV who wish to prevent pregnancy is critical for upholding their reproductive rights and continues to be an important strategy for reducing vertical HIV transmission. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
Summary of the evidence (Question 2: disease progression; Question 3: female-to-male transmission)
Two systematic reviews investigating Questions 2 and 3 informed the contraceptive eligibility recommendations for women living with severe or advanced HIV clinical disease (WHO stage 3 or 4).
All of the identified studies excluded women with severe or advanced HIV clinical disease (WHO stage 3 or 4) from enrolment, although some participants experienced progression to severe or advanced disease during the trials.
Combined hormonal contraceptives (CHCs)
Out of eight available studies, seven suggest no association between use of COCs and progression of HIV, as measured by CD4 count < 200 cells/mm3, initiation of ART, or mortality (29–35). One randomized trial found an increased risk of a composite outcome of declining CD4 count or death among COC users when compared with users of copper-bearing IUDs (Cu-IUDs) (36, 37).
Two prospective observational studies directly assessed the effects of different hormonal contraceptive methods on female-to-male HIV transmission by measuring seroconversions in male partners of women known to be using hormonal contraceptives. One of these studies reported an elevated, but not statistically significant, point estimate for oral contraceptives (OCs) (5). The other study also did not find a statistically significant association for OCs (4).
Studies indirectly assessing the effect of various hormonal contraceptive methods on female-to-male HIV transmission by measuring genital viral shedding as a proxy for infectivity have had mixed results. The majority of indirect studies measuring whether various hormonal contraceptive methods affect plasma HIV viral load have found no effect (38–53).
Progestogen-only contraceptives (POCs), including LNG-IUD
Out of six available studies, five suggested no association between use of progestogen-only injectable contraceptives and progression of HIV, as measured by CD4 count < 200 cells/mm3, initiation of ART, or mortality (31–35). One randomized trial found an increased risk of a composite outcome of declining CD4 count or death among OC (COC and POP) users when compared with Cu-IUD users; this study, however, had significant loss to follow-up and method-switching among groups, limiting its interpretation (36, 37). One study found no difference in ART initiation or CD4 count between users and non-users of the LNG-IUD (54).
Two prospective observational studies directly assessed the effects of different hormonal contraceptive methods on female-to-male HIV transmission by measuring seroconversions in male partners of women with known hormonal contraceptive use status. One of these studies reported a statistically significant association between injectable contraception and female-to-male transmission of HIV (5), while the other study did not find a statistically significant association between use of DMPA and female-to-male HIV transmission (4).
The findings of studies indirectly assessing the effect of various hormonal contraceptive methods on female-to-male HIV transmission by measuring genital viral shedding as a proxy for infectivity have been mixed. The majority of indirect studies measuring whether various hormonal contraceptive methods affect plasma HIV viral load have found no effect (38–53).
Quality of the evidence
12d. Recommendations among women living with HIV using antiretroviral therapy (ART)
- Women taking any nucleoside/nucleotide reverse transcriptase inhibitor (NRTI) can use all hormonal contraceptive methods without restriction: combined oral contraceptive pills (COCs), contraceptive patches and rings, combined injectable contraceptives (CICs), progestogen-only pills (POPs), progestogen-only injectables (DMPA and NET-EN), and levonorgestrel (LNG) and etonogestrel (ETG) implants (MEC Category 1).
- Women using ART containing either efavirenz or nevirapine can generally use COCs, patches, rings, CICs, POPs, NET-EN and implants (MEC Category 2). However, women using efavirenz or nevirapine can use DMPA without restriction (MEC Category 1).
- Women using the newer non-nucleoside/nucleotide reverse transcriptase inhibitors (NNRTIs), etravirine and rilpivirine, can use all hormonal contraceptive methods without restriction (MEC Category 1).
- Women using protease inhibitors (e.g. ritonavir and ARVs boosted with ritonavir) can generally use COCs, contraceptive patches and rings, CICs, POPs, NET-EN, and LNG and ETG implants (MEC Category 2), and can use DMPA without restriction (MEC Category 1).
