NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Alliance (UK). Faltering Growth – recognition and management. London: National Institute for Health and Care Excellence (NICE); 2017 Sep. (NICE Guideline, No. 75.)
A.1. Guideline title
Faltering growth in children: recognition and management
A.2. Topic
The Department of Health in England has asked NICE to develop a clinical guideline on the identification and management of failure to thrive, also known as faltering growth. Following discussion with stakeholders, the title has been changed to refer to ‘faltering growth’.
For more information about why this guideline is being developed, and how the guideline will fit into current practice, see the context section.
A.3. Who the guideline is for
- Parents and carers of children with faltering growth, and the public
- Healthcare professionals
- Providers of children’s services
- Commissioners of children’s services.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in Welsh Government, Scottish Government, and Northern Ireland Executive.
A.4. Equality considerations
NICE has carried out an equality impact assessment during scoping. The assessment:
- lists equality issues identified, and how they have been addressed
- explains why any groups are excluded from the scope.
A.5. What the guideline is about
A.5.1. Who is the focus?
A.5.1.1. Groups that will be covered
- Infants and preschool children in whom growth concerns have been raised, through either routine monitoring (defined in recommendation 17 of the NICE guideline on maternal and child nutrition) or professional or parental concern.
- The following subgroups have been identified as needing specific consideration:
- infants and preschool children who
- were born prematurely
- were born with intrauterine growth restriction (IUGR)
- with a specific disorder known to cause faltering growth, but only with regard to recognition of growth thresholds for concern
A.5.2. Settings
A.5.2.1. Settings that will be covered
- All settings in which support and services to infants and preschool children are provided.
A.5.3. Activities, services or aspects of care
A.5.3.1. Key areas that will be covered
- Recognition of faltering growth, including defining growth thresholds for concern (including, early weight loss after birth).
- Identification of risk factors for faltering growth.
- Assessment of infants and preschool children with faltering growth. This includes identifying possible causes of faltering growth and, in the absence of any other symptoms or signs, deciding on appropriate investigations.
- Growth monitoring in infants and preschool children with suspected or confirmed faltering growth.
- Referral to secondary care.
- Interventions to manage faltering growth, including:
- breastfeeding support
- support for other types of feeding
- dietary advice and supplementation
- family support.
- Design of services for the management of faltering growth.
- Information and support for parents and carers of infants and preschool children with suspected or confirmed faltering growth.
A.5.3.2. Areas that will not be covered
Specialist management of specific disorders causing faltering growth, for example coeliac disease.
A.5.4. Economic aspects
We will take economic aspects into account when making recommendations. We will develop an economic plan that states for each review question (or key area in the scope) whether economic considerations are relevant, and if so whether this is an area that should be prioritised for economic modelling and analysis. We will review the economic evidence and carry out economic analyses using an NHS and personal social services (PSS) perspective.
A.5.5. Key issues and questions
While writing this scope, we have identified the following key issues, and key questions related to them:
- Recognising faltering growth, including defining thresholds for concern
- What are the growth thresholds for enhanced monitoring or intervention for suspected or confirmed faltering growth in infants and preschool children?
- Identifying the risk factors for faltering growth
- What are the risk factors for faltering growth that could inform recognition and management?
- Assessing infants and preschool children with faltering growth
- What is the prevalence of specific conditions in infants and preschool children who present with faltering growth and no other symptoms or signs, to help determine appropriate investigations?
- Growth monitoring in infants and preschool children with suspected or confirmed faltering growth
- What growth monitoring should be carried out in infants and preschool children with suspected or confirmed faltering growth?
- Referring to secondary care
- What factors determine the need for referral to secondary care for infants and preschool children with suspected or confirmed faltering growth?
- Providing interventions to manage faltering growth
- What interventions related to breastfeeding are effective in the management of faltering growth?
- What interventions related to feeding practices other than breastfeeding are effective in the management of faltering growth?
- What interventions related to dietary advice or supplementation are effective in the management of faltering growth?
- What family support interventions are effective in the management of faltering growth?
- Designing services for the management of faltering growth
- What service configurations are effective for the management of faltering growth in infants and preschool children?
- Providing information and support to parents and carers
- What information and support should be provided for parents and carers of infants and preschool children with suspected or confirmed faltering growth?
The key questions may be used to develop more detailed review questions, which guide the systematic review of the literature.
A.5.6. Main outcomes
The main outcomes that will be considered when searching for and assessing the evidence are:
- measurements of nutritional status (weight, length or height, head circumference, mid-arm circumference)
- continued breastfeeding
- increased nutritional intake
- health-related quality of life
- parent or carer satisfaction
- adherence to interventions
- adverse effects of interventions
- use of health services.
A.6. Links with other NICE guidance and NICE Pathways
A.6.1. NICE guidance
A.6.1.1. NICE guidance in development that is closely related to this guideline
NICE is currently developing the following guidance that is closely related to this guideline:
- Developmental follow-up of preterm babies NICE guideline. Publication expected August 2017
- Child abuse and neglect NICE guideline. Publication expected September 2017.
