NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
1. Diagnostic accuracy of ultrasound features for tubal ectopic pregnancy
Review question
What ultrasound features are most diagnostic of a tubal ectopic pregnancy?
Introduction
Ectopic pregnancy remains the leading cause of maternal mortality in early pregnancy in the UK and early diagnosis is important to reduce this risk. Early diagnosis may also allow non-surgical treatment options, including expectant or medical management. The diagnosis of ectopic pregnancy is made using a combination of the clinical presentation, serum human chorionic gonadotrophin (hCG) levels and pelvic ultrasound scan findings.
Ultrasound features of ectopic pregnancy can vary widely between different individuals, and depend on a variety of factors, including the gestation of the pregnancy, experience of the sonographer, route of scanning (transabdominal or transvaginal) as well as features of the scan equipment. The aim of this review was to identify ultrasound scan features which have high diagnostic accuracy for the identification of ectopic pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Index test, Reference test, and Outcome (PIRO) characteristics of this review.
For full details see the review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014. Please see the methods section of the 2012 guideline for further details.
Methods specific to this review question are described in the review protocol in appendix A.
The use of GRADE for reviews of diagnostic test accuracy has recently been adopted by NICE, and this methodology was applied to the review. Cross-sectional diagnostic test accuracy studies were initially rated as high quality, and the rating was amended according to the risk of bias (as assessed using the QUADAS-2 checklist) inconsistency, imprecision, indirectness and other factors, in a manner analogous to intervention reviews. Imprecision was assessed according to pre-specified thresholds for sensitivity and specificity, which were identified by the guideline committee as representing clinically meaningful results. In determining these thresholds, the committee recognised that the identification of ectopic pregnancy often requires an assessment of a combination of features (including the woman’s symptoms and hCG levels as well as ultrasound findings). Therefore they agreed a threshold of ≥75% for sensitivity and ≥80% for specificity would represent a very useful test. The lower threshold (representing a not useful test) was set at <50%.
Declarations of interest were recorded according to NICE’s 2018 conflicts of interest policy (see Register of Interests).
Clinical evidence
Included studies
Ten cohort studies were included in this review (4 prospective cohorts: Dart 2002, Malek-Mellouli 2013, Moore 2007, Sadek 1995; 6 retrospective cohorts: Ahmed 2004, Barnhart 2011, Dart 1998, Hammoud 2005, Mehta 1999, Nadim 2018).
All studies examined features seen using transvaginal ultrasonography (TVUS), and two studies additionally used transabdominal ultrasonography (TAS) (Hammoud 2005, Moore 2007).
Studies were conducted in three distinct populations of women and so the results have been analysed for these separate sub-populations:
- three studies included any women with bleeding and/or pain during the first trimester, who were referred for ultrasound (sub-population 1, all symptomatic women: Barnhart 2011, Moore 2007, Sadek 1995).
- two studies included only women with a suspected ectopic pregnancy or pregnancy of unknown location (PUL), where women with confirmed intrauterine pregnancies (IUP) were excluded from the analysis (sub-population 2, IUPs excluded: Hammoud 2005, Mehta 1999).
- five studies included women with PULs, where women with definite ectopic pregnancies and IUPs were excluded (sub-population 3, IUP and EP excluded, Ahmed 2004, Dart 1998, Dart 2002, Malek-Mellouli 2013, Nadim 2018).
Terminology used to define findings seen on the ultrasound varied across studies, and did not align precisely with terms used in the protocol. Consequently, the description given within each study was used to group like with like, and the wording in this review has been modified to reflect this:
- An adnexal mass with a gestational sac and yolk sac or fetal pole with/without fetal heartbeat is termed “adnexal ectopic”
- Sonographic findings reported as inhomogeneous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole visible) are termed “complex adnexal mass”
Meta-analysis of diagnostic accuracy measures for the different features identified on the ultrasound was not possible due to the small number of comparable studies (different populations, and/or different features visualised).
Studies are summarised in Table 2.
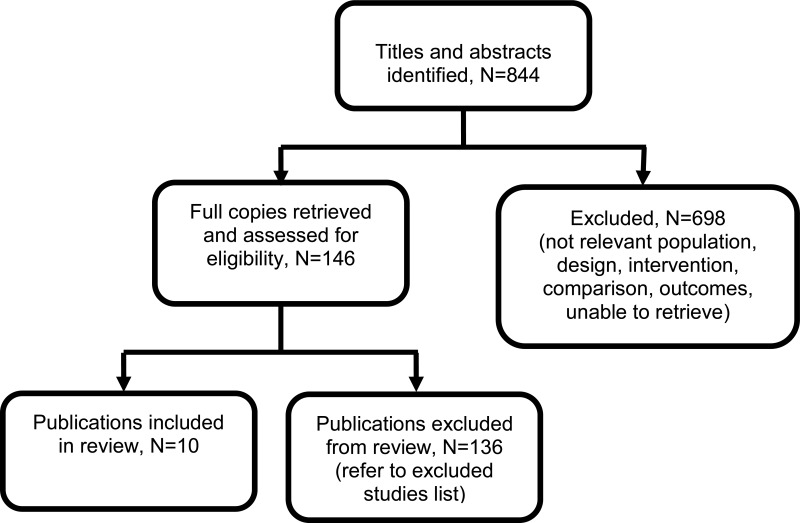
See also the literature search strategy in appendix B and study selection flowchart in appendix C.
Excluded studies
Studies not included in this systematic review with reasons for their exclusions are provided in appendix K.
Summary of clinical studies included in the evidence review
Table 2 provides a brief summary of the included studies.
See appendix D for full evidence tables.
Quality assessment of clinical outcomes included in the evidence review
See appendix F for full GRADE tables.
Economic evidence
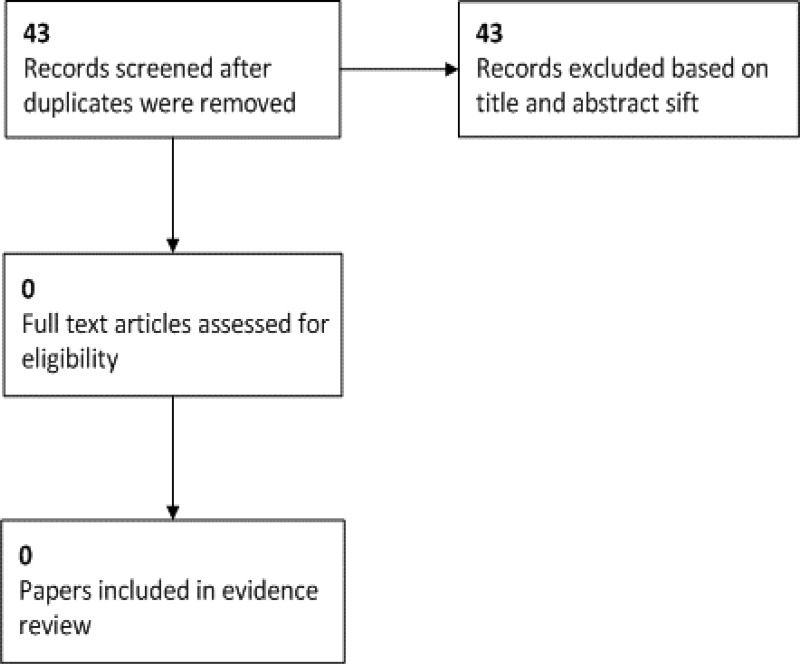
A systematic review of economic literature was conducted, but no studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review.
Evidence statements
Sub-population 1. All symptomatic women (women with pain/bleeding or referred for a scan due to high risk of ectopic pregnancy)
TVUS: adnexal ectopic (adnexal mass with gestational sac and yolk sac or fetal pole +/− fetal heartbeat)
- Low quality evidence from 1 cohort study (N=1880) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using the visualisation of an adnexal ectopic pregnancy with transvaginal ultrasound. The positive likelihood ratio showed this was a very useful feature: when an adnexal ectopic is visualised there is more likely to be a tubal ectopic pregnancy. The negative likelihood ratio showed it was not a useful feature: failure to identify an adnexal ectopic does not markedly reduce the chance of having an ectopic pregnancy.
TVUS: complex adnexal mass: inhomogeneous, heterogeneous, or adnexal mass (no yolk sac or fetal pole)
- Low quality evidence from 1 cohort study (N=1880) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using the visualisation of a complex adnexal mass with transvaginal ultrasound. The positive likelihood ratio showed this to be a very useful feature: when visualised, it has increased likelihood of being an ectopic pregnancy. The negative likelihood ratio showed it was not a useful feature.
TVUS: Free fluid in the pelvis
- Moderate quality evidence from 1 cohort study (N=226) showed moderate sensitivity and specificity to detect tubal ectopic pregnancy using visualisation of free fluid in the pelvis with transvaginal ultrasound. The positive and negative likelihood ratios showed this was not a useful feature.
- High quality evidence from 1 cohort study (N=525) showed high sensitivity and specificity to detect tubal ectopic pregnancy using visualisation of free fluid in the pelvis with transvaginal ultrasound. The positive and negative likelihood ratios showed this to be a very useful feature.
TAS: Free fluid in the pelvis
- Moderate quality evidence from 1 cohort study (N=241) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of free fluid in the pelvis with transabdominal ultrasound. The positive likelihood ratio showed this to be a moderately useful feature, but the negative likelihood ratio showed it was not a useful feature.
Sub-population 2. High risk of ectopic pregnancy: includes pregnancy of unknown location and ectopic pregnancy (all intrauterine pregnancies excluded)
TVUS: Pseudo-sac
- Moderate quality evidence from 1 cohort study (N=403) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of a pseudo-sac with transvaginal ultrasound. The positive and negative likelihood ratios showed this was not a useful feature.
TVUS: Intrauterine fluid
- Low quality evidence from 1 cohort study (N=128) showed low sensitivity and moderate specificity to detect tubal ectopic pregnancy using visualisation of intrauterine fluid with transvaginal ultrasound. The positive and negative likelihood ratios showed this was not a useful feature.
TVUS: Complex adnexal mass: inhomogeneous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole)
- Low quality evidence from 1 cohort study (N=128) showed moderate sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of a complex adnexal mass with transvaginal ultrasound. The positive likelihood ratio showed this was a very useful feature. The negative likelihood ratio showed it was not a useful feature.
TVUS: Free fluid in the peritoneal cavity
- Low quality evidence from 1 cohort study (N=128) showed moderate sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of free fluid in the peritoneal cavity with transvaginal ultrasound. The positive likelihood ratio was not calculable (due to a specificity of 100%). The negative likelihood ratio showed that it was not a useful feature.
Sub-population 3. High risk of ectopic pregnancy: pregnancy of unknown location only (all intrauterine pregnancies and definite ectopic pregnancies excluded)
TVUS: Empty uterus
- Low quality evidence from 2 cohort studies (N=228 and N=635) showed high sensitivity and moderate specificity to detect tubal ectopic pregnancy using visualisation of an empty uterus with transvaginal ultrasound. The positive and negative likelihood ratios showed this was a not useful feature.
TVUS: Pseudo-sac
- Low quality evidence from 1 cohort study (N=77) showed low sensitivity and specificity to detect tubal ectopic pregnancy using visualisation of a pseudo-sac with transvaginal ultrasound. The positive and negative likelihood ratios showed this was a not useful feature.
TVUS: Intrauterine fluid
- Low and moderate quality evidence from 2 cohort studies (N=228 and N=635) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of intrauterine fluid with transvaginal ultrasound. The positive and negative likelihood ratios showed this was not a useful feature.
TVUS: Tubal ring sign (bagel sign)
- Low quality evidence from 1 cohort study (N=612) showed high sensitivity and specificity to detect tubal ectopic pregnancy using visualisation of the tubal ring sign with transvaginal ultrasound. The positive likelihood ratio showed this was a very useful feature. The negative likelihood ratio showed this was a moderately useful feature.
TVUS: Complex adnexal mass: inhomogeneous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole)
- Very low quality evidence from 1 cohort study (N=77) showed moderate sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of a complex adnexal mass with transvaginal ultrasound. The positive likelihood ratio showed this was a useful feature. The negative likelihood ratio showed this was not a useful feature.
- Moderate quality evidence from 1 cohort study (N=663) showed high sensitivity and specificity to detect tubal ectopic pregnancy using visualisation of a complex adnexal mass with transvaginal ultrasound. The positive and negative likelihood ratios showed this to be a very useful feature.
TVUS: Free fluid in the peritoneal cavity
- High quality evidence from 1 cohort study (N=94) showed low sensitivity and high specificity to detect tubal ectopic pregnancy using visualisation of free fluid in the peritoneal cavity with transvaginal ultrasound. The positive and negative likelihood ratios showed this to be not a useful feature.
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
The committee agreed that the correct and timely diagnosis of an ectopic pregnancy was vital to be able to offer the most appropriate management options to women. The committee identified the positive likelihood ratio as being of use in making a diagnosis of ectopic pregnancy. Features with a high positive likelihood ratio would increase the chance of identifying an ectopic pregnancy, making the correct diagnosis more likely.
This review aimed to determine the usefulness of individual features seen on an ultrasound scan, rather than whether or not ultrasound itself is a useful tool. Therefore it was noted that the sensitivity of individual features may not be particularly high – women with an ectopic pregnancy may have a variety of different features identified on scan, and a single feature could not be expected to be present in all women. The committee also noted that, overall, it was important not to miss a diagnosis of ectopic pregnancy (high sensitivity preferable), but that this would be accomplished through the current pathway of clinical follow up where scan findings were uncertain.
In addition, the specificity of certain features appeared to be very high in some studies – as the majority of women in the study had a viable, intrauterine pregnancy that was easily identified. Therefore the number of correctly identified “true negative” test results was high.
The committee therefore focused on the likelihood ratios when considering the evidence. Features showing a high positive likelihood ratio would mean that the chance of an ectopic pregnancy being present would be considerably increased. Similarly, a low positive likelihood ratio would reduce the clinical suspicion of an ectopic pregnancy.
The quality of the evidence
The quality of the evidence ranged from very low to high, with downgrading predominantly due to imprecision (based on the confidence intervals of both sensitivity and specificity) and concern over the risk of bias from participant flow (loss-to-follow up resulting in missing data from the final analysis).
On review of the evidence, it was noted that studies included different sub-populations of women. Some studies included all women with pain or bleeding in early pregnancy, others focused on women in whom a viable intrauterine pregnancy had been excluded. It was noted that the pre-test probability of an ectopic pregnancy differed markedly in these populations. Although an ectopic pregnancy is a relatively rare occurrence, if a viable intrauterine pregnancy cannot be seen, then the likelihood of an ectopic pregnancy is increased. Several studies reported on any woman presenting with pain or bleeding or any asymptomatic woman presenting for an ultrasound scan before 13+0 weeks gestation. Other studies excluded obvious IUPs (on first scan), and others excluded obvious IUPs and obvious ectopic pregnancies, so only presenting data for women with pregnancy of unknown location, or complex scan results.
Each of these populations were felt to be relevant to clinical practise, as women may undergo multiple ultrasound scans during the course of early pregnancy. For the first scan, data on all women is relevant. However, if a viable intrauterine pregnancy cannot be confirmed on this scan, then data on the “higher risk” populations becomes relevant. Therefore, the studies were separated into three distinct populations for consideration, but the quality of evidence was not downgraded for indirectness unless other concerns were noted.
The committee considered making separate recommendations for these groups of women (all women, and those at higher risk of ectopic pregnancy – in whom an intrauterine pregnancy had been excluded). However, it was felt that this may lead to a lack of clarity about how to apply the recommendations. Therefore the evidence from the different populations was considered together in order to make recommendations.
The committee discussed the age of the studies, and how the technical capabilities of ultrasound machines have improved over the last 20 years. They highlighted that the reported diagnostic accuracy for the visualisation of features in the studies pre-2000 may not reflect current practice, especially with the use of the transabdominal ultrasound in these earlier studies.
Benefits and harms
The committee noted that the evidence showed that visualisation of an adnexal mass with features of an early pregnancy (a gestational sac containing a yolk sac or fetal pole, with or without a fetal heartbeat) had a very high positive likelihood ratio for the diagnosis of ectopic pregnancy. This was entirely consistent with their clinical experience – that the identification of a mass showing such features would give a firm diagnosis. The committee did not consider that any other features could make such a definite diagnosis of an ectopic pregnancy.