- Women using the integrase inhibitor raltegravir can use all hormonal contraceptive methods without restriction (MEC Category 1).
- Women using ARV medication can generally use LNG-IUDs (MEC Category 2), provided that their HIV clinical disease is asymptomatic or mild (WHO stage 1 or 2). Women living with severe or advanced HIV clinical disease (WHO stage 3 or 4) generally should not initiate use of the LNG-IUD (MEC Category 3 for initiation) until their illness has improved to asymptomatic or mild HIV clinical disease. However, women who already have an LNG-IUD inserted and who develop severe or advanced HIV clinical disease need not have their IUD removed (MEC Category 2 for continuation). LNG-IUD users with severe or advanced HIV clinical disease should be closely monitored for pelvic infection.
Remarks
- Hormonal contraceptives do not protect against sexually transmitted infections (STIs), including HIV. Consistent and correct use of condoms, male or female, is critical for prevention of HIV transmission to non-infected sexual partners, and for protection against other STIs. Female condoms are effective and safe, but are not used as widely by national programmes as male condoms.
- Voluntary use of contraception by women living with HIV who wish to prevent pregnancy is critical for upholding their reproductive rights and continues to be an important strategy for reducing vertical HIV transmission. All women have the right to evidence-based, comprehensive contraceptive information, education and counselling to ensure informed choice. Women's contraceptive choices are made in a particular time, societal and cultural context; choices are complex, multifactorial and subject to change. Decision-making for contraceptive methods usually requires the need to make trade-offs among the different methods, with advantages and disadvantages of specific contraceptive methods varying according to individual circumstances, perceptions and interpretations.
- Women living with HIV and using ARVs should discuss the potential impact of certain ARVs on contraceptive efficacy with their health-care provider.
Summary of the evidence (Question 4: hormonal contraception–ART interactions)
Nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs)
NRTIs do not appear to have significant risk of interactions with hormonal contraceptive methods (55, 56).
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
Three clinical studies, including one large study, found use of nevirapine-containing ART did not increase ovulation or pregnancy rates in women using COCs (57–60). For efavirenz-containing ART, a pharmacokinetic study showed consistent significant decreases in contraceptive hormone levels in women using COCs, and a small clinical study showed higher ovulation rates in women taking efavirenz-containing ART and COCs (57, 61, 62). Etravirine and rilpivirine do not interact with COCs (63, 64). One retrospective chart review of women using efavirenz-containing ART showed increased contraceptive failure rates for women using LNG implants (65). Based primarily on pharmacokinetic data, the effectiveness of DMPA is likely not affected by NNRTIs, and vice versa (66, 67).
Protease inhibitors (PIs)
Pharmacokinetic data suggest decreases in COC progestin levels with ritonavir and ritonavir-boosted PIs. In women using the patch, co-administration resulted in higher progestin levels (68). One study found higher progestin levels with concurrent PI use in users of POPs (69). Based primarily on pharmacokinetic data, the effectiveness of DMPA is likely not affected by PIs, and vice versa (66, 67).
Quality of the evidence
GRADE table 1
(Question 1): Does the use of a particular method of hormonal contraception directly increase the risk of HIV acquisition in women?
GRADE table 2
(Question 2): Does the use of various hormonal contraceptive methods accelerate HIV disease progression in women living with HIV?
GRADE table 3
(Question 3): Does the use of various hormonal contraceptive methods increase the risk of female-to-male HIV sexual transmission?
GRADE table 4
(Question 4): Are there any possible interactions between hormonal contraceptive methods and ARV medications?
References
- 1.
- Hormonal contraceptive methods for women at high risk for HIV and living with HIV: 2014 guidance statement. Geneva: World Health Organization; 2014. [PubMed: 26110193]
- 2.
- Heffron R, Rees H, Mugo N, Baeten JM. Use of hormonal contraceptives and risk of HIV-1 transmission - authors' reply. Lancet Infect Dis. 2012;12(7):510–1. [PubMed: 22742633]
- 3.
