NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-.

PDQ Cancer Information Summaries [Internet].
Show detailsThis PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood vascular tumors. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions.
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
General Information About Childhood Vascular Tumors
Vascular anomalies are a spectrum of rare diseases classified as vascular tumors or malformations. An updated classification system was adopted at the General Assembly of the International Society for the Study of Vascular Anomalies (ISSVA, April 2014) and recently published.[1] Generally, vascular tumors are proliferative, while malformations enlarge through expansion of a developmental anomaly without underlying proliferation.
Growth and/or expansion of vascular anomalies can cause clinical problems such as disfigurement, chronic pain, recurrent infections, coagulopathies (thrombotic and hemorrhagic), organ dysfunction, and death. Individuals often experience progressive clinical symptoms with worsening quality of life.
Limited treatment options are available; their efficacy has not been validated in prospective clinical trials. Historically, therapies have been mostly interventional and surgical to palliate symptoms. New drugs such as propranolol and sirolimus are now available for the treatment of patients with some of these complex conditions. The first prospective clinical trial using propranolol for infantile hemangioma has been published, as well as the first prospective clinical trial that studied the effectiveness of sirolimus for complicated vascular anomalies.[2,3]
With a prevalence of 4% to 5%, infantile hemangiomas are the most common benign tumors of infancy. Other vascular tumors are rare. The classification of these tumors has been difficult, especially in the pediatric population, because of their rarity, unusual morphologic appearance, diverse clinical behavior, and the lack of independent stratification for pediatric tumors. In 2013, The World Health Organization (WHO) updated the classification of soft tissue vascular tumors. Pediatric tumors were not independently stratified and the terminology was mostly left unchanged, but the intermediate category of tumors was divided into locally aggressive and rarely metastasizing. The ISSVA classification of tumors is based on the WHO classification (refer to Tables 1 and 2) but the ISSVA classification uses more precise terminology and phenotypes that have been agreed upon by the members of ISSVA.
Table 1. 2013 World Health Organization Classification of Vascular Tumors
| Category | Vascular Tumor Type |
|---|---|
| Benign | Hemangioma |
| Epithelioid hemangioma | |
| Angiomatosis | |
| Lymphangioma | |
| Intermediate (locally aggressive) | Kaposiform hemangioendothelioma |
| Intermediate (rarely metastasizing) | Retiform hemangioendothelioma |
| Papillary intralymphatic angioendothelioma | |
| Composite hemangioendothelioma | |
| Kaposi sarcoma | |
| Malignant | Epithelioid hemangioendothelioma |
| Angiosarcoma of soft tissue |
aAdapted from Fletcher et al.[4]
Table 2. 2014 International Society for the Study of Vascular Anomalies (ISSVA) Classification of Vascular Tumorsa
| Category | Vascular Tumor Type |
|---|---|
| Benign | Infantile hemangioma/hemangioma of infancy |
| Congenital hemangioma | |
| —Rapidly involuting (RICH) | |
| —Non-involuting (NICH) | |
| —Involuting (PICH) | |
| Tufted angioma | |
| Spindle cell hemangioma | |
| Pyogenic granuloma (also known as lobular capillary hemangioma) | |
| Others | |
| Locally aggressive or borderline | Kaposiform hemangioendothelioma |
| Retiform hemangioendothelioma | |
| Papillary intralymphatic angioendothelioma (PILA), Dabska tumor | |
| Composite hemangioendothelioma | |
| Kaposi sarcoma | |
| Others | |
| Malignant | Epithelioid hemangioendothelioma |
| Angiosarcoma | |
| Others |
aAdapted from ISSVA Classification of Vascular Anomalies. ©2014 International Society for the Study of Vascular Anomalies. Available at "issva
.org/classification." Accessed January 2016.[5]
The quality of evidence regarding childhood vascular tumors is limited by retrospective data collection, small sample size, cohort selection and participation bias, and heterogeneity of the disorders.
References
- Wassef M, Blei F, Adams D, et al.: Vascular Anomalies Classification: Recommendations From the International Society for the Study of Vascular Anomalies. Pediatrics 136 (1): e203-14, 2015. [PubMed: 26055853]
- Léauté-Labrèze C, Hoeger P, Mazereeuw-Hautier J, et al.: A randomized, controlled trial of oral propranolol in infantile hemangioma. N Engl J Med 372 (8): 735-46, 2015. [PubMed: 25693013]
- Adams DM, Trenor CC 3rd, Hammill AM, et al.: Efficacy and Safety of Sirolimus in the Treatment of Complicated Vascular Anomalies. Pediatrics 137 (2): e20153257, 2016. [PMC free article: PMC4732362] [PubMed: 26783326]
- Fletcher CDM, Bridge JA, Hogendoorn P, et al., eds.: WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon, France: IARC Press, 2013.
- International Society for the Study of Vascular Anomalies: ISSVA Classification for Vascular Anomalies. Melbourne, Australia: International Society for the Study of Vascular Anomalies, 2014. Available online. Last accessed August 31, 2017.
Benign Tumors
Benign vascular tumors include the following:
Infantile Hemangioma
Incidence and epidemiology
Infantile hemangiomas (IH) are the most common benign vascular tumor of infancy, occurring in 4% to 5% of infants. They are not usually present at birth and are diagnosed most commonly at age 3 to 6 weeks.[1-3] The lesion proliferates for an average of 5 months, stabilizes, and then involutes over several years.
Infantile hemangiomas are more common in females, non-Hispanic white patients, and premature infants. Multiple hemangiomas are more common in infants who are the product of multiple gestations.[1,4] Infantile hemangiomas are associated with advanced maternal age and placental complications.[1]
Biology
Most infantile hemangiomas occur sporadically. However, they may rarely be caused by an abnormality of chromosome 5 and present in an autosomal dominant pattern.[5] In a study that evaluated inheritance patterns of infantile hemangiomas, 34% of patients had a family history of infantile hemangioma, most commonly in a first-degree relative.[6]
Infantile hemangioma endothelial cells have proven to be clonal in nature.[7,8] Infantile hemangioma proliferation occurs during vasculogenesis (the formation of new blood vessels from angioblasts), as opposed to angiogenesis (the formation of new blood vessels from existing blood vessels). During proliferation, provasculogenic factors are expressed, such as vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), CD34, CD31, CD133, LYVE-1, and insulin-like growth factor (IGF)-2.[9-12] In involution, infantile hemangiomas express increased apoptosis.[12] During this phase, there are also increased mast cells and levels of metalloproteinase, as well as upregulation of interferon and decreased basic FGF (bFGF).[12-14] Throughout their development, endothelial cells in infantile hemangioma express a particular phenotype showing positive staining for glucose transporter (GLUT1). GLUT1 is also expressed on placental endothelial cells but is absent in other vascular tumors such as congenital hemangioma and vascular malformations.[15]
Hypoxia may have a role in the pathogenesis of hemangiomas. As described above, hemangiomas are associated with conditions related to placental hypoxia,[1] and multiple targets of hypoxia [16,17] are demonstrated in proliferating hemangiomas such as VEGF-A, GLUT1, and IGF-2.[9,11,15] The hypotheses suggest that a proliferating hemangioma is an attempt to normalize hypoxic tissue that occurred in utero.
Clinical presentation
Most infantile hemangiomas are not present at birth but precursor lesions such as telangiectasia or faint discoloration of the skin or hypopigmentation can often be seen. The lesion can be mistaken as a bruise from birth trauma or as a capillary malformation (port wine stain) (refer to Figure 1).[18,19]

Figure 1. The photos on the left depict the precursor lesion (faint color with halo). The photos on the right depict the hemangioma after proliferation (slightly raised with a brighter central color). Credit: Israel Fernandez-Pineda, M.D.
Infantile hemangiomas can be superficial in the dermis, deep in the subcutaneous tissue, combined, or in the viscera. Combined lesions are common. They are most common in the head and neck but can be anywhere on the body. They can be localized, segmental, or multiple in nature.
The cutaneous appearance of infantile hemangiomas is usually red to crimson, firm, and warm in the proliferative phase. The lesion then lightens centrally and becomes less warm and softer; it then flattens and loses its color. The process of involution can take several years and once involution has occurred, regrowth is uncommon. In two patients treated with growth hormone, regrowth after involution was noted.[20] On further investigation, growth hormone receptors were found on the infantile hemangioma cells. Although preliminary, this may advance the research into the etiology of hemangioma growth.
Permanent sequelae, such as telangiectasia, anetodermal skin, redundant skin, and a persistent superficial component, can occur after hemangioma involution (refer to Figure 2). In a retrospective cohort study of 184 hemangiomas, the overall incidence of significant sequelae was 54.9%. Sequelae were more common in combined hemangiomas, hemangiomas with a step or abrupt border, and cobblestone surface hemangiomas. Furthermore, this study revealed that the average age to hemangioma involution was 3.5 years.[21]
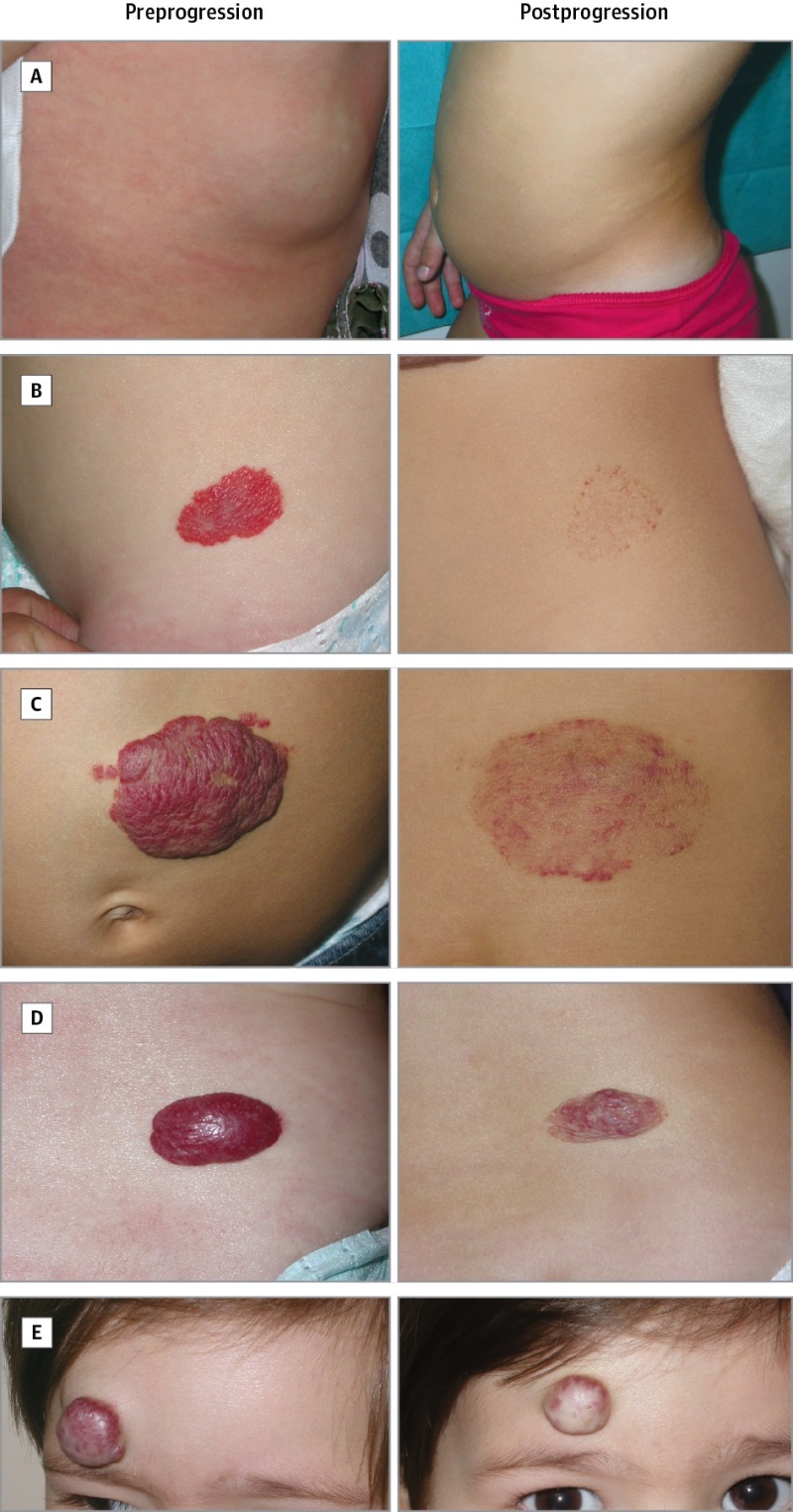
Figure 2. Examples of different types of sequelae. A, deep hemangioma that regressed without sequelae; B, superficial hemangioma that left only telangiectasia; C, mixed hemangioma that left anetodermic skin; D, mixed hemangioma that left redundant skin; and E, mixed hemangioma that left fibrofatty tissue. Reproduced with permission from JAMA Dermatology. 2016. 152 (11): 1239–1243. Copyright © (2016) American Medical Association. All rights reserved.
Diagnostic and staging evaluation
Infantile hemangiomas are usually diagnosed by the history and clinical appearance. Biopsy is rarely needed and performed only if there is an atypical appearance and/or atypical history and presentation. Imaging is not usually necessary, but if there is a deeper lesion without a cutaneous component, ultrasound imaging is beneficial for diagnosis because it reveals a high flow lesion with a typical Doppler wave characteristic.[22]
Infantile hemangioma with minimal or arrested growth
Infantile hemangioma with minimal or arrested growth (IH-MAG) is a variant of hemangioma that can be confused with capillary malformation or other syndromic hemangioma, such as PHACE syndrome, because of their unusual characteristics. These hemangiomas are mostly fully formed at birth and are characterized by telangiectasia and venules with light and dark areas of skin coloration (refer to Figure 3). They resolve spontaneously and are pathologically GLUT1 positive.[23]
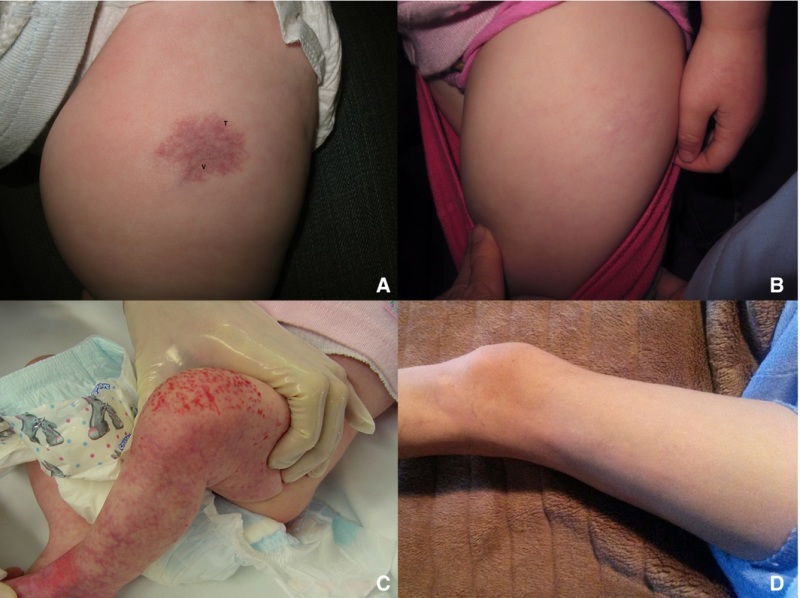
Figure 3. Patient 4 at (A) presentation and (B) resolution. Patient 5 at (C) presentation and (D) resolution. Ma, E. H., Robertson, S. J., Chow, C. W., and Bekhor, P. S. (2017), Infantile Hemangioma with Minimal or Arrested Growth: Further Observations on Clinical and Histopathologic Findings of this Unique but Underrecognized Entity. Pediatr Dermatol, 34: 64–71. doi:10.1111/pde.13022. Used with permission.