However, other features were also shown to have a high positive likelihood ratio for the identification of ectopic pregnancy. Therefore, the committee agreed that these features should raise a strong suspicion of the diagnosis. These included the presence of a complex, inhomogeneous or non-cystic adnexal mass, or the presence of an adnexal mass with an empty gestation sac (containing no yolk sac, fetal pole or fetal heartbeat) (which may sometimes be described as a “tubal ring sign” or “bagel sign”).
The identification of a collection of fluid in the uterine cavity (which may sometimes be described as a pseudo-sac) or an empty uterus were not shown to have a high positive likelihood ratio for the diagnosis of ectopic pregnancy. However, based on their clinical expertise, the committee members agreed that these features, when present, should raise suspicion of ectopic pregnancy, but women presenting with these features would require further investigation.
The presence of free fluid in the peritoneal cavity on ultrasound scan was noted to cause challenges in interpretation. The committee were aware that a scan finding of “free fluid” could vary between a trace of fluid identified on transvaginal scan, to a large amount of free fluid visible transabdominally. The likelihood of an ectopic pregnancy would be very different in each of these circumstances. This was reflected in the evidence, where some studies showed a high positive likelihood ratio for the diagnosis of ectopic based on the presence of free fluid, and others showed a low positive likelihood ratio. From the evidence, there was no information as to the volume of free fluid in the peritoneal cavity that was visualised, how to measure it, or how the volume could be interpreted. The committee agreed that it may be a marker of an ectopic pregnancy based on the evidence presented, but free fluid alone could not be relied upon for a diagnosis, and women presenting with only this feature would require further investigation.
When scan findings were not conclusive (a diagnosis of ectopic pregnancy could not be made nor excluded) the committee stressed the importance of using other features to help determine the likelihood of an ectopic pregnancy being present. This would include assessing the clinical presentation and serum hCG levels, rather than relying on scan features alone.
The committee were aware that, although the incidence of heterotopic pregnancy (co-existing intrauterine pregnancy and ectopic pregnancy) is rare, it is known to be increasing. The committee members made a recommendation to highlight this issue, as clinicians should scan both the uterus and adnexa for any of the physical features of a pregnancy in all possible locations.
Diagnosis of tubal ectopic pregnancy using visualisation and correct interpretation of certain ultrasound features, will result in reduced delay in treatment and management of the ectopic pregnancy. This may permit a wider range of management options, such as medical or expectant management, in addition to surgery, giving greater choice for women. Early diagnosis should also reduce maternal mortality and morbidity.
Possible harms included the uncertainty of diagnosis in cases where an ultrasound is not definitive. This may lead to unnecessary concern or follow up for women who ultimately are identified as having an intrauterine pregnancy. However, the committee considered that the risks of a missed diagnosis of ectopic pregnancy were so great that this justified the additional follow up and monitoring that may be required.
The committee noted that the majority of the evidence reflected the accuracy of transvaginal, rather than transabdominal, scanning. Transabdominal scanning was considered less accurate, with poorer resolution, particularly at a lower gestational age. However, the committee were aware that some women may decline transvaginal scanning for a variety of reasons, and that this may put them at increased risk of an uncertain diagnosis.
The committee could not identify any obvious disadvantages to the use of certain features visualised on an ultrasound scan to make a diagnosis of ectopic pregnancy, however they acknowledged that ultrasound scan findings can be subjective, may depend on the operator experience, cannot be 100% accurate, and there will still be some false positives and false negatives.
Cost effectiveness and resource use
Ultrasound scanning is already used in women presenting to an early pregnancy unit and therefore there are no additional ultrasound costs due to these recommendations and no significant resource impact is anticipated. The committee agreed that early diagnosis of ectopic pregnancy using the visualisation of certain features on an ultrasound scan may lead to savings as it would lead to:
- Fewer visits to the hospital, clinic, or early pregnancy assessment unit to make a diagnosis
- Reduced number of blood tests (serum hCG) to make a diagnosis
- Reduced costs due to emergency admissions with ruptured ectopic pregnancies.
Overall, the committee agreed that there would be no significant resource impact from these recommendations.
Other factors the committee took into account
The committee were aware that interpretation of ultrasound findings is dependent upon the training of individuals performing the ultrasound scan and considered that each unit has to take the responsibility of having adequately trained and accredited professionals performing ultrasound scans.
The committee discussed that there may be additional factors regarding language barriers in women who did not speak English or women with learning disabilities, and therefore difficulty communicating the different degrees of certainty or uncertainty around the diagnosis of an ectopic pregnancy, and that clear information should be provided, tailored to an individual women’s needs.
The committee also noted that some women, or women from conservative groups within society may avoid transvaginal ultrasound (TVUS) due to possible stigma surrounding the insertion of an object into the vagina, and thus delay a diagnosis. These factors are often highlighted in maternal mortality reports, and the committee acknowledged the importance of working towards educating and supporting women to understand their health/clinical problems and help them to understand that TVUS can be helpful in making a more accurate diagnosis, but that transabdominal ultrasound could be used in these women if necessary (although was not as effective a tool for diagnosis).
References
Ahmed 2004
Ahmed, Ahmed A., Tom, Brian D. M., Calabrese, Peter, Ectopic pregnancy diagnosis and the pseudo-sac, Fertility and Sterility, 81, 1225–8, 2004 [PubMed: 15136081]Barnhart 2011
Barnhart, Kurt T., Fay, Courtney A., Suescum, Maria, Sammel, Mary D., Appleby, Dina, Shaunik, Alka, Dean, Anthony J., Clinical factors affecting the accuracy of ultrasonography in symptomatic first-trimester pregnancy, Obstetrics and Gynecology, 117, 299–306, 2011 [PubMed: 21252743]Dart 1998
Dart,R., Howard,K., Subclassification of indeterminate pelvic ultrasonograms: stratifying the risk of ectopic pregnancy, Academic Emergency Medicine, 5, 313–319, 1998 [PubMed: 9562194]Dart 2002
Dart, Robert Gerard, Burke, Garett, Dart, Linda, Subclassification of indeterminate pelvic ultrasonography: prospective evaluation of the risk of ectopic pregnancy, Annals of Emergency Medicine, 39, 382–8, 2002 [PubMed: 11919524]Hammoud 2005
Hammoud, Ahmad O., Hammoud, Ihab, Bujold, Emmanuel, Gonik, Bernard, Diamond, Michael P., Johnson, Samuel C., The role of sonographic endometrial patterns and endometrial thickness in the differential diagnosis of ectopic pregnancy, American Journal of Obstetrics and Gynecology, 192, 1370–5, 2005 [PubMed: 15902112]Malek-Mellouli 2013
Malek-Mellouli, Monia, Oumara, Maina, Ben Amara, Fethi, Zouch, Ons, Neji, Khaled, Reziga, Hedi, Prediction of ectopic pregnancy in early pregnancy of unknown location, La Tunisie medicale, 91, 27–32, 2013 [PubMed: 23404594]Mehta 1999
Mehta,T.S., Levine,D., McArdle,C.R., Lack of sensitivity of endometrial thickness in predicting the presence of an ectopic pregnancy, Journal of Ultrasound in Medicine, 18, 117–122, 1999 [PubMed: 10206804]Moore 2007
Moore, Chris, Todd, William M., O’Brien, Elizabeth, Lin, Henry, Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy, Academic emergency medicine : official journal of the Society for Academic Emergency Medicine, 14, 755–8, 2007 [PubMed: 17554008]Nadim 2018
Nadim, B., Infante, F., Lu, C., Sathasivam, N., Condous, G., Morphological ultrasound types known as ‘blob’ and ‘bagel’ signs should be reclassified from suggesting probable to indicating definite tubal ectopic pregnancy, Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology, 51, 543–549, 2018 [PubMed: 28195383]Sadek 1995
Sadek,A.L., Schiotz,H.A., Transvaginal sonography in the management of ectopic pregnancy, Acta Obstetricia et Gynecologica Scandinavica, 74, 293–296, 1995 [PubMed: 7732802]
Appendices
Appendix A. Review protocols
Table 3Review protocol for diagnostic accuracy for ultrasound features for tubal ectopic pregnancy
| Field (based on PRISMA-P) | Content |
|---|---|
| Key area in the scope | The accuracy and interpretation of biomarkers (human chorionic gonadotrophin [hCG], progesterone) and ultrasound in diagnosis, and identifying both the location and the viability of the pregnancy |
| Draft review question from the previous guideline | N/A |
| Actual review question | What ultrasound features are most diagnostic of a tubal ectopic pregnancy? |
| Type of review question | Diagnostic accuracy |
| Objective of the review | To identify what ultrasound criteria can be used to make a diagnosis of tubal ectopic pregnancy (new evidence identified by surveillance) |
| Eligibility criteria – population/disease/condition/issue/domain |
Pregnant women presenting in early pregnancy (<13 weeks) with pain or vaginal bleeding, (includes women with a previous history of ectopic pregnancy, pelvic inflammatory disease, pregnancy with coil in situ, women with IVF) Asymptomatic pregnant women with indeterminate features on ultrasound, or pregnancy of unknown location (when scan does not show any pregnancy) |
| Eligibility criteria – intervention(s)/exposure(s)/prognostic factor(s) | Ultrasonography with the following features: Uterus:
Tube and ovary:
Peritoneal cavity:
|
| Eligibility criteria – comparator(s)/control or reference (gold) standard |
|
| Outcomes and prioritisation |
|
| Eligibility criteria – study design | Only published full text papers in English
Conference abstracts will only be considered if no evidence is available from full published studies |
| Other exclusion criteria |
|
| Proposed stratified, sensitivity/sub-group analysis, or meta-regression |
Transabdominal and transvaginal scans will be analysed as separate subgroups, and data will not be combined If possible, asymptomatic women will be analysed as a subgroup |
| Selection process – duplicate screening/selection/analysis | Duplicate screening/selection/analysis will not be undertaken for this review as this question was not prioritised for it. Included and excluded studies will be cross checked with the committee and with published systematic reviews when available. |
| Data management (software) |
A bivariate random effects model will be used to conduct pairwise meta-analysis with, for example, the metandi package in STATA. STAR will be used for bibliographies/citations, text mining, and study sifting, data extraction and quality assessment/critical appraisal. |
| Information sources – databases and dates |
Sources to be searched: Medline, Medline In-Process, CCTR, CDSR, DARE, HTA and Embase. Limits (e.g. date, study design): All study designs. Apply standard animal/non-English language filters. Date limited to 1995 onwards. Supplementary search techniques: No supplementary search techniques were used. See appendix B for full strategies. Key papers:
|
| Identify if an update | Not an update |
| Author contacts |
Developer: National Guideline Alliance |
| Highlight if amendment to previous protocol | For details please see section 4.5 of Developing NICE guidelines: the manual 2014 |
| Search strategy – for one database | For details please see appendix B |
| Data collection process – forms/duplicate | A standardised evidence table format will be used, and published as appendix D (clinical evidence tables) |
| Data items – define all variables to be collected | For details please see evidence tables in appendix D (clinical evidence tables) |
| Methods for assessing bias at outcome/study level |
Appraisal of methodological quality: The methodological quality of each study will be assessed using an appropriate checklist: QUADAS –II checklist for diagnostic studies For details please see section 6.2 of Developing NICE guidelines: the manual 2014 The risk of bias across all available evidence will evaluated for each outcome using an adaptation of the ‘Grading of Recommendations Assessment, Development and Evaluation (GRADE) toolbox’ developed by the international GRADE working group http://www |
