Except where otherwise noted, this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Preface
RISING HEALTH CARE COSTS are a major challenge to the American economy, particularly at a time of deepening recession and a renewed commitment to extend coverage to the uninsured. Dartmouth Atlas research on geographic differences in health care delivery and spending points to an opportunity to achieve significant savings in health care costs without compromising health care quality and outcomes. More spending and more utilization do not translate into improved life expectancy for those with chronic illness. The differences in the use of discretionary surgery do not reflect differences in patient preferences and informed patient choice. This paper discusses opportunities for Congress and the Obama Administration to address key shortcomings in our health care system that result in unwarranted geographic variation and uncontrolled growth in health care spending. Success in this effort will not only improve the quality of care, it will make it possible to extend coverage to America’s uninsured without inducing a major increase in health care spending.
This Dartmouth Atlas White Paper was written by John E. Wennberg, Shannon Brownlee, Elliott S. Fisher, Jonathan S. Skinner and James N. Weinstein.
December 2008
Executive Summary
HEALTH CARE IN AMERICA is not nearly as good as it should be. Quality is inconsistent and often poor, rates of errors and other adverse events are unacceptably high, and costs are higher than anywhere else in the world. Indeed, even as cost growth in the U.S. outpaces that of many European countries, life expectancy is lagging behind.i
This much is now widely known, in part because health care policy experts have spent the last three decades defining the myriad ways in which the U.S. health care delivery system is failing to serve patients. But not all health care in America is alike. There are islands of excellence in the sea of high cost mediocrity—hospitals and physician practices that are delivering high value health care that is less costly, more efficient, and produces better health outcomes.
What’s so special about these hospitals and physician practices? They are organized systems of care—group practices and integrated hospital systems—and they have names that many Americans would recognize: the Billings Clinic in Montana; Geisinger Clinic in Pennsylvania; the Marshfield Clinic in Wisconsin; Kaiser Permanente in California, the Mayo Clinic in Minnesota, Group Health Cooperative in Washington; and Intermountain Healthcare in Utah, to list just a few. These systems have figured out how to improve the quality of the care they deliver and simultaneously contain costs, without denying patients needed, effective care. All Americans deserve to have access to such superior health care, not just those who happen to live near these hospitals and physicians. Now is the time to build high-performing, high-quality, organized health care systems throughout the nation.
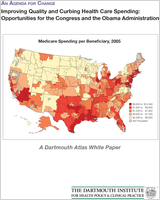
This white paper proposes strategies to move the rest of the nation toward organized delivery systems, improve the quality of health care and scale back costs and cost growth. Our strategies are based on extensive original research and 20 years of data gathered by the Dartmouth Atlas Project, which has documented remarkable differences in per capita Medicare spending from one geographic location in the country to another. We have found a 2.5-fold variation in Medicare spending in different regions of the country, even after adjusting for differences in local prices, and the age, race and underlying health of the population. This geographic variation in spending is unwarranted. Patients who live in areas where Medicare spends more per capita are neither sicker than those who live in regions where Medicare spends less, nor do they prefer more care. Perhaps most surprising, they show no evidence of better health outcomes. These insights therefore overturn the conventional views that more spending on health care translates automatically into better health outcomes.
This paper summarizes our analysis of this unwarranted geographic variation, and it offers a new way to address the root causes of some of the most evident flaws in American health care.
Our recommendations are particularly important at a time when the nation seems committed to addressing the problem of the uninsured, lest an expansion of coverage become unsustainable due to runaway health care costs. This white paper addresses the following key shortcomings in our health care system:
- disorganized, poorly coordinated, and inefficient care that results in the underuse of effective medical interventions and the overuse of physician visits, consultations, hospitalizations and stays in intensive care units, particularly in treating chronic illness;
- clinical decisions that fail to adequately take patient preferences into account, resulting in unnecessary, unwanted elective surgery;
- poor clinical science;
- workforce policies that have resulted in an undersupply of primary care physicians, and an oversupply of physician specialists; and
- insurance markets that are ill equipped to address unwarranted geographic variation in health care delivery because the prices of premiums in any given region are not closely linked to the local cost of medical care.