Airway infantile hemangioma
Airway infantile hemangiomas are usually associated with segmental hemangiomas in a bearded distribution, which may include all or some of the following—the preauricular skin, mandible, lower lip, chin, or anterior neck. Airway infantile hemangioma can occur without skin lesions. It is important for an otolaryngologist to proactively assess lesions in this distribution before signs of stridor occur. The incidence of an airway infantile hemangioma increases with increased area of bearded involvement.[24]
Periorbital infantile hemangioma
Periorbital hemangiomas can cause visual compromise.[25] This usually occurs with hemangiomas of the upper medial eyelid but any hemangioma around the eye that is large enough can obstruct the visual axis. The clinician should be aware of subcutaneous periocular hemangiomas, as these lesions can extend into the orbit, causing exophthalmos or globe displacement with only limited cutaneous manifestations. Issues with these lesions include astigmatism from direct pressure of the growing hemangioma, ptosis, proptosis, and strabismus. One of the leading causes of preventable blindness in children is stimulus-deprivation amblyopia caused by hemangioma obstruction. All periorbital hemangiomas or those with any possibility of potential visual impairment should have an ophthalmologic evaluation.
Syndromes associated with infantile hemangioma
Syndromes associated with infantile hemangioma include the following:
- PHACE syndrome: PHACE syndrome represents a spectrum of diseases and is defined by the presence of a large segmental infantile hemangioma, usually on the face or head, in association with one or more congenital malformations (refer to Figure 4). PHACE syndrome is more common in girls and in full-term, normal birth weight and singleton infants.[26-31,31] The syndrome is not rare among patients with infantile hemangiomas. A prospective study of 108 infants with large facial hemangiomas observed that 31% of patients had PHACE syndrome.[32]

Figure 4. A large segmental infantile hemangioma (plaque-like) in a bearded distribution. This patient has an increased risk of PHACE syndrome, airway infantile hemangioma, and ulceration. A tracheostomy was placed secondary to a very diffuse airway hemangioma. Credit: Denise Adams, M.D.
Consensus criteria for definite and possible PHACE syndrome were developed at an expert panel meeting, as follows:[28]PHACE
- -
Posterior fossa abnormalities. Anomalies include posterior fossa malformations, including Dandy-Walker complex, cerebellar hypoplasia, atrophy, and dysgenesis/agenesis of the vermis. Effects of these anomalies include developmental delays and pituitary dysfunction.[33]
- -
Hemangioma. A large segmental hemangioma over the face, neck, and rarely, the chest and shoulder area.
- -
Arterial abnormalities. Cerebrovascular anomalies can include carotid artery abnormalities and absence, dilation, or narrowing of cerebral vessels. These anomalies, especially the carotid anomalies, can lead to progressive arterial occlusion and even stroke. Other neurological issues are noted in infancy and childhood.[30,31,34-36]
- -
Cardiac abnormalities. Cardiac anomalies are most commonly coarctation of the aorta (coarctation is more proximal and affects longer segments), complex aortic arch anomalies, and ventricular and atrial septal defects.
- -
Eye abnormalities. Ophthalmologic anomalies can include microphthalmos, retinal vascular abnormalities, persistent fetal retinal vessels, exophthalmos, coloboma, and optic nerve atrophy.
Diagnosis of PHACE requires clinical examination, cardiac evaluation with echocardiogram, ophthalmologic evaluation, and magnetic resonance imaging (MRI)/magnetic resonance angiogram (MRA) of the head, neck, and mediastinum. Patients need to be monitored for short- and long-term effects as noted above. Other issues include speech and language delay, swallowing dysfunction, hearing loss (conductive and sensorineural), and early-onset migraines.[37-39]A report of two patients with retro-orbital infantile hemangioma and arteriopathy suggested a possible new presentation of PHACE syndrome.[40] For patients with proptosis, globe deviation, and strabismus, an MRI/MRA is recommended. Further workup for PHACE may be needed on the basis of central nervous system (CNS) findings. - LUMBAR/PELVIS/SACRAL syndrome: Infantile hemangiomas located over the lumbar or sacral spine may be associated with genitourinary, anorectal anomalies, or neurological issues such as tethered cord.[41-43] The following criteria have been used to describe segmental infantile hemangioma syndrome in the lumbar, pelvic, and sacral areas. This syndrome has been described in the literature using several acronyms.
LUMBAR
- -
Lower-body hemangioma and other cutaneous defects.
- -
Urogenital anomalies or ulceration.
- -
Myelopathy.
- -
Bony deformities.
- -
Anorectal malformations or arterial anomalies.
- -
Renal anomalies.
PELVIS
- -
Perineal hemangioma.
- -
External genital malformations.
- -
Lipomyelomeningocele.
- -
Vesicorenal abnormalities.
- -
Imperforate anus.
- -
Skin tag.
SACRAL
- -
Spinal dysraphism.
- -
Anogenital.
- -
Cutaneous.
- -
Renal and urologic anomalies Associated with an angioma of Lumbosacral localization.
Segmental lesions over the gluteal cleft and lumbar spine need to be evaluated with either ultrasound or MRI, depending on the age of the patient.
Infants with more than five infantile hemangiomas need to be evaluated for visceral hemangiomas. The most common site of involvement is the liver, in which multiple or diffuse lesions can be noted.[44,45] Often these lesions are asymptomatic, but in a minority of cases, symptoms such as heart failure secondary to large vessel shunts, compartment syndrome, or profound hypothyroidism can occur due to the expression of iodothyronine deiodinase.[46] Multiple or diffuse liver hemangiomas can occur in the absence of skin lesions. (Refer to the Benign Vascular Tumors of the Liver section of this summary for more information.) Other rare potential complications of visceral hemangiomas, dependent on specific organ involvement, include gastrointestinal hemorrhage, obstructive jaundice, and CNS sequelae, caused by mass effects.
Treatment of infantile hemangioma
Treatment options for infantile hemangioma include the following:
- Pulsed dye laser therapy. Usually used for ulcerated infantile hemangiomas and residual lesions, such as telangiectasia after the proliferative period.[47] Pulsed dye laser therapy helps with pain from ulcerative infantile hemangiomas. The use of pulsed dye laser therapy as upfront treatment for infantile hemangiomas is controversial.
- Excisional surgery. With the advent of new medical treatments, the use of surgery is reserved for ulcerated lesions, residual lesions, large periocular lesions that interfere with vision, and facial lesions with aesthetic impact that do not respond to medical therapy.[48]
Propranolol therapy
Propranolol, a nonselective beta-blocker, is the first-line therapy for infantile hemangiomas. Potential mechanisms of action include vasoconstriction and/or decreased expression of VEGF and bFGF, leading to apoptosis.[49,50] Specific mechanisms of action are under investigation.
The use of propranolol was first noted in two infants treated for cardiac issues in Europe. A change in color, softening, and decrease in hemangioma size was noted. Since that time, the results of a randomized controlled trial have been reported.[51] In 2014, the U.S. Food and Drug Administration (FDA) approved the drug propranolol hydrochloride for the treatment of proliferating infantile hemangioma.
There are many other published reports about the efficacy and safety of propranolol.[52-56] Lack of response to treatment is rare. Propranolol therapy is usually used during the proliferative phase but has been effective in patients older than 12 months with infantile hemangiomas.[57]
Evidence (propranolol therapy):
- In a large industry-sponsored randomized trial, 456 infants aged 5 weeks to 5 months with a proliferating infantile hemangioma of at least 1.5 cm received either a placebo or propranolol (1 mg/kg per day or 3 mg/kg per day) for 3 or 6 months. After interim analysis of the first 188 patients who completed 24 weeks of trial treatment, the regimen of 3 mg/kg per day for 6 months was selected for the final efficacy analysis.[51][Level of evidence: 1iDiv]
- Of patients who received the selected regimen, 88% showed improvement by week 5, compared with 5% of patients who received the placebo.
- Adverse events occurred infrequently.
- In 635 infants with infantile hemangioma, the overall response rate was 91% after 2 mg/kg per day, with most patients showing regression and only 2% with side effects, none of which were severe.[56][Level of evidence: 3iiiDiv]
- A meta-analysis that evaluated 5,130 patients from 61 studies concluded that propranolol was more effective and safer than were other treatments for infantile hemangioma.[58]
- Airway infantile hemangioma lesions are rare; thus, there are limited prospective studies. A meta-analysis of 61 patients noted a trend of decreased treatment failure with increased dosing strategies, which is consistent with the use of higher doses of propranolol in these patients (3 mg/kg/day). The analysis also suggested that the concurrent use of steroids and propranolol may have reduced efficacy in patients with segmental airway hemangiomas, but previous treatment with steroids had no deleterious effect.[59] Additional prospective studies are needed to validate these findings.
Based on expert consensus panel recommendations and updated reviews, considerations for the administration of propranolol therapy include the following:[60-62]
- Initiation of treatment: Treatment should be undertaken in consultation with a pediatric vascular anomaly specialist with expertise in the diagnosis and treatment of pediatric vascular tumors and in the use of propranolol in children. In accord with an expert consensus panel, it is suggested that hospitalization for initiation of oral propranolol be considered in the following circumstances:[60]
- -
Infant aged 5 weeks or younger (corrected for gestational age).
- -
Infant of any age with inadequate social support.
- -
Infant of any age with comorbid conditions affecting the cardiovascular or respiratory system, including symptomatic airway infantile hemangiomas.
- -
Infant of any age with conditions affecting blood glucose maintenance.
The pretreatment evaluation (inpatient or outpatient) includes the following:- -
History, with focus on cardiovascular and respiratory abnormalities (e.g., poor feeding, dyspnea, tachypnea, diaphoresis, wheezing, heart murmur) and family history of heart block or arrhythmia.
- -
Physical examination including cardiac and pulmonary assessment and measurement of heart rate and blood pressure.
- -
Consideration of an electrocardiogram, especially in children with heart rate lower than normal for age and history of arrhythmia or arrhythmia detected during examination.
- -
Family history of congenital heart disease or maternal history of connective tissue disease.
- Dosing: The dosing used is generally 1 mg/kg per day to 3 mg/kg per day divided into two or three doses. Patients are initially started at a dose of 0.5 mg/kg per day to 1 mg/kg per day and increased over time. Initially, dosing of three times per day is recommended for infants younger than 8 weeks and for patients with PHACE syndrome.
- Monitoring: Monitoring varies depending on the institution. However, oral propranolol peaks at 1 to 3 hours after administration and most centers measure heart rate and blood pressure 1 and 2 hours after each dose with initiation and then when the dose is increased by at least 0.5 mg/kg per day. Parent and patient education includes when to hold the medication, signs of hypoglycemia, feeding necessity through the night, and when to call the physician with issues, such as illness, that may interfere with oral intake or lead to dehydration or respiratory problems.
- Contraindications: Propranolol treatment is contraindicated in infants and children with the following:
- -
Sinus bradycardia.
- -
Hypotension.
- -
Heart block greater than first degree.
- -
Heart failure.
- -
Asthma.
- -
Hypersensitivity.
- -
PHACE syndrome. PHACE syndrome with CNS arterial disease and/or coarctation of the aorta may be a relative contraindication. A decision to treat should be made in consultation with neurology and cardiology.
- Adverse effects: Adverse effects of propranolol include the following:[63]
- -
Hypoglycemia.
- -
Hypotension.
- -
Bradycardia.
- -
Sleep disturbance.
- -
Diarrhea/constipation.
- -
Cold extremities.
These complications have been reported in several studies, and severe complications have been rare.[63] The risk of these complications is increased in patients with comorbidities and concomitant diseases, including diarrhea, vomiting, and respiratory infections. The need for close monitoring and possible periods of drug discontinuation should be considered during periods of illness. - Rebound growth after propranolol therapy: Rebound refers to the growth of infantile hemangiomas after propranolol cessation. A multi-institutional, retrospective review of 997 patients with infantile hemangiomas found a rebound rate of 25.3% in 912 patients with adequate data. On univariate analysis, the factors associated with rebound included discontinuation of treatment before age 9 months, female sex, location on head/neck, segmental pattern, and deep or mixed skin involvement. On multivariate analysis, only deep infantile hemangiomas and female sex were significantly related.[64]
Other selective beta-blocker therapy
Because of the nonselective and lipophilic nature of propranolol with the ability to cross the blood-brain barrier, other beta-blockers are being used for the treatment of infantile hemangiomas. In two small comparison studies, there was no difference in efficacy between propranolol and atenolol.[65,66] In a retrospective study using nadolol, similar results were seen.[67] A prospective study of 76 infants treated with atenolol noted efficacy and safety similar to propranolol.[68][Level of evidence: 3iiDiv] Additional studies are needed to assess differences between the toxicities of these agents and the toxicities of propranolol. There is some suggestion that the more selective beta-blockers have fewer side effects.[69]
Corticosteroid therapy
Before propranolol, corticosteroids were the first line of treatment for infantile hemangiomas. They were first used in the late 1950s but were never approved by the U.S. FDA. Corticosteroid therapy has become less popular secondary to the acute and long-term side effects of steroids (gastrointestinal irritability, immunosuppression, adrenocortical suppression, cushingoid features, and growth failure).
Corticosteroids (prednisone or methylprednisolone) are used at times when there is a contraindication to beta-blocker therapy or as initial treatment while a patient is started on beta-blocker therapy.[70]
Topical beta-blocker therapy
Topical beta-blockers are used mainly for the treatment of small, localized, superficial hemangiomas as an alternative to observation. They have also been used in combination with systemic therapy in complicated hemangiomas or to prevent rebound in a hemangioma being tapered off of systemic treatment.[71-73]
The topical timolol that is used is the ophthalmic gel-forming solution 0.5%. One drop is applied to the hemangioma two to three times per day until stable response is achieved.
This treatment has limited side effects, but infants with a postmenstrual age of younger than 44 weeks and weight at treatment initiation of less than 2,500 grams may be at risk of adverse events, including bradycardia, hypotension, apnea, and hypothermia.[74,75] Close monitoring of temperature, blood pressure, and heart rate in premature and low birth weight infants with infantile hemangiomas at initiation of and during therapy with topical timolol is necessary.