| Criteria for quantitative synthesis | For details please see section 6.4 of Developing NICE guidelines: the manual 2014 |
| Methods for quantitative analysis – combining studies and exploring (in)consistency |
Synthesis of data: Meta-analysis will be conducted where appropriate using STATA. Minimally important differences Sensitivity: ≥ 75% very useful test < 50% not a useful test Specificity: ≥ 80% very useful test < 50% not a useful test |
| Meta-bias assessment – publication bias, selective reporting bias | For details please see section 6.2 of Developing NICE guidelines: the manual 2014. |
| Confidence in cumulative evidence | For details please see sections 6.4 and 9.1 of Developing NICE guidelines: the manual 2014 |
| Rationale/context – what is known | For details please see the introduction to the evidence review |
| Describe contributions of authors and guarantor |
A multidisciplinary committee developed the guideline. The committee was convened by the NGA and chaired by Sarah Fishburn in line with section 3 of Developing NICE guidelines: the manual 2014. Staff from the NGA undertook systematic literature searches, appraised the evidence, conducted meta-analysis and cost-effectiveness analysis where appropriate, and drafted the guideline in collaboration with the committee. For details please see Supplement 2 |
| Sources of funding/support | The NGA is funded by NICE and hosted by the Royal College of Obstetricians and Gynaecologists |
| Name of sponsor | The NGA is funded by NICE and hosted by the Royal College of Obstetricians and Gynaecologists |
| Roles of sponsor | NICE funds the NGA to develop guidelines for the NHS in England. |
| PROSPERO registration number | Not registered with PROSPERO |
Appendix B. Literature search strategies
Review question search strategies
Databases: Medline; Medline EPub Ahead of Print; and Medline In-Process & Other Non-Indexed Citations
| # | Searches |
|---|---|
| 1 | exp PREGNANCY, ECTOPIC/ |
| 2 | ((ectopic or extra uterine or extra?uterine or tub$ or ampullary or isthm$ or fimbrial or cornual or interstitial or abdom$ or ovar$ or cervi$) adj3 (pregnan$ or gestat$)).ti,ab. |
| 3 | (pregnan$ adj3 ((unknown or uncertain) adj (location$ or site$))).ti,ab. |
| 4 | PUL.ti,ab. |
| 5 | or/1–4 |
| 6 | DIAGNOSIS/ |
| 7 | exp DIAGNOSIS, COMPUTER-ASSISTED/ |
| 8 | DIAGNOSIS, DIFFERENTIAL/ |
| 9 | exp DIAGNOSTIC ERRORS/ |
| 10 | EARLY DIAGNOSIS/ |
| 11 | diagnos$.ti,ab. |
| 12 | or/6–11 |
| 13 | (ultraso$ adj3 featur$).ti,ab. |
| 14 | (empty adj3 uterus$).ti,ab. |
| 15 | (no adj3 intrauterin$ adj3 pregnanc$).ti,ab. |
| 16 | (pseudo$ adj3 sac?).ti,ab. |
| 17 | (decidual adj3 cyst?).ti,ab. |
| 18 | (cyst$ adj3 inside adj3 uterus$).ti,ab. |
| 19 | (fluid? adj3 inside adj3 uterus$).ti,ab. |
| 20 | (heterotopic$ adj3 pregnan$).ti,ab. |
| 21 | ((coexist$ or co-exist$) adj3 (intrauterin$ or IUP) adj3 (ectopic$ or EP)).ti,ab. |
| 22 | adnexal mass$.ti,ab. |
| 23 | yolk sac?.ti,ab. |
| 24 | ((fetal or fetus) adj2 pole?).ti,ab. |
| 25 | ((fetal or fetus) adj2 (heartbeat? or heartrate?)).ti,ab. |
| 26 | ((fetal or fetus) adj2 heart adj2 (beat$ or rate?)).ti,ab. |
| 27 | (Tubal adj3 ring?).ti,ab. |
| 28 | ((bagel? or donut? or doughnut? or blob?) adj3 sign?).ti,ab. |
| 29 | Adnexal cyst?.ti,ab. |
| 30 | (Identif$ adj3 (fluid? or blood$)).ti,ab. |
| 31 | (Free$ adj3 fluid?).ti,ab. |
| 32 | H?emoperitoneum.ti,ab. |
| 33 | (Free$ adj3 blood$ adj3 pelvi$).ti,ab. |
| 34 | or/13–33 |
| 35 | exp ULTRASONOGRAPHY/ |
| 36 | ultrasonograph$.ti,ab. |
| 37 | sonograph$.ti,ab. |
| 38 | ultrasound.ti,ab. |
| 39 | ultrasonic$.ti,ab. |
| 40 | sonogram?.ti,ab. |
| 41 | Echocardiograph$.ti,ab. |
| 42 | Echoencephalograph$.ti,ab. |
| 43 | Echograph$.ti,ab. |
| 44 | Echotomograph$.ti,ab. |
| 45 | Endosonograph$.ti,ab. |
| 46 | or/35–45 |
| 47 | Positive likelihood ratio?.ti,ab. |
| 48 | LR+.ti,ab. |
| 49 | Negative likelihood ratio?.ti,ab. |
| 50 | LR-.ti,ab. |
| 51 | AREA UNDER CURVE/ |
| 52 | (area? under adj2 curve?).ti,ab. |
| 53 | AUC?.ti,ab. |
| 54 | “SENSITIVITY AND SPECIFICITY”/ |
| 55 | (sensitiv$ adj10 specific$).ti,ab. |
| 56 | or/47–55 |
| 57 | exp PREGNANCY, ECTOPIC/di [Diagnosis] |
| 58 | exp PREGNANCY, ECTOPIC/dg [Diagnostic Imaging] |
| 59 | 5 and 12 and 34 |
| 60 | 5 and 12 and 46 and 56 |
| 61 | 34 and 57 |
| 62 | 34 and 58 |
| 63 | or/59–62 |
| 64 | limit 63 to english language |
| 65 | limit 64 to yr=“1995 -Current” |
| 66 | LETTER/ |
| 67 | EDITORIAL/ |
| 68 | NEWS/ |
| 69 | exp HISTORICAL ARTICLE/ |
| 70 | ANECDOTES AS TOPIC/ |
| 71 | COMMENT/ |
| 72 | CASE REPORT/ |
| 73 | (letter or comment*).ti. |
| 74 | or/66–73 |
| 75 | RANDOMIZED CONTROLLED TRIAL/ or random*.ti,ab. |
| 76 | 74 not 75 |
| 77 | ANIMALS/ not HUMANS/ |
| 78 | exp ANIMALS, LABORATORY/ |
| 79 | exp ANIMAL EXPERIMENTATION/ |
| 80 | exp MODELS, ANIMAL/ |
| 81 | exp RODENTIA/ |
| 82 | (rat or rats or mouse or mice).ti. |
| 83 | or/76–82 |
| 84 | 65 not 83 |
Databases: Embase; and Embase Classic
| # | Searches |
|---|---|
| 1 | exp ECTOPIC PREGNANCY/ |
| 2 | ((ectopic or extra uterine or extra?uterine or tub$ or ampullary or isthm$ or fimbrial or cornual or interstitial or abdom$ or ovar$ or cervi$) adj3 (pregnan$ or gestat$)).ti,ab. |
| 3 | (pregnan$ adj3 ((unknown or uncertain) adj (location$ or site$))).ti,ab. |
| 4 | PUL.ti,ab. |
| 5 | or/1–4 |
| 6 | *DIAGNOSIS/ |
| 7 | *COMPUTER ASSISTED DIAGNOSIS/ |
| 8 | *DIFFERENTIAL DIAGNOSIS/ |
| 9 | exp *DIAGNOSTIC ERROR/ |
| 10 | *EARLY DIAGNOSIS/ |
| 11 | diagnos$.ti,ab. |
| 12 | or/6–11 |
| 13 | (ultraso$ adj3 featur$).ti,ab. |
| 14 | (empty adj3 uterus$).ti,ab. |
| 15 | (no adj3 intrauterin$ adj3 pregnanc$).ti,ab. |
| 16 | (pseudo$ adj3 sac?).ti,ab. |
| 17 | (decidual adj3 cyst?).ti,ab. |
| 18 | (cyst$ adj3 inside adj3 uterus$).ti,ab. |
| 19 | (fluid? adj3 inside adj3 uterus$).ti,ab. |
| 20 | (heterotopic$ adj3 pregnan$).ti,ab. |
| 21 | ((coexist$ or co-exist$) adj3 (intrauterin$ or IUP) adj3 (ectopic$ or EP)).ti,ab. |
| 22 | adnexal mass$.ti,ab. |
| 23 | yolk sac?.ti,ab. |
| 24 | ((fetal or fetus) adj2 pole?).ti,ab. |
| 25 | ((fetal or fetus) adj2 (heartbeat? or heartrate?)).ti,ab. |
| 26 | ((fetal or fetus) adj2 heart adj2 (beat$ or rate?)).ti,ab. |
| 27 | (Tubal adj3 ring?).ti,ab. |
| 28 | ((bagel? or donut? or doughnut? or blob?) adj3 sign?).ti,ab. |
| 29 | Adnexal cyst?.ti,ab. |
| 30 | (Identif$ adj3 (fluid? or blood$)).ti,ab. |
| 31 | (Free$ adj3 fluid?).ti,ab. |
| 32 | H?emoperitoneum.ti,ab. |
| 33 | (Free$ adj3 blood$ adj3 pelvi$).ti,ab. |
| 34 | or/13–33 |
| 35 | exp *ECHOGRAPHY/ |
| 36 | ultrasonograph$.ti,ab. |
| 37 | sonograph$.ti,ab. |
| 38 | ultrasound.ti,ab. |
| 39 | ultrasonic$.ti,ab. |
| 40 | sonogram?.ti,ab. |
| 41 | Echocardiograph$.ti,ab. |
| 42 | Echoencephalograph$.ti,ab. |
| 43 | Echograph$.ti,ab. |
| 44 | Echotomograph$.ti,ab. |
| 45 | Endosonograph$.ti,ab. |
| 46 | or/35–45 |
| 47 | Positive likelihood ratio?.ti,ab. |
| 48 | LR+.ti,ab. |
| 49 | Negative likelihood ratio?.ti,ab. |
| 50 | LR-.ti,ab. |
| 51 | AREA UNDER THE CURVE/ |
| 52 | (area? under adj2 curve?).ti,ab. |
| 53 | AUC?.ti,ab. |
| 54 | “SENSITIVITY AND SPECIFICITY”/ |
| 55 | (sensitiv$ adj10 specific$).ti,ab. |
| 56 | or/47–55 |
| 57 | exp *ECTOPIC PREGNANCY/di [Diagnosis] |
| 58 | 5 and 12 and 34 |
| 59 | 5 and 12 and 46 and 56 |
| 60 | 34 and 57 |
| 61 | or/58–60 |
| 62 | limit 61 to english language |
| 63 | limit 62 to yr=“1995 -Current” |
| 64 | letter.pt. or LETTER/ |
| 65 | note.pt. |
| 66 | editorial.pt. |
| 67 | CASE REPORT/ or CASE STUDY/ |
| 68 | (letter or comment*).ti. |
| 69 | or/64–68 |
| 70 | RANDOMIZED CONTROLLED TRIAL/ or random*.ti,ab. |
| 71 | 69 not 70 |
| 72 | ANIMAL/ not HUMAN/ |
| 73 | NONHUMAN/ |
| 74 | exp ANIMAL EXPERIMENT/ |
| 75 | exp EXPERIMENTAL ANIMAL/ |
| 76 | ANIMAL MODEL/ |
| 77 | exp RODENT/ |
| 78 | (rat or rats or mouse or mice).ti. |
| 79 | or/71–78 |
| 80 | 63 not 79 |
Databases: Cochrane Central Register of Controlled Trials; Cochrane Database of Systematic Reviews; Database of Abstracts of Reviews of Effects; and Health Technology Assessment
| # | Searches |
|---|---|
| 1 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees |
| 2 | ((ectopic or extra uterine or extra*uterine or tub* or ampullary or isthm* or fimbrial or cornual or interstitial or abdom* or ovar* or cervi*) near/3 (pregnan* or gestat*)):ti,ab |
| 3 | (pregnan* near/3 ((unknown or uncertain) near/1 (location* or site*))):ti,ab |
| 4 | PUL:ti,ab |
| 5 | #1 or #2 or #3 or #4 |
| 6 | MeSH descriptor: [DIAGNOSIS] this term only |
| 7 | MeSH descriptor: [DIAGNOSIS, COMPUTER-ASSISTED] explode all trees |
| 8 | MeSH descriptor: [DIAGNOSIS, DIFFERENTIAL] this term only |
| 9 | MeSH descriptor: [DIAGNOSTIC ERRORS] explode all trees |
| 10 | MeSH descriptor: [EARLY DIAGNOSIS] this term only |
| 11 | diagnos*:ti,ab |
| 12 | #6 or #7 or #8 or #9 or #10 or #11 |
| 13 | (ultraso* near/3 featur*):ti,ab |
| 14 | (empty near/3 uterus*):ti,ab |
| 15 | (no near/3 intrauterin* near/3 pregnanc*):ti,ab |
| 16 | (pseudo* near/3 sac*):ti,ab |
| 17 | (decidual near/3 cyst*):ti,ab |
| 18 | (cyst* near/3 inside near/3 uterus*):ti,ab |
| 19 | (fluid* near/3 inside near/3 uterus*):ti,ab |
| 20 | (heterotopic* near/3 pregnan*):ti,ab |
| 21 | ((coexist* or co-exist*) near/3 (intrauterin* or IUP) near/3 (ectopic* or EP)):ti,ab |
| 22 | “adnexal mass*”:ti,ab |
| 23 | “yolk sac*”:ti,ab |
| 24 | ((fetal or fetus) near/2 pole*):ti,ab |
| 25 | ((fetal or fetus) near/2 (heartbeat* or heartrate*)):ti,ab |
| 26 | ((fetal or fetus) near/2 heart near/2 (beat* or rate*)):ti,ab |
| 27 | (Tubal near/3 ring*):ti,ab |
| 28 | ((bagel* or donut* or doughnut* or blob*) near/3 sign*):ti,ab |
| 29 | “Adnexal cyst*”:ti,ab |
| 30 | (Identif* near/3 (fluid* or blood*)):ti,ab |
| 31 | (Free* near/3 fluid*):ti,ab |
| 32 | (Hemoperitoneum or Haemoperitoneum):ti,ab |
| 33 | (Free* near/3 blood* near/3 pelvi*):ti,ab |
| 34 | #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 |
| 35 | MeSH descriptor: [ULTRASONOGRAPHY] explode all trees |
| 36 | ultrasonograph*:ti,ab |
| 37 | sonograph*:ti,ab |
| 38 | ultrasound:ti,ab |
| 39 | ultrasonic*:ti,ab |
| 40 | sonogram*:ti,ab |
| 41 | Echocardiograph*:ti,ab |
| 42 | Echoencephalograph*:ti,ab |
| 43 | Echograph*:ti,ab |
| 44 | Echotomograph*:ti,ab |
| 45 | Endosonograph*:ti,ab |
| 46 | #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 |
| 47 | “Positive likelihood ratio*”:ti,ab |
| 48 | “Negative likelihood ratio*”:ti,ab |
| 49 | LR*:ti,ab |
| 50 | MeSH descriptor: [AREA UNDER CURVE] this term only |
| 51 | (“area* under” near/2 curve*):ti,ab |
| 52 | AUC*:ti,ab |
| 53 | MeSH descriptor: [SENSITIVITY AND SPECIFICITY] this term only |
| 54 | (sensitiv* near/10 specific*):ti,ab |
| 55 | #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 |
| 56 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnosis - DI] |
| 57 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnostic imaging - DG] |
| 58 | #5 and #12 and #34 |
| 59 | #5 and #12 and #46 and #55 |
| 60 | #34 and #56 |
| 61 | #34 and #57 |
| 62 | #58 or #59 or #60 or #61 Publication Year from 1995 to 2018 |
Health economics search strategies
Databases: Medline; Medline EPub Ahead of Print; and Medline In-Process & Other Non-Indexed Citations
| # | Searches |
|---|---|
| 1 | ECONOMICS/ |
| 2 | VALUE OF LIFE/ |
| 3 | exp “COSTS AND COST ANALYSIS”/ |
| 4 | exp ECONOMICS, HOSPITAL/ |
| 5 | exp ECONOMICS, MEDICAL/ |
| 6 | exp RESOURCE ALLOCATION/ |
| 7 | ECONOMICS, NURSING/ |
| 8 | ECONOMICS, PHARMACEUTICAL/ |
| 9 | exp “FEES AND CHARGES”/ |
| 10 | exp BUDGETS/ |
| 11 | budget*.ti,ab. |
| 12 | cost*.ti,ab. |
| 13 | (economic* or pharmaco?economic*).ti,ab. |
| 14 | (price* or pricing*).ti,ab. |
| 15 | (financ* or fee or fees or expenditure* or saving*).ti,ab. |
| 16 | (value adj2 (money or monetary)).ti,ab. |
| 17 | resourc* allocat*.ti,ab. |
| 18 | (fund or funds or funding* or funded).ti,ab. |
| 19 | (ration or rations or rationing* or rationed).ti,ab. |
| 20 | ec.fs. |
| 21 | or/1–20 |
| 22 | exp PREGNANCY, ECTOPIC/ |
| 23 | ((ectopic or extra uterine or extra?uterine or tub$ or ampullary or isthm$ or fimbrial or cornual or interstitial or abdom$ or ovar$ or cervi$) adj3 (pregnan$ or gestat$)).ti,ab. |
| 24 | (pregnan$ adj3 ((unknown or uncertain) adj (location$ or site$))).ti,ab. |
| 25 | PUL.ti,ab. |
| 26 | or/22–25 |
| 27 | DIAGNOSIS/ |
| 28 | exp DIAGNOSIS, COMPUTER-ASSISTED/ |
| 29 | DIAGNOSIS, DIFFERENTIAL/ |
| 30 | exp DIAGNOSTIC ERRORS/ |
| 31 | EARLY DIAGNOSIS/ |
| 32 | diagnos$.ti,ab. |
| 33 | or/27–32 |
| 34 | (ultraso$ adj3 featur$).ti,ab. |
| 35 | (empty adj3 uterus$).ti,ab. |
| 36 | (no adj3 intrauterin$ adj3 pregnanc$).ti,ab. |
| 37 | (pseudo$ adj3 sac?).ti,ab. |
| 38 | (decidual adj3 cyst?).ti,ab. |
| 39 | (cyst$ adj3 inside adj3 uterus$).ti,ab. |
| 40 | (fluid? adj3 inside adj3 uterus$).ti,ab. |
| 41 | (heterotopic$ adj3 pregnan$).ti,ab. |
| 42 | ((coexist$ or co-exist$) adj3 (intrauterin$ or IUP) adj3 (ectopic$ or EP)).ti,ab. |
| 43 | adnexal mass$.ti,ab. |
| 44 | yolk sac?.ti,ab. |