We believe the federal government is uniquely situated to drive real change in the health care delivery system. Only the federal government, by virtue of its influence over the delivery system through Medicare and Medicaid; its influence over federal science policy; its potential power to shape the size and specialty mix of the physician workforce; and the role it will play in extending insurance coverage to the uninsured, is in a position to bring about the coordinated changes required to address these problems.
In addition to improving the quality of care, transforming the delivery system would also save money. How much could the nation save, if all providers were to adopt the practices of organized practices? Using the Mayo Clinic as a benchmark, the nation could reduce health care spending by as much as 30 percent for acute and chronic illnesses; a benchmark based on Intermountain Healthcare predicts a reduction of more than 40 percent. Substantial savings in Medicare spending on surgery—perhaps as much as 30 percent—are also possible if demand for elective surgery were based on informed patient choice.
The Obama Administration and the Congress should build consensus around the following priorities for a new American health care policy:
- Promote the Growth of Organized Systems of CareFederal policy is currently trying to reduce unwarranted variation in piecemeal fashion, through the Pay-for-Performance program at Medicare, for example, or web-based information systems such as Hospital Compare. We recommend that the federal government develop a multi-year plan to improve the quality of care and improve health outcomes through a different strategy—by promoting organized care. We offer a set of specific payment changes that would spur hospitals and other providers to develop organized delivery systems that would reduce the underuse of effective care and the overuse of unnecessary care through a shared savings program.
- Require Informed Patient Choice and Shared Decision-MakingThe current standard of care fails to adequately inform patients about the risks and benefits of treatment options, including the pros and cons of invasive treatments such as elective surgery. This in turn leads to higher costs—patients getting treatments they don’t want—and may encourage malpractice suits. Changing the standard for informing patients and promoting shared decision-making offers a means for reducing the misuse of such care. We recommend two parallel strategies to achieve this goal.First, the Administration should move rapidly to implement standardized approaches to ensuring informed patient choice within federal health programs. (We also urge state legislatures to redraft informed consent laws to promote informed patient choice as the standard of practice for discretionary treatments.)Second, the Centers for Medicare and Medicaid Services should reform payment policies to reimburse providers for the costs of supporting shared decision-making; reward providers who achieve high quality patient decision-making; and, ultimately, require that hospitals and surgery centers support shared decision-making as a condition for participation in the Medicare program.
- Establish a Federal Physician Workforce Policy that Achieves the Goals of Organized CareThe nation does not need to expand its supply of physicians; it already has enough active physicians and trainees in the pipeline to take care of the needs of America’s citizens well into the future. Congress should resist efforts to remove limits on the number of graduate medical training posts funded by Medicare. Instead, Medicare should promote the training of primary care physicians and preferentially fund post-graduate training programs that teach coordinated, community-based care in treating chronic illness. It should also favor programs that support shared decision-making and emphasize the development of communication skills.
- Fund a Federal Science Policy that Builds the Scientific Basis for Cost-Effective CareMedical effectiveness research must create a system for continuous evaluation of emerging clinical theories and technologies. Federal medical science policy should support research to establish best ways to provide physicians and patients with the information they need to make informed choices.
This white paper does not address specific proposals that are emerging to fix the problem of America’s uninsured. However, our recommendations could fit into any plan for covering more Americans, and this white paper draws attention to two significant implications of our research for coverage reform:
- Geographic Equity and Regional MarketsTo accurately measure cost and effectiveness in health care, policy makers need to understand a fundamental distinction: health care market boundaries differ from geographic/political boundaries. Today’s insurance market is ill equipped to encourage more efficient delivery systems such as organized group practices, in part because the cost of insurance premiums is not closely linked to actual costs of medical care in a given market. As a result, citizens in markets where providers are better organized and more efficient are subsidizing the inefficient, more costly care in other regions of the country. Accordingly, legislative initiatives to expand coverage must also establish regional boundaries around true health care markets, rather than political regions. This will promote geographic equity and draw attention to the need for promoting organized delivery systems. Premiums and taxes should be adjusted to reflect (price and illness-adjusted) regional per capita costs.
- Increasing Coverage Without Increasing the Overall Costs of CareMost analyses of coverage reform predict that we will spend substantially more on health care once the uninsured gain coverage. But we believe that expanding coverage will have a smaller impact on health care spending, providing that capacity is not increased. This underscores the importance for the Congress and the administration to address the root causes of unwarranted variation.
