Evidence review for patient information
Evidence review K
NICE Guideline, No. 132
Authors
National Guideline Centre (UK).1. Patient information
1.1. Review question: What information is useful for people with primary hyperparathyroidism?
1.2. Introduction
The NICE guideline on patient experience in adult NHS services (CG138) outlines the key principles of general care. It is also important to identify and address the unique needs of people who are being considered for a diagnosis of primary hyperparathyroidism (PHPT), and those who have a diagnosis of PHPT and are receiving care and monitoring. Information and support is required to enable people to understand their condition and make the best choices for their care. A qualitative review is being undertaken to try to find out what specific information people with PHPT should be given.
1.3. Characteristics table
For full details see the review protocol in appendix A.
Table 1
Characteristics of review question.
1.4. Qualitative evidence
1.4.1. Included studies
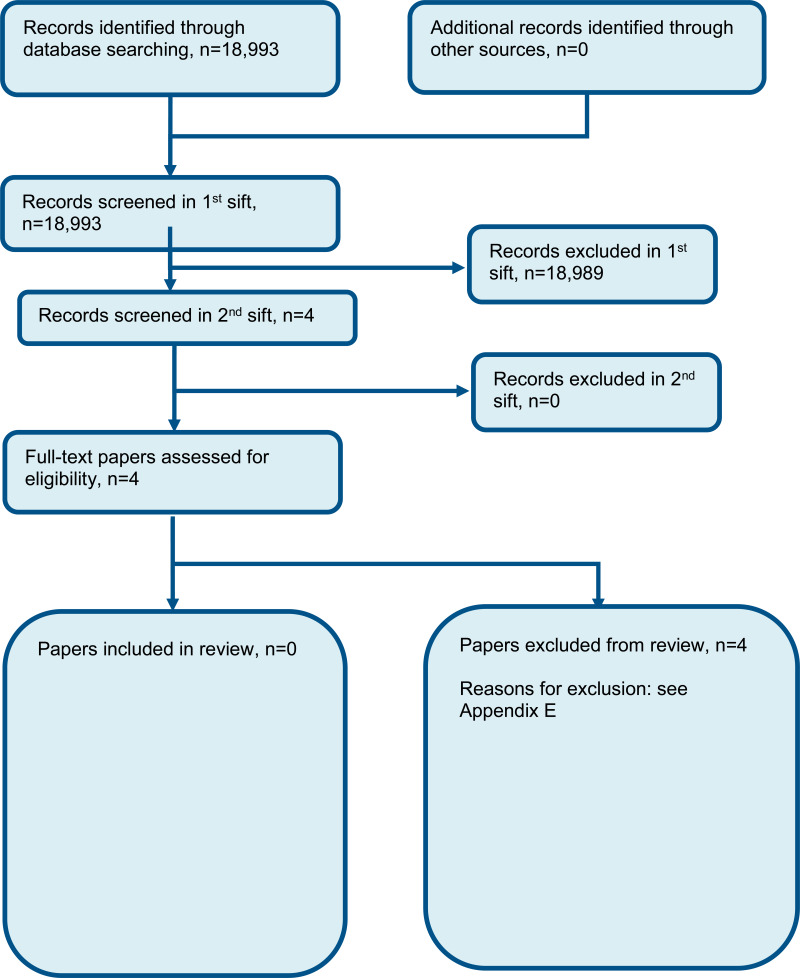
A search was conducted for identifying what information is useful for people with primary hyperparathyroidism. No relevant qualitative studies exploring this topic were identified. See the study selection flow chart in appendix C.
1.4.2. Excluded studies
See the excluded studies list in appendix E.
1.4.3. Summary of qualitative studies included in the evidence review
No qualitative evidence was identified for this review question.
1.4.4. Qualitative evidence synthesis
No qualitative evidence was identified for this review question.
1.4.4.1. Narrative summary of review findings
No qualitative evidence was identified for this review question.
1.4.5. Qualitative evidence summary
No qualitative evidence identified for this review question.
1.5. Economic evidence
The committee agreed that health economic studies would not be relevant to this review question, and so were not sought.
1.6. Resource impact
The recommendations made by the committee based on this review are not expected to have a substantial impact on resources.
1.7. Evidence statements
1.7.1. Qualitative evidence statements
No qualitative evidence was identified for this review question.
1.8. The committee’s discussion of the evidence
1.8.1. Interpreting the evidence
1.8.1.1. The quality of the evidence
No qualitative evidence was identified for this review question.
1.8.1.2. Findings identified in the evidence synthesis
No qualitative evidence was identified for this review question.
1.8.2. Cost effectiveness and resource use
Health economic studies were not sought for this question as it is a qualitative review.
The recommendations generally provide guidance regarding the content of information and support specific to people with primary hyperparathyroidism in line with the general principles of provision of information already established in the existing NICE Patient Experience Guideline and so were not considered likely to have a substantial resource impact over and above this.