| 45 | ((fetal or fetus) adj2 pole?).ti,ab. |
| 46 | ((fetal or fetus) adj2 (heartbeat? or heartrate?)).ti,ab. |
| 47 | ((fetal or fetus) adj2 heart adj2 (beat$ or rate?)).ti,ab. |
| 48 | (Tubal adj3 ring?).ti,ab. |
| 49 | ((bagel? or donut? or doughnut? or blob?) adj3 sign?).ti,ab. |
| 50 | Adnexal cyst?.ti,ab. |
| 51 | (Identif$ adj3 (fluid? or blood$)).ti,ab. |
| 52 | (Free$ adj3 fluid?).ti,ab. |
| 53 | H?emoperitoneum.ti,ab. |
| 54 | (Free$ adj3 blood$ adj3 pelvi$).ti,ab. |
| 55 | or/34–54 |
| 56 | exp ULTRASONOGRAPHY/ |
| 57 | ultrasonograph$.ti,ab. |
| 58 | sonograph$.ti,ab. |
| 59 | ultrasound.ti,ab. |
| 60 | ultrasonic$.ti,ab. |
| 61 | sonogram?.ti,ab. |
| 62 | Echocardiograph$.ti,ab. |
| 63 | Echoencephalograph$.ti,ab. |
| 64 | Echograph$.ti,ab. |
| 65 | Echotomograph$.ti,ab. |
| 66 | Endosonograph$.ti,ab. |
| 67 | or/56–66 |
| 68 | Positive likelihood ratio?.ti,ab. |
| 69 | LR+.ti,ab. |
| 70 | Negative likelihood ratio?.ti,ab. |
| 71 | LR-.ti,ab. |
| 72 | AREA UNDER CURVE/ |
| 73 | (area? under adj2 curve?).ti,ab. |
| 74 | AUC?.ti,ab. |
| 75 | “SENSITIVITY AND SPECIFICITY”/ |
| 76 | (sensitiv$ adj10 specific$).ti,ab. |
| 77 | or/68–76 |
| 78 | exp PREGNANCY, ECTOPIC/di [Diagnosis] |
| 79 | exp PREGNANCY, ECTOPIC/dg [Diagnostic Imaging] |
| 80 | 26 and 33 and 55 |
| 81 | 26 and 33 and 67 and 77 |
| 82 | 55 and 78 |
| 83 | 55 and 79 |
| 84 | or/80–83 |
| 85 | limit 84 to english language |
| 86 | limit 85 to yr=“1995 -Current” |
| 87 | LETTER/ |
| 88 | EDITORIAL/ |
| 89 | NEWS/ |
| 90 | exp HISTORICAL ARTICLE/ |
| 91 | ANECDOTES AS TOPIC/ |
| 92 | COMMENT/ |
| 93 | CASE REPORT/ |
| 94 | (letter or comment*).ti. |
| 95 | or/87–94 |
| 96 | RANDOMIZED CONTROLLED TRIAL/ or random*.ti,ab. |
| 97 | 95 not 96 |
| 98 | ANIMALS/ not HUMANS/ |
| 99 | exp ANIMALS, LABORATORY/ |
| 100 | exp ANIMAL EXPERIMENTATION/ |
| 101 | exp MODELS, ANIMAL/ |
| 102 | exp RODENTIA/ |
| 103 | (rat or rats or mouse or mice).ti. |
| 104 | or/97–103 |
| 105 | 86 not 104 |
| 106 | 21 and 105 |
Databases: Embase; and Embase Classic
| # | Searches |
|---|---|
| 1 | HEALTH ECONOMICS/ |
| 2 | exp ECONOMIC EVALUATION/ |
| 3 | exp HEALTH CARE COST/ |
| 4 | exp FEE/ |
| 5 | BUDGET/ |
| 6 | FUNDING/ |
| 7 | RESOURCE ALLOCATION/ |
| 8 | budget*.ti,ab. |
| 9 | cost*.ti,ab. |
| 10 | (economic* or pharmaco?economic*).ti,ab. |
| 11 | (price* or pricing*).ti,ab. |
| 12 | (financ* or fee or fees or expenditure* or saving*).ti,ab. |
| 13 | (value adj2 (money or monetary)).ti,ab. |
| 14 | resourc* allocat*.ti,ab. |
| 15 | (fund or funds or funding* or funded).ti,ab. |
| 16 | (ration or rations or rationing* or rationed).ti,ab. |
| 17 | or/1–16 |
| 18 | exp ECTOPIC PREGNANCY/ |
| 19 | ((ectopic or extra uterine or extra?uterine or tub$ or ampullary or isthm$ or fimbrial or cornual or interstitial or abdom$ or ovar$ or cervi$) adj3 (pregnan$ or gestat$)).ti,ab. |
| 20 | (pregnan$ adj3 ((unknown or uncertain) adj (location$ or site$))).ti,ab. |
| 21 | PUL.ti,ab. |
| 22 | or/18–21 |
| 23 | *DIAGNOSIS/ |
| 24 | *COMPUTER ASSISTED DIAGNOSIS/ |
| 25 | *DIFFERENTIAL DIAGNOSIS/ |
| 26 | exp *DIAGNOSTIC ERROR/ |
| 27 | *EARLY DIAGNOSIS/ |
| 28 | diagnos$.ti,ab. |
| 29 | or/23–28 |
| 30 | (ultraso$ adj3 featur$).ti,ab. |
| 31 | (empty adj3 uterus$).ti,ab. |
| 32 | (no adj3 intrauterin$ adj3 pregnanc$).ti,ab. |
| 33 | (pseudo$ adj3 sac?).ti,ab. |
| 34 | (decidual adj3 cyst?).ti,ab. |
| 35 | (cyst$ adj3 inside adj3 uterus$).ti,ab. |
| 36 | (fluid? adj3 inside adj3 uterus$).ti,ab. |
| 37 | (heterotopic$ adj3 pregnan$).ti,ab. |
| 38 | ((coexist$ or co-exist$) adj3 (intrauterin$ or IUP) adj3 (ectopic$ or EP)).ti,ab. |
| 39 | adnexal mass$.ti,ab. |
| 40 | yolk sac?.ti,ab. |
| 41 | ((fetal or fetus) adj2 pole?).ti,ab. |
| 42 | ((fetal or fetus) adj2 (heartbeat? or heartrate?)).ti,ab. |
| 43 | ((fetal or fetus) adj2 heart adj2 (beat$ or rate?)).ti,ab. |
| 44 | (Tubal adj3 ring?).ti,ab. |
| 45 | ((bagel? or donut? or doughnut? or blob?) adj3 sign?).ti,ab. |
| 46 | Adnexal cyst?.ti,ab. |
| 47 | (Identif$ adj3 (fluid? or blood$)).ti,ab. |
| 48 | (Free$ adj3 fluid?).ti,ab. |
| 49 | H?emoperitoneum.ti,ab. |
| 50 | (Free$ adj3 blood$ adj3 pelvi$).ti,ab. |
| 51 | or/30–50 |
| 52 | exp *ECHOGRAPHY/ |
| 53 | ultrasonograph$.ti,ab. |
| 54 | sonograph$.ti,ab. |
| 55 | ultrasound.ti,ab. |
| 56 | ultrasonic$.ti,ab. |
| 57 | sonogram?.ti,ab. |
| 58 | Echocardiograph$.ti,ab. |
| 59 | Echoencephalograph$.ti,ab. |
| 60 | Echograph$.ti,ab. |
| 61 | Echotomograph$.ti,ab. |
| 62 | Endosonograph$.ti,ab. |
| 63 | or/52–62 |
| 64 | Positive likelihood ratio?.ti,ab. |
| 65 | LR+.ti,ab. |
| 66 | Negative likelihood ratio?.ti,ab. |
| 67 | LR-.ti,ab. |
| 68 | AREA UNDER THE CURVE/ |
| 69 | (area? under adj2 curve?).ti,ab. |
| 70 | AUC?.ti,ab. |
| 71 | “SENSITIVITY AND SPECIFICITY”/ |
| 72 | (sensitiv$ adj10 specific$).ti,ab. |
| 73 | or/64–72 |
| 74 | exp *ECTOPIC PREGNANCY/di [Diagnosis] |
| 75 | 22 and 29 and 51 |
| 76 | 22 and 29 and 63 and 73 |
| 77 | 51 and 74 |
| 78 | or/75–77 |
| 79 | limit 78 to english language |
| 80 | limit 79 to yr=“1995 -Current” |
| 81 | letter.pt. or LETTER/ |
| 82 | note.pt. |
| 83 | editorial.pt. |
| 84 | CASE REPORT/ or CASE STUDY/ |
| 85 | (letter or comment*).ti. |
| 86 | or/81–85 |
| 87 | RANDOMIZED CONTROLLED TRIAL/ or random*.ti,ab. |
| 88 | 86 not 87 |
| 89 | ANIMAL/ not HUMAN/ |
| 90 | NONHUMAN/ |
| 91 | exp ANIMAL EXPERIMENT/ |
| 92 | exp EXPERIMENTAL ANIMAL/ |
| 93 | ANIMAL MODEL/ |
| 94 | exp RODENT/ |
| 95 | (rat or rats or mouse or mice).ti. |
| 96 | or/88–95 |
| 97 | 80 not 96 |
| 98 | 17 and 97 |
Database: Cochrane Central Register of Controlled Trials
| # | Searches |
|---|---|
| 1 | MeSH descriptor: [ECONOMICS] this term only |
| 2 | MeSH descriptor: [VALUE OF LIFE] this term only |
| 3 | MeSH descriptor: [COSTS AND COST ANALYSIS] explode all trees |
| 4 | MeSH descriptor: [ECONOMICS, HOSPITAL] explode all trees |
| 5 | MeSH descriptor: [ECONOMICS, MEDICAL] explode all trees |
| 6 | MeSH descriptor: [RESOURCE ALLOCATION] explode all trees |
| 7 | MeSH descriptor: [ECONOMICS, NURSING] this term only |
| 8 | MeSH descriptor: [ECONOMICS, PHARMACEUTICAL] this term only |
| 9 | MeSH descriptor: [FEES AND CHARGES] explode all trees |
| 10 | MeSH descriptor: [BUDGETS] explode all trees |
| 11 | budget*:ti,ab |
| 12 | cost*:ti,ab |
| 13 | (economic* or pharmaco?economic*):ti,ab |
| 14 | (price* or pricing*):ti,ab |
| 15 | (financ* or fee or fees or expenditure* or saving*):ti,ab |
| 16 | (value near/2 (money or monetary)):ti,ab |
| 17 | resourc* allocat*:ti,ab |
| 18 | (fund or funds or funding* or funded):ti,ab |
| 19 | (ration or rations or rationing* or rationed):ti,ab |
| 20 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 |
| 21 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees |
| 22 | ((ectopic or extra uterine or extra*uterine or tub* or ampullary or isthm* or fimbrial or cornual or interstitial or abdom* or ovar* or cervi*) near/3 (pregnan* or gestat*)):ti,ab |
| 23 | (pregnan* near/3 ((unknown or uncertain) near/1 (location* or site*))):ti,ab |
| 24 | PUL:ti,ab |
| 25 | #21 or #22 or #23 or #24 |
| 26 | MeSH descriptor: [DIAGNOSIS] this term only |
| 27 | MeSH descriptor: [DIAGNOSIS, COMPUTER-ASSISTED] explode all trees |
| 28 | MeSH descriptor: [DIAGNOSIS, DIFFERENTIAL] this term only |
| 29 | MeSH descriptor: [DIAGNOSTIC ERRORS] explode all trees |
| 30 | MeSH descriptor: [EARLY DIAGNOSIS] this term only |
| 31 | diagnos*:ti,ab |
| 32 | #26 or #27 or #28 or #29 or #30 or #31 |
| 33 | (ultraso* near/3 featur*):ti,ab |
| 34 | (empty near/3 uterus*):ti,ab |
| 35 | (no near/3 intrauterin* near/3 pregnanc*):ti,ab |
| 36 | (pseudo* near/3 sac*):ti,ab |
| 37 | (decidual near/3 cyst*):ti,ab |
| 38 | (cyst* near/3 inside near/3 uterus*):ti,ab |
| 39 | (fluid* near/3 inside near/3 uterus*):ti,ab |
| 40 | (heterotopic* near/3 pregnan*):ti,ab |
| 41 | ((coexist* or co-exist*) near/3 (intrauterin* or IUP) near/3 (ectopic* or EP)):ti,ab |
| 42 | “adnexal mass*”:ti,ab |
| 43 | “yolk sac*”:ti,ab |
| 44 | ((fetal or fetus) near/2 pole*):ti,ab |
| 45 | ((fetal or fetus) near/2 (heartbeat* or heartrate*)):ti,ab |
| 46 | ((fetal or fetus) near/2 heart near/2 (beat* or rate*)):ti,ab |
| 47 | (Tubal near/3 ring*):ti,ab |
| 48 | ((bagel* or donut* or doughnut* or blob*) near/3 sign*):ti,ab |
| 49 | “Adnexal cyst*”:ti,ab |
| 50 | (Identif* near/3 (fluid* or blood*)):ti,ab |
| 51 | (Free* near/3 fluid*):ti,ab |
| 52 | (Hemoperitoneum or Haemoperitoneum):ti,ab |
| 53 | (Free* near/3 blood* near/3 pelvi*):ti,ab |
| 54 | #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 |
| 55 | MeSH descriptor: [ULTRASONOGRAPHY] explode all trees |
| 56 | ultrasonograph*:ti,ab |
| 57 | sonograph*:ti,ab |
| 58 | ultrasound:ti,ab |
| 59 | ultrasonic*:ti,ab |
| 60 | sonogram*:ti,ab |
| 61 | Echocardiograph*:ti,ab |
| 62 | Echoencephalograph*:ti,ab |
| 63 | Echograph*:ti,ab |
| 64 | Echotomograph*:ti,ab |
| 65 | Endosonograph*:ti,ab |
| 66 | #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 |
| 67 | “Positive likelihood ratio*”:ti,ab |
| 68 | “Negative likelihood ratio*”:ti,ab |
| 69 | LR*:ti,ab |
| 70 | MeSH descriptor: [AREA UNDER CURVE] this term only |
| 71 | (“area* under” near/2 curve*):ti,ab |
| 72 | AUC*:ti,ab |
| 73 | MeSH descriptor: [SENSITIVITY AND SPECIFICITY] this term only |
| 74 | (sensitiv* near/10 specific*):ti,ab |
| 75 | #67 or #68 or #69 or #70 or #71 or #72 or #73 or #74 |
| 76 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnosis - DI] |
| 77 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnostic imaging - DG] |
| 78 | #25 and #32 and #54 |
| 79 | #25 and #32 and #66 and #75 |
| 80 | #54 and #76 |
| 81 | #54 and #77 |
| 82 | #78 or #79 or #80 or #81 Publication Year from 1995 to 2018 |
| 83 | #20 and #82 |
Databases: Health Technology Assessment; and NHS Economic Evaluation Database
| # | Searches |
|---|---|
| 1 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees |
| 2 | ((ectopic or extra uterine or extra*uterine or tub* or ampullary or isthm* or fimbrial or cornual or interstitial or abdom* or ovar* or cervi*) near/3 (pregnan* or gestat*)):ti,ab |
| 3 | (pregnan* near/3 ((unknown or uncertain) near/1 (location* or site*))):ti,ab |
| 4 | PUL:ti,ab |
| 5 | #1 or #2 or #3 or #4 |
| 6 | MeSH descriptor: [DIAGNOSIS] this term only |
| 7 | MeSH descriptor: [DIAGNOSIS, COMPUTER-ASSISTED] explode all trees |
| 8 | MeSH descriptor: [DIAGNOSIS, DIFFERENTIAL] this term only |
| 9 | MeSH descriptor: [DIAGNOSTIC ERRORS] explode all trees |
| 10 | MeSH descriptor: [EARLY DIAGNOSIS] this term only |
| 11 | diagnos*:ti,ab |
| 12 | #6 or #7 or #8 or #9 or #10 or #11 |
| 13 | (ultraso* near/3 featur*):ti,ab |
| 14 | (empty near/3 uterus*):ti,ab |
| 15 | (no near/3 intrauterin* near/3 pregnanc*):ti,ab |
| 16 | (pseudo* near/3 sac*):ti,ab |
| 17 | (decidual near/3 cyst*):ti,ab |
| 18 | (cyst* near/3 inside near/3 uterus*):ti,ab |
| 19 | (fluid* near/3 inside near/3 uterus*):ti,ab |
| 20 | (heterotopic* near/3 pregnan*):ti,ab |
| 21 | ((coexist* or co-exist*) near/3 (intrauterin* or IUP) near/3 (ectopic* or EP)):ti,ab |
| 22 | “adnexal mass*”:ti,ab |
| 23 | “yolk sac*”:ti,ab |
| 24 | ((fetal or fetus) near/2 pole*):ti,ab |
| 25 | ((fetal or fetus) near/2 (heartbeat* or heartrate*)):ti,ab |
| 26 | ((fetal or fetus) near/2 heart near/2 (beat* or rate*)):ti,ab |
| 27 | (Tubal near/3 ring*):ti,ab |
| 28 | ((bagel* or donut* or doughnut* or blob*) near/3 sign*):ti,ab |
| 29 | “Adnexal cyst*”:ti,ab |
| 30 | (Identif* near/3 (fluid* or blood*)):ti,ab |
| 31 | (Free* near/3 fluid*):ti,ab |
| 32 | (Hemoperitoneum or Haemoperitoneum):ti,ab |
| 33 | (Free* near/3 blood* near/3 pelvi*):ti,ab |
| 34 | #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 |
| 35 | MeSH descriptor: [ULTRASONOGRAPHY] explode all trees |
| 36 | ultrasonograph*:ti,ab |
| 37 | sonograph*:ti,ab |
| 38 | ultrasound:ti,ab |
| 39 | ultrasonic*:ti,ab |
| 40 | sonogram*:ti,ab |
| 41 | Echocardiograph*:ti,ab |
| 42 | Echoencephalograph*:ti,ab |
| 43 | Echograph*:ti,ab |
| 44 | Echotomograph*:ti,ab |
| 45 | Endosonograph*:ti,ab |
| 46 | #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 |
| 47 | “Positive likelihood ratio*”:ti,ab |
| 48 | “Negative likelihood ratio*”:ti,ab |
| 49 | LR*:ti,ab |
| 50 | MeSH descriptor: [AREA UNDER CURVE] this term only |
| 51 | (“area* under” near/2 curve*):ti,ab |
| 52 | AUC*:ti,ab |
| 53 | MeSH descriptor: [SENSITIVITY AND SPECIFICITY] this term only |
| 54 | (sensitiv* near/10 specific*):ti,ab |
| 55 | #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 |
| 56 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnosis - DI] |
| 57 | MeSH descriptor: [PREGNANCY, ECTOPIC] explode all trees and with qualifier(s): [Diagnostic imaging - DG] |
| 58 | #5 and #12 and #34 |
| 59 | #5 and #12 and #46 and #55 |
| 60 | #34 and #56 |
| 61 | #34 and #57 |
| 62 | #58 or #59 or #60 or #61 Publication Year from 1995 to 2018 |
Appendix C. Clinical evidence study selection
Appendix D. Clinical evidence tables
Appendix E. Forest plots
There are no forest plots for this evidence review as no meta-analysis was performed.