Comprehensive health care reform is not only possible, it is imperative. Conventional wisdom would assert that in the current fiscal crisis, we cannot afford to embark on reform, and that Americans are not prepared to stomach dramatic changes in either their coverage or the way care is delivered. But a recent survey published in the New England Journal of Medicine reported that 70 percent of respondents believe that the system needs major changes, if not a complete overhaul. Moreover, the Congressional Budget Office (CBO) projects that health care costs will rise from 17 percent of GDP today to 25 percent by 2025. We believe that affordable, high quality health care coverage should be the goal. The way to achieve that goal is through fundamental changes in the delivery system, and the time to begin making those changes is now.
The Problem of Unwarranted Variation in Medical Practice
For the past 35 years, research has documented remarkable differences in per capita Medicare spending from one geographic location in the country to another, even after adjusting for differences in local prices, and the age, race and underlying health of the population. These variations are unwarranted because they cannot be explained on the basis of illness, medical evidence or patient preferences. Our research shows that many, if not most, of the clinical decisions doctors make are driven by local medical opinion and the local supply of medical resources, rather than sound science or the preferences of well-informed patients.
This white paper focuses on two kinds of care that vary across regions. The first is “preference-sensitive care,” or care whose frequency of use is driven in large measure by physician opinion. Despite the current talk about patients as “consumers,” capable of directing their own care and being prudent and discerning health care purchasers, most patients continue to defer to their physicians when it comes to deciding what care they receive. When it comes to elective surgery, we know that physician opinion can vary widely as to when the treatment is necessary, and which patients are appropriate. Consequently, the frequency of discretionary surgery such as knee or hip replacement, or back surgery, also varies remarkably from one region to another.
The decision about which treatment to use should be shared with the fully informed patient. Yet only rarely are patients fully informed. Failure to base the determination of medical necessity on informed patient choice leads to misuse of care, to what should be considered a form of medical error: operations on patients who, had they been adequately informed, and given a real chance to share in the decision-making, would not have consented to surgical treatment.
The second form of care that varies dramatically from place to place is “supply-sensitive care.” For the 90 million Americans with chronic illness, the frequency with which they see a doctor, are hospitalized or admitted to an intensive care unit, and their chances of dying in the ICU, hospice, or at home, depends less on what care the patient needs or wants and far more on the numbers of available hospital beds, clinics, CT scanners, doctors and hospice workers per capita in their community. For such supply-sensitive services, decisions surrounding medical necessity are strongly influenced by capacity, rather than medical evidence or severity of illness. As a result, the amount and type of care patients get varies from place to place, depending in large measure upon the capacity of the medical sector in the region where they happen to live. In many regions of the country, particularly those served by disorganized delivery systems, we have documented both underuse, or the failure to deliver needed, evidence-based care, and overuse, or the delivery of unnecessary supply-sensitive care.
These findings bear directly on both the cost and quality of U.S. health care. A growing body of evidence shows that much of the supply-sensitive care being delivered in this country has at best no impact on the nation’s health. At worst, excess care is leading to net harm. At the same time, spending more is not resulting in more patients receiving effective care.
This paper summarizes our analysis of this geographic variation and proposes strategies for building high-performing, high-quality, organized health care systems throughout the nation.
Understanding Supply-Sensitive Care
Much of our research at the Dartmouth Atlas Project has focused on the remarkable variation in “supply-sensitive” care. The patients most affected are those with progressive chronic illnesses, such as chronic lung disease, cancer, diabetes or heart failure. For patients with such conditions, clinical science has yet to determine the most effective and efficient means of delivering health care. Therefore, it provides few evidence-based guidelines to govern the frequency of use of routine care such as physician visits, hospitalizations to the medical wards, admission to intensive care units, and imaging tests. In the absence of evidence, the prevailing cultural assumption that more medical care is better takes hold, leading physicians unconsciously to use available resource capacity up to the point of its exhaustion. This assumption is amplified in a fee-for-service environment that pays providers more for doing more.
The per capita utilization of this type of care is strongly correlated with the capacity of local regions and hospitals. For example, we have shown that half of the regional variation associated with hospitalizations for medical conditions, visits to medical specialists, and the use of coronary angiography can be explained by the per capita supply of beds, specialists, and angiography units. This is why we call this kind of care “supply-sensitive.”