Evidence (topical beta-blocker therapy):
- In a multicenter, retrospective, cohort study, 731 children with predominantly superficial hemangiomas were treated with topical timolol 0.5% twice daily. Ninety-two percent of patients showed significant improvement in color and 77% showed improvement in size, extent, and volume. Topical timolol is generally well tolerated. However, data on its safety are limited.[73]
Combined therapy for complicated hemangiomas
Combined therapy is considered either at initiation of treatment in complicated lesions in which there is functional impairment or organ compromise or used at the end of systemic therapy to prevent regrowth of the hemangioma rebound. Further investigation of efficacy and safety is needed for these regimens.
Evidence (combined therapy for complicated hemangiomas):
- A prospective randomized study that compared propranolol and 2 weeks of steroid therapy with propranolol alone revealed a decrease in the size of the hemangioma at 2, 4, and 8 weeks but no statistical difference in the size at 6 months.[76]
- A prospective randomized study that compared timolol and propranolol with propranolol alone reported a decrease in color of the infantile hemangioma in the timolol group but no difference in overall size of the infantile hemangioma between the two treatment groups.[77]
- Topical therapy with timolol combined with oral propranolol has been used.[78,79][Level of evidence: 3iiDiv]
Treatment options under clinical evaluation for infantile hemangiomas
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- NCT02505971 (Nadolol Versus Propranolol in Children With Infantile Hemangioma): This randomized, controlled, double-blinded study at Toronto Sick Kids is evaluating the efficacy and safety of both groups (nadolol and propranolol). Inclusion is for patients with hemangiomas that require systemic treatment.
- NCT02913612 (Efficacy, Safety, and Pharmacokinetics of Topical Timolol in Infants With Infantile Hemangioma [TIM01]): This is a multicenter, double-masked, randomized, efficacy, safety, and pharmacokinetic study. Timolol maleate 0.25% is being compared with timolol maleate 0.5%.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Congenital Hemangiomas
Congenital hemangiomas are benign vascular tumors that proliferate in utero. Development of these lesions is complete at birth. Histologically, these lesions are GLUT1 negative, unlike infantile hemangiomas. They are usually cutaneous, but can be found in the viscera. Complications include hemorrhage, transient heart failure, and transient coagulopathy.[80]
To the clinician unfamiliar with these lesions, congenital hemangiomas can be difficult to diagnose. Diagnostic criteria include a purpuric lesion fully formed at birth, frequently with a halo around the lesion, with high flow noted on ultrasound imaging. Essential to the diagnosis is observation of decrease in size over time or stability. These lesions do not enlarge unless there is hemorrhage into the tumor.
Somatic activating mutations of GNAQ and GNA11 have been found to be associated with congenital hemangiomas.[81] Additional research is necessary to assess the significance of these findings, as this may aid in diagnosis and pathophysiology.
Congenital hemangiomas are divided into the following three forms:
- Rapidly Involuting Congenital Hemangiomas (RICH). These lesions are large high-flow lesions that are completely formed at birth but rapidly involute by 12 to 15 months. They can ulcerate and bleed and can cause transient heart failure and mild coagulopathy. After involution, usually some residual changes in the skin are present (refer to Figure 5).[82-85]
- Partial Involuting Congenital Hemangiomas (PICH). These lesions are completely formed at birth and involute only partially.[86]
Benign Vascular Tumors of the Liver
In the literature, vascular liver tumors are usually classified as liver hemangioendotheliomas, a broad classification no longer in use. These tumors are classified according to their clinical characteristics and radiologic assessment.
Lesions are usually divided into the following three categories:[45]
On MRI, vascular liver tumors are hyperintense on T2 imaging and hypointense on T1 imaging, with postcontrast imaging demonstrating early peripheral enhancement with eventual diffuse enhancement.[45]
Focal vascular lesions (congenital hemangiomas)
Focal lesions of the liver are usually congenital hemangiomas (RICH or NICH) (refer to Figure 6). RICH can present with symptoms of heart failure and mild to moderate coagulopathy.
Treatment options for focal vascular lesions include the following:
- Supportive management.
- Embolization for symptomatic shunting. These procedures need to be performed by interventional radiologists with expertise in vascular anomalies.[89]
- Surgery. Patients with focal symptomatic hepatic congenital hemangioma unresponsive to supportive management or radiological intervention may be surgical candidates for resection. This is a rare circumstance and needs to be evaluated by an interdisciplinary vascular anomaly team.
No medication has proven to be an effective treatment for these lesions, and infants need to be supported during this initial period until involution begins.[45] These lesions may be diagnosed prenatally. In rare situations, maternal treatment with medications such as steroids appeared to be effective but, more likely, natural involution may have been responsible.[90]
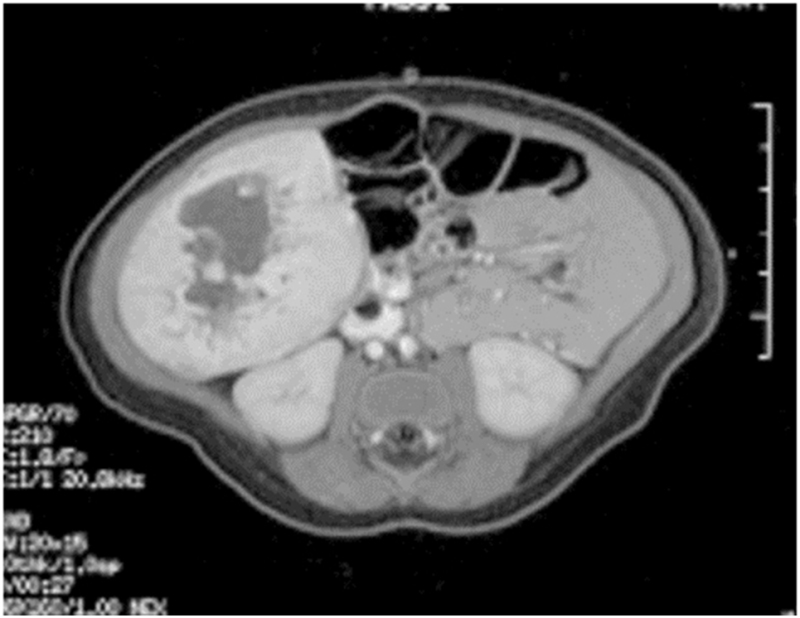
Figure 6. Single liver lesion (intrahepatic congenital hemangioma). MRI image of a congenital hemangioma. Note the central enhancement, which is typical for an intrahepatic congenital hemangioma. Credit: Denise Adams, M.D.
Multiple liver lesions (infantile hemangiomas)
Multifocal hepatic lesions are infantile hemangiomas. Multifocal lesions may not need to be treated if the patient is asymptomatic, and they typically follow the same proliferative and involution course as cutaneous hemangiomas.[45] These lesions are monitored closely and if there is growth, propranolol therapy should be considered. If propranolol is needed, doses of up to 2 mg/kg per day are effective.
Diffuse liver lesions (infantile hemangiomas)
Diffuse liver lesions can be very serious (refer to Figure 7). Complications include hypothyroidism caused by the expression of iodothyronine deiodinase, congestive heart failure, and compartment syndrome.[44,45,91,92]
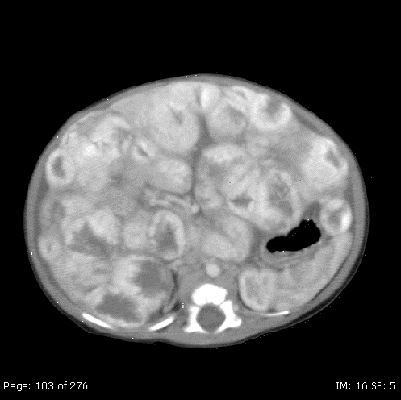
Figure 7. Diffuse liver lesions with classical imaging on CT. Note the peripheral enhancement in early contrast phase. Credit: Denise Adams, M.D.
Treatment options for diffuse liver lesions may include the following:
- Propranolol: Beta-blockers are the most common treatment for diffuse and some multifocal infantile hemangiomas of the liver. Treatment doses of 2 to 3 mg/kg per day are indicated.[51]
- Transplant: If a patient does not respond to medical management, a transplant may be indicated.[95] Transplantation is considered only for patients with severe diffuse lesions who have multisystem organ failure and there is insufficient time for effective pharmacologic therapy.
There have been isolated reports of malignancy in patients with diffuse hepatic infantile hemangiomas.[96] It is not clear if all cases were transformation of a benign lesion to a malignant phenotype; however, if the lesion does not respond to standard therapy, biopsy should be considered. Further evaluation and consensus is needed to assess whether these patients need to be monitored over a longer period of time with liver ultrasound. (Refer to the Angiosarcoma of the Soft Tissue section of this summary for more information.)
The differential diagnosis of vascular liver lesions always includes malignant liver tumors; thus, alpha-fetoprotein (AFP) should be included in the initial lab work. AFP can be elevated above baseline in congenital and infantile hemangiomas of the liver, but will rapidly fall to normal levels in 1 to 2 months, although there are no prospective studies investigating AFP elevation.[97,98] Some hypervascular hepatoblastomas in neonates with congestive heart failure have been mistaken for infantile hemangiomas. Other tumors in the differential diagnosis include angiosarcoma, metastatic neuroblastoma, and mesenchymal hamartomas. If there is any question about the diagnosis, a biopsy is recommended, although bleeding is a risk of the procedure.[99]
Spindle Cell Hemangioma
Clinical presentation
Spindle cell hemangiomas, initially called spindle cell hemangioendotheliomas, often occur as superficial (skin and subcutis), painful lesions involving distal extremities in children and adults.[100,101] The tumors appear as red-brown or bluish lesions that can begin as a single nodule and develop into multifocal painful lesions over years. The lesions can be seen in Maffucci syndrome (cutaneous spindle cell hemangiomas occurring with cartilaginous tumors, enchondromas) and Klippel-Trenaunay syndrome (capillary/lymphatic/venous malformations), generalized lymphatic anomalies, lymphedema, and organized thrombus.[102,103]
These tumors are well circumscribed, occasionally contain phleboliths, and consist of cavernous blood spaces alternating with areas of nodular spindle cell proliferation. A significant percentage of spindle cell hemangiomas are completely intravascular. The vein containing the tumor is abnormal, as are blood vessels apart from the tumor mass.[102,103]
Epithelioid Hemangioma
Clinical presentation
Epithelioid hemangiomas are benign lesions that usually occur in the skin and subcutis but can occur in other areas such as the bone, with focal and multifocal lesions.[102,104] Epithelioid hemangiomas may be a reactive process, as they can be associated with local trauma and can develop in pregnancy. Patients usually present with local swelling and pain at the involved site. In the bone, they present as well-defined lytic lesions that involve the metaphysis and diaphysis of long bones.[102,105] They can have a mixed lytic and sclerotic pattern of bone destruction.
On pathologic evaluation, they have small caliber capillaries with eosinophilic, vacuolated cytoplasm and large oval, grooved, and lobulated nuclei. The endothelial cells are plump and are mature, well-formed vessels surrounded by multiple epithelioid endothelial cells within abundant cytoplasm. They lack cellular atypia and mitotic activity.[102,104,105]
Pyogenic Granuloma (Lobular Capillary Hemangioma)
Clinical presentation
Pyogenic granuloma, known as lobular capillary hemangioma, is a benign reactive lesion that can present at any age, including infancy, although it is most common in older children and young adults. They can present as single or multiple lesions.[106-109] These lesions can arise spontaneously, in sites of trauma, or within capillary and arteriovenous malformations. Pyogenic granulomas have also been associated with medications including oral contraceptives and retinoids. Most occur as solitary growths, but multiple (grouped) or rarely disseminated lesions have been described. These lesions appear as small or large, smooth or lobulated vascular nodules that can grow rapidly, sometimes over weeks to months and have a tendency to bleed profusely.
Histologically, these lesions are composed of capillaries and venules with plump endothelial cells separated into lobules by fibromyxoid stroma. Some untreated lesions eventually atrophy, become fibromatous, and slowly regress.
Treatment of pyogenic granuloma
Treatment often consists of full-thickness excision, curettage, or laser photocoagulation, but recurrence is common.[110] A small case series of four patients with acquired ocular surface pyogenic granulomas were treated with topical timolol 0.5% twice daily for 21 days. In all cases, complete resolution with no recurrence occurred for at least 3 months. More studies are needed to validate these findings.[111]
Angiofibroma
Clinical presentation
Angiofibromas are rare, benign neoplasms in the pediatric population. Typically, they are cutaneous lesions associated with tuberous sclerosis, appearing as red papules on the face.
Juvenile Nasopharyngeal Angiofibroma
Clinical presentation
Juvenile nasopharyngeal angiofibromas (JNA) account for 0.5% of all head and neck tumors.[114] Histologically, juvenile nasopharyngeal angiofibromas are benign vascular tumors but they can be locally destructive, spreading from the nasal cavity to the nasopharynx, paranasal sinuses, and orbit skull base, with intracranial extension. Some publications have suggested a hormonal influence on juvenile nasopharyngeal angiofibroma, with emphasis on the molecular mechanisms involved.[115,116]
Treatment of juvenile nasopharyngeal angiofibroma
Surgical excision is the treatment of choice but this can be challenging because of the extent of the lesion. A single-institution retrospective review of juvenile nasopharyngeal angiofibromas identified 37 patients with lateral extension.[117] Anterior lateral extension to the pterygopalatine fossa occurred in 36 patients (97%) and further to the infratemporal fossa in 20 patients (54%). In 16 patients (43%), posterior lateral spread was observed (posterior to the pterygoid process and/or between its plates). The recurrence rate was 29.7% (11 of 37 patients). The recurrence rate in patients with anterior and/or posterior lateral extension was significantly higher than in patients with anterior lateral extension only.