- McCoy SI, Zheng W, Montgomery ET, Blanchard K, van der Straten A, de Bruyn G, et al. Oral and injectable contraception use and risk of HIV acquisition among women in sub-Saharan Africa. AIDS. 2013;27(6):1001–9. [PubMed: 23698064]
- 4.
- Lutalo T, Musoke R, Kong X, Makumbi F, Serwadda D, Nalugoda F, et al. Effects of hormonal contraceptive use on HIV acquisition and transmission among HIV-discordant couples. AIDS. 2013;27 Suppl 1:S27–34. [PubMed: 24088681]
- 5.
- Heffron R, Donnell D, Rees H, Celum C, Mugo N, Were E, et al. Use of hormonal contraceptives and risk of HIV-1 transmission: a prospective cohort study. Lancet Infect Dis. 2012;12(1):19–26. [PMC free article: PMC3266951] [PubMed: 21975269]
- 6.
- Morrison CS, Chen PL, Kwok C, Richardson BA, Chipato T, Mugerwa R, et al. Hormonal contraception and HIV acquisition: reanalysis using marginal structural modeling. AIDS. 2010;24(11):1778–81. [PMC free article: PMC3148067] [PubMed: 20588106]
- 7.
- Morrison CS, Richardson BA, Mmiro F, Chipato T, Celentano DD, Luoto J, et al. Hormonal contraception and the risk of HIV acquisition. AIDS. 2007;21(1):85–95. [PubMed: 17148972]
- 8.
- Morrison CS, Skoler-Karpoff S, Kwok C, Chen PL, van de Wijgert J, Gehret-Plagianos M, et al. Hormonal contraception and the risk of HIV acquisition among women in South Africa. AIDS. 2012;26(4):497–504. [PubMed: 22156973]
- 9.
- Myer L, Denny L, Wright TC, Kuhn L. Prospective study of hormonal contraception and women's risk of HIV infection in South Africa. Int J Epidemiol. 2007;36(1):166–74. [PubMed: 17175547]
- 10.
- Reid SE, Dai JY, Wang J, Sichalwe BN, Akpomiemie G, Cowan FM, et al. Pregnancy, contraceptive use, and HIV acquisition in HPTN 039: relevance for HIV prevention trials among African women. J Acquir Immune Defic Syndr. 2010;53(5):606–13. [PMC free article: PMC2845724] [PubMed: 19838129]
- 11.
- Wand H, Ramjee G. The effects of injectable hormonal contraceptives on HIV seroconversion and on sexually transmitted infections. AIDS. 2012;26(3):375–80. [PubMed: 22156970]
- 12.
- Baeten JM, Benki S, Chohan V, Lavreys L, McClelland RS, Mandaliya K, et al. Hormonal contraceptive use, herpes simplex virus infection, and risk of HIV-1 acquisition among Kenyan women. AIDS. 2007;21(13):1771–7. [PubMed: 17690576]
- 13.
- Kleinschmidt I, Rees H, Delany S, Smith D, Dinat N, Nkala B, et al. Injectable progestin contraceptive use and risk of HIV infection in a South African family planning cohort. Contraception. 2007;75(6):461–7. [PubMed: 17519153]
- 14.
- Bulterys M, Chao A, Habimana P, Dushimimana A, Nawrocki P, Saah A. Incident HIV-1 infection in a cohort of young women in Butare, Rwanda. AIDS. 1994;8(11):1585–91. [PubMed: 7848595]
- 15.
- Feldblum PJ, Lie CC, Weaver MA, Van Damme L, Halpern V, Adeiga A, et al. Baseline factors associated with incident HIV and STI in four microbicide trials. Sex Transm Dis. 2010;37(10):594–601. [PubMed: 20879087]
- 16.
- Kapiga SH, Lyamuya EF, Lwihula GK, Hunter DJ. The incidence of HIV infection among women using family planning methods in Dar es Salaam, Tanzania. AIDS. 1998;12(1):75–84. [PubMed: 9456257]
- 17.
- Kilmarx PH, Limpakarnjanarat K, Mastro TD, Saisorn S, Kaewkungwal J, Korattana S, et al. HIV-1 seroconversion in a prospective study of female sex workers in northern Thailand: continued high incidence among brothel-based women. AIDS. 1998;12(14):1889–98. [PubMed: 9792390]
- 18.