A.6.2. NICE Pathways
When this guideline is published, the recommendations will be added to NICE Pathways. NICE Pathways bring together all related NICE guidance and associated products on a topic in an interactive topic-based flow chart.
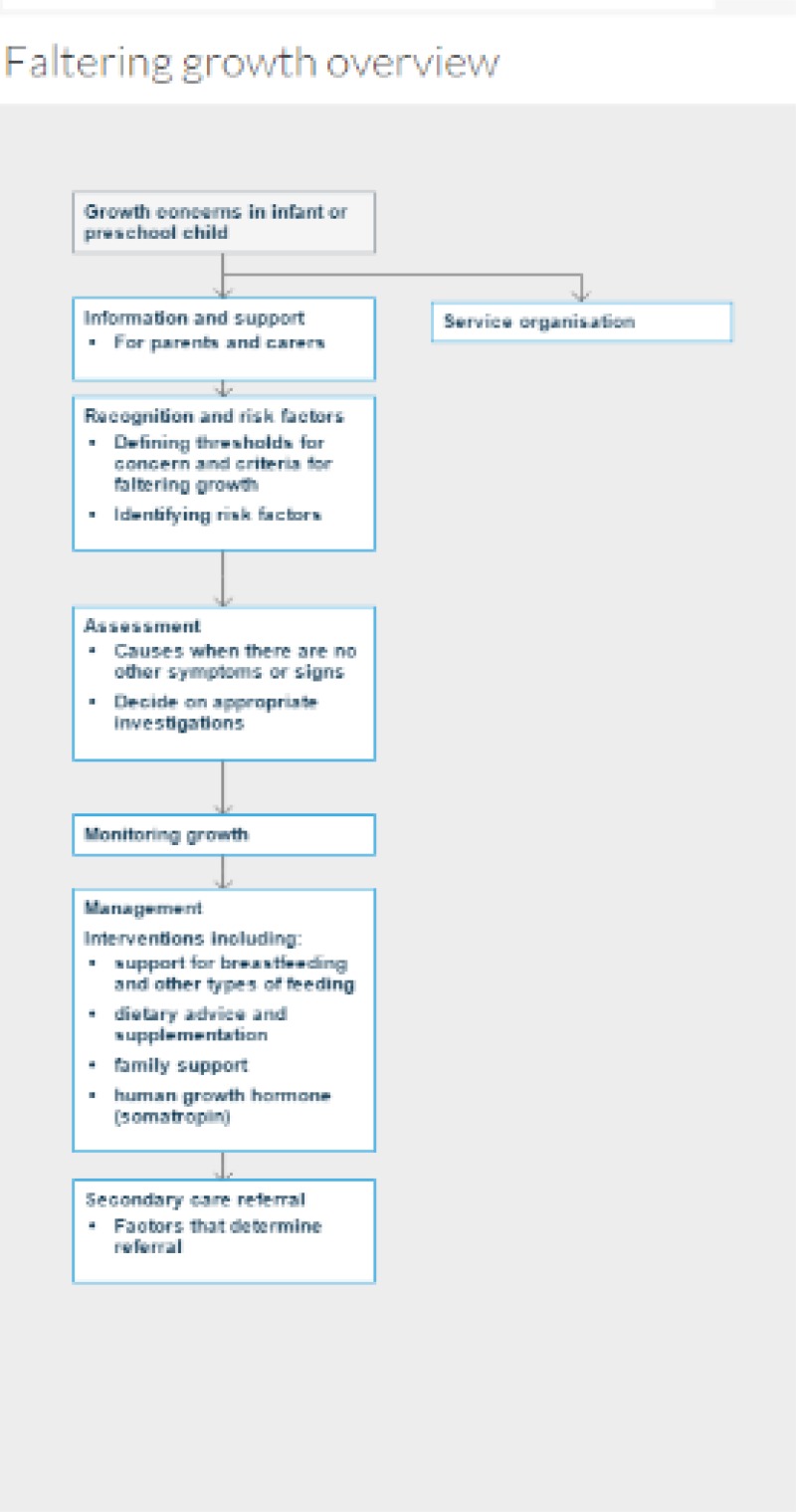
A draft pathway outline on faltering growth, based on this draft scope, is included below. It will be adapted and more detail added as the recommendations are written during guideline development.
Other NICE guidance that may be included in this pathway is the NICE technology appraisal guidance on human growth hormone (somatropin) for the treatment of growth failure in children.
A.7. Context
A.7.1. Key facts and figures
The term ‘faltering growth’ is widely used in relation to infants and young children whose weight gain occurs more slowly than expected for their age and sex. In the past this was often described as a ‘failure to thrive’ but this is no longer the preferred term, partly because ‘failure’ could be perceived as pejorative, but also because lesser degrees of faltering growth may not necessarily indicate a significant problem but merely represent variation from the usual pattern. Estimates of the prevalence of faltering growth in the UK vary widely, depending on the definition used.