Juvenile nasopharyngeal angiofibromas have also been treated with radiation therapy, chemotherapy, alpha-interferon therapy, and sirolimus.[118-121]
References
- Munden A, Butschek R, Tom WL, et al.: Prospective study of infantile haemangiomas: incidence, clinical characteristics and association with placental anomalies. Br J Dermatol 170 (4): 907-13, 2014. [PMC free article: PMC4410180] [PubMed: 24641194]
- Darrow DH, Greene AK, Mancini AJ, et al.: Diagnosis and Management of Infantile Hemangioma. Pediatrics 136 (4): e1060-104, 2015. [PubMed: 26416931]
- Darrow DH, Greene AK, Mancini AJ, et al.: Diagnosis and Management of Infantile Hemangioma: Executive Summary. Pediatrics 136 (4): 786-91, 2015. [PubMed: 26416928]
- Haggstrom AN, Drolet BA, Baselga E, et al.: Prospective study of infantile hemangiomas: demographic, prenatal, and perinatal characteristics. J Pediatr 150 (3): 291-4, 2007. [PubMed: 17307549]
- Blei F, Walter J, Orlow SJ, et al.: Familial segregation of hemangiomas and vascular malformations as an autosomal dominant trait. Arch Dermatol 134 (6): 718-22, 1998. [PubMed: 9645641]
- Castrén E, Salminen P, Vikkula M, et al.: Inheritance Patterns of Infantile Hemangioma. Pediatrics 138 (5): , 2016. [PubMed: 27940781]
- Boye E, Yu Y, Paranya G, et al.: Clonality and altered behavior of endothelial cells from hemangiomas. J Clin Invest 107 (6): 745-52, 2001. [PMC free article: PMC208946] [PubMed: 11254674]
- Yu Y, Flint AF, Mulliken JB, et al.: Endothelial progenitor cells in infantile hemangioma. Blood 103 (4): 1373-5, 2004. [PubMed: 14576053]
- Barnés CM, Huang S, Kaipainen A, et al.: Evidence by molecular profiling for a placental origin of infantile hemangioma. Proc Natl Acad Sci U S A 102 (52): 19097-102, 2005. [PMC free article: PMC1323205] [PubMed: 16365311]
- Walter JW, North PE, Waner M, et al.: Somatic mutation of vascular endothelial growth factor receptors in juvenile hemangioma. Genes Chromosomes Cancer 33 (3): 295-303, 2002. [PubMed: 11807987]
- Ritter MR, Dorrell MI, Edmonds J, et al.: Insulin-like growth factor 2 and potential regulators of hemangioma growth and involution identified by large-scale expression analysis. Proc Natl Acad Sci U S A 99 (11): 7455-60, 2002. [PMC free article: PMC124252] [PubMed: 12032304]
- Takahashi K, Mulliken JB, Kozakewich HP, et al.: Cellular markers that distinguish the phases of hemangioma during infancy and childhood. J Clin Invest 93 (6): 2357-64, 1994. [PMC free article: PMC294441] [PubMed: 7911127]
- Ritter MR, Reinisch J, Friedlander SF, et al.: Myeloid cells in infantile hemangioma. Am J Pathol 168 (2): 621-8, 2006. [PMC free article: PMC1606494] [PubMed: 16436675]
- Bielenberg DR, Bucana CD, Sanchez R, et al.: Progressive growth of infantile cutaneous hemangiomas is directly correlated with hyperplasia and angiogenesis of adjacent epidermis and inversely correlated with expression of the endogenous angiogenesis inhibitor, IFN-beta. Int J Oncol 14 (3): 401-8, 1999. [PubMed: 10024670]
- North PE, Waner M, Mizeracki A, et al.: A unique microvascular phenotype shared by juvenile hemangiomas and human placenta. Arch Dermatol 137 (5): 559-70, 2001. [PubMed: 11346333]
- Colonna V, Resta L, Napoli A, et al.: Placental hypoxia and neonatal haemangioma: clinical and histological observations. Br J Dermatol 162 (1): 208-9, 2010. [PubMed: 19863512]
- de Jong S, Itinteang T, Withers AH, et al.: Does hypoxia play a role in infantile hemangioma? Arch Dermatol Res 308 (4): 219-27, 2016. [PubMed: 26940670]
- Chang LC, Haggstrom AN, Drolet BA, et al.: Growth characteristics of infantile hemangiomas: implications for management. Pediatrics 122 (2): 360-7, 2008. [PubMed: 18676554]
- Tollefson MM, Frieden IJ: Early growth of infantile hemangiomas: what parents' photographs tell us. Pediatrics 130 (2): e314-20, 2012. [PubMed: 22826568]
- Munabi NC, Tan QK, Garzon MC, et al.: Growth Hormone Induces Recurrence of Infantile Hemangiomas After Apparent Involution: Evidence of Growth Hormone Receptors in Infantile Hemangioma. Pediatr Dermatol 32 (4): 539-43, 2015 Jul-Aug. [PMC free article: PMC5433863] [PubMed: 25690955]
- Baselga E, Roe E, Coulie J, et al.: Risk Factors for Degree and Type of Sequelae After Involution of Untreated Hemangiomas of Infancy. JAMA Dermatol 152 (11): 1239-1243, 2016. [PubMed: 27540637]
- Dubois J, Patriquin HB, Garel L, et al.: Soft-tissue hemangiomas in infants and children: diagnosis using Doppler sonography. AJR Am J Roentgenol 171 (1): 247-52, 1998. [PubMed: 9648798]
- Ma EH, Robertson SJ, Chow CW, et al.: Infantile Hemangioma with Minimal or Arrested Growth: Further Observations on Clinical and Histopathologic Findings of this Unique but Underrecognized Entity. Pediatr Dermatol 34 (1): 64-71, 2017. [PubMed: 27873347]
- Elluru RG, Friess MR, Richter GT, et al.: Multicenter Evaluation of the Effectiveness of Systemic Propranolol in the Treatment of Airway Hemangiomas. Otolaryngol Head Neck Surg 153 (3): 452-60, 2015. [PubMed: 26124263]
- Xue L, Sun C, Xu DP, et al.: Clinical Outcomes of Infants With Periorbital Hemangiomas Treated With Oral Propranolol. J Oral Maxillofac Surg 74 (11): 2193-2199, 2016. [PubMed: 27235180]
- Metry DW, Garzon MC, Drolet BA, et al.: PHACE syndrome: current knowledge, future directions. Pediatr Dermatol 26 (4): 381-98, 2009 Jul-Aug. [PubMed: 19689512]
- Frieden IJ, Reese V, Cohen D: PHACE syndrome. The association of posterior fossa brain malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, and eye abnormalities. Arch Dermatol 132 (3): 307-11, 1996. [PubMed: 8607636]
- Metry D, Heyer G, Hess C, et al.: Consensus Statement on Diagnostic Criteria for PHACE Syndrome. Pediatrics 124 (5): 1447-56, 2009. [PubMed: 19858157]
- Metry DW, Haggstrom AN, Drolet BA, et al.: A prospective study of PHACE syndrome in infantile hemangiomas: demographic features, clinical findings, and complications. Am J Med Genet A 140 (9): 975-86, 2006. [PubMed: 16575892]
- Drolet BA, Dohil M, Golomb MR, et al.: Early stroke and cerebral vasculopathy in children with facial hemangiomas and PHACE association. Pediatrics 117 (3): 959-64, 2006. [PubMed: 16510684]
- Heyer GL, Dowling MM, Licht DJ, et al.: The cerebral vasculopathy of PHACES syndrome. Stroke 39 (2): 308-16, 2008. [PubMed: 18174492]
- Haggstrom AN, Garzon MC, Baselga E, et al.: Risk for PHACE syndrome in infants with large facial hemangiomas. Pediatrics 126 (2): e418-26, 2010. [PubMed: 20643720]
- Poindexter G, Metry DW, Barkovich AJ, et al.: PHACE syndrome with intracerebral hemangiomas, heterotopia, and endocrine dysfunction. Pediatr Neurol 36 (6): 402-6, 2007. [PubMed: 17560503]
- Burrows PE, Robertson RL, Mulliken JB, et al.: Cerebral vasculopathy and neurologic sequelae in infants with cervicofacial hemangioma: report of eight patients. Radiology 207 (3): 601-7, 1998. [PubMed: 9609880]
- Hess CP, Fullerton HJ, Metry DW, et al.: Cervical and intracranial arterial anomalies in 70 patients with PHACE syndrome. AJNR Am J Neuroradiol 31 (10): 1980-6, 2010. [PMC free article: PMC5967888] [PubMed: 20705698]
- Yu J, Siegel DH, Drolet BA, et al.: Prevalence and Clinical Characteristics of Headaches in PHACE Syndrome. J Child Neurol 31 (4): 468-73, 2016. [PMC free article: PMC6457900] [PubMed: 26271792]
- Martin KL, Arvedson JC, Bayer ML, et al.: Risk of dysphagia and speech and language delay in PHACE syndrome. Pediatr Dermatol 32 (1): 64-9, 2015 Jan-Feb. [PubMed: 25440893]
- Chiu YE, Siegel DH, Drolet BA, et al.: Tooth enamel hypoplasia in PHACE syndrome. Pediatr Dermatol 31 (4): 455-8, 2014 Jul-Aug. [PubMed: 24916277]
- Duffy KJ, Runge-Samuelson C, Bayer ML, et al.: Association of hearing loss with PHACE syndrome. Arch Dermatol 146 (12): 1391-6, 2010. [PubMed: 20713775]
- Antonov NK, Spence-Shishido A, Marathe KS, et al.: Orbital Hemangioma with Intracranial Vascular Anomalies and Hemangiomas: A New Presentation of PHACE Syndrome? Pediatr Dermatol 32 (6): e267-72, 2015 Nov-Dec. [PubMed: 26446288]
- Iacobas I, Burrows PE, Frieden IJ, et al.: LUMBAR: association between cutaneous infantile hemangiomas of the lower body and regional congenital anomalies. J Pediatr 157 (5): 795-801.e1-7, 2010. [PubMed: 20598318]
- Girard C, Bigorre M, Guillot B, et al.: PELVIS Syndrome. Arch Dermatol 142 (7): 884-8, 2006. [PubMed: 16847205]
- Stockman A, Boralevi F, Taïeb A, et al.: SACRAL syndrome: spinal dysraphism, anogenital, cutaneous, renal and urologic anomalies, associated with an angioma of lumbosacral localization. Dermatology 214 (1): 40-5, 2007. [PubMed: 17191046]
- Rialon KL, Murillo R, Fevurly RD, et al.: Risk factors for mortality in patients with multifocal and diffuse hepatic hemangiomas. J Pediatr Surg 50 (5): 837-41, 2015. [PubMed: 25783331]
- Hsi Dickie B, Fishman SJ, Azizkhan RG: Hepatic vascular tumors. Semin Pediatr Surg 23 (4): 168-72, 2014. [PubMed: 25241093]
- Huang SA, Tu HM, Harney JW, et al.: Severe hypothyroidism caused by type 3 iodothyronine deiodinase in infantile hemangiomas. N Engl J Med 343 (3): 185-9, 2000. [PubMed: 10900278]
- Kessels JP, Hamers ET, Ostertag JU: Superficial hemangioma: pulsed dye laser versus wait-and-see. Dermatol Surg 39 (3 Pt 1): 414-21, 2013. [PubMed: 23279058]
- Keller RG, Patel KG: Evidence-Based Medicine in the Treatment of Infantile Hemangiomas. Facial Plast Surg Clin North Am 23 (3): 373-92, 2015. [PubMed: 26208774]
- Sharifpanah F, Saliu F, Bekhite MM, et al.: β-Adrenergic receptor antagonists inhibit vasculogenesis of embryonic stem cells by downregulation of nitric oxide generation and interference with VEGF signalling. Cell Tissue Res 358 (2): 443-52, 2014. [PubMed: 25130141]
- Ma X, Zhao T, Ouyang T, et al.: Propranolol enhanced adipogenesis instead of induction of apoptosis of hemangiomas stem cells. Int J Clin Exp Pathol 7 (7): 3809-17, 2014. [PMC free article: PMC4128992] [PubMed: 25120757]
- Léauté-Labrèze C, Hoeger P, Mazereeuw-Hautier J, et al.: A randomized, controlled trial of oral propranolol in infantile hemangioma. N Engl J Med 372 (8): 735-46, 2015. [PubMed: 25693013]
- Bauman NM: Propanolol effectively treats significant infantile hemangiomas. J Pediatr 167 (1): 210, 2015. [PubMed: 26117643]
- Chang L, Ye X, Qiu Y, et al.: Is Propranolol Safe and Effective for Outpatient Use for Infantile Hemangioma? A Prospective Study of 679 Cases From One Center in China. Ann Plast Surg 76 (5): 559-63, 2016. [PubMed: 26101993]
- Ames JA, Sykes JM: Current trends in medical management of infantile hemangioma. Curr Opin Otolaryngol Head Neck Surg 23 (4): 286-91, 2015. [PubMed: 26101875]
- Lou Y, Peng WJ, Cao Y, et al.: The effectiveness of propranolol in treating infantile haemangiomas: a meta-analysis including 35 studies. Br J Clin Pharmacol 78 (1): 44-57, 2014. [PMC free article: PMC4168379] [PubMed: 24033819]
- Luo Y, Zeng Y, Zhou B, et al.: A retrospective study of propranolol therapy in 635 infants with infantile hemangioma. Pediatr Dermatol 32 (1): 151-2, 2015 Jan-Feb. [PubMed: 24602103]
- Vivas-Colmenares GV, Bernabeu-Wittel J, Alonso-Arroyo V, et al.: Effectiveness of propranolol in the treatment of infantile hemangioma beyond the proliferation phase. Pediatr Dermatol 32 (3): 348-52, 2015 May-Jun. [PubMed: 25721095]
- Liu X, Qu X, Zheng J, et al.: Effectiveness and Safety of Oral Propranolol versus Other Treatments for Infantile Hemangiomas: A Meta-Analysis. PLoS One 10 (9): e0138100, 2015. [PMC free article: PMC4573957] [PubMed: 26375455]
- Hardison S, Wan W, Dodson KM: The use of propranolol in the treatment of subglottic hemangiomas: A literature review and meta-analysis. Int J Pediatr Otorhinolaryngol 90: 175-180, 2016. [PubMed: 27729127]
- Drolet BA, Frommelt PC, Chamlin SL, et al.: Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics 131 (1): 128-40, 2013. [PMC free article: PMC3529954] [PubMed: 23266923]
- Hoeger PH, Harper JI, Baselga E, et al.: Treatment of infantile haemangiomas: recommendations of a European expert group. Eur J Pediatr 174 (7): 855-65, 2015. [PubMed: 26021855]
- Raphael MF, Breugem CC, Vlasveld FA, et al.: Is cardiovascular evaluation necessary prior to and during beta-blocker therapy for infantile hemangiomas?: A cohort study. J Am Acad Dermatol 72 (3): 465-72, 2015. [PubMed: 25592625]
- Prey S, Voisard JJ, Delarue A, et al.: Safety of Propranolol Therapy for Severe Infantile Hemangioma. JAMA 315 (4): 413-5, 2016. [PubMed: 26813215]
- Shah SD, Baselga E, McCuaig C, et al.: Rebound Growth of Infantile Hemangiomas After Propranolol Therapy. Pediatrics 137 (4): , 2016. [PubMed: 26952504]
- Ábarzúa-Araya A, Navarrete-Dechent CP, Heusser F, et al.: Atenolol versus propranolol for the treatment of infantile hemangiomas: a randomized controlled study. J Am Acad Dermatol 70 (6): 1045-9, 2014. [PubMed: 24656727]
- Bayart CB, Tamburro JE, Vidimos AT, et al.: Atenolol Versus Propranolol for Treatment of Infantile Hemangiomas During the Proliferative Phase: A Retrospective Noninferiority Study. Pediatr Dermatol 34 (4): 413-421, 2017. [PubMed: 28556385]
- Randhawa HK, Sibbald C, Garcia Romero MT, et al.: Oral Nadolol for the Treatment of Infantile Hemangiomas: A Single-Institution Retrospective Cohort Study. Pediatr Dermatol 32 (5): 690-5, 2015 Sep-Oct. [PubMed: 26215612]