- Kiddugavu M, Makumbi F, Wawer MJ, Serwadda D, Sewankambo NK, Wabwire-Mangen F, et al. Hormonal contraceptive use and HIV-1 infection in a population-based cohort in Rakai, Uganda. AIDS. 2003;17(2):233–40. [PubMed: 12545084]
- 19.
- Kumwenda NI, Kumwenda J, Kafulafula G, Makanani B, Taulo F, Nkhoma C, et al. HIV-1 incidence among women of reproductive age in Malawi. Int J STD AIDS. 2008;19(5):339–41. [PubMed: 18482966]
- 20.
- Laga M, Manoka A, Kivuvu M, Malele B, Tuliza M, Nzila N, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS. 1993;7(1):95–102. [PubMed: 8442924]
- 21.
- Lavreys L, Baeten JM, Martin HL Jr., Overbaugh J, Mandaliya K, Ndinya-Achola J, et al. Hormonal contraception and risk of HIV-1 acquisition: results of a 10-year prospective study. AIDS. 2004;18(4):695–7. [PubMed: 15090778]
- 22.
- Martin HL Jr., Nyange PM, Richardson BA, Lavreys L, Mandaliya K, Jackson DJ, et al. Hormonal contraception, sexually transmitted diseases, and risk of heterosexual transmission of human immunodeficiency virus type 1. J Infect Dis. 1998;178(4):1053–9. [PubMed: 9806034]
- 23.
- Plummer FA, Simonsen JN, Cameron DW, Ndinya-Achola JO, Kreiss JK, Gakinya MN, et al. Cofactors in male-female sexual transmission of human immunodeficiency virus type 1. J Infect Dis. 1991;163(2):233–9. [PubMed: 1988508]
- 24.
- Saracco A, Musicco M, Nicolosi A, Angarano G, Arici C, Gavazzeni G, et al. Man-to-woman sexual transmission of HIV: longitudinal study of 343 steady partners of infected men. J Acquir Immune Defic Syndr. 1993;6(5):497–502. [PubMed: 8097789]
- 25.
- Sinei SK, Fortney JA, Kigondu CS, Feldblum PJ, Kuyoh M, Allen MY, et al. Contraceptive use and HIV infection in Kenyan family planning clinic attenders. Int J STD AIDS. 1996;7(1):65–70. [PubMed: 8652717]
- 26.
- Ungchusak K, Rehle T, Thammapornpilap P, Spiegelman D, Brinkmann U, Siraprapasiri T. Determinants of HIV infection among female commercial sex workers in northeastern Thailand: results from a longitudinal study. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;12(5):500–7. [PubMed: 8757428]
- 27.
- Watson-Jones D, Baisley K, Weiss HA, Tanton C, Changalucha J, Everett D, et al. Risk factors for HIV incidence in women participating in an HSV suppressive treatment trial in Tanzania. AIDS. 2009;23(3):415–22. [PMC free article: PMC3223401] [PubMed: 19114859]
- 28.
- Polis CB, Phillips SJ, Curtis KM, Westreich DJ, Steyn PS, Raymond E, et al. Hormonal contraceptive methods and risk of HIV acquisition in women: a systematic review of epidemiological evidence. Contraception. 2014;90(4):360–90. [PubMed: 25183264]
- 29.
- Heffron R, Mugo N, Ngure K, Celum C, Donnell D, Were E, et al. Hormonal contraceptive use and risk of HIV-1 disease progression. AIDS. 2013;27(2):261–7. [PMC free article: PMC3740957] [PubMed: 23079806]
- 30.
- Study Group for the MRC Collaborative Study of HIV Infection in Women. Survival and progression of HIV disease in women attending GUM/HIV clinics in Britain and Ireland. Sex Transm Infect. 1999;75(4):247–52. [8 July 2014]; http://www
.ncbi.nlm.nih .gov/pmc/articles /PMC1758227/pdf/v075p00247.pdf. [PMC free article: PMC1758227] [PubMed: 10615311] - 31.