The principal argument made against our findings has been that regions1 and hospitals that deliver more care have sicker patients than regions and hospitals that deliver less care. But 20 years of data show clearly that there is remarkably little correlation between prevalence of severe chronic illness and the 2.5-fold variation in per capita Medicare spending across regions. What does correlate with that large variation in spending is the intensity of care provided to patients once they are sick—most notably, the number of days spent in hospital and the number of physician visits per capita. Indeed, it is the frequency of use of acute care hospitals among those with chronic illness that is the strongest predictor of Medicare spending, not prevalence of chronic disease. And the intensity of care delivered is largely uncoupled from illness (Figure 1).
Doing more (and spending more) might be justified if it resulted in better health outcomes. But at the population level, our research and that of others has shown that more resources and more care (and more spending) aren’t necessarily better. Patient populations with severe chronic illness living in regions where providers deliver the most intensive inpatient care do not enjoy improved survival or better quality of life. The quality of care is no better. Providers in regions of the country where Medicare spends more per capita are no better at consistently delivering evidence-based care than those in regions where Medicare spends less. Moreover, physicians in high-spending regions report worse communication among caregivers, and patients report being less satisfied with their care than peers in regions where Medicare spends less.
The most surprising and significant conclusion is that more care may in fact be worse. Research has shown that mortality is higher in regions where the intensity of care in managing chronic illness is higher.ii In other words, chronically ill patients are at greater risk of dying in regions where the health care system delivers more supply-sensitive care.
How can more care result in higher mortality? Patients can be harmed by medical intervention in many ways. It is becoming increasingly evident that hospitals can be dangerous places, where patients face the risk of medical error, adverse events, and hospital-acquired antibiotic-resistant infections, which according to some accounts are responsible for about 100,000 deaths annually.iii Patients with chronic illness are particularly vulnerable; the more time spent in the hospital, the greater their exposure to error, infection, and adverse events. As care becomes more complex, and as more physicians get involved in an individual patient’s care, it becomes less and less clear who is responsible, and miscommunication—and medical errors—become more likely. Greater use of diagnostic tests increases the risk of finding— and being treated for—abnormalities that are unlikely to have caused the patient any problem (a condition referred to as “pseudodisease”). Patients who receive care for conditions that would have never caused a problem can only experience the risk of the intervention.
In regions of the country where patients receive fewer services, providers are not necessarily rationing valuable care. Rather, they are providing higher quality care on average, greater patient satisfaction, and population-based outcomes that are as good as if not better than those of providers who are delivering more care per capita. They are delivering higher value care.
How are they doing it? Regions with low Medicare spending profiles—those in the bottom 20 percent of regions on per capita spending—are typically served by organized systems of care, either large group practices or integrated hospital systems. A growing body of evidence has built an impressive case that organized practices are better situated than the disorganized, fragmented practices that characterize most of our health care system to deliver high quality, high value care. The Dartmouth Atlas documents that most organized delivery systems are more efficient. They provide high quality care at a much lower per capita cost than most providers throughout the United States in the management of patients with chronic illness.
Implications for Reform
Our findings suggest several new ways to bend the health care cost curve downward and build high-value delivery systems. First, federal, state, and local health care policy makers must understand the following about supply-sensitive care:
- The patchy distribution of health care resources combined with the variation in overuse of acute care hospitals and the way Medicare is financed have created the inequitable situation in which taxpayers (and employers) in low-cost regions, where providers are relatively efficient, are subsidizing relatively inefficient providers in high-cost regions.
- Health care utilization in managing chronic illness is rising everywhere, but it is rising fastest in the highest-cost, least efficient regions of the country—the regions that are already overusing care the most. For example, between 2001 and 2005, the number of days that Medicare recipients spent in ICUs during the last two years of life rose 18 percent in regions that ranked in the highest quintile of per capita Medicare spending in 2001. Among regions ranking in the lowest quintile, it rose 11 percent.
- Fee-for-service patients in high-cost regions are also losing financially, because greater utilization means higher co-payments. For example, the average co-payment for Medicare beneficiaries with chronic illness living in Miami, a high cost region, is $5,000 dollars in the last two years of life. For those living in Minneapolis, it is $1,900, because beneficiaries with chronic illness in Minneapolis receive less unnecessary care.