The World Health Organization (WHO) has produced growth standards, based on longitudinal studies of healthy breastfed infants. These standards, along with UK full-term and preterm infant growth data, have been incorporated into UK-WHO growth charts for monitoring children’s growth in the UK. A child’s weight, length or height, and head circumference can be plotted to provide a visual representation of their growth over time. Epidemiological studies have shown that healthy children usually progress relatively consistently along a growth centile.
Faltering growth can occur when a child’s nutritional intake does not meet their specific energy requirements. Undernutrition may underlie relatively slow weight gain and movement downwards across weight centiles on a growth chart. Faltering growth in early childhood may be associated with persisting problems with appetite and feeding.
Certain health conditions predispose children to faltering growth (for example, cystic fibrosis or coeliac disease). Specific treatment for such conditions (for example, pancreatic enzyme supplementation for cystic fibrosis and a gluten free diet for coeliac disease) can improve or restore normal weight gain. Simple interventions (such as extra calories and protein) may also be effective in supporting nutrition and weight gain.
The causes of faltering growth in the absence of an underlying condition may be complex and have a variety of causes. In the past, child neglect or socioeconomic and educational disadvantage were often considered to be likely contributors. While neglected children may be undernourished, neglect is now thought to be an uncommon explanation for faltering growth. Similarly, socioeconomic and educational factors have not emerged as important associations in more recent research.
A.7.2. Current practice
Infants and preschool children with faltering growth are often identified by routine growth monitoring. Others may be identified through concern expressed by parents or healthcare professionals. Initial management is often community based and involves providing support and advice to increase calorie intake and manage challenging feeding behaviour. Some children are referred to paediatric dietitians or paediatricians for further assessment and support.
There is variation in practice across the UK in how infants, preschool children and families are supported, referred and investigated where concerns are raised about faltering growth. There is cultural and socioeconomic variation in the rates of initiation and maintenance of breastfeeding, approaches to weaning and choices of weaning foods. Expectations and behaviour at mealtimes, for example whether families eat together, may also be relevant to the risk of infants developing challenging feeding behaviour. These may also influence how readily parents accept feeding support and advice.
A.7.3. Policy, legislation, regulation and commissioning
A.7.3.1. Policy
The National service framework for children, young people and maternity services aims for long-term and sustained improvement in children’s health, and sets standards for health and social care services for children, young people and pregnant women.
The UK National Screening Committee advises on evidence-based whole population screening for conditions which may cause faltering growth, including congenital heart disease and cystic fibrosis.
The Healthy Child Programme describes standards of care for screening and providing advice during pregnancy and the first 5 years of life. It includes broad recommendations on monitoring growth in infants and children.
The NICE guideline will give more specific guidance on when and how to monitor children when growth concerns arise and when referral is appropriate.
A.7.3.2. Legislation, regulation and guidance
The NICE guideline on maternal and child nutrition makes the following recommendation for growth monitoring in infants and children: ‘as a minimum, ensure babies are weighed at birth and in the first week, as part of an overall assessment of feeding. Thereafter, healthy babies should usually be weighed at 8, 12 and 16 weeks and at 1 year, at the time of routine immunisations. If there is concern, weigh more often, but no more than once a month up to 6 months of age, once every 2 months from 6–12 months of age and once every 3 months over the age of 1 year.’ In addition, the NICE quality standard on postnatal care includes the quality statement ‘babies have a complete 6–8 week physical examination’ which includes measuring and plotting weight. However, in practice additional measurements are frequently taken at a variety of intervals and there is uncertainty as to the clinical value of such additional measurements.
A.8. Further information
This is the final scope, incorporating comments from registered stakeholders during consultation.
The guideline is expected to be published in October 2017.
You can follow progress of the guideline.
Our website has information about how NICE guidelines are developed.
- Scope - Faltering Growth – recognition and managementScope - Faltering Growth – recognition and management
- Mystus cavasius isolate CIFRI.NAIH.MC-9 cytochrome b gene, partial cds; mitochon...Mystus cavasius isolate CIFRI.NAIH.MC-9 cytochrome b gene, partial cds; mitochondrialgi|2574880732|gb|OR046981.1|Nucleotide
- MAG: Veillonella sp. LMAG:2 MEG_2_5, whole genome shotgun sequenceMAG: Veillonella sp. LMAG:2 MEG_2_5, whole genome shotgun sequencegi|2540146149|ref|NZ_NAJT01000005.1 |WGS:NZ_NAJT01|MEG_2_5Nucleotide
- PREDICTED: Danio rerio gap junction protein, alpha 3 (gja3), transcript variant ...PREDICTED: Danio rerio gap junction protein, alpha 3 (gja3), transcript variant X2, mRNAgi|2800598063|ref|XM_021478628.2|Nucleotide
Your browsing activity is empty.
Activity recording is turned off.
See more...