- Allen S, Stephenson R, Weiss H, Karita E, Priddy F, Fuller L, et al. Pregnancy, hormonal contraceptive use, and HIV-related death in Rwanda. J Womens Health (Larchmt). 2007;16(7):1017–27. [PubMed: 17903079]
- 32.
- Kilmarx PH, Limpakarnjanarat K, Kaewkungwal J, Srismith R, Saisorn S, Uthaivoravit W, et al. Disease progression and survival with human immunodeficiency virus type 1 subtype E infection among female sex workers in Thailand. J Infect Dis. 2000;181(5):1598–606. [PubMed: 10823759]
- 33.
- Morrison CS, Chen PL, Nankya I, Rinaldi A, Van Der Pol B, Ma YR, et al. Hormonal contraceptive use and HIV disease progression among women in Uganda and Zimbabwe. J Acquir Immune Defic Syndr. 2011;57(2):157–64. [PMC free article: PMC3164299] [PubMed: 21358412]
- 34.
- Polis CB, Wawer MJ, Kiwanuka N, Laeyendecker O, Kagaayi J, Lutalo T, et al. Effect of hormonal contraceptive use on HIV progression in female HIV seroconverters in Rakai, Uganda. AIDS. 2010;24(12):1937–44. [PMC free article: PMC2939866] [PubMed: 20502314]
- 35.
- Stringer EM, Giganti M, Carter RJ, El-Sadr W, Abrams EJ, Stringer JS. Hormonal contraception and HIV disease progression: a multicountry cohort analysis of the MTCT-Plus Initiative. AIDS. 2009;23 Suppl 1:S69–77. [PMC free article: PMC3865610] [PubMed: 20081390]
- 36.
- Stringer EM, Kaseba C, Levy J, Sinkala M, Goldenberg RL, Chi BH, et al. A randomized trial of the intrauterine contraceptive device vs hormonal contraception in women who are infected with the human immunodeficiency virus. Am J Obstet Gynecol. 2007;197(2):144.e1–8. [PMC free article: PMC2730754] [PubMed: 17689627]
- 37.
- Stringer EM, Levy J, Sinkala M, Chi BH, Matongo I, Chintu N, et al. HIV disease progression by hormonal contraceptive method: secondary analysis of a randomized trial. AIDS. 2009;23(11):1377–82. [PMC free article: PMC4217202] [PubMed: 19448528]
- 38.
- Cejtin HE, Jacobson L, Springer G, Watts DH, Levine A, Greenblatt R, et al. Effect of hormonal contraceptive use on plasma HIV-1-RNA levels among HIV-infected women. AIDS. 2003;17(11):1702–4. [PubMed: 12853757]
- 39.
- Richardson BA, Otieno PA, Mbori-Ngacha D, Overbaugh J, Farquhar C, John-Stewart GC. Hormonal contraception and HIV-1 disease progression among postpartum Kenyan women. AIDS. 2007;21(6):749–53. [PMC free article: PMC3380082] [PubMed: 17413696]
- 40.
- Clark RA, Theall KP, Amedee AM, Dumestre J, Wenthold L, Kissinger PJ. Lack of association between genital tract HIV-1 RNA shedding and hormonal contraceptive use in a cohort of Louisiana women. Sex Transm Dis. 2007;34(11):870–2. [PubMed: 17565332]
- 41.
- Clemetson DB, Moss GB, Willerford DM, Hensel M, Emonyi W, Holmes KK, et al. Detection of HIV DNA in cervical and vaginal secretions. Prevalence and correlates among women in Nairobi, Kenya. JAMA. 1993;269(22):2860–4. [PubMed: 8497089]
- 42.
- Graham SM, Masese L, Gitau R, Jalalian-Lechak Z, Richardson BA, Peshu N, et al. Antiretroviral adherence and development of drug resistance are the strongest predictors of genital HIV-1 shedding among women initiating treatment. J Infect Dis. 2010;202(10):1538–42. [PMC free article: PMC2957525] [PubMed: 20923373]
- 43.