Appendix F. GRADE tables
Table 5All symptomatic women (women with pain/bleeding or referred for a scan due to high risk of ectopic pregnancy)
| Number of studies (author) | Number of women | Risk of bias | Inconsistency | Indirectness | Imprecision | Sensitivity (95% CI) | Specificity (95% CI) | Effect size | Quality of the evidence (GRADE) |
|---|---|---|---|---|---|---|---|---|---|
| LR+ (95% CI) | |||||||||
| LR− (95% CI) | |||||||||
| TVUS: adnexal ectopic (Adnexal mass with gestational sac and yolk sac or fetal pole +/− fetal heartbeat) | |||||||||
| 1 (Barnhart 2011)1 | 1880 | Serious risk of bias2 | No serious inconsistency | Serious3 | No serious imprecision | 0.13 (0.10 to 0.17) | 1.00 (1.00 to 1.00) | 197.37 (27.35 to 1424.15) |
LOW ⊕⊕⊝⊝ |
| 0.87 (0.84 to 0.90) | |||||||||
| TVUS: Complex adnexal mass: inhomogenous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole) | |||||||||
| 1 (Barnhart 2011)1 | 1880 | Serious risk of bias2 | No serious inconsistency | Serious3 | No serious imprecision | 0.42 (0.37 to 0.48) | 0.98 (0.97 to 0.99) | 18.92 (12.89 to 27.78) |
LOW ⊕⊕⊝⊝ |
| 0.65 (0.60 to 0.70) | |||||||||
| TVUS: Free fluid in the pelvis | |||||||||
| 1 (Moore 2007)4 | 226 | No serious risk of bias | No serious inconsistency | No serious indirectness | Serious5 | 0.53 (0.36 to 0.69) | 0.74 (0.67 to 0.80) | 2.0 (1.4 to 3.0) |
MODERATE ⊕⊕⊕⊝ |
| 0.63 (0.42 to 0.93) | |||||||||
| 1 (Sadek 1995)6 | 525 | No serious risk of bias | No serious inconsistency | No serious indirectness | No serious imprecision | 0.96 (0.87 to 1.00) | 0.99 (0.98 to 1.00) | 151.40 (48.94 to 468.32) |
HIGH ⊕⊕⊕⊕ |
| 0.04 (0.01 to 0.15) | |||||||||
| TAS: Free fluid in the pelvis | |||||||||
| 1 (Moore 2007)4 | 241 | No serious risk of bias | No serious inconsistency | No serious indirectness | Serious7 | 0.39 (0.29 to 0.59) | 0.94 (0.90 to 0.97) | 7.0 (3.4 to 14) |
MODERATE ⊕⊕⊕⊝ |
| 0.65 (0.48 to 0.87) | |||||||||
CI: confidence interval; EP: ectopic pregnancy; IUP: intrauterine pregnancy; IVF: in vitro fertilisation; LR+: positive likelihood ratio; LR-: negative likelihood ratio; MID: minimally important difference; NGA: National Guideline Alliance; TAS: transabdominal ultrasound; TVUS: transvaginal ultrasound
- 1
Additional data calculated by the NGA technical team: LR using RevMan 5.3 calculator and vassarstats online calculator (http://vassarstats
.net/clin1.html) - 2
The quality of the evidence was downgraded by 1 level as there was an unclear risk of bias in the participant flow
- 3
The quality of the evidence was downgraded by 1 level as the study excluded simple viable IUPs (included abnormal, unclear, or IUP with need for further gynaecological consult), therefore a higher risk population
- 4
Additional data calculated by the NGA technical team: LR− using RevMan 5.3 calculator and vassarstats online calculator (http://vassarstats
.net/clin1.html) - 5
The quality of the evidence was downgraded by 1 level as the 95% CI for sensitivity crosses 0.50: protocol-specified MID thresholds for sensitivity are 0.50 and 0.75
- 6
Additional data calculated by the NGA technical team: 95% CI for sensitivity and specificity using RevMan5.3 calculator, and LR using vassarstats online calculator (http://vassarstats
.net/clin1.html) - 7
The quality of the evidence was downgraded by 1 level as the 95% CI for sensitivity crosses 0.50: protocol-specified MID thresholds for sensitivity are 0.50 and 0.75
Table 6High risk of ectopic pregnancy: includes PUL and ectopic pregnancy (all IUPs excluded)
| Number of studies (author) | Number of women | Risk of bias | Inconsistency | Indirectness | Imprecision | Sensitivity (95%CI) | Specificity (95%CI) | Effect size | Quality of the evidence (GRADE) |
|---|---|---|---|---|---|---|---|---|---|
| LR+ (95%CI) | |||||||||
| LR− (95%CI) | |||||||||
| TVUS: Pseudosac | |||||||||
| 1 (Hammoud 2005)1 | 403 | Serious risk of bias2 | No serious inconsistency | No serious indirectness | No serious imprecision | 0.03 (0.01 to 0.06) | 0.99 (0.95 to 1.00) | 2.27 (0.49 to 10.56) |
MODERATE ⊕⊕⊕⊝ |
| 0.98 (0.96 to 1.00) | |||||||||
| TVUS: Intrauterine fluid | |||||||||
| 1 (Mehta 1999)1 | 128 | Serious risk of bias3 | No serious inconsistency | No serious indirectness | Serious4 | 0.26 (0.14 to 0.42) | 0.52 (0.41 to 0.63) | 0.55 (0.32 to 0.96) |
LOW ⊕⊕⊝⊝ |
| 1.41 (1.15 to 1.72) | |||||||||
| TVUS: Complex adnexal mass: inhomogeneous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole) | |||||||||
| 1 (Mehta 1999)1,5 | 128 | Serious risk of bias3 | No serious inconsistency | No serious indirectness | Serious6 | 0.60 (0.43 to 0.74) | 0.99 (0.94 to 1.00) | 51.19 (7.18 to 365.03) |
LOW ⊕⊕⊝⊝ |
| 0.41 (0.28 to 0.60) | |||||||||
| TVUS: Free fluid in peritoneal cavity | |||||||||
| 1 (Mehta 1999)1 | 128 | Serious risk of bias3 | No serious inconsistency | No serious indirectness | Serious6 | 0.60 (0.43 to 0.74) | 1.00 (0.96 to 1.00) | Not calculable7 |
LOW ⊕⊕⊝⊝ |
| 0.40 (0.28 to 0.58) | |||||||||
CI: confidence interval; EP: ectopic pregnancy; IUP: intrauterine pregnancy; LR+: positive likelihood ratio; LR-: negative likelihood ratio; MID: minimally important difference; NGA: National Guideline Alliance; PUL: pregnancy of unknown location; TVUS: transvaginal ultrasound
- 1
Additional data calculated by the NGA technical team: sensitivity and specificity using RevMan 5.3 calculator, and LR using vassarstats online calculator (http://vassarstats
.net/clin1.html) - 2
The quality of the evidence was downgraded by 1 level due to an unclear risk of bias in participant flow, as 8.6% of women were excluded from the final analysis due to loss to follow up.
- 3
The quality of the evidence was downgraded by 1 level due to an unclear risk of bias in participant flow – there was an unclear interval between the index test and reference standard, patients received different reference standards and participants were excluded if there was insufficient clinical or sonographic follow up, or no serum hCG measurement within 24 hours of the scan.
- 4
The quality of the evidence was downgraded by 1 level as the 95% CI for specificity crosses 0.50: protocol-specified MID thresholds for specificity are 0.50 and 0.80
- 5
Study may have included adnexal masses with additional features (such as yolk sac and/or fetal pole) – described only as adnexal mass
- 6
The quality of the evidence was downgraded by 1 level as the 95% CI for sensitivity crosses 0.50: protocol-specified MID thresholds for sensitivity are 0.50 and 0.77
- 7
Positive likelihood ratio (LR+) not calculable as specificity is 1.00 (100%)
Table 7High risk of ectopic pregnancy: PULs only – excluded all IUPs and definite ectopic pregnancy
| Number of studies (author) | Number of women | Risk of bias | Inconsistency | Indirectness | Imprecision | Sensitivity (95%CI) | Specificity (95%CI) | Effect size | AUC (95% CI) | Quality of the evidence (GRADE) |
|---|---|---|---|---|---|---|---|---|---|---|
| LR+ (95%CI) | ||||||||||
| LR− (95%CI) | ||||||||||
| TVUS: Empty uterus | ||||||||||
| 1 (Dart 1998)1 | 228 | Serious risk of bias2 | No serious inconsistency | No serious indirectness | Serious3 | 0.78 (0.60 to 0.91) | 0.65 (0.58 to 0.71) | 2.22 (1.1–5.0) | - |
LOW ⊕⊕⊝⊝ |
| 0.34 (0.17 to 0.65) | ||||||||||
| 1 (Dart 2002)4 | 635 | Serious risk of bias5 | No serious inconsistency | No serious indirectness | Serious3 | 0.78 (0.64 to 0.89) | 0.62 (0.58 to 0.66) | 2.07 (1.72 to 2.48) | - |
LOW ⊕⊕⊝⊝ |
| 0.35 (0.20 to 0.61) | ||||||||||
| TVUS: Pseudosac | ||||||||||
| 1 (Ahmed 2004)4 | 77 | Serious risk of bias6 | No serious inconsistency | No serious indirectness | Serious7 | 0.06 (0.01 to 0.16) | 0.42 (0.22 to 0.63) | 0.10 (0.03 to 0.31) | - |
LOW ⊕⊕⊝⊝ |
| 2.26 (1.89 to 2.71) | ||||||||||
| TVUS: Intrauterine fluid | ||||||||||
| 1 (Dart 1998)1 | 228 | Serious risk of bias2 | No serious inconsistency | No serious indirectness | No serious imprecision | 0.13 (0.04 to 0.29) | 0.87 (0.81 to 0.91) | 1.0 (0.32 to 3.1) | - |
MODERATE ⊕⊕⊕⊝ |
| 1.01 (0.88 to 1.15) | ||||||||||
| 1 (Dart 2002)4 | 635 | Serious risk of bias5 | No serious inconsistency | No serious indirectness | Serious8 | 0.13 (0.05 to 0.26) | 0.80 (0.76 to 0.83) | 0.63 (0.29 to 1.36) | - |
LOW ⊕⊕⊝⊝ |
| 1.09 (0.98 to 1.23) | ||||||||||
| TVUS: Tubal ring sign (bagel sign) | ||||||||||
| 1 (Nadim 2018)9 | 612 | Serious10 | No serious inconsistency | No serious indirectness | Serious3 | 0.83 (0.70 to 0.91) | 1.00 (0.99 to 1.00) | 235.0 (58.6 to 942.8) | - |
LOW ⊕⊕⊝⊝ |
| 0.167 (0.089 to 0.315) | ||||||||||
| TVUS: Complex adnexal mass: inhomogeneous mass, heterogeneous mass, or adnexal mass (no yolk sac or fetal pole) | ||||||||||
| 1 (Ahmed 2004)4 | 77 | Serious risk of bias6 | No serious inconsistency | No serious indirectness | Very serious11 | 0.64 (0.50 to 0.77) | 0.88 (0.68 to 0.97) | 5.13 (1.75 to 15.07) | - |
VERY LOW ⊕⊝⊝⊝ |
| 0.41 (0.28 to 0.59) | ||||||||||
| 1 (Nadim 2018)9 | 663 | Serious10 | No serious inconsistency | No serious indirectness | No serious imprecision | 0.90 (0.82 to 0.94) | 1.00 (0.99 to 1.00) | 169.1 (54.6 to 523.8) | - |
MODERATE ⊕⊕⊕⊝ |
| 0.103 (0.057 to 0.185) | ||||||||||
| TVUS: Free fluid in peritoneal cavity | ||||||||||
| 1 (Malek-Mellouli 2013)12 | 94 | No serious risk of bias | No serious inconsistency | No serious indirectness | No serious imprecision | 0.26 (0.14 to 0.42) | 0.94 (0.84 to 0.99) | 4.5 (1.32 to 15.30) 13 | 0.60 |
HIGH ⊕⊕⊕⊕ |
| 0.79 (0.66 to 0.95)13 | ||||||||||
AUC: area under the curve; CI: confidence interval; EP: ectopic pregnancy; IUP: intrauterine pregnancy; LR+: positive likelihood ratio; LR-: negative likelihood ratio; MID: minimally important difference; NGA: National Guideline Alliance; PUL: pregnancy of unknown location; TVUS: transvaginal ultrasound
- 1
Additional data calculated by the NGA technical team: sensitivity and specificity using RevMan 5,3 calculator, and LR− using vassarstats online calculator (http://vassarstats
.net/clin1.html) - 2
The quality of the evidence was downgraded by 1 level due to high risk of bias in participant flow: 8% of women were excluded from the analysis as the reference standard was not available (lost to follow up before a final diagnosis was made)
- 3
The quality of the evidence was downgraded by 1 level as the 95% CI for sensitivity crosses 0.75: protocol-specified MID thresholds for sensitivity are 0.50 and 0.75
- 4
Additional data calculated by the NGA technical team: sensitivity and specificity using RevMan 5.3 calculator, and LR using vassarstats online calculator (http://vassarstats
.net/clin1.html) - 5
The quality of the evidence was downgraded by 1 level due to a high risk of bias in participant flow: 18% of participants were excluded from the final analysis as they were lost to follow up (reference standard was not available)
- 6
The quality of the evidence was downgraded by 1 level due to a high risk of bias in participant selection, as 13/90 women undergoing laparoscopy for suspected ectopic pregnancy were excluded
- 7
The quality of the evidence was downgraded by 1 level as the 95% CI for specificity crosses 0.50: protocol-specified MID thresholds for specificity are 0.50 and 0.80
- 8
The quality of the evidence was downgraded by 1 level as the 95% CI for specificity crosses 0.80: protocol-specified MID thresholds for specificity are 0.50 and 0.80
- 9
Study excluded definite EP and IUP, and non-tubal pregnancy (additional exclusion to other studies)
- 10
The quality of the evidence was downgraded by 1 level due to possible selection bias (women were excluded if they had conservative management instead of surgery and histological confirmation)
- 11
The quality of the evidence was downgraded by 2 levels as the 95% CI for sensitivity crosses 0.75 (protocol-specified MID thresholds for sensitivity are 0.50 and 0.75), and for specificity crosses 0.80 (protocol-specified MID thresholds for specificity are 0.50 and 0.80)
- 12
Additional data calculated by the NGA technical team: LR using vassarstats online calculator (http://vassarstats
.net/clin1.html) - 13
Values back-calculated by the NGA technical team using RevMan 5.3 calculator and vasserstats online calculator (http://vassarstats
.net/clin1.html) from reported sensitivity and specificity in the study. Unable to extract original data for 2×2 DTA table
Appendix G. Economic evidence study selection
Appendix H. Economic evidence tables
No economic evidence was identified for this review question.
Appendix I. Health economic evidence profiles
No economic evidence was identified for this review question.
Appendix J. Health economic analysis
No health economic analysis was conducted for this review question.
Appendix K. Excluded studies
Table 8Clinical studies
| Study | Reason for Exclusion |
|---|---|
| Abeia, A., Assefa, G., Diagnostic performance of transvesical ultrasound in clinically suspected ectopic pregnancy in a public and tertiary, hospital setup, Ethiopian Medical Journal, 51, 49–57, 2013 | Diagnostic accuracy using US for EP, but no diagnostic detail on characteristics - frequency reported of some |
| Abrahamson,L., Newton,W., What is the optimal protocol for diagnosis of ectopic pregnancy?, Journal of Family Practice, 50, 570-, 2001 | Short overview of a study - no usable data |
| Achanna,S., Har,W.Y., Predictive value of transabdominal ultrasonography in the diagnosis of ectopic pregnancy, Biomedical Research, 13, 85–3, 2002 | Diagnostic accuracy using US for EP, but no diagnostic detail on characteristics - frequency reported of each |
| Adhikari, Srikar, Blaivas, Michael, Lyon, Matthew, Diagnosis and management of ectopic pregnancy using bedside transvaginal ultrasonography in the ED: a 2-year experience, The American journal of emergency medicine, 25, 591–6, 2007 | Sonographer experience |
| Ali, J., Lotfi, G., Retrospective cross-sectional analysis of diagnosis criteria and management outcomes for patients diagnosed with caesarean scar pregnancy (CSP) at a single tertiary center, Gynecological Surgery, 13, S352, 2016 | Full text is an abstract |
| Al-Memar, M., Bobdiwala, S., Madhra, M., Cock, B. D., Calster, B. V., Bottomley, C., Horne, A., Bourne, T., The potential value of activin B and fibronectin as biomarkers to predict outcome in pregnancies of unknown location and first trimester viability, BJOG: An International Journal of Obstetrics and Gynaecology, 123, 241, 2016 | Full text is an abstract |
| Al-Memar, M., Bobdiwala, S., Madhra, M., Saso, S., De Cock, B., Van Calster, B., Brown, J. K., Mukri, F., Bottomley, C., Papageorghiou, A., Timmerman, D., Horne, A. W., Bourne, T., The potential value of activin B and fibronectin for the triage of pregnancies of unknown location and prediction of first trimester viability, Australasian Journal of Ultrasound in Medicine, 2018 | Not diagnostic for US - accuracy of biomarkers only |
| Ankum, W. M., Van der Veen, F., Hamerlynck, J. V., Lammes, F. B., Suspected ectopic pregnancy. What to do when human chorionic gonadotropin levels are below the discriminatory zone, Journal of Reproductive Medicine, 40, 525–8, 1995 | Diagnostic accuracy using US for EP, but no diagnostic detail on US features. Focus on a treatment pathway/ protocol/ algorithm |
| Asaravala, M., Wang, R., Hensley, B., Neilson, J., Jacoby, V., Stein, J., Does the finding of gestational sac on point of care ultrasound decrease the risk of ectopic pregnancy?, Academic Emergency Medicine, 20, S254, 2013 | Full text is an abstract |
| Atri, M., Leduc, C., Gillett, P., Bret, P. M., Reinhold, C., Kintzen, G., Aldis, A. E., Thibodeau, M., Role of endovaginal sonography in the diagnosis and management of ectopic pregnancy, Radiographics, 16, 755–74; discussion 775, 1996 | Narrative overview |
| Atri, Mostafa, Ectopic pregnancy versus corpus luteum cyst revisited: best Doppler predictors, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 22, 1181–4, 2003 | Not diagnostic accuracy |
| Atri, Mostafa, Valenti, David A., Bret, Patrice M., Gillett, Peter, Effect of transvaginal sonography on the use of invasive procedures for evaluating patients with a clinical diagnosis of ectopic pregnancy, Journal of clinical ultrasound : JCU, 31, 1–8, 2003 | Diagnostic accuracy using US for EP, but no diagnostic detail on characteristics - frequency reported of some. Focus on different eras of sonography |
| Banu, S. A., Khatun, S., Shamsuddin, L., Assesment of adnexal masses by transvaginal sonography and serum CA125 assay in pre- and postmenopausal women, Bangladesh Journal of Obstetrics and Gynecology, 24, 56–62, 2009 | Diagnostic accuracy of type of adnexal mass - not ectopic pregnancy |
| Barnhart, Kurt T., Casanova, Bruno, Sammel, Mary D., Timbers, Kelly, Chung, Karine, Kulp, J. L., Prediction of location of a symptomatic early gestation based solely on clinical presentation, Obstetrics and Gynecology, 112, 1319–26, 2008 | Diagnostic accuracy of different decision models (for management) |
| Barnhart,K.T., Simhan,H., Kamelle,S.A., Diagnostic accuracy of ultrasound above and below the beta-hCG discriminatory zone, Obstetrics and Gynecology, 94, 583–587, 1999 | Diagnostic accuracy using US HCG for EP, but no detail on US characteristics used in diagnosis |
| Basak, S., Van Roon, Y., Ghosh, B., Sriemevan, A., Diagnosis and management of pregnancy of unknown location (PUL): The completed audit cycle, BJOG: An International Journal of Obstetrics and Gynaecology, 120, 560–561, 2013 | Full text is an abstract |
| Bayyarapu, Vijaya B., Gundabattula, Sirisha R., Diagnosis and Management of ‘Cornual’ Pregnancies from 2002 to 2015 at a Tertiary Referral Centre in South India: Insights from Introspection, Journal of obstetrics and gynaecology of India, 67, 414–420, 2017 | Does not look at tubal EP |
| Benacerraf,B.R., Shipp,T.D., Bromley,B., Does the 10-MHz transvaginal transducer improve the diagnostic certainty that an intrauterine fluid collection is a true gestational sac?, Journal of Clinical Ultrasound, 27, 374–377, 1999 | Comparison in diagnostic accuracy of different US frequencies. Not characteristics of ectopic pregnancy |
| Benson, Carol B., Doubilet, Peter M., Peters, Hope E., Frates, Mary C., Intrauterine fluid with ectopic pregnancy: a reappraisal, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 32, 389–93, 2013 | No diagnostic outcomes available |
| Bignardi, Tommaso, Alhamdan, Dalya, Condous, George, Is ultrasound the new gold standard for the diagnosis of ectopic pregnancy?, Seminars in ultrasound, CT, and MR, 29, 114–20, 2008 | Narrative review |
| Birkhahn, Robert H., Gaeta, Theodore J., Van Deusen, Shawn K., Tloczkowski, John, The ability of traditional vital signs and shock index to identify ruptured ectopic pregnancy, American Journal of Obstetrics and Gynecology, 189, 1293–6, 2003 | Diagnostic accuracy of shock index and heart rate, not US |
| Bixby, Sarah, Tello, Richard, Kuligowska, Ewa, Presence of a yolk sac on transvaginal sonography is the most reliable predictor of single-dose methotrexate treatment failure in ectopic pregnancy, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 24, 591–8, 2005 | Accuracy of model for assessing whether a certain treatment would work in cases of ectopic pregnancy |
| Blaivas, Michael, Lyon, Matthew, Reliability of adnexal mass mobility in distinguishing possible ectopic pregnancy from corpus luteum cysts, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 24, 599–605, 2005 | Not reliant on US for diagnosis - based on adnexal mass mobility |
| Bottomley, C., Van Belle, V., Pexsters, A., Papageorghiou, A. T., Mukri, F., Kirk, E., Van Huffel, S., Timmerman, D., Bourne, T., A model and scoring system to predict outcome of intrauterine pregnancies of uncertain viability, Ultrasound in Obstetrics & Gynecology, 37, 588–95, 2011 | Diagnostic accuracy of a model determining viability of pregnancy |
| Cacciatore,B., Korhonen,J., Stenman,U.H., Ylostalo,P., Transvaginal sonography and serum hCG in monitoring of presumed ectopic pregnancies selected for expectant management, Ultrasound in Obstetrics and Gynecology, 5, 297–300, 1995 | Descriptive - incidence of certain ectopic characteristics in cohort, and diagnostic accuracy for HCG not US |
| Chama,C.M., Obed,J.Y., Ekanem,I.A., Transvaginal ultrasound scan versus laparoscopy in the diagnosis of suspected ectopic pregnancy, Journal of Obstetrics and Gynaecology, 21, 184–186, 2001 | Diagnostic accuracy using US for EP, but no diagnostic detail on US features - frequency reported of each |
| Chen, P. C., Sickler, G. K., Dubinsky, T. J., Maklad, N., Jacobi, R. L., Weaver, J. E., Sonographic detection of echogenic fluid and correlation with culdocentesis in the evaluation of ectopic pregnancy, AJR. American Journal of Roentgenology, 170, 1299–302, 1998 | Diagnostic accuracy of hemoperitoneum, not tubal EP |
| Chen, Z. Y., Liu, J. H., Liang, K., Liang, W. X., Ma, S. H., Zeng, G. J., Xiao, S. Y., He, J. G., The diagnostic value of a multivariate logistic regression analysis model with transvaginal power Doppler ultrasonography for the prediction of ectopic pregnancy, Journal of International Medical Research, 40, 184–93, 2012 | Diagnostic accuracy of prediction model based on endometrial thickness |
| Chew,S., Anandakumar,C., Vanaja,K., Wong,Y.C., Chia,D., Ratnam,S.S., The role of transvaginal ultrasonography and colour Doppler imaging in the detection of ectopic pregnancy, Journal of Obstetrics and Gynaecology Research, 22, 455–460, 1996 | Cannot extract data for US features of EP, only for overall US diagnosis of EP |
| Col-Madendag, Ilknur, Madendag, Yusuf, KanatPektas, Mine, Danisman, Nuri, Can sonographic endometrial pattern be an early indicator for tubal ectopic pregnancy and related tubal rupture?, Archives of Gynecology and Obstetrics, 281, 189–94, 2010 | Diagnostic accuracy of logistic model based on endometrial pattern |
| Comstock, Christine, Huston, Kathleen, Lee, Wesley, The ultrasonographic appearance of ovarian ectopic pregnancies, Obstetrics and Gynecology, 105, 42–5, 2005 | Not diagnostic accuracy - case review of 6 ovarian ectopic pregnancies |
| Condous, G., Kirk, E., Lu, C., Van Huffel, S., Gevaert, O., De Moor, B., De Smet, F., Timmerman, D., Bourne, T., Diagnostic accuracy of varying discriminatory zones for the prediction of ectopic pregnancy in women with a pregnancy of unknown location, Ultrasound in Obstetrics & Gynecology, 26, 770–5, 2005 | Diagnostic accuracy of serum HCG and progesterone |
| Condous, G., Van Calster, B., Kirk, E., Haider, Z., Timmerman, D., Van Huffel, S., Bourne, T., Prediction of ectopic pregnancy in women with a pregnancy of unknown location, Ultrasound in Obstetrics & Gynecology, 29, 680–7, 2007 | Accuracy of logistic models for prediction of EP based on HCG |
| Condous, George, Okaro, Emeka, Khalid, Asma, Lu, Chuan, Van Huffel, Sabine, Timmerman, D., Bourne, Tom, The accuracy of transvaginal ultrasonography for the diagnosis of ectopic pregnancy prior to surgery, Human reproduction (Oxford, England), 20, 1404–9, 2005 | Diagnostic accuracy using US for EP, but no diagnostic detail on US features - frequency reported of each |
| Crochet, J. R., Bastian, L. A., Chireau, M. V., Does this woman have an ectopic pregnancy? The rational clinical examination systematic review, JAMA - Journal of the American Medical Association, 309, 1722–1729, 2013 | SR with MA includes data that does not adhere to the protocol - pre-1995. Included studies checked for inclusion/exclusion |
| Dart,R., Kaplan,B., Ortiz,L., Cloherty,J., Lavoie,T., Normal intrauterine pregnancy is unlikely in emergency department patients with either menstrual days > 38 days or beta-hCG > 3,000 mIU/mL, but without a gestational sac on ultrasonography, Academic Emergency Medicine, 4, 967–971, 1997 | Not diagnostic accuracy |
| Dart,R.G., Dart,L., Mitchell,P., Berty,C., The predictive value of endometrial stripe thickness in patients with suspected ectopic pregnancy who have an empty uterus at ultrasonography, Academic Emergency Medicine, 6, 602–609, 1999 | Diagnostic accuracy based on endometrial stripe thickness and hCG |
| Dart,R.G., Mitterando,J., Dart,L.M., Rate of change of serial beta-human chorionic gonadotropin values as a predictor of ectopic pregnancy in patients with indeterminate transvaginal ultrasound findings, Annals of Emergency Medicine, 34, 703–710, 1999 | Not diagnostic accuracy |
| Devarajan, S. D., Balachandren, N. B., Ramalingam, K. R., Fleming, D. F., Shankar, M., Diagnosis of ectopic pregnancy: Is ultrasound a reliable tool?, BJOG: An International Journal of Obstetrics and Gynaecology, 120, 543, 2013 | Full text is an abstract |
| Dhiman, Pooja, Senthilkumar, G. P., Rajendiran, Soundravally, Sivaraman, K., Soundararaghavan, S., Kulandhasamy, Maheshwari, Serum activin B concentration as predictive biomarker for ectopic pregnancy, Clinical biochemistry, 49, 609–12, 2016 | Diagnostic of serum markers, not US |
| Dilbaz, S., Guvendag Guven, E. S., Yildirim, B., Gelisen, O., Karcaaltincaba, D., Kurtaran, V., Haberal, A., Is it necessary to operate on all women with an acute abdomen following medical treatment of tubal ectopic pregnancy?, Journal of Obstetrics and Gynaecology, 30, 496500, 2010 | Efficacy of treatment in ectopic cohorts. Not diagnostic accuracy of US |
| Dogra, Vikram, Paspulati, Raj Mohan, Bhatt, Shweta, First trimester bleeding evaluation, Ultrasound Quarterly, 21, 69–4, 2005 | Narrative review |
| Drobny,J., Sonography in the management of symptomatic pregnancies of unknown location, Bratislavske lekarske listy, 109, 254–259, 2008 | Cannot extract usable data. Diagnostic accuracy using US for ectopic pregnancy overall, and reports frequency of some US characteristics, but no diagnostic accuracy for those features |
| Durham,B., Lane,B., Burbridge,L., Balasubramaniam,S., Mateer,J., Pelvic ultrasound performed by emergency physicians for the detection of ectopic pregnancy in complicated first-trimester pregnancies, Annals of Emergency Medicine, 29, 338–347, 1997 | Cannot extract data for separate features seen by US as categorised by protocol (sums complex and simple adnexal mass) |
| Ellaithy, Mohamed, Abdelaziz, Ahmed, Hassan, Mahmoud Fathy, Outcome prediction in pregnancies of unknown location using endometrial thickness measurement: is this of real clinical value?, European journal of obstetrics, gynecology, and reproductive biology, 168, 68–74, 2013 | Diagnostic accuracy using endometrial thickness |
| Erol, Onur, Suren, Dinc, Karaca, Mehmet, Sezer, Cem, Ultrasonography for the prediction of extension of trophoblastic infiltration into the tubal wall in ampullary pregnancy, Ginekologia polska, 86, 16–20, 2015 | Diagnostic accuracy for assessing depth of infiltration into tubal wall |
| Farren, J., Kirk, E., Mitchell, H., Sayasneh, A., Condous, G., Stalder, C., Bourne, T., The characteristics of 671 cases of tubal ectopic pregnancy, BJOG: An International Journal of Obstetrics and Gynaecology, 120, 539, 2013 | Full text is an abstract |
| Fauconnier, Arnaud, Mabrouk, Ali, Salomon, Laurent J., Bernard, Jean-Pierre, Ville, Yves, Ultrasound assessment of haemoperitoneum in ectopic pregnancy: derivation of a prediction model, World journal of emergency surgery : WJES, 2, 23, 2007 | Diagnostic accuracy to predict haemoperitoneum, using confirmed ectopic pregnancy as cohort |