- Moreover, Medicare enrollees in Minneapolis who enroll in Medicare HMOs receive fewer benefits than enrollees in Miami because payments to HMOs are tied to county-level per capita fee-for-service payments. Such financial inequities can be a powerful incentive for reform.
But the need to curb the overuse of supply-sensitive care isn’t just a matter of geographic unfairness or economics. Overuse also alters the life experience of the patient. We already know that most Americans will die from chronic illness, but how they die varies according to where they live. Among the chronically ill, about 30 percent of those living in such high-cost regions as Los Angeles and Miami will experience a stay in an intensive care unit at the time of their death; in Minneapolis and Portland, OR, by contrast, the proportion of patients whose death is associated with a stay in the ICU is only 14 percent.
It is also vital that we recognize that the overuse of care is not just an end-of-life phenomenon. Care intensity during terminal care and the last six months of life is part of a pattern: providers who deliver aggressive care at this stage in the progression of chronic illness also do so at earlier stages. If a high tech death were the price the dying must pay to make sure those at earlier stages of disease enjoy a longer life, then it might be viewed as the cost of medical progress. But in view of the evidence that greater care intensity is not paying off in terms of improved life expectancy, this does not appear to be the case. Reducing overuse will likely improve the outcomes of care, and it could lead to more compassionate care of patients as they near the end of life.
It is vital to both patients and the American economy that we curb overuse, rationalize the supply of medical resources, promote organized care, and improve the scientific basis of clinical decision-making. Since Medicare spends most of its dollars on the chronically ill in acute care hospitals, reducing the overuse of acute care hospitals would substantially cut Medicare spending, and improve both geographic equity and the financial consequences to patients.
How much could Medicare save? Given the strong national reputations enjoyed by such organized practices as the Mayo Clinic and Intermountain Healthcare, and the objective evidence that they deliver more efficient, higher quality care, it seems reasonable to use these systems as benchmarks for the rest of the country. Were all providers in the country to achieve the same level of efficiency for inpatient spending on supply-sensitive care, we estimate a 28 percent reduction in hospital spending under a Mayo benchmark and a 43 percent reduction under an Intermountain benchmark.
Reducing Overuse of Supply-Sensitive Care and Promoting Organized Care
We recommend that the federal government develop a multi year plan to reduce overuse of supply-sensitive care, promote the growth of organized care, and move the nation toward cost-effective management of chronic illness.iv
The plan would begin with a voluntary shared savings program in which Medicare would return to participating providers a portion of the savings from lower utilization that would follow from improving care organization and matching medical resources to the patient population. Providers could be individual hospitals, hospital chains, multispecialty group practices, and large primary care groups. Routine performance reports, generated from Medicare claims (and now available in prototype on the Dartmouth Atlas website) can be used to monitor change and measure savings as providers improve efficiency.2
As a condition of participation in the voluntary program, providers would agree to establish an organized delivery system for caring for their populations of chronically ill patients. These systems would emphasize coordinated, community-based care over the course of illness. For many, if not most, participating systems, improving quality and efficiency will mean reducing capacity—cutting the number of ICU beds per capita, for example, and other overused resources such as imaging machines. The savings shared with providers would be targeted to cover the cost of downsizing (including the amortization of debt and reallocation of professional workforce to new tasks), and investments made in organizing care, such as the capital costs of installing electronic medical records and establishing the infrastructure for disease management.
The greatest potential for generating savings for Medicare will be in regions where providers are the most disorganized and least efficient. For example, if in 2005, hospitals in Los Angeles had achieved the care intensity benchmark of Sacramento hospitals, Medicare would have spent $468 million less for inpatient care.3
We envision the voluntary phase as the testing ground for innovative, workable models for transforming today’s disorganized care systems into accountable care organizations (ACOs), capable of managing capacity and providing organized heath care delivery to their patient populations, particularly those with chronic illness. Organized practices such as the Mayo Clinic, Billings Clinic, and Kaiser Permanente would be well positioned to respond to the incentives of a shared savings program, by expanding within markets where they already have a presence, and entering new markets through the purchase of hospitals and recruitment of resident physicians. CMS could speed the growth of organized care by designating groups of providers and the hospitals with which they are associated as ACOs, which would