- Kovacs A, Wasserman SS, Burns D, Wright DJ, Cohn J, Landay A, et al. Determinants of HIV-1 shedding in the genital tract of women. Lancet. 2001;358(9293):1593–601. [PubMed: 11716886]
- 44.
- Kreiss J, Willerford DM, Hensel M, Emonyi W, Plummer F, Ndinya-Achola J, et al. Association between cervical inflammation and cervical shedding of human immunodeficiency virus DNA. J Infect Dis. 1994;170(6):1597–601. [PubMed: 7996003]
- 45.
- Kumwenda JJ, Makanani B, Taulo F, Nkhoma C, Kafulafula G, Li Q, et al. Natural history and risk factors associated with early and established HIV type 1 infection among reproductive-age women in Malawi. Clin Infect Dis. 2008;46(12):1913–20. [PubMed: 18462100]
- 46.
- Lavreys L, Baeten JM, Kreiss JK, Richardson BA, Chohan BH, Hassan W, et al. Injectable contraceptive use and genital ulcer disease during the early phase of HIV-1 infection increase plasma virus load in women. J Infect Dis. 2004;189(2):303–11. [PubMed: 14722896]
- 47.
- Morrison CS, Demers K, Kwok C, Bulime S, Rinaldi A, Munjoma M, et al. Plasma and cervical viral loads among Ugandan and Zimbabwean women during acute and early HIV-1 infection. AIDS. 2010;24(4):573–82. [PMC free article: PMC3148071] [PubMed: 20154581]
- 48.
- Mostad SB, Overbaugh J, DeVange DM, Welch MJ, Chohan B, Mandaliya K, et al. Hormonal contraception, vitamin A deficiency, and other risk factors for shedding of HIV-1 infected cells from the cervix and vagina. Lancet. 1997;350(9082):922–7. [PubMed: 9314871]
- 49.
- Polis CB, Gray RH, Bwanika JB, Kigozi G, Kiwanuka N, Nalugoda F, et al. Effect of hormonal contraceptive use before HIV seroconversion on viral load setpoint among women in Rakai, Uganda. J Acquir Immune Defic Syndr. 2011;56(2):125–30. [PMC free article: PMC3023004] [PubMed: 21068673]
- 50.
- Roccio M, Gardella B, Maserati R, Zara F, Iacobone D, Spinillo A. Low-dose combined oral contraceptive and cervicovaginal shedding of human immunodeficiency virus. Contraception. 2011;83(6):564–70. [PubMed: 21570555]
- 51.
- Sagar M, Lavreys L, Baeten JM, Richardson BA, Mandaliya K, Ndinya-Achola JO, et al. Identification of modifiable factors that affect the genetic diversity of the transmitted HIV-1 population. AIDS. 2004;18(4):615–9. [PubMed: 15090766]
- 52.
- Seck K, Samb N, Tempesta S, Mulanga-Kabeya C, Henzel D, Sow PS, et al. Prevalence and risk factors of cervicovaginal HIV shedding among HIV-1 and HIV-2 infected women in Dakar, Senegal. Sex Transm Infect. 2001;77(3):190–3. [PMC free article: PMC1744303] [PubMed: 11402227]
- 53.
- Tanton C, Weiss HA, Le Goff J, Changalucha J, Rusizoka M, Baisley K, et al. Correlates of HIV-1 genital shedding in Tanzanian women. PloS One. 2011;6(3):e17480. [PMC free article: PMC3046975] [PubMed: 21390251]
- 54.
- Heikinheimo O, Lehtovirta P, Aho I, Ristola M, Paavonen J. The levonorgestrel-releasing intrauterine system in human immunodeficiency virus-infected women: a 5-year follow-up study. Am J Obstet Gynecol. 2011;204(2):126.e1–4. [PubMed: 21035781]
- 55.
- Aweeka FT, Rosenkranz SL, Segal Y, Coombs RW, Bardeguez A, Thevanayagam L, et al. The impact of sex and contraceptive therapy on the plasma and intracellular pharmacokinetics of zidovudine. AIDS. 2006;20(14):1833–41. [PubMed: 16954724]
- 56.