| Fistouris, J., Bergh, C., Strandell, A., Classification of pregnancies of unknown location according to four different hCG-based protocols, Human Reproduction, 31, 2203–11, 2016 | Diagnostic accuracy based on change in hCG level |
| Florio, Pasquale, Severi, Filiberto Maria, Bocchi, Caterina, Luisi, Stefano, Mazzini, Massimo, Danero, Secondo, Torricelli, Michela, Petraglia, Felice, Single serum activin a testing to predict ectopic pregnancy, The Journal of clinical endocrinology and metabolism, 92, 1748–53, 2007 | Diagnostic accuracy using serum biomarkers: hCG, progesterone, and activin A |
| Frates, M. C., Visweswaran, A., Laing, F. C., Comparison of tubal ring and corpus luteum echogenicities: a useful differentiating characteristic, Journal of Ultrasound in Medicine, 20, 27–31; quiz 33, 2001 | Not diagnostic accuracy - echogenicity of difference characteristics |
| Frates, Mary C., Doubilet, Peter M., Peters, Hope E., Benson, Carol B., Adnexal sonographic findings in ectopic pregnancy and their correlation with tubal rupture and human chorionic gonadotropin levels, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 33, 697–703, 2014 | Not diagnostic accuracy for ectopic pregnancy |
| Frates,M.C., Laing,F.C., Sonographic evaluation of ectopic pregnancy: An update, American Journal of Roentgenology, 165, 251–259, 1995 | Narrative review |
| Fukami, Tatsuya, Emoto, Makoto, Tamura, Riko, Kawarabayashi, Tatsuhiko, Sonographic findings of transvaginal color Doppler ultrasound in ectopic pregnancy, Journal of medical ultrasonics (2001), 33, 37–42, 2006 | Not diagnostic accuracy |
| Gracia,C.R., Barnhart,K.T., Diagnosing ectopic pregnancy: decision analysis comparing six strategies, Obstetrics and Gynecology, 97, 464470, 2001 | Assessment of decision algorithms - order of assessment/treatment |
| Guvendag Guven, E. S., Dilbaz, S., Dilbaz, B., Guven, S., Sahin Ozdemir, D., Haberal, A., Serum biochemistry correlates with the size of tubal ectopic pregnancy on sonography, Ultrasound in Obstetrics & Gynecology, 28, 826–30, 2006 | Not diagnostic accuracy - correlation between serum biomarkers and US |
| Hajenius, P. J., Mol, B. W., Ankum, W. M., van der Veen, F., Bossuyt, P. M., Lammes, F. B., Suspected ectopic pregnancy: expectant management in patients with negative sonographic findings and low serum hCG concentrations, Early Pregnancy, 1, 258–62, 1995 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of each |
| Harvey, S., Gillespie, M., McMurray, C., Robb, H., Mackay, V., A retrospective case note analysis of the diagnostic effectiveness of a single transvaginal scan in detecting ectopic pregnancy, BJOG: An International Journal of Obstetrics and Gynaecology, 123, 235, 2016 | Full text is an abstract |
| Hertzberg,B.S., Kliewer,M.A., Paulson,E.K., Ovarian cyst rupture causing hemoperitoneum: imaging features and the potential for misdiagnosis, Abdominal Imaging, 24, 304–308, 1999 | Data not available to calculate diagnostic accuracy |
| Hinney,B., Bertagnoli,C., Tobler-Sommer,M., Osmers,R., Wuttke,W., Kuhn,W., Diagnosis of early ectopic pregnancy by measurement of the maternal serum to cul-de-sac fluid beta-hCG ratio, Ultrasound in Obstetrics and Gynecology, 5, 260–266, 1995 | Diagnostic accuracy using ratio of maternal serum (hCG) to cul-de-sac fluid (taken via USguided puncture system) |
| Hoffmann, Beatrice, Nurnberg, Dieter, Westergaard, Mary C., Focus on abnormal air: diagnostic ultrasonography for the acute abdomen, European journal of emergency medicine : official journal of the European Society for Emergency Medicine, 19, 284–91, 2012 | Narrative review |
| Hourani, Roula, Hachem, Kamal, HaddadZebouni, Soha, Mansour, Fersan, Elhage, Abdo, Checrallah, Antoine, Ghossain, Michel A., The multiple ultrasound patterns of ectopic pregnancy, Le Journal medical libanais. The Lebanese medical journal, 56, 27–34, 2008 | Narrative overview |
| Hsu,C.Y., Jeng,C.J., Lin,S.Y., Wang,Y.L., Wu,J.J., Wang,K.G., Impact of ultrasonography on the management of tubal pregnancy: Current status, Journal of Medical Ultrasound, 4, 33–38, 1996 | Incidence of characteristics - no diagnostic accuracy data |
| Huang, K. S., Tsai, Y. S., Jan, Y. T., Yang, F. S., Retrospective image observation of ectopic pregnancy on computed tomography in the emergency condition: How useful is adnexal ring sign?, Chinese Journal of Radiology (Taiwan), 41, 7–12, 2016 | Use of CT not US |
| Hung,F.Y., Jeng,C.J., Hsieh,F.J., Yang,Y.C., Su,T.H., Wang,K.G., Transvaginal sonographic features of cervical pregnancy, Journal of Medical Ultrasound, 5, 95–100, 1997 | Not diagnostic accuracy for ectopic pregnancy. Cohort diagnosed and treated for cervical ectopic pregnancy (not tubal ectopic pregnancy) using US |
| Ignacio, Elizabeth A., Hill, Michael C., Ultrasound of the acute female pelvis, Ultrasound Quarterly, 19, 86–10, 2003 | Narrative review |
| Jakiel,G., Wieczorek,P., Bokiniec,M., Bakalczuk,S., Ectopic pregnancy diagnosis in very high risk patients, Ginekologia Polska, 69, 575–579, 1998 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of some |
| Jilian, S., Jiale, Q., Junmei, W., Jiamin, L., Haili, L., Application value of transvaginal ultrasound combined with abdominal ultrasonography in the diagnosis of ectopic pregnancy, Biomedical Research (India), 28, 9358–9361, 2017 | Cohort already had confirmed ectopic pregnancy. Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on US features - frequency reported of each |
| Kahyaoglu, Serkan, Turgay, Inci, Gocmen, Muhammed, Sut, Necdet, Batioglu, Sertac, A new predictive scoring system including shock index for unruptured tubal pregnancy patients, European journal of obstetrics, gynecology, and reproductive biology, 126, 99–103, 2006 | Predicting whether a treatment would work. Diagnostic accuracy using Shock Index (ratio of HR to SBP) instead of US |
| Kaplan, B. C., Dart, R. G., Moskos, M., Kuligowska, E., Chun, B., Hamid, M. A., Northern, K., Schmidt, J., Kharwadkar, A., Ectopic pregnancy: Prospective study with improved diagnostic accuracy, Annals of Emergency Medicine, 28, 10–17, 1996 | Diagnostic accuracy using US for ectopic pregnancy, but no usable diagnostic detail on US features (data cannot be separated for individual features as per protocol) |
| Karakus, S., Yildiz, C., Akkar, O., Sancakdar, E., Ulger, D., Cetin, A., The significance of the neutrophil-to-lymphocyte ratio in differantial diagnosis of ectopic pregnancy and miscarriage, International Journal of Clinical and Experimental Medicine, 9, 11327–11333, 2016 | Diagnostic accuracy based on biomarkers and biochemistry only |
| Kemp, B., Funk, A., Rath, W., Doppler sonographic criteria for viability in ectopic pregnancy in correlation with histology, International Journal of Gynaecology & Obstetrics, 54, 179–81, 1996 | Brief/short communication |
| Kirk, E., Bottomley, C., Bourne, T., Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location, Human Reproduction Update, 20, 250–61, 2014 | Narrative overview |
| Kirk, Emma, Bourne, Tom, Diagnosis of ectopic pregnancy with ultrasound, Best practice & research. Clinical obstetrics & gynaecology, 23, 501–8, 2009 | Narrative overview |
| Kirk, Emma, Daemen, Anneleen, Papageorghiou, Aris T., Bottomley, Cecilia, Condous, George, De Moor, Bart, Timmerman, Dirk, Bourne, Tom, Why are some ectopic pregnancies characterized as pregnancies of unknown location at the initial transvaginal ultrasound examination?, Acta Obstetricia et Gynecologica Scandinavica, 87, 1150–4, 2008 | Not diagnostic accuracy - comparison of characteristics of women with PUL or ectopic pregnancy |
| Kirk, Emma, Papageorghiou, Aris T., Condous, George, Tan, Linda, Bora, Shabana, Bourne, Tom, The diagnostic effectiveness of an initial transvaginal scan in detecting ectopic pregnancy, Human reproduction (Oxford, England), 22, 2824–8, 2007 | Overall ectopic pregnancy data show discrepancies between text and table - cannot extract accurate data. Cannot separate tubal and non-tubal ectopic pregnancies |
| Laing, F. C., Brown, D. L., Price, J. F., Teeger, S., Wong, M. L., Intradecidual sign: is it effective in diagnosis of an early intrauterine pregnancy?, Radiology, 204, 655–60, 1997 | Focus on sensitivity and specificity of different classes of sonographer: fellow, resident, student, attending sonographer |
| Lavie,O., Boldes,R., Neuman,M., Rabinovitz,R., Algur,N., Beller,U., Ultrasonographic “endometrial three-layer” pattern: a unique finding in ectopic pregnancy, Journal of Clinical Ultrasound, 24, 179–183, 1996 | Diagnostic accuracy using endometrial threelayer pattern |
| Leiserowitz, Gary S., Xing, Guibo, Cress, Rosemary, Brahmbhatt, Bhoomi, Dalrymple, John L., Smith, Lloyd H., Adnexal masses in pregnancy: how often are they malignant?, Gynecologic oncology, 101, 315–21, 2006 | Incidence of malignant masses during pregnancy - not diagnostic for ectopic pregnancy |
| Li, X. H., Ouyang, Y., Lu, G. X., Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilization with embryo transfer, Ultrasound in Obstetrics & Gynecology, 41, 563–9, 2013 | Diagnostic accuracy using US for heterotopic pregnancy (incorrect reference standard) |
| Lin, Edward P., Bhatt, Shweta, Dogra, Vikram S., Diagnostic clues to ectopic pregnancy, Radiographics : a review publication of the Radiological Society of North America, Inc, 28, 1661–71, 2008 | Not diagnostic accuracy - narrative overview and teaching points |
| Lipscomb, Gary H., Gomez, Isabel G., Givens, Vanessa M., Meyer, Norman L., Bran, Derita F., Yolk sac on transvaginal ultrasound as a prognostic indicator in the treatment of ectopic pregnancy with single-dose methotrexate, American Journal of Obstetrics and Gynecology, 200, 338.e1–4, 2009 | Risk factors for treatment success/failure - not diagnostic accuracy |
| Loubeyre, Pierre, Patel, Seema, Copercini, Michele, Petignat, Patrick, Dallenbach, Patrick, Dubuisson, Jean Bernard, Role of sonography in the diagnostic workup of ovarian and adnexal masses except in pregnancy and during ovarian stimulation, Journal of clinical ultrasound : JCU, 40, 424–32, 2012 | Diagnostic overview for ovarian and adnexal masses not in pregnancy |
| Louis-Sylvestre,C., Morice,P., Chapron,C., Dubuisson,J.B., The role of laparoscopy in the diagnosis and management of heterotopic pregnancies, Human Reproduction, 12, 1100–1102, 1997 | Heterotopic pregnancy case reports (not diagnostic accuracy) |
| Majeed, H., Bor, P., The diagnostic value of the presence of pelvic fluid in the cul-de-sac in women with pregnancy of unknown location, Acta Obstetricia et Gynecologica Scandinavica, 91, 110, 2012 | Full text is an abstract |
| Malik, S. A., Malik, S., Maqbool, A., Comparison of transabdominal and transvaginal sonography in the diagnosis of ectopic pregnancy, Pakistan Journal of Medical and Health Sciences, 4, 2227, 2010 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of some |
| Mateer,J.R., Valley,V.T., Aiman,E.J., Phelan,M.B., Thoma,M.E., Kefer,M.P., Outcome analysis of a protocol including bedside endovaginal sonography in patients at risk for ectopic pregnancy, Annals of Emergency Medicine, 27, 283–289, 1996 | Not diagnostic accuracy for ectopic pregnancy - incidence of ruptured ectopic pregnancy when using bedside US in ED |
| Mathlouthi, N., Slimani, O., Fatnassi, A., Ben Temime, R., Makhlouf, T., Attia, L., Chachia, A., Ultrasound diagnosis of ectopic pregnancy: Prospective study about 200 cases, Tunisie Medicale, 91, 254–257, 2013 | Full text in French |
| McCord,M.L., Muram,D., Buster,J.E., Arheart,K.L., Stovall,T.G., Carson,S.A., Single serum progesterone as a screen for ectopic pregnancy: Exchanging specificity and sensitivity to obtain optimal test performance, Fertility and Sterility, 66, 513–516, 1996 | Diagnostic accuracy of serum progesterone |
| McRae,A., Edmonds,M., Murray,H., Diagnostic accuracy and clinical utility of emergency department targeted ultrasonography in the evaluation of first-trimester pelvic pain and bleeding: A systematic review, Canadian Journal of Emergency Medicine, 11, 355–364, 2009 | SR with no MA (narrative review). Diagnostic accuracy for IUP, not ectopic pregnancy. Included studies checked for relevance |
| Miller, V. I., Coughlin, B. F., Pregnancy and abdominal pain: Value of ultrasound in diagnosis, Emergency Radiology, 3, 118–125, 1996 | Ectopic pregnancy not listed as gynaecological pathology with diagnostic data |
| Mol, B. W., Hajenius, P. J., Ankum, W. M., Bossuyt, P. M., van der Veen, F., Screening for ectopic pregnancy in symptom-free women at increased risk, Obstetrics & Gynecology, 89, 704–7, 1997 | Distribution of ectopic pregnancy per risk factor (not characteristic seen on US) |
| Mol, B. W., Hajenius, P. J., Engelsbel, S., Ankum, W. M., van der Veen, F., Hemrika, D. J., Bossuyt, P. M., Are gestational age and endometrial thickness alternatives for serum human chorionic gonadotropin as criteria for the diagnosis of ectopic pregnancy?, Fertility & Sterility, 72, 643–5, 1999 | Diagnostic accuracy of gestational age and endometrial stripe thickness compared to serum hCG |
| Moon, Min Hoan, Lee, Young Ho, Lim, Kyung Taek, Yang, Jae Hyug, Park, Seong Ho, Outcome prediction for treatment of tubal pregnancy using an intramuscular methotrexate protocol, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 27, 1461–7, 2008 | Not diagnostic accuracy - presence of different characteristics to predict whether a certain treatment would be successful |
| Nahar, M. N., Quddus, M. A., Sattar, A., Shirin, M., Khatun, A., Ahmed, R., Sultana, F., Comparison of transvaginal and transabdominal ultrasonography in the diagnosis of ectopic pregnancy, Bangladesh Medical Research Council Bulletin, 39, 104–8, 2013 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on US features - only overall accuracy presented for US ability to identify ectopic pregnancy |
| Naseem, Iram, Bari, Vaqar, Nadeem, Naila, Multiple parameters in the diagnosis of ectopic pregnancy, JPMA. The Journal of the Pakistan Medical Association, 55, 74–6, 2005 | Diagnostic accuracy using US for ectopic pregnancy (TAS followed by TVS), but no diagnostic detail on US features - frequency reported for some. Unable to extract relevant data for diagnostic on US features |
| Panelli, Danielle M., Phillips, Catherine H., Brady, Paula C., Incidence, diagnosis and management of tubal and nontubal ectopic pregnancies: a review, Fertility research and practice, 1, 15, 2015 | Narrative overview |
| Pereira,P.P., Cabar,F.R., Schultz,R., Zugaib,M., Association between ultrasound findings and extent of trophoblastic invasion into the tubal wall in ampullary pregnancy, Ultrasound in Obstetrics and Gynecology, 33, 472–476, 2009 | Cohort already diagnosed with ectopic pregnancy (not diagnostic accuracy). Study examines depth of trophoblastic infiltration into wall |
| Perriera, Lisa, Reeves, Matthew F., Ultrasound criteria for diagnosis of early pregnancy failure and ectopic pregnancy, Seminars in reproductive medicine, 26, 373–82, 2008 | Narrative overview |