1.8.3. Other factors the committee took into account
The committee recognised the importance of having recommendations on what information should be given to patients, and drew on the experiences of the committee members and their interaction with their patient networks to inform their recommendations. They noted that there are two related areas that this information should address: information to inform the patient’s understanding of the condition, and information to help the patient make informed decisions about their care. Currently the information provided to patients is not always felt to be adequate to inform understanding of the condition and decision-making, and from the experience of the lay members of the committee patients often resort to using the internet to find information. They highlighted in particular that it is important for GPs to be aware of the condition and to give full information to patients, although the need to give enough accurate, balanced and current information could still be improved in secondary care, particularly in the area of informed decision making for surgery.
The committee noted that the decision about whether to undergo surgery is a key one in the patient’s experience of the condition. They emphasised the importance of clinicians being able to offer a balanced view based on the individual patient they are treating, with the acknowledgement upfront that in the majority of cases the treatment is surgery, and that pharmacological therapy is not curative. The lay members of the committee highlighted that where patients have chosen to have surgery, they often want to know how many procedures the surgeon has undertaken, their success rates and surgical experience. Clinicians should acknowledge this and provide information to patients where requested.
The committee highlighted people who are waiting for surgery or who have not met the criteria for surgery. Clinicians should be aware that this can be frustrating for patients, and should continue to provide timely information for those patients.
The lay members of the committee noted that it is important for clinicians to explain what the person can expect during the course of the management of their condition, including who will be involved in their care and at what stages. The committee highlighted that there is a concern about support being given too late, for example after the patient has recovered from surgery. They highlighted the need for timely support in their recommendations. The committee noted that it is important to provide people with information regarding what signs and symptoms to watch out for following surgery.
There is currently large variation in practice in terms of what monitoring and follow up is offered, and the committee considered it important for the clinician to fully explain what is being offered, when it will happen and why it is needed (see the recommendations on monitoring). Ongoing care may include advice on follow-up tests, supplementation (including calcium, vitamin D, magnesium and boron), exercises for the neck, and programmes of exercise and diet to help recover bone density.
There was no evidence for information and support for pregnant women with primary hyperparathyroidism. The committee discussed the need for clinicians to give advice to patients about the possible impact of primary hyperparathyroidism on the fetus, including survival and child development, and any potential long-term impact on intelligence or future disease. The committee discussed the importance of information on the risks and benefits of treatments including medicines and parathyroid surgery during pregnancy. The committee also felt that post-partum advice about breastfeeding would be appropriate.
References
- 1.
- Jones KR, Burney RE, Christy B. Patient expectations for surgery: are they being met? Joint Commission Journal on Quality Improvement. 2000; 26(6):349–60 [PubMed: 10840667]
- 2.
- McGill JF, Moo TA, Kato M, Hoda R, Allendorf JD, Inabnet WB et al. World wide what? The quality of information on parathyroid disease available on the Internet. Surgery. 2009; 146(6):1123–9 [PubMed: 19958939]
- 3.
- Neary PM, Sung R, Corrigan M, O’Donovan M, Cahill RA, Redmond HP. The benefits of an interactive, individualized online patient pathway for patients undergoing minimally invasive radioguided parathyroidectomy: a prospective, double-blinded, randomized clinical trial. Surgical Innovation. 2010; 17(3):236–41 [PubMed: 20647234]
- 4.
- Perez-Ruiz L, Lasheras-Alonso M, Gomez-Arbones X, Ros-Lopez S, Pelayo-Salas A, Salcedo-Mata MD. The effects of successful parathyroidectomy on clinical and biological manifestations of primary hyperparathyroidism. Acta Chirurgica Belgica. 2006; 106(5):532–6 [PubMed: 17168264]
Appendices
Appendix A. Review protocols
Appendix B. Literature search strategies
The literature searches for this review are detailed below and complied with the methodology outlined in Developing NICE guidelines: the manual 2014, updated 2017 https://www.nice.org.uk/guidance/pmg20/resources/developing-nice-guidelines-the-manual-pdf-72286708700869
For more detailed information, please see the Methodology Review.
B.1. Clinical search literature search strategy
Searches for patient views were run in Medline (OVID), Embase (OVID), CINAHL, Current Nursing and Allied Health Literature (EBSCO) and PsycINFO (ProQuest). Search filters were applied to the search where appropriate.
Appendix C. Qualitative evidence selection
Figure 1. Flow chart of qualitative study selection for the review of information
Appendix D. Qualitative evidence tables
No qualitative evidence identified for this review question.
Appendix E. Excluded studies
E.1. Excluded qualitative studies
Final
Qualitative evidence review
This evidence review was developed by the National Guideline Centre
Disclaimer: The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. All NICE guidance is subject to regular review and may be updated or withdrawn.