- Kearney BP, Mathias A. Lack of effect of tenofovir disoproxil fumarate on pharmacokinetics of hormonal contraceptives. Pharmacotherapy. 2009;29(8):924–9. [PubMed: 19637945]
- 57.
- Landolt NK, Phanuphak N, Ubolyam S, Pinyakorn S, Kriengsinyot R, Ahluwalia J, et al. Efavirenz, in contrast to nevirapine, is associated with unfavorable progesterone and antiretroviral levels when coadministered with combined oral contraceptives. J Acquir Immune Defic Syndr. 2013;62(5):534–9. [PubMed: 23187949]
- 58.
- Mildvan D, Yarrish R, Marshak A, Hutman HW, McDonough M, Lamson M, et al. Pharmacokinetic interaction between nevirapine and ethinyl estradiol/norethindrone when administered concurrently to HIV-infected women. J Acquir Immune Defic Syndr. 2002;29(5):471–7. [PubMed: 11981363]
- 59.
- Nanda K, Delany-Moretlwe S, Dube K, Lendvay A, Kwok C, Molife L, et al. Nevirapine-based antiretroviral therapy does not reduce oral contraceptive effectiveness. AIDS. 2013;27 Suppl 1:S17–25. [PubMed: 24088680]
- 60.
- Stuart GS, Moses A, Corbett A, Phiri G, Kumwenda W, Mkandawire N, et al. Combined oral contraceptives and antiretroviral PK/PD in Malawian women: pharmacokinetics and pharmacodynamics of a combined oral contraceptive and a generic combined formulation antiretroviral in Malawi. J Acquir Immune Defic Syndr. 2011;58(2):e40–3. [PMC free article: PMC3176587] [PubMed: 21921726]
- 61.
- Carten ML, Kiser JJ, Kwara A, Mawhinney S, Cu-Uvin S. Pharmacokinetic interactions between the hormonal emergency contraception, levonorgestrel (Plan B), and Efavirenz. Infect Dis Obstet Gynecol. 2012;2012:137192. [PMC free article: PMC3299227] [PubMed: 22536010]
- 62.
- Sevinsky H, Eley T, Persson A, Garner D, Yones C, Nettles R, et al. The effect of efavirenz on the pharmacokinetics of an oral contraceptive containing ethinyl estradiol and norgestimate in healthy HIV-negative women. Antivir Ther. 2011;16(2):149–56. [PubMed: 21447863]
- 63.
- Crauwels HM, van Heeswijk RP, Buelens A, Stevens M, Hoetelmans RM. Lack of an effect of rilpivirine on the pharmacokinetics of ethinylestradiol and norethindrone in healthy volunteers. Int J Clin Pharmacol Ther. 2014;52(2):118–28. [PubMed: 24161160]
- 64.
- Scholler-Gyure M, Kakuda TN, Woodfall B, Aharchi F, Peeters M, Vandermeulen K, et al. Effect of steady-state etravirine on the pharmacokinetics and pharmacodynamics of ethinylestradiol and norethindrone. Contraception. 2009;80(1):44–52. [PubMed: 19501215]
- 65.
- Perry SH, Swamy P, Preidis GA, Mwanyumba A, Motsa N, Sarero HN. Implementing the Jadelle implant for women living with HIV in a resource-limited setting in sub-Saharan Africa: concerns for drug interactions leading to unintended pregnancies. AIDS. 2014;28(5):791–3. [PubMed: 24401645]
- 66.
- Cohn SE, Park JG, Watts DH, Stek A, Hitti J, Clax PA, et al. Depo-medroxyprogesterone in women on antiretroviral therapy: effective contraception and lack of clinically significant interactions. Clin Pharmacol Ther. 2007;81(2):222–7. [PubMed: 17192768]
- 67.
- Nanda K, Amaral E, Hays M, Viscola MA, Mehta N, Bahamondes L. Pharmacokinetic interactions between depot medroxyprogesterone acetate and combination antiretroviral therapy. Fertil Steril. 2008;90(4):965–71. [PubMed: 17880953]
- 68.