- Ji Y, Wang Q, Chen S, et al.: Oral atenolol therapy for proliferating infantile hemangioma: A prospective study. Medicine (Baltimore) 95 (24): e3908, 2016. [PMC free article: PMC4998480] [PubMed: 27310994]
- Bernabeu-Wittel J, Narváez-Moreno B, de la Torre-García JM, et al.: Oral Nadolol for Children with Infantile Hemangiomas and Sleep Disturbances with Oral Propranolol. Pediatr Dermatol 32 (6): 853-7, 2015 Nov-Dec. [PubMed: 26447831]
- Chinnadurai S, Fonnesbeck C, Snyder KM, et al.: Pharmacologic Interventions for Infantile Hemangioma: A Meta-analysis. Pediatrics 137 (2): e20153896, 2016. [PubMed: 26772662]
- Xu DP, Cao RY, Tong S, et al.: Topical timolol maleate for superficial infantile hemangiomas: an observational study. J Oral Maxillofac Surg 73 (6): 1089-94, 2015. [PubMed: 25843815]
- Tawfik AA, Alsharnoubi J: Topical timolol solution versus laser in treatment of infantile hemangioma: a comparative study. Pediatr Dermatol 32 (3): 369-76, 2015 May-Jun. [PubMed: 25740672]
- Püttgen K, Lucky A, Adams D, et al.: Topical Timolol Maleate Treatment of Infantile Hemangiomas. Pediatrics 138 (3): , 2016. [PubMed: 27527799]
- Weibel L, Barysch MJ, Scheer HS, et al.: Topical Timolol for Infantile Hemangiomas: Evidence for Efficacy and Degree of Systemic Absorption. Pediatr Dermatol 33 (2): 184-90, 2016 Mar-Apr. [PubMed: 26840644]
- Frommelt P, Juern A, Siegel D, et al.: Adverse Events in Young and Preterm Infants Receiving Topical Timolol for Infantile Hemangioma. Pediatr Dermatol 33 (4): 405-14, 2016. [PubMed: 27246751]
- Aly MM, Hamza AF, Abdel Kader HM, et al.: Therapeutic superiority of combined propranolol with short steroids course over propranolol monotherapy in infantile hemangioma. Eur J Pediatr 174 (11): 1503-9, 2015. [PubMed: 25982338]
- Li G, Xu DP, Tong S, et al.: Oral Propranolol With Topical Timolol Maleate Therapy for Mixed Infantile Hemangiomas in Oral and Maxillofacial Regions. J Craniofac Surg 27 (1): 56-60, 2016. [PubMed: 26716547]
- Tong S, Xu DP, Liu ZM, et al.: Evaluation of the efficacy and safety of topical timolol maleate combined with oral propranolol treatment for parotid mixed infantile hemangiomas. Oncol Lett 12 (3): 1806-1810, 2016. [PMC free article: PMC4998099] [PubMed: 27588127]
- Ge J, Zheng J, Zhang L, et al.: Oral propranolol combined with topical timolol for compound infantile hemangiomas: a retrospective study. Sci Rep 6: 19765, 2016. [PMC free article: PMC4730155] [PubMed: 26819072]
- Vildy S, Macher J, Abasq-Thomas C, et al.: Life-threatening hemorrhaging in neonatal ulcerated congenital hemangioma: two case reports. JAMA Dermatol 151 (4): 422-5, 2015. [PubMed: 25565634]
- Ayturk UM, Couto JA, Hann S, et al.: Somatic Activating Mutations in GNAQ and GNA11 Are Associated with Congenital Hemangioma. Am J Hum Genet 98 (4): 789-95, 2016. [PMC free article: PMC4833432] [PubMed: 27058448]
- Maguiness S, Uihlein LC, Liang MG, et al.: Rapidly involuting congenital hemangioma with fetal involution. Pediatr Dermatol 32 (3): 321-6, 2015 May-Jun. [PubMed: 25492638]
- Scalise R, Bolton J, Gibbs NF: Rapidly involuting congenital hemangioma (RICH): a brief case report. Dermatol Online J 20 (11): , 2014. [PubMed: 25419759]
- Kumarasamy MT, Castrisios G, Sharma BK: Rapidly involuting congenital haemangioma in a term neonate. BMJ Case Rep 2014: , 2014. [PMC free article: PMC4024566] [PubMed: 24798357]
- Hughes R, McAleer M, Watson R, et al.: Rapidly involuting congenital hemangioma with pustules: two cases. Pediatr Dermatol 31 (3): 398-400, 2014 May-Jun. [PubMed: 24689686]
- Nasseri E, Piram M, McCuaig CC, et al.: Partially involuting congenital hemangiomas: a report of 8 cases and review of the literature. J Am Acad Dermatol 70 (1): 75-9, 2014. [PubMed: 24176519]
- Lee PW, Frieden IJ, Streicher JL, et al.: Characteristics of noninvoluting congenital hemangioma: a retrospective review. J Am Acad Dermatol 70 (5): 899-903, 2014. [PubMed: 24630000]
- Enjolras O, Mulliken JB, Boon LM, et al.: Noninvoluting congenital hemangioma: a rare cutaneous vascular anomaly. Plast Reconstr Surg 107 (7): 1647-54, 2001. [PubMed: 11391180]
- Kayaalp C, Sabuncuoglu MZ: Embolization of Liver Hemangiomas. Hepat Mon 15 (8): e30334, 2015. [PMC free article: PMC4546810] [PubMed: 26322113]
- Schmitz R, Heinig J, Klockenbusch W, et al.: Antenatal diagnosis of a giant fetal hepatic hemangioma and treatment with maternal corticosteroid. Ultraschall Med 30 (3): 223-6, 2009. [PubMed: 19507116]
- Rialon KL, Murillo R, Fevurly RD, et al.: Impact of Screening for Hepatic Hemangiomas in Patients with Multiple Cutaneous Infantile Hemangiomas. Pediatr Dermatol 32 (6): 808-12, 2015 Nov-Dec. [PubMed: 26223454]
- Yeh I, Bruckner AL, Sanchez R, et al.: Diffuse infantile hepatic hemangiomas: a report of four cases successfully managed with medical therapy. Pediatr Dermatol 28 (3): 267-75, 2011 May-Jun. [PubMed: 21517953]
- Wasserman JD, Mahant S, Carcao M, et al.: Vincristine for successful treatment of steroid-dependent infantile hemangiomas. Pediatrics 135 (6): e1501-5, 2015. [PubMed: 25986022]
- Vlahovic A, Simic R, Djokic D, et al.: Diffuse neonatal hemangiomatosis treatment with cyclophosphamide: a case report. J Pediatr Hematol Oncol 31 (11): 858-60, 2009. [PubMed: 19829152]
- Sundar Alagusundaramoorthy S, Vilchez V, Zanni A, et al.: Role of transplantation in the treatment of benign solid tumors of the liver: a review of the United Network of Organ Sharing data set. JAMA Surg 150 (4): 337-42, 2015. [PubMed: 25714928]
- Jeng MR, Fuh B, Blatt J, et al.: Malignant transformation of infantile hemangioma to angiosarcoma: response to chemotherapy with bevacizumab. Pediatr Blood Cancer 61 (11): 2115-7, 2014. [PubMed: 24740626]
- Sari N, Yalçin B, Akyüz C, et al.: Infantile hepatic hemangioendothelioma with elevated serum alpha-fetoprotein. Pediatr Hematol Oncol 23 (8): 639-47, 2006. [PubMed: 17065140]
- Seo IS, Min KW, Mirkin LD: Hepatic hemangioendothelioma of infancy associated with elevated alpha fetoprotein and catecholamine by-products. Pediatr Pathol 8 (6): 625-31, 1988. [PubMed: 2469076]
- Langham MR Jr, Furman WL, Fernandez-Pineda I: Current Management of Neonatal Liver Tumors. Curr Pediatr Rev 11 (3): 195-204, 2015. [PubMed: 26168944]
- Perkins P, Weiss SW: Spindle cell hemangioendothelioma. An analysis of 78 cases with reassessment of its pathogenesis and biologic behavior. Am J Surg Pathol 20 (10): 1196-204, 1996. [PubMed: 8827025]
- Fletcher CD, Beham A, Schmid C: Spindle cell haemangioendothelioma: a clinicopathological and immunohistochemical study indicative of a non-neoplastic lesion. Histopathology 18 (4): 291-301, 1991. [PubMed: 2071088]
- Enjolras O, Mulliken JB, Kozakewich HPW: Vascular tumors and tumor-like lesions. In: Mulliken JB, Burrows PE, Fishman SJ, eds.: Mulliken & Young's Vascular Anomalies: Hemangiomas and Malformations. 2nd ed. New York, NY: Oxford University Press, 2013, pp 259-324.
- Hoeger PH, Colmenero I: Vascular tumours in infants. Part I: benign vascular tumours other than infantile haemangioma. Br J Dermatol 171 (3): 466-73, 2014. [PubMed: 24117053]
- Guo R, Gavino AC: Angiolymphoid hyperplasia with eosinophilia. Arch Pathol Lab Med 139 (5): 683-6, 2015. [PubMed: 25927152]
- O'Connell JX, Nielsen GP, Rosenberg AE: Epithelioid vascular tumors of bone: a review and proposal of a classification scheme. Adv Anat Pathol 8 (2): 74-82, 2001. [PubMed: 11236956]
- Wassef M, Hunt SF, Santa Cruz DJ: Vascular tumors and vascular malformations. In: Barnhi RL, Crowson AN, Magro CM, et al., eds.: Dermatopathology. 3rd ed. New York, NY: McGraw Hill Medical, 2010, pp 802-56.
- Swerlick RA, Cooper PH: Pyogenic granuloma (lobular capillary hemangioma) within port-wine stains. J Am Acad Dermatol 8 (5): 627-30, 1983. [PubMed: 6863618]
- Campbell JP, Grekin RC, Ellis CN, et al.: Retinoid therapy is associated with excess granulation tissue responses. J Am Acad Dermatol 9 (5): 708-13, 1983. [PubMed: 6227639]
- Mills SE, Cooper PH, Fechner RE: Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 4 (5): 470-9, 1980. [PubMed: 7435775]
- Patrizi A, Gurioli C, Dika E: Pyogenic granulomas in childhood: New treatment modalities. Dermatol Ther 28 (5): 332, 2015 Sep-Oct. [PubMed: 25818498]
- Oke I, Alkharashi M, Petersen RA, et al.: Treatment of Ocular Pyogenic Granuloma With Topical Timolol. JAMA Ophthalmol 135 (4): 383-385, 2017. [PubMed: 28301661]
- Haemel AK, O'Brian AL, Teng JM: Topical rapamycin: a novel approach to facial angiofibromas in tuberous sclerosis. Arch Dermatol 146 (7): 715-8, 2010. [PubMed: 20644030]
- Pignatti M, Spaggiari A, Sala P, et al.: Laser treatment of angiofibromas in tuberous sclerosis. Minerva Pediatr 66 (6): 585-6, 2014. [PubMed: 25336102]
- Coutinho-Camillo CM, Brentani MM, Nagai MA: Genetic alterations in juvenile nasopharyngeal angiofibromas. Head Neck 30 (3): 390-400, 2008. [PubMed: 18228521]
- Riggs S, Orlandi RR: Juvenile nasopharyngeal angiofibroma recurrence associated with exogenous testosterone therapy. Head Neck 32 (6): 812-5, 2010. [PubMed: 19626637]
- Liu Z, Wang J, Wang H, et al.: Hormonal receptors and vascular endothelial growth factor in juvenile nasopharyngeal angiofibroma: immunohistochemical and tissue microarray analysis. Acta Otolaryngol 135 (1): 51-7, 2015. [PubMed: 25384380]
- Szymańska A, Szymański M, Czekajska-Chehab E, et al.: Two types of lateral extension in juvenile nasopharyngeal angiofibroma: diagnostic and therapeutic management. Eur Arch Otorhinolaryngol 272 (1): 159-66, 2015. [PMC free article: PMC4282713] [PubMed: 24599598]
- Samanta D: Topical mTOR (mechanistic target of rapamycin) inhibitor therapy in facial angiofibroma. Indian J Dermatol Venereol Leprol 81 (5): 540-1, 2015 Sep-Oct. [PubMed: 26323682]
- Krakowski AC, Nguyen TA: Inhibition of Angiofibromas in a Tuberous Sclerosis Patient Using Topical Timolol 0.5% Gel. Pediatrics 136 (3): e709-13, 2015. [PubMed: 26304829]
- Mallick S, Benson R, Bhasker S, et al.: Long-term treatment outcomes of juvenile nasopharyngeal angiofibroma treated with radiotherapy. Acta Otorhinolaryngol Ital 35 (2): 75-9, 2015. [PMC free article: PMC4443565] [PubMed: 26019389]
- Peters T, Traboulsi D, Tibbles LA, et al.: Sirolimus: a therapeutic advance for dermatologic disease. Skin Therapy Lett 19 (4): 1-4, 2014 Jul-Aug. [PubMed: 25188522]
Intermediate Tumors (Locally Aggressive)
Kaposiform Hemangioendothelioma and Tufted Angioma
Kaposiform hemangioendothelioma (KHE) and tufted angioma are rare vascular tumors that typically occur during infancy or early childhood but have been reported in adults. Both tumors are thought to be a spectrum of the same disease, because both can be locally aggressive and cause Kasabach-Merritt phenomenon, a serious life-threatening coagulopathy characterized by profound thrombocytopenia and hypofibrinogenemia. They are discussed here as a single entity, kaposiform hemangioendothelioma.
Incidence
The exact incidence of kaposiform hemangioendothelioma is unknown but is estimated to be 0.07 cases per 100,000 children per year.[1-3] The lesions affect both sexes equally, with most developing in the neonatal period, one-half presenting at birth, and others presenting during childhood or adulthood.[4]
Pathology
Kaposiform hemangioendothelioma is characterized by sheets of spindle cells with an infiltrative pattern in the dermis, subcutaneous fat, and muscle. There are often areas of fibrosis, with dilated thin-walled vessels infiltrated around the areas of spindle cells. Mixed with these areas are nests of rounded epithelioid cells of vascular origin and aggregates of capillaries with round or irregularly shaped lumens containing platelet-rich fibrin thrombi. There is usually the presence of abnormal lymphatic spaces, either within or at the periphery of the lesion. The rate of mitosis is variable but usually low. Tufted angioma is characterized by multiple, discrete lobules of tightly packed capillaries (tufts) scattered in the dermis and sometimes in the subcutis, so called cannonball pattern.[5] Mitoses are rare.
The pathogenesis is poorly understood. There is some evidence that kaposiform hemangioendothelioma may be derived from lymphatic endothelium, as the spindle cell expresses the vascular markers CD31 and CD34, the vascular endothelial growth factor receptor-3, a receptor required for lymphangiogenesis, and the lymphatic markers D2-40 and PROX1.[5-7] There is no evidence of association with human herpesvirus 8 infection as is present in Kaposi sarcoma.[7]
Clinical presentation
Kaposiform hemangioendothelioma most frequently involves the extremities and less frequently involves the trunk and head and neck area.[3] Most lesions involve the skin (refer to Figure 8). Deeper lesions (retroperitoneum, thoracic cavity, and muscle) can appear as a bluish-purpuric hue on the skin, whereas superficial lesions can be firm, purpuric or ecchymotic, and painful. Lesions are usually unifocal and growth is contiguous. Local lymph nodes may be involved, but they never metastasize. Rare multifocal presentations have been reported mostly in the bone.[1-3]

Figure 8. Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon. The lesion is indurated, firm, and warm with petechiae and purpura. Credit: Denise Adams, M.D.