| Platek,D.N., Henderson,C.E., Goldberg,G.L., The management of a persistent adnexal mass in pregnancy, American Journal of Obstetrics and Gynecology, 173, 1236–1240, 1995 | Not ectopic pregnancy - relates to treatment pathway for adnexal mass during pregnancy |
| Polena, V., Huchon, C., Ramos, C. V., Rouzier, R., Dumont, A., Fauconnier, A., Non-invasive tools for the diagnosis of potentially lifethreatening gynaecological emergencies: A Systematic Review, PLoS ONE, 10, e0114189, 2015 | Diagnostic accuracy using Tranabdominal US for: haemoperitoneum; TVS for: Pelvic inflammatory disease, haemoperitoneum, complicated ectopic (one paper - Sadek 1995 using echogenic fluid - included elsewhere) |
| Popowski, Thomas, Huchon, Cyrille, ToretLabeeuw, Flavy, Chantry, Anne A., Aegerter, Philippe, Fauconnier, Arnaud, Hemoperitoneum assessment in ectopic pregnancy, International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 116, 97–100, 2012 | Cohort of ectopic pregnancies without haemodynamic shock only (confirmed surgically). Characteristics used to predict volume of haemoperitoneum before surgery |
| Ramanan,R.V., Gajaraj,J., Ectopic pregnancy-the leash sign. A new sign on transvaginal Doppler ultrasound, Acta Radiologica, 47, 529535, 2006 | Feature described not in the protocol |
| Rempen,A., The shape of the endometrium evaluated with three-dimensional ultrasound: an additional predictor of extrauterine pregnancy, Human Reproduction, 13, 450–454, 1998 | US Diagnosis of IUP/ ectopic pregnancy /SA using shape of the endometrium, endometrial thickness, endometrial echoes |
| Richardson, A., Gallos, I., Dobson, S., Campbell, B. K., Coomarasamy, A., RaineFenning, N., Accuracy of first-trimester ultrasound in diagnosis of tubal ectopic pregnancy in the absence of an obvious extrauterine embryo: systematic review and meta-analysis, Ultrasound in Obstetrics & Gynecology, 47, 28–37, 2016 | SR includes multiple pre-1995 (does not adhere to protocol). Unable to use MA/pooled/summary statistics. Included studies (1995 onwards) checked for relevance |
| Richardson, A., Gallos, I., Dobson, S., Campbell, B. K., Coomarasamy, A., RaineFenning, N., Accuracy of first-trimester ultrasound in diagnosis of intrauterine pregnancy prior to visualization of the yolk sac: a systematic review and meta-analysis, Ultrasound in Obstetrics & Gynecology, 46, 142–9, 2015 | Diagnostic accuracy of IUP (not ectopic pregnancy) |
| Richardson, A., Hopkisson, J., Campbell, B., Raine-Fenning, N., Use of double decidual sac sign to confirm intrauterine pregnancy location prior to sonographic visualization of embryonic contents, Ultrasound in Obstetrics & Gynecology, 49, 643–648, 2017 | Diagnostic accuracy for IUP (not ectopic pregnancy) |
| Rogers, R. G., Kammerer-Doak, D., Miller, M., Byrn, F., Conway, S., Hall, R., A comparison of ultrasound and surgical findings in suspected ectopic pregnancy, Journal of Diagnostic Medical Sonography, 16, 60–64, 2000 | Cohort already had surgically confirmed and treated ectopic pregnancy (retrospective analysis of US features). Reporting on location of adnexal mass during surgery |
| Roghaei, Ma, Sabet, F, Mohamadi, K, Diagnostic accuracy of serum activin A in detection of ectopic pregnancy, Journal of research in medical sciences, 17, 378–381, 2012 | Diagnostic accuracy of serum Activin A for ectopic pregnancy |
| Scaldarella, L. O., Carbone, L., Mazzarella, A., Ricciardi, D., Chiacchio, G., Valentino, A., Mancino, D., Ciccarelli, G. T., Tolino, A., Retrospective study on 43 patients with diagnosis of ectopic pregnancy, Giornale Italiano di Ostetricia e Ginecologia, 35, 419–426, 2013 | Initial cohort already had ectopic pregnancy diagnosis. Study about identifying best treatment pathway for ectopic pregnancy |
| Segal,S., Mercado,R., Rivnay,B., Ectopic pregnancy early diagnosis markers, Minerva Ginecologica, 62, 49–62, 2010 | Narrative overview |
| Seo, Mi Rang, Choi, Joong Sub, Bae, Jaeman, Lee, Won Moo, Eom, Jeong Min, Lee, Eunhyun, Keum, Jihyun, Preoperative diagnostic clues to ovarian pregnancy: retrospective chart review of women with ovarian and tubal pregnancy, Obstetrics & gynecology science, 60, 462–468, 2017 | Not diagnostic accuracy. Study examines characteristics in Ovarian pregnancy and Tubal pregnancy. |
| Shah, Anish A., Grotegut, Chad A., Likes, Creighton E., 3rd, Miller, Michael J., Walmer, David K., Heterotopic cervical pregnancy treated with transvaginal ultrasound-guided aspiration resulting in cervical site varices within the myometrium, Fertility and Sterility, 91, 934.e1922, 2009 | Case report of heterotopic cervical pregnancy |
| Shalev,E., Yarom,I., Bustan,M., Weiner,E., BenShlomo,I., Transvaginal sonography as the ultimate diagnostic tool for the management of ectopic pregnancy: experience with 840 cases, Fertility and Sterility, 69, 62–65, 1998 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of some |
| Shetty, Vishma H., Gowda, Some, Muralidhar, Lakshmidevi, Role of ultrasonography in diagnosis of ectopic pregnancy with clinical analysis and management in tertiary care hospital, Journal of obstetrics and gynaecology of India, 64, 354–7, 2014 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of some |
| Stein, J. C., Wang, R., Adler, N., Goldstein, R., McAlpine, I., Won, G., Jacoby, V., Kohn, M., Evaluation of ectopic pregnancy with bedside ultrasound by emergency physicians: A metaanalysis, Annals of Emergency Medicine, 54, S69, 2009 | Full text is an abstract |
| Stein, John C., Wang, Ralph, Adler, Naomi, Boscardin, John, Jacoby, Vanessa L., Won, Gloria, Goldstein, Ruth, Kohn, Michael A., Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis, Annals of Emergency Medicine, 56, 674–83, 2010 | SR with MA includes pre-1995 studies, cannot use pooled result. Only uses overall ectopic pregnancy diagnostic accuracy/summary statistic, not accuracy of individual features. Included studies checked for relevance |
| Stein, Marjorie W., Ricci, Zina J., Novak, Leon, Roberts, Jeffrey H., Koenigsberg, Mordecai, Sonographic comparison of the tubal ring of ectopic pregnancy with the corpus luteum, Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 23, 57–62, 2004 | Not diagnostic accuracy. Comparison of characteristics in ectopic pregnancy and corpus luteum (echogenicity, presence of free fluid, endometrial wall thickness) |
| Teixeira, Joao L. G., Rabaioli, Paola, Savaris, Ricardo F., Sensitivity and specificity of a urinary screening test used in an emergency setting to detect abnormal first trimester pregnancies, American Journal of Obstetrics and Gynecology, 212, 58.e1–5, 2015 | US used as reference standard to assess diagnostic accuracy of urinary screening test in ED |
| Timor-Tritsch, Ilan E., Monteagudo, Ana, Cali, Giuseppe, El Refaey, Hazem, Kaelin Agten, Andrea, Arslan, Alan A., Easy sonographic differential diagnosis between intrauterine pregnancy and cesarean delivery scar pregnancy in the early first trimester, American Journal of Obstetrics and Gynecology, 215, 225.e1–7, 2016 | US to differentiate between Caesarean scar pregnancy and IUP |
| Tong, Stephen, Skubisz, Monika M., Horne, Andrew W., Molecular diagnostics and therapeutics for ectopic pregnancy, Molecular Human Reproduction, 21, 126–35, 2015 | Narrative overview of biomarkers for diagnosis of ectopic pregnancy |
| Turan, C., Ugur, M., Dogan, M., Ekici, E., Vicdan, K., Gokmen, O., Transvaginal sonographic findings of chronic ectopic pregnancy, European Journal of Obstetrics, Gynecology, & Reproductive Biology, 67, 115–9, 1996 | Cohort confirmed as having chronic ectopic pregnancy. Description of characteristics related to chronic ectopic pregnancy |
| Turkmen, G. G., Karcaaltincaba, D., Isik, H., Fidanci, V., Kaayalp, D., Timur, H., Batioglu, S., Does adenosine deaminase activity play a role in the early diagnosis of ectopic pregnancy?, Journal of Obstetrics & Gynaecology, 36, 347–50, 2016 | Diagnostic accuracy of enzyme adenosine deaminase for ectopic pregnancy |
| Van Mello, N. M., Mol, F., Ankum, W. M., Van Der Veen, F., Barnhart, K., Mol, B. W., Hajenius, P. J., Predictive value of serum hCG on the outcome of pregnancy of unknown location: A systematic review and meta-analysis, Journal of Reproductive Immunology, 90, 181, 2011 | Full text is an abstract |
| Verhaegen, J., Gallos, I. D., Van Mello, N. M., Abdel-Aziz, M., Takwoingi, Y., Harb, H., Deeks, J. J., Mol, B. W. J., Coomarasamy, A., Accuracy of a single progesterone test to predict early pregnancy outcome in women with pain or bleeding: A meta-analysis of cohort studies, BJOG: An International Journal of Obstetrics and Gynaecology, 1), 550–551, 2013 | Full text is an abstract |
| Wachsberg, R. H., Karimi, S., Sonographic endometrial three-layer pattern in symptomatic first-trimester pregnancy: not diagnostic of ectopic pregnancy, Journal of Clinical Ultrasound, 26, 199–201, 1998 | Diagnostic accuracy of endometrial three layer pattern for ectopic pregnancy |
| Wachsberg,R.H., Karimi,S., Chorionic rim sign on transvaginal sonography: Unrealiable of intrauterine pregnancy, Journal of Women’s Imaging, 3, 60–62, 2001 | Not diagnostic accuracy. Retrospective (unblinded) review of confirmed ectopic pregnancy cohort only |
| Wherry,K.L., Dubinsky,T.J., Waitches,G.M., Richardson,M.L., Reed,S., Low-resistance endometrial arterial flow in the exclusion of ectopic pregnancy revisited, Journal of Ultrasound in Medicine, 20, 335–342, 2001 | Diagnostic accuracy using endometrial blood flow |
| Willrich, M. A. V., Baumann, N. A., Tolan, N. V., Klee, G. G., Brown, D., Coddington, C. C., Evaluation of a discriminatory zone for serum Beta-human chorionic gonadotropin (betahCG) in early pregnancy, Clinical Chemistry, 60, S208-S209, 2014 | Full text is an abstract |
| Wong,T.W., Lau,C.C., Yeung,A., Lo,L., Tai,C.M., Efficacy of transabdominal ultrasound examination in the diagnosis of early pregnancy complications in an emergency department, Journal of Accident and Emergency Medicine, 15, 155–158, 1998 | Cannot extract diagnostic accuracy data for specific features seen on US - combination of features |
| Yadav, Poonam, Singla, Anshuja, Sidana, Anu, Suneja, Amita, Vaid, Neelam B., Evaluation of sonographic endometrial patterns and endometrial thickness as predictors of ectopic pregnancy, International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 136, 70–75, 2017 | Diagnostic accuracy using endometrial pattern. n=2/100 for pseudogestational sac. |
| Yakasai, I. A., Bappa, L. A., Diagnosis and management of adnexal masses in pregnancy, Journal of Surgical Technique and Case Report, 4, 79–85, 2012 | Management techniques after diagnosis of an adnexal mass. Narrative overview |
| Young, Lee, Barnard, Cecilia, Lewis, Elisabeth, Jones, Matthew, Furlan, Jana, Karatasiou, Angela, Necas, Martin, The diagnostic performance of ultrasound in the detection of ectopic pregnancy, The New Zealand medical journal, 130, 17–22, 2017 | Diagnostic accuracy using US for ectopic pregnancy, but no mention of characteristics seen on US |
| Yuri, M., Buzzi, J., Young, E., Diradourian, M., Isa, L., Garcia, B., Kenny, A., Our experience in ovarian ectopic pregnancy: Ultrasound, clinical and therapeutical correlation, Human Reproduction, 30, 2015 | Full text is an abstract |
| Yuri, M., Marconi, G., Diradourian, M., Vilela, M., Kenny, A., Young, E., Buzzi, J., Early diagnosis in ovarian pregnancy. Ultrasound, clinical and therapeutical correlation, International Journal of Gynecology and Obstetrics, 119, S524, 2012 | Full text is an abstract |
| Zaki,Z.M.S., Bahar,A.M., Ectopic pregnancy. Diagnosis using transabdominal ultrasound and a qualitative serum hCG test. Five years’ experience in the Middle East, Journal of Obstetrics and Gynaecology, 15, 157–160, 1995 | Diagnostic accuracy using US for ectopic pregnancy, but no diagnostic detail on characteristics - frequency reported of some |
Economic studies
No economic evidence was identified for this review question.
Appendix L. Research recommendations
No research recommendations were made for this review question.
Tables
Table 1Summary of the protocol (PIRO table)
| Population |
Pregnant women presenting in early pregnancy (<13+0 weeks) with pain or vaginal bleeding Asymptomatic pregnant women with indeterminate features on ultrasound, or pregnancy of unknown location |
|---|---|
| Index tests |
Ultrasonography with the following features: Uterus:
|
| Reference tests |
|
| Outcome |
|
AUC: area under the curve; ERPC: evacuation of retained products of conception; hCG: human chorionic gonadotrophin; IVF: in vitro fertilisation; LR: likelihood ratio; PUL: pregnancy of unknown location
Table 2Summary of included studies
| Study | Population | Index test | Reference test | Outcomes |
|---|---|---|---|---|
|
Retrospective cohort UK | N=77
| TVUS | Histopathological examination was performed to confirm the diagnosis of ectopic pregnancy |
|
|
Retrospective cohort USA | N=1880
| TVUS | Followed by the gynaecology service until a definitive diagnosis was made |
|
|
Retrospective cohort USA | N=228
| TVUS | Visualised at laparoscopy or laparotomy and confirmed by histopathology |
|
|
Prospective cohort USA | N=635
| TVUS |
(1) Extrauterine pregnancy visualised at laparoscopy; (2) Confirmed in patients managed with methotrexate (ectopic pregnancy confirmed with US follow-up; or hCG values that increased or plateaued after curettage) |
|
|
Retrospective cohort USA | N=403
| TAS and TVUS |
(1) When surgical: pathological diagnosis; (2) When medical: clinical follow up, and established sonographic criteria |
|
|
Prospective cohort Tunisia | N=94
| TVUS | Visualised at laparoscopy or laparotomy and confirmed by histopathology |
|
|
Retrospective cohort USA | N=128
| TVUS | Medical records, clinical and sonographic follow up |
|
|
Prospective cohort USA | N=226
| TAS and TVUS | Medical and operative records, clinical and sonographic follow up |
|
|
Retrospective cohort Australia | N=849
| TVUS |
(1) Visualised at laparoscopy or laparotomy and confirmed by histopathology of removed fallopian tube; (2) PULs: repeat TVUS and clinical follow up (hCG analysis) until diagnosis |
|
|
Prospective cohort Norway | N=525
| TVUS | Visualised at laparoscopy or laparotomy and confirmed by histopathology |
|
AUC: area under the curve; DTA: diagnostic test accuracy; ED: emergency department; IUP: intrauterine pregnancy; LR: likelihood ratio; N: number of women; PUL: pregnancy of unknown location; TAS: transabdominal sonography; TVUS: transvaginal ultrasonography; US: ultrasound
FINAL
Evidence reviews
developed by the National Guideline Alliance, hosted by the Royal College of Obstetricians and Gynaecologists
Disclaimer: The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. All NICE guidance is subject to regular review and may be updated or withdrawn.