- Vogler MA, Patterson K, Kamemoto L, Park JG, Watts H, Aweeka F, et al. Contraceptive efficacy of oral and transdermal hormones when co-administered with protease inhibitors in HIV-1-infected women: pharmacokinetic results of ACTG trial A5188. J Acquir Immune Defic Syndr. 2010;55(4):473–82. [PMC free article: PMC4197050] [PubMed: 20842042]
- 69.
- Atrio J, Stanczyk FZ, Neely M, Cherala G, Kovacs A, Mishell DR Jr. Effect of protease inhibitors on steady-state pharmacokinetics of oral norethindrone contraception in HIV-infected women. J Acquir Immune Defic Syndr. 2014;65(1):72–7. [PMC free article: PMC3946363] [PubMed: 24025339]
- 70.
- Anderson MS, Hanley WD, Moreau AR, Jin B, Bieberdorf FA, Kost JT, et al. Effect of raltegravir on estradiol and norgestimate plasma pharmacokinetics following oral contraceptive administration in healthy women. Br J Clin Pharmacol. 2011;71(4):616–20. [PMC free article: PMC3080652] [PubMed: 21395656]
- 71.
- Song I, Mark S, Borland J, Chen S, Wajima T, Peppercorn A, et al. Dolutegravir has no effect on the pharmacokinetics of methadone or oral contraceptives with norgestimate and ethinyl estradiol; 20th Conference on Retroviruses and Opportunistic Infections; Atlanta (GA). 3–6 March 2013; [18 July 2014]. http://www
.hiv-druginteractions .org/data /NewsItem/103_CROI_2013.pdf.
Footnotes
- 1
Mohllajee AP, Curtis KM, Flanagan RG, Rinehart W, Gaffield ML, Peterson HB. Keeping up with evidence: a new system for WHO's evidence-based family planning guidance. Am J Prev Med. 2005;28(5):483–90. [PubMed: 15894153].
- 2
The first edition was published in 2012, the second edition in 2014.
- 3
For further information on GRADE, see: www
.gradeworkinggroup.org/index.htm - 4
Moher D, Liberati A, Tetzlaff J, Altman DG., The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6(6):e1000097. [PMC free article: PMC2707599] [PubMed: 19621072].
- 5
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 Suppl):21–35. [PubMed: 11306229].
- 6
Madden T, Secura GM, Nease RF, Politi MC, Peipert JF. The role of contraceptive attributes in women's contraceptive decision making. Am J Obstet Gynecol. 2015 [Epub ahead of print] S0002-9378(15)00107–6. [PMC free article: PMC4485538] [PubMed: 25644443]
- 7
Hooper DJ. Attitudes, awareness, compliance and preferences among hormonal contraception users: a global, cross-sectional, self-administered, online survey. Clin Drug Investig. 2010;30(11):749–63 [PubMed: 20818837].
- 8
d'Arcangues CM, Ba-Thike K, Say L. Expanding contraceptive choice in the developing world: lessons from the Lao People's Republic and the Republic of Zambia. Eur J Contracept Reprod Health Care. 2013;18:421–34. [PubMed: 23978240].
- 9
Blanc A, Tsui AO, Croft TN, Trevitt JL. Patterns and trends in adolescents' contraceptive use and discontinuation in developing countries and comparisons with adult women. Int Perspect Sex Reprod Health. 2009;35(2):63–71. [PubMed: 19620090].
- 10
Singh S, Darroch JE. Adding it up: costs and benefits of contraceptive services – estimates for 2012. New York (NY): Guttmacher Institute and United Nations Population Fund (UNFPA); 2012. [24 March 2015]. https://www
.guttmacher .org/pubs/AIU-2012-estimates.pdf..
Publication Details
Copyright
All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob).
Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html).
Publisher
World Health Organization, Geneva
NLM Citation
Medical Eligibility Criteria for Contraceptive Use. 5th edition. Geneva: World Health Organization; 2015. I, Development of the Medical eligibility criteria for contraceptive use, fifth edition.