Seventy percent of patients with kaposiform hemangioendothelioma develop Kasabach-Merritt phenomenon, which is a life-threatening complication characterized by profound thrombocytopenia (range, 3,000/µL–60,000/µL) and profound hypofibrinogenemia (<1 g/L). D-dimer and fibrin degradation products are elevated. Severe anemia can occur secondary to tumor sequestration. Severe hemorrhage is rare; however, trauma (biopsy, surgical procedure), ulceration, infection, or delay in initiating treatment may induce progression to disseminated intravascular coagulation and serious bleeding and death can occur. Aggressive replacement of blood products, especially platelets, can increase the size of the lesion, causing significant pain and should only be considered with active bleeding and under the direction of a vascular anomaly specialist.[3]
Diagnostic evaluation
The diagnosis is based on the combination of clinical, histologic, and imaging features. Laboratory evaluation is essential for the diagnosis of Kasabach-Merritt phenomenon. Whenever possible, histologic confirmation should be obtained, because prolonged therapy is often needed. However, if clinical and imaging findings are highly suggestive of the diagnosis, deferring biopsy is an option but needs to be planned with an interdisciplinary approach.
Magnetic resonance imaging is the imaging preference. T1-weighted sequences typically show a poorly circumscribed soft tissue mass with soft tissue and dermal thickening and diffuse enhancement with gadolinium. T2-weighted sequences show a diffuse increased signal, with stranding in the subcutaneous fat. Gradient sequences show mildly dilated vessels in and around the soft-tissue mass.[3]
Treatment of kaposiform hemangioendothelioma and tufted angioma
Treatment varies according to severity; there is no evidence-based standard of care. An American and Canadian multidisciplinary expert panel published guidelines for the management of complicated kaposiform hemangioendothelioma.[8] A number of treatment therapies have been reported but none have been uniformly effective.[9,10]
Treatment options for kaposiform hemangioendothelioma include the following:[8-17]
- Steroid therapy.
- Antiplatelet agent (aspirin) therapy.
- Alpha-interferon.
- Antifibrinolytic agent therapy.
- Chemotherapy, including vincristine, cyclophosphamide, actinomycin, and methotrexate used alone or in combination.
- Propranolol therapy.
- Surgical excision with or without embolization.
- Sirolimus as a single agent or in combination with steroids.
Initial treatment is most commonly steroids followed by vincristine. A retrospective review identified 37 children with kaposiform hemangioendothelioma whose lesions did not respond to steroids.[11][Level of evidence: 3iiiDiv] Twenty-six kaposiform hemangioendothelioma lesions achieved complete remission, with platelet counts reaching normal levels within 7.6 ± 5.2 weeks after vincristine treatment.
Propranolol therapy has been reported as a treatment option for kaposiform hemangioendothelioma. Its use is based on the positive results of propranolol for other more benign vascular tumors. Results have been mixed, with a report of improved effectiveness using higher doses of propranolol.[18,19] Preliminary results indicate that propranolol should be reserved for patients with kaposiform hemangioendothelioma without Kasabach-Merritt phenomenon and with smaller, less complicated lesions.
Secondary to promising case reports, case series and a prospective clinical trial, sirolimus may be considered an alternative first-line therapy for kaposiform hemangioendothelioma.[14,15,20] There are limited studies investigating its effect on kaposiform hemangioendothelioma/tufted angioma without Kasabach-Merritt phenomenon.
Reports that support the use of sirolimus include the following:
- In a prospective study that assessed the efficacy and safety of sirolimus for the treatment of complicated vascular anomalies, 13 patients with kaposiform hemangioendothelioma were treated.[21]
- In patients with kaposiform hemangioendothelioma and Kasabach-Merritt phenomenon, ten of ten patients had a partial response, with normalization of their platelet count and fibrinogen at the end of six and 12 courses.
- In three of three patients with kaposiform hemangioendothelioma without Kasabach-Merritt phenomenon, one patient with multifocal bony disease had disease progression while the other two patients revealed a partial response at the end of course 12. Side effects were minimal in this group of young patients and no patient with kaposiform hemangioendothelioma required a dose adjustment or was removed from study secondary to toxicity.
- A single case report of a child with kaposiform hemangioendothelioma who developed recurrence of pain and fibrosis years after initial therapy and was treated with sirolimus for 26 months observed the following:[20]
- The patient's contracture and range of motion improved, the lesion shrank, and the child was well 2 years later.
- In a multicenter, retrospective cohort study, 52 Chinese patients with progressive kaposiform hemangioendothelioma were analyzed. Thirty-seven patients (71%) had Kasabach-Merritt phenomenon. Those without Kasabach-Merritt phenomenon received sirolimus alone, and 21 of the patients with Kasabach-Merritt phenomenon received a combination of sirolimus and prednisone.[22]
- Overall, 96% and 98% of patients demonstrated improvement in notable symptoms and/or had improved complications at 6 and 12 months, respectively.
Additional studies are needed to determine the long-term efficacy and safety of sirolimus for the treatment of vascular tumors associated with Kasabach-Merritt phenomenon.
Surgical excision may be possible for lesions that are smaller, have failed medical management, or are life threatening. Embolization may be performed in conjunction with surgery or medical therapy; usually it is a temporizing measure.
The mortality associated with this tumor is primarily from the extensive coagulopathy associated with Kasabach-Merritt phenomenon.
Even with therapy, these lesions do not fully regress and can recur; worsened symptomatology (pain, inflammation) can occur with age, especially around the time of puberty.[23]
Long-term effects include chronic pain, lymphedema, heart failure, and orthopedic issues.[23] These lesions prove to be a difficult dilemma for the practitioner because they have a varied clinical spectrum and response to therapy.
Treatment options under clinical evaluation for kaposiform hemangioendothelioma
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following is an example of national and/or institutional clinical trial that is currently being conducted:
- NCT02110069 (A Study to Compare Vincristine to Sirolimus for Treatment of High-Risk Vascular Tumors): This is a study comparing vincristine with sirolimus for the treatment of high-risk kaposiform hemangioendothelioma. A multicenter adaptive study design determining efficacy (initially defined as the time to hematologic response) by comparing vincristine with sirolimus therapy while patients are on a steroid wean.
References
- Rodriguez V, Lee A, Witman PM, et al.: Kasabach-merritt phenomenon: case series and retrospective review of the mayo clinic experience. J Pediatr Hematol Oncol 31 (7): 522-6, 2009. [PubMed: 19564750]
- Ryan C, Price V, John P, et al.: Kasabach-Merritt phenomenon: a single centre experience. Eur J Haematol 84 (2): 97-104, 2010. [PubMed: 19889011]
- Croteau SE, Liang MG, Kozakewich HP, et al.: Kaposiform hemangioendothelioma: atypical features and risks of Kasabach-Merritt phenomenon in 107 referrals. J Pediatr 162 (1): 142-7, 2013. [PMC free article: PMC3494787] [PubMed: 22871490]
- Lee B, Chiu M, Soriano T, et al.: Adult-onset tufted angioma: a case report and review of the literature. Cutis 78 (5): 341-5, 2006. [PubMed: 17186794]
- Enjolras O, Soupre V, Picard A: Uncommon benign infantile vascular tumors. Adv Dermatol 24: 105-24, 2008. [PubMed: 19263597]
- Zukerberg LR, Nickoloff BJ, Weiss SW: Kaposiform hemangioendothelioma of infancy and childhood. An aggressive neoplasm associated with Kasabach-Merritt syndrome and lymphangiomatosis. Am J Surg Pathol 17 (4): 321-8, 1993. [PubMed: 8494101]
- Arai E, Kuramochi A, Tsuchida T, et al.: Usefulness of D2-40 immunohistochemistry for differentiation between kaposiform hemangioendothelioma and tufted angioma. J Cutan Pathol 33 (7): 492-7, 2006. [PubMed: 16872472]
- Drolet BA, Trenor CC 3rd, Brandão LR, et al.: Consensus-derived practice standards plan for complicated Kaposiform hemangioendothelioma. J Pediatr 163 (1): 285-91, 2013. [PubMed: 23796341]
- Haisley-Royster C, Enjolras O, Frieden IJ, et al.: Kasabach-merritt phenomenon: a retrospective study of treatment with vincristine. J Pediatr Hematol Oncol 24 (6): 459-62, 2002 Aug-Sep. [PubMed: 12218593]
- Hauer J, Graubner U, Konstantopoulos N, et al.: Effective treatment of kaposiform hemangioendotheliomas associated with Kasabach-Merritt phenomenon using four-drug regimen. Pediatr Blood Cancer 49 (6): 852-4, 2007. [PubMed: 16411198]
- Wang Z, Li K, Yao W, et al.: Steroid-resistant kaposiform hemangioendothelioma: a retrospective study of 37 patients treated with vincristine and long-term follow-up. Pediatr Blood Cancer 62 (4): 577-80, 2015. [PubMed: 25346262]
- Fernandez-Pineda I, Lopez-Gutierrez JC, Ramirez G, et al.: Vincristine-ticlopidine-aspirin: an effective therapy in children with Kasabach-Merritt phenomenon associated with vascular tumors. Pediatr Hematol Oncol 27 (8): 641-5, 2010. [PubMed: 20863161]
- Kai L, Wang Z, Yao W, et al.: Sirolimus, a promising treatment for refractory Kaposiform hemangioendothelioma. J Cancer Res Clin Oncol 140 (3): 471-6, 2014. [PubMed: 24464150]
- Hammill AM, Wentzel M, Gupta A, et al.: Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer 57 (6): 1018-24, 2011. [PubMed: 21445948]
- Blatt J, Stavas J, Moats-Staats B, et al.: Treatment of childhood kaposiform hemangioendothelioma with sirolimus. Pediatr Blood Cancer 55 (7): 1396-8, 2010. [PubMed: 20730884]
- Fernandez-Pineda I, Lopez-Gutierrez JC, Chocarro G, et al.: Long-term outcome of vincristine-aspirin-ticlopidine (VAT) therapy for vascular tumors associated with Kasabach-Merritt phenomenon. Pediatr Blood Cancer 60 (9): 1478-81, 2013. [PubMed: 23609996]
- Chiu YE, Drolet BA, Blei F, et al.: Variable response to propranolol treatment of kaposiform hemangioendothelioma, tufted angioma, and Kasabach-Merritt phenomenon. Pediatr Blood Cancer 59 (5): 934-8, 2012. [PMC free article: PMC3528889] [PubMed: 22648868]
- Filippi L, Tamburini A, Berti E, et al.: Successful Propranolol Treatment of a Kaposiform Hemangioendothelioma Apparently Resistant to Propranolol. Pediatr Blood Cancer 63 (7): 1290-2, 2016. [PubMed: 27100060]
- Wang Z, Li K, Dong K, et al.: Variable response to propranolol treatment of kaposiform hemangioendothelioma, tufted angioma, and Kasabach-Merritt phenomenon. Pediatr Blood Cancer 61 (8): 1518-9, 2014. [PubMed: 24482015]
- Oza VS, Mamlouk MD, Hess CP, et al.: Role of Sirolimus in Advanced Kaposiform Hemangioendothelioma. Pediatr Dermatol 33 (2): e88-92, 2016 Mar-Apr. [PubMed: 26864138]
- Adams DM, Trenor CC 3rd, Hammill AM, et al.: Efficacy and Safety of Sirolimus in the Treatment of Complicated Vascular Anomalies. Pediatrics 137 (2): e20153257, 2016. [PMC free article: PMC4732362] [PubMed: 26783326]
- Ji Y, Chen S, Xiang B, et al.: Sirolimus for the treatment of progressive kaposiform hemangioendothelioma: A multicenter retrospective study. Int J Cancer 141 (4): 848-855, 2017. [PubMed: 28486787]
- Schaefer BA, Wang D, Merrow AC, et al.: Long-term outcome for kaposiform hemangioendothelioma: A report of two cases. Pediatr Blood Cancer 64 (2): 284-286, 2017. [PubMed: 27701822]
Intermediate Tumors (Rarely Metastasizing)
Intermediate vascular tumors (rarely metastasizing) include the following:
Pseudomyogenic Hemangioendothelioma
Incidence and outcome
Pseudomyogenic hemangioendothelioma is a rare, newly designated, distinct vascular tumor. It is characterized as an intermediate-grade tumor with moderately aggressive local spread and rare distant metastatic disease.
Pathology and biology
Pseudomyogenic hemangioendothelioma is characterized by loose fascicles of plump spindle and epithelioid cells with abundant eosinophils, cytoplasm, and coexpression of keratins and endothelial markers.[1-3] The etiology for this tumor is unclear, although a balanced translocation t(7;19) resulting in the SERPINE1-FOSB fusion gene was reported.[4]
Clinical presentation and diagnostic evaluation
The tumor usually presents in young men aged 20 to 50 years.[1,2] Multifocal disease occurs in 70% of patients. Sites of involvement include the dermis, subcutis, and bones. Patients usually present with pain or a soft tissue mass.[1,5]
Treatment of pseudomyogenic hemangioendothelioma
Most patients are treated with surgery, including amputation with multifocal bony disease.[1] In reported cases, chemotherapy has had limited response. Recently, the mammalian target of rapamycin (mTOR) inhibitors have been considered as treatment options.[6,7]
Retiform Hemangioendothelioma
Pathology and clinical presentation
Retiform hemangioendotheliomas are slow growing, exophytic, flat tumors found in young adults and occasionally children.[8] They are usually located in the limbs and trunk. Histologically, they are located in the dermis and subcutaneous tissue. Vessels exhibit a pattern resembling the rete testis and are lined by protruding endothelial cells. They do not express lymphatic markers but stain positive for endothelial markers.[9]
Prognostic factors
Local recurrences are common, but distinct metastases are extremely rare.[9]
Papillary Intralymphatic Angioendothelioma
Pathology and clinical presentation
Papillary intralymphatic angioendothelioma, also known as Dabska tumor, can occur in the adult and pediatric population.[14] The lesions occur in the dermis and subcutis on all body parts and there have been some reports of lymph node involvement. They can be large or small raised purplish firm nodules.
Pathologically, they reveal intravascular growth of well-differentiated endothelial cells in a columnar configuration. They have thickened hyaline walls with hobnailed endothelium. Vascular endothelial growth factor receptor type 3, a marker for lymphatic endothelium, is positive in most cases. There is minimal cytologic atypia.[15] Some are associated with vascular malformations.
Treatment of papillary intralymphatic angioendothelioma
Surgical excision is the treatment of choice.[16]
Composite Hemangioendothelioma
Pathology and clinical presentation
Composite hemangioendothelioma is a very rare vascular tumor classified because of the combined benign and malignant vascular components. Usually, combined epithelioid and retiform variants are noted but some tumors have three components (epithelioid, retiform, and spindle cell).[17] Angiosarcoma foci have been noted. Pathology reveals positivity for CD31, factor VIII, and vimentin.[17,18] Rarely, D-240 is positive with a Ki-67 index of approximately 20%.[17]
This tumor usually occurs in the dermis and subcutis of the distal extremities but has been found in other areas such as the head, neck, and mediastinum.[17] They have been reported in all age groups.[17]
Kaposi Sarcoma
Pathology and clinical presentation
Kaposi sarcoma (KS) is a rare malignant vascular tumor associated with a viral etiology (human herpesvirus 8).[21] The skin lesions were first described in 1872 by Moritz Kaposi. The incidence has increased worldwide secondary to the HIV-AIDS epidemic. It is an extremely rare diagnosis in children. Epidemic and iatrogenic forms of Kaposi sarcoma in children result from profound acquired T-cell deficiency that results from HIV infection and rare immune disorders.
A retrospective study has investigated the presentation of Kaposi sarcoma in children in endemic areas of Africa. Children usually present with cutaneous lesions, lymphadenopathy, and intrathoracic and oral lesions. Cutaneous lesions initially appear as red, purple, or brown macules, later developing into plaques and then nodules.[22-24]
Kaposi sarcoma is exceedingly rare in the pediatric population and is usually associated with immunocompromised states such as HIV infection or solid organ transplant.
Treatment of Kaposi sarcoma
Children with Kaposi sarcoma have responded to treatment with chemotherapy regimens, including bleomycin, vincristine, and taxanes, although there are no prospective clinical trials. Other treatment options have been based on adult studies (see below).
Because Kaposi sarcoma is rare in the pediatric population, there are no evidence-based studies. Even in adults, the evidence and quality of studies is inferior and it is difficult to recommend particular treatment regimens. Fifty-six Malawian children aged 3 to 12 years with Kaposi sarcoma were treated with six courses of vincristine, bleomycin, and oral etoposide. This was a high-risk population because 48 of the patients (86%) were HIV positive, of whom 36 (77%) were on antiretroviral therapy. Quality of life improved in 45 patients (80%). Eighteen patients (32%) had a complete remission. At 12 months, the overall survival rate was 71%, and the event-free survival rate was 50%.[25][Level of evidence: 3iiA]
In a systematic review of treatment for classic Kaposi sarcoma, 26 articles published from 1980 to 2010 were reviewed; articles describing populations at high risk secondary to previous transplantation and endemic and epidemic Kaposi sarcoma were excluded.[26] All articles had a minimum of five patients per intervention. A greater than 50% decrease in the size of the lesions or lymphedema was considered a response. The quality of the articles was considered poor, primarily because of lack of uniform staging criteria and variable means of assessing response. The following response rates for systemic treatments were noted:
- Pegylated doxorubicin—71% to 100%.
- Vinca alkaloids—58% to 90%.
- Etoposide—74% to 76%.
- Taxanes—93% to 100%.
- Gemcitabine—100%.
- Vinblastine and bleomycin—97%.
- Interferon alfa-2—71% to 100%.
For local therapies, the following response rates were reported:
- Intralesional vincristine—62%.
- Intralesional interferon alfa-2—50% to 90%.
- Imiquimod—56%.
- Radiation therapy—63% to 93%.
(Refer to the PDQ summary on Kaposi Sarcoma Treatment for information about the treatment of Kaposi sarcoma in adults.)
References
- Hornick JL, Fletcher CD: Pseudomyogenic hemangioendothelioma: a distinctive, often multicentric tumor with indolent behavior. Am J Surg Pathol 35 (2): 190-201, 2011. [PubMed: 21263239]
- Billings SD, Folpe AL, Weiss SW: Epithelioid sarcoma-like hemangioendothelioma. Am J Surg Pathol 27 (1): 48-57, 2003. [PubMed: 12502927]
- Mirra JM, Kessler S, Bhuta S, et al.: The fibroma-like variant of epithelioid sarcoma. A fibrohistiocytic/myoid cell lesion often confused with benign and malignant spindle cell tumors. Cancer 69 (6): 1382-95, 1992. [PubMed: 1371711]
- Walther C, Tayebwa J, Lilljebjörn H, et al.: A novel SERPINE1-FOSB fusion gene results in transcriptional up-regulation of FOSB in pseudomyogenic haemangioendothelioma. J Pathol 232 (5): 534-40, 2014. [PubMed: 24374978]
- Amary MF, O'Donnell P, Berisha F, et al.: Pseudomyogenic (epithelioid sarcoma-like) hemangioendothelioma: characterization of five cases. Skeletal Radiol 42 (7): 947-57, 2013. [PubMed: 23381465]
- Joseph J, Wang WL, Patnana M, et al.: Cytotoxic and targeted therapy for treatment of pseudomyogenic hemangioendothelioma. Clin Sarcoma Res 5: 22, 2015. [PMC free article: PMC4615364] [PubMed: 26500758]
- Ozeki M, Nozawa A, Kanda K, et al.: Everolimus for Treatment of Pseudomyogenic Hemangioendothelioma. J Pediatr Hematol Oncol 39 (6): e328-e331, 2017. [PubMed: 28121744]
- El Darouti M, Marzouk SA, Sobhi RM, et al.: Retiform hemangioendothelioma. Int J Dermatol 39 (5): 365-8, 2000. [PubMed: 10849129]
- Colmenero I, Hoeger PH: Vascular tumours in infants. Part II: vascular tumours of intermediate malignancy [corrected] and malignant tumours. Br J Dermatol 171 (3): 474-84, 2014. [PubMed: 24965196]
- Keiler SA, Honda K, Bordeaux JS: Retiform hemangioendothelioma treated with Mohs micrographic surgery. J Am Acad Dermatol 65 (1): 233-5, 2011. [PubMed: 21679834]
- Hirsh AZ, Yan W, Wei L, et al.: Unresectable retiform hemangioendothelioma treated with external beam radiation therapy and chemotherapy: a case report and review of the literature. Sarcoma 2010: , 2010. [PMC free article: PMC2948930] [PubMed: 20936126]
- Enjolras O, Mulliken JB, Kozakewich HPW: Vascular tumors and tumor-like lesions. In: Mulliken JB, Burrows PE, Fishman SJ, eds.: Mulliken & Young's Vascular Anomalies: Hemangiomas and Malformations. 2nd ed. New York, NY: Oxford University Press, 2013, pp 259-324.
- Tamhankar AS, Vaidya A, Pai P: Retiform hemangioendothelioma over forehead: A rare tumor treated with chemoradiation and a review of literature. J Cancer Res Ther 11 (3): 657, 2015 Jul-Sep. [PubMed: 26458658]
- Dabska M: Malignant endovascular papillary angioendothelioma of the skin in childhood. Clinicopathologic study of 6 cases. Cancer 24 (3): 503-10, 1969. [PubMed: 5343389]
- Fanburr-Smith JC: Papillary intralymphatic angioendothelioma. In: Fletcher CDM, Bridge JA, Hogendoorn P, et al., eds.: WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon, France: IARC Press, 2013, pp 148.
- Neves RI, Stevenson J, Hancey MJ, et al.: Endovascular papillary angioendothelioma (Dabska tumor): underrecognized malignant tumor in childhood. J Pediatr Surg 46 (1): e25-8, 2011. [PubMed: 21238627]
- Shang Leen SL, Fisher C, Thway K: Composite hemangioendothelioma: clinical and histologic features of an enigmatic entity. Adv Anat Pathol 22 (4): 254-9, 2015. [PubMed: 26050262]
- Mahmoudizad R, Samrao A, Bentow JJ, et al.: Composite hemangioendothelioma: An unusual presentation of a rare vascular tumor. Am J Clin Pathol 141 (5): 732-6, 2014. [PubMed: 24713748]
- Tateishi J, Saeki H, Ito K, et al.: Cutaneous composite hemangioendothelioma on the nose treated with electron beam. Int J Dermatol 52 (12): 1618-9, 2013. [PubMed: 22998114]
- Soldado F, Fontecha CG, Haddad S, et al.: Composite vascularized fibular epiphyseo-osteo-periosteal transfer for hip reconstruction after proximal femoral tumoral resection in a 4-year-old child. Microsurgery 32 (6): 489-92, 2012. [PubMed: 22511340]
- Jackson CC, Dickson MA, Sadjadi M, et al.: Kaposi Sarcoma of Childhood: Inborn or Acquired Immunodeficiency to Oncogenic HHV-8. Pediatr Blood Cancer 63 (3): 392-7, 2016. [PMC free article: PMC4984265] [PubMed: 26469702]
- Dow DE, Cunningham CK, Buchanan AM: A Review of Human Herpesvirus 8, the Kaposi's Sarcoma-Associated Herpesvirus, in the Pediatric Population. J Pediatric Infect Dis Soc 3 (1): 66-76, 2014. [PMC free article: PMC3933043] [PubMed: 24567845]
- El-Mallawany NK, Kamiyango W, Slone JS, et al.: Clinical Factors Associated with Long-Term Complete Remission versus Poor Response to Chemotherapy in HIV-Infected Children and Adolescents with Kaposi Sarcoma Receiving Bleomycin and Vincristine: A Retrospective Observational Study. PLoS One 11 (4): e0153335, 2016. [PMC free article: PMC4833299] [PubMed: 27082863]
- Rees CA, Keating EM, Lukolyo H, et al.: Mapping the Epidemiology of Kaposi Sarcoma and Non-Hodgkin Lymphoma Among Children in Sub-Saharan Africa: A Review. Pediatr Blood Cancer 63 (8): 1325-31, 2016. [PMC free article: PMC7340190] [PubMed: 27082516]
- Macken M, Dale H, Moyo D, et al.: Triple therapy of vincristine, bleomycin and etoposide for children with Kaposi sarcoma: Results of a study in Malawian children. Pediatr Blood Cancer 65 (2): , 2018. [PubMed: 28988435]
- Régnier-Rosencher E, Guillot B, Dupin N: Treatments for classic Kaposi sarcoma: a systematic review of the literature. J Am Acad Dermatol 68 (2): 313-31, 2013. [PubMed: 22695100]
Malignant Tumors
Malignant vascular tumors include the following:
Epithelioid Hemangioendothelioma
Incidence and outcome
This tumor was first described in soft tissue by Weiss and Enzinger in 1982. Epithelioid hemangioendotheliomas can occur at younger ages, but the peak incidence is in the fourth and fifth decades of life. The tumors can have an indolent or very aggressive course, with overall survival of 73% at 5 years. There are case reports of patients with untreated multiple lesions who have a very benign course compared with other patients who have a very aggressive course. Some pathologists have tried to stratify patients to evaluate risks and adjust treatment, but more research is needed.[1-7]
The presence of effusions, tumor size larger than 3 cm, and a high mitotic index (>3 mitoses/50 high-power fields) have been associated with unfavorable outcomes.[3]
Pathology and biology
A WWTR1-CAMTA1 gene fusion has been found in a large percentage of patients; less commonly, a YAP1-TFE3 gene fusion has been reported.[1] These fusions are not directly targetable with current medicines. Monoclonality has been described in multiple liver lesions, suggesting a metastatic process.
Histologically, these lesions are characterized as epithelioid lesions arranged in nests, strands, and trabecular patterns, with infrequent vascular spaces. Features that may be associated with aggressive clinical behavior include cellular atypia, one or more mitoses per 10 high-power fields, an increased proportion of spindled cells, focal necrosis, and metaplastic bone formation.[3]
The number of pediatric patients reported in the literature is limited.
Clinical presentation and diagnostic evaluation
Common sites of involvement are liver alone (21%), liver plus lung (18%), lung alone (12%), and bone alone (14%).[3,8,9] Clinical presentation depends on site of involvement, as follows:
- Liver: Hepatic nodules have central vascularity on ultrasound, contrast-enhancing lesions by computed tomography, and low T1 signal and moderate T2 signal on magnetic resonance imaging.
- Lung: Pulmonary epithelioid hemangioendothelioma may be an asymptomatic finding on chest x-ray or be associated with pleuritic pain, hemoptysis, anemia, and fibrosis.
- Bone: Bone metastasis may be associated with pathologic fracture. On x-rays, they are well-defined osteolytic lesions and can be multiple or solitary.
- Soft tissue: Thirty percent of soft tissue cases are associated with metastases, and when present, can have a very aggressive course, with limited response to chemotherapy.
- Skin: Cutaneous lesions can be raised and nodular or can be warm red-brown plaques.
Treatment of epithelioid hemangioendothelioma
Treatment options for epithelioid hemangioendothelioma include the following:
- Observation.
- Surgery.
- Immunotherapy.
- Targeted therapy.
- Chemotherapy.
For indolent cases, observation is warranted. For more aggressive cases, multiple medications have been used, including interferon, thalidomide, sorafenib, pazopanib, and sirolimus.[10] The most aggressive cases are treated with angiosarcoma-type chemotherapy. Surgery is used when possible. Liver transplantation has been used with aggressive liver lesions, both with and without metastases.[3,11-14]
Treatment options under clinical evaluation for epithelioid hemangioendothelioma
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- NCT03148275 (Trametinib in Treating Patients with Epithelioid Hemangioendothelioma That Is Metastatic, Locally Advanced, or Cannot Be Removed by Surgery): This is a phase II trial assessing the efficacy of trametinib, with patient-reported outcomes as secondary aims.
- NCT01532687 (Gemcitabine Hydrochloride With or Without Pazopanib Hydrochloride in Treating Patients With Refractory Soft Tissue Sarcoma): This randomized phase II trial studies how well gemcitabine hydrochloride works with or without pazopanib hydrochloride in treating patients with refractory soft tissue sarcoma.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
Angiosarcoma of the Soft Tissue
Incidence
Angiosarcoma is a rare (accounting for 2% of sarcomas), aggressive, vascular tumor that can arise in any part of the body, but is more common in the soft tissue. Angiosarcoma has an estimated incidence of 2 cases per 1 million; in the United States, it annually affects approximately 600 people who are typically aged 60 to 70 years.[15]
Angiosarcomas are extremely rare in children and it is unclear if the pathophysiology of this tumor is different in the pediatric population. Cases have been reported in neonates and toddlers, with presentation of multiple cutaneous lesions and liver lesions, some of which are GLUT1 positive.[16-19] Most angiosarcomas involve the skin and superficial soft tissue, although the liver, spleen, and lung can be affected; bone is rarely affected.
Risk factors
Established risk factors include vinyl chloride exposure, radiation exposure, and chronic lymphedema from any cause, including Stewart-Treves syndrome.[20]
Pathology and biology
Angiosarcomas are largely aneuploid tumors. The rare cases of angiosarcoma that arise from benign lesions such as hemangiomas have a distinct pathway that needs to be investigated. MYC amplification is seen in radiation-induced angiosarcoma. KDR-VEGFR2 mutations and FLT4-VEGFR3 amplifications have been seen with a frequency of less than 50%.[20]
Histopathologic diagnosis can be very difficult because there can be areas of varied atypia. The common feature is an irregular network of channels in a dissective pattern along dermal collagen bundles. There is varied cellular shape, size, mitosis, endothelial multilayering, and papillary formation. Epithelioid cells can also be present. Necrosis and hemorrhage are common. Tumors stain for factor VIII, CD31, and CD34. Some liver lesions can mimic infantile hemangiomas and have focal GLUT1 positivity. Nomenclature of these liver lesions has been difficult and confusing with use of terminology from 1971 (e.g., type I hemangioendothelioma: infantile hemangioma; type II hemangioendothelioma: low-grade angiosarcoma; type III hemangioendothelioma: high-grade angiosarcoma).[17]
Treatment of angiosarcoma of the soft tissue
Treatment options for angiosarcoma of the soft tissue include the following:
- Surgery (localized disease).
- Radiation therapy (localized cutaneous disease in adults).
- Surgery, chemotherapy, and radiation therapy (metastatic disease).
Localized disease is cured by aggressive surgery. Complete surgical excision appears to be crucial for angiosarcomas and lymphangiosarcomas despite evidence of tumor shrinkage in some patients who were treated with local or systemic therapy.[18,21-23] A review of 222 patients (median age, 62 years; range, age 15–90 years) showed an overall disease-specific survival (DSS) rate of 38% at 5 years. Five-year DSS was 44% in 138 patients with localized, resected tumors but only 16% in 43 patients with metastases at diagnosis.[23] Data on liver transplantation for localized angiosarcoma are limited.[24][Level of evidence: 3iiA]
Localized disease, especially cutaneous angiosarcoma, can be treated with radiation therapy. Most of these reported cases are in adults.[25]
Multimodal treatment with surgery, systemic chemotherapy, and radiation therapy is used for metastatic disease, although it is rarely curative.[26] Disease control is the objective in metastatic angiosarcoma, with published progression-free survival rates between 3 months and 7 months [27] and a median overall survival (OS) rate of 14 months to 18 months.[28] In both adults and children, 5-year OS rates between 20% and 35% are reported.[18,19,29]
In a child diagnosed with angiosarcoma secondary to malignant transformation from infantile hemangioma, response to treatment with bevacizumab, a monoclonal antibody against vascular endothelial growth factor, combined with systemic chemotherapy, has been reported.[16,26] A report of eight cases of liver angiosarcoma in children highlighted the misuse of the term hemangioendothelioma and the importance of early diagnosis and treatment of these tumors.[30]
Biologic agents that inhibit angiogenesis have shown activity in adults with angiosarcoma.[17,29]
Treatment options under clinical evaluation for angiosarcoma of the soft tissue
Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- ARST1321 (NCT02180867) (Radiation Therapy With or Without Combination Chemotherapy or Pazopanib Hydrochloride Before Surgery in Treating Patients With Newly Diagnosed Nonrhabdomyosarcoma Soft Tissue Sarcomas That Can be Removed by Surgery [PAZNTIS]): This study will first determine the feasibility of adding a tyrosine kinase inhibitor in combination with radiation therapy or chemotherapy (ifosfamide/etoposide) and radiation therapy in pediatric and adult patients newly diagnosed with unresected intermediate-risk and high-risk nonrhabdomyosarcomatous soft tissue sarcoma. Subsequently, this trial will compare the rates of near-complete pathologic response (>90% necrosis) of: 1) preoperative pazopanib plus chemoradiation therapy versus preoperative chemoradiation therapy alone for potentially resectable (>5 cm), grade 3 intermediate-risk to high-risk chemotherapy-sensitive adult and pediatric nonrhabdomyosarcomatous soft tissue sarcoma; and 2) pazopanib plus preoperative radiation therapy versus preoperative radiation therapy alone for potentially resectable intermediate-risk to high-risk adult and pediatric nonrhabdomyosarcomatous soft tissue sarcoma. Patients with angiosarcoma of the soft tissue are eligible for this trial.
- NCT01532687 (Gemcitabine Hydrochloride With or Without Pazopanib Hydrochloride in Treating Patients With Refractory Soft Tissue Sarcoma): This randomized phase II trial studies how well gemcitabine hydrochloride works with or without pazopanib hydrochloride in treating patients with refractory soft tissue sarcoma.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Mehrabi A, Kashfi A, Fonouni H, et al.: Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 107 (9): 2108-21, 2006. [PubMed: 17019735]
- Haro A, Saitoh G, Tamiya S, et al.: Four-year natural clinical course of pulmonary epithelioid hemangioendothelioma without therapy. Thorac Cancer 6 (4): 544-7, 2015. [PMC free article: PMC4511336] [PubMed: 26273413]
- Sardaro A, Bardoscia L, Petruzzelli MF, et al.: Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev 8 (2): 259, 2014. [PMC free article: PMC4419652] [PubMed: 25992243]
- Dong K, Wang XX, Feng JL, et al.: Pathological characteristics of liver biopsies in eight patients with hepatic epithelioid hemangioendothelioma. Int J Clin Exp Pathol 8 (9): 11015-23, 2015. [PMC free article: PMC4637634] [PubMed: 26617819]
- Adams DM, Hammill A: Other vascular tumors. Semin Pediatr Surg 23 (4): 173-7, 2014. [PubMed: 25241094]
- Xiao Y, Wang C, Song Y, et al.: Primary epithelioid hemangioendothelioma of the kidney: the first case report in a child and literature review. Urology 82 (4): 925-7, 2013. [PubMed: 23726166]
- Reich S, Ringe H, Uhlenberg B, et al.: Epithelioid hemangioendothelioma of the lung presenting with pneumonia and heart rhythm disturbances in a teenage girl. J Pediatr Hematol Oncol 32 (4): 274-6, 2010. [PubMed: 20445417]
- Daller JA, Bueno J, Gutierrez J, et al.: Hepatic hemangioendothelioma: clinical experience and management strategy. J Pediatr Surg 34 (1): 98-105; discussion 105-6, 1999. [PubMed: 10022152]
- Ackermann O, Fabre M, Franchi S, et al.: Widening spectrum of liver angiosarcoma in children. J Pediatr Gastroenterol Nutr 53 (6): 615-9, 2011. [PubMed: 21832953]
- Stacchiotti S, Provenzano S, Dagrada G, et al.: Sirolimus in Advanced Epithelioid Hemangioendothelioma: A Retrospective Case-Series Analysis from the Italian Rare Cancer Network Database. Ann Surg Oncol 23 (9): 2735-44, 2016. [PubMed: 27334221]
- Semenisty V, Naroditsky I, Keidar Z, et al.: Pazopanib for metastatic pulmonary epithelioid hemangioendothelioma-a suitable treatment option: case report and review of anti-angiogenic treatment options. BMC Cancer 15: 402, 2015. [PMC free article: PMC4437555] [PubMed: 25967676]
- Raheja A, Suri A, Singh S, et al.: Multimodality management of a giant skull base hemangioendothelioma of the sphenopetroclival region. J Clin Neurosci 22 (9): 1495-8, 2015. [PubMed: 25986183]
- Ahmad N, Adams DM, Wang J, et al.: Hepatic epithelioid hemangioendothelioma in a patient with hemochromatosis. J Natl Compr Canc Netw 12 (9): 1203-7, 2014. [PubMed: 25190690]
- Otte JB, Zimmerman A: The role of liver transplantation for pediatric epithelioid hemangioendothelioma. Pediatr Transplant 14 (3): 295-7, 2010. [PubMed: 20331517]
- Cioffi A, Reichert S, Antonescu CR, et al.: Angiosarcomas and other sarcomas of endothelial origin. Hematol Oncol Clin North Am 27 (5): 975-88, 2013. [PubMed: 24093171]
- Jeng MR, Fuh B, Blatt J, et al.: Malignant transformation of infantile hemangioma to angiosarcoma: response to chemotherapy with bevacizumab. Pediatr Blood Cancer 61 (11): 2115-7, 2014. [PubMed: 24740626]
- Dehner LP, Ishak KG: Vascular tumors of the liver in infants and children. A study of 30 cases and review of the literature. Arch Pathol 92 (2): 101-11, 1971. [PubMed: 5559952]
- Ferrari A, Casanova M, Bisogno G, et al.: Malignant vascular tumors in children and adolescents: a report from the Italian and German Soft Tissue Sarcoma Cooperative Group. Med Pediatr Oncol 39 (2): 109-14, 2002. [PubMed: 12116058]
- Deyrup AT, Miettinen M, North PE, et al.: Pediatric cutaneous angiosarcomas: a clinicopathologic study of 10 cases. Am J Surg Pathol 35 (1): 70-5, 2011. [PubMed: 21164289]
- Elliott P, Kleinschmidt I: Angiosarcoma of the liver in Great Britain in proximity to vinyl chloride sites. Occup Environ Med 54 (1): 14-8, 1997. [PMC free article: PMC1128629] [PubMed: 9072028]
- Lezama-del Valle P, Gerald WL, Tsai J, et al.: Malignant vascular tumors in young patients. Cancer 83 (8): 1634-9, 1998. [PubMed: 9781959]
- Fata F, O'Reilly E, Ilson D, et al.: Paclitaxel in the treatment of patients with angiosarcoma of the scalp or face. Cancer 86 (10): 2034-7, 1999. [PubMed: 10570428]
- Lahat G, Dhuka AR, Hallevi H, et al.: Angiosarcoma: clinical and molecular insights. Ann Surg 251 (6): 1098-106, 2010. [PubMed: 20485141]
- Orlando G, Adam R, Mirza D, et al.: Hepatic hemangiosarcoma: an absolute contraindication to liver transplantation--the European Liver Transplant Registry experience. Transplantation 95 (6): 872-7, 2013. [PubMed: 23354302]
- Sanada T, Nakayama H, Irisawa R, et al.: Clinical outcome and dose volume evaluation in patients who undergo brachytherapy for angiosarcoma of the scalp and face. Mol Clin Oncol 6 (3): 334-340, 2017. [PMC free article: PMC5403362] [PubMed: 28451409]
- Dickson MA, D'Adamo DR, Keohan ML, et al.: Phase II Trial of Gemcitabine and Docetaxel with Bevacizumab in Soft Tissue Sarcoma. Sarcoma 2015: 532478, 2015. [PMC free article: PMC4446476] [PubMed: 26074722]
- North PE, Waner M, Mizeracki A, et al.: A unique microvascular phenotype shared by juvenile hemangiomas and human placenta. Arch Dermatol 137 (5): 559-70, 2001. [PubMed: 11346333]
- Boye E, Yu Y, Paranya G, et al.: Clonality and altered behavior of endothelial cells from hemangiomas. J Clin Invest 107 (6): 745-52, 2001. [PMC free article: PMC208946] [PubMed: 11254674]
- Ravi V, Patel S: Vascular sarcomas. Curr Oncol Rep 15 (4): 347-55, 2013. [PubMed: 23852636]
- Grassia KL, Peterman CM, Iacobas I, et al.: Clinical case series of pediatric hepatic angiosarcoma. Pediatr Blood Cancer 64 (11): , 2017. [PubMed: 28521077]
Special Considerations for the Treatment of Children With Cancer
Cancer in children and adolescents is rare, although the overall incidence of childhood cancer has been slowly increasing since 1975.[1] Children and adolescents with cancer should be referred to medical centers that have a multidisciplinary team of cancer specialists with experience treating the cancers that occur during childhood and adolescence. This multidisciplinary team approach incorporates the skills of the primary care physician, a surgeon experienced in vascular tumors, a pathologist, radiation oncologists, pediatric oncologists, rehabilitation specialists, pediatric nurse specialists, social workers, and others to ensure that children receive treatment, supportive care, and rehabilitation that will achieve optimal survival and quality of life. (Refer to the PDQ summaries on Supportive and Palliative Care for specific information about supportive care for children and adolescents with cancer.)
Guidelines for pediatric cancer centers and their role in the treatment of pediatric patients with cancer have been outlined by the American Academy of Pediatrics.[2] At these pediatric cancer centers, clinical trials are available for most types of cancer that occur in children and adolescents, and the opportunity to participate in these trials is offered to most patients and families. Clinical trials for children and adolescents with cancer are generally designed to compare potentially better therapy with therapy that is currently accepted as standard. Most of the progress made in identifying curative therapies for childhood cancers has been achieved through clinical trials. Information about ongoing clinical trials is available from the NCI website.
Dramatic improvements in survival have been achieved for children and adolescents with cancer. Between 1975 and 2010, childhood cancer mortality decreased by more than 50%.[1] Childhood and adolescent cancer survivors require close monitoring because cancer therapy side effects may persist or develop months or years after treatment. (Refer to the PDQ summary on Late Effects of Treatment for Childhood Cancer for specific information about the incidence, type, and monitoring of late effects in childhood and adolescent cancer survivors.)
References
- Smith MA, Altekruse SF, Adamson PC, et al.: Declining childhood and adolescent cancer mortality. Cancer 120 (16): 2497-506, 2014. [PMC free article: PMC4136455] [PubMed: 24853691]
- Corrigan JJ, Feig SA; American Academy of Pediatrics: Guidelines for pediatric cancer centers. Pediatrics 113 (6): 1833-5, 2004. [PubMed: 15173520]
Changes to This Summary (01/26/2018)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Added Infantile hemangioma with minimal or arrested growth as a new subsection.
This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® - NCI's Comprehensive Cancer Database pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood vascular tumors. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Childhood Vascular Tumors Treatment are:
- Denise Adams, MD (Children's Hospital Boston)
- Louis S. Constine, MD (James P. Wilmot Cancer Center at University of Rochester Medical Center)
- Holcombe Edwin Grier, MD
- Paul A. Meyers, MD (Memorial Sloan-Kettering Cancer Center)
- Thomas A. Olson, MD (Aflac Cancer and Blood Disorders Center of Children's Healthcare of Atlanta - Egleston Campus)
- Alberto S. Pappo, MD (St. Jude Children's Research Hospital)
- R Beverly Raney, MD (Consultant)
- Stephen J. Shochat, MD (St. Jude Children's Research Hospital)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Vascular Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/soft-tissue-sarcoma/hp/child-vascular-tumors-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26844334]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
Based on the strength of the available evidence, treatment options may be described as either “standard” or “under clinical evaluation.” These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.
- Review Childhood Vascular Tumors Treatment (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Childhood Vascular Tumors Treatment (PDQ®): Patient Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Liver Cancer Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Liver Cancer Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Soft Tissue Sarcoma Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Soft Tissue Sarcoma Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Extracranial Germ Cell Tumors Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Extracranial Germ Cell Tumors Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Craniopharyngioma Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Craniopharyngioma Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Childhood Vascular Tumors Treatment (PDQ®) - PDQ Cancer Information SummariesChildhood Vascular Tumors Treatment (PDQ®) - PDQ Cancer Information Summaries
- PREDICTED: Homo sapiens beta-1,4-galactosyltransferase 6 (B4GALT6), transcript v...PREDICTED: Homo sapiens beta-1,4-galactosyltransferase 6 (B4GALT6), transcript variant X3, mRNAgi|2462561991|ref|XM_054319369.1|Nucleotide
- PREDICTED: Homo sapiens family with sequence similarity 168 member B (FAM168B), ...PREDICTED: Homo sapiens family with sequence similarity 168 member B (FAM168B), transcript variant X5, mRNAgi|2462570053|ref|XM_054340508.1|Nucleotide
- triple QxxK/R motif-containing protein [Homo sapiens]triple QxxK/R motif-containing protein [Homo sapiens]gi|300388180|ref|NP_001177965.1|Protein
- LOC134486706 uncharacterized LOC134486706 [Rattus norvegicus]LOC134486706 uncharacterized LOC134486706 [Rattus norvegicus]Gene ID:134486706Gene
Your browsing activity is empty.
Activity recording is turned off.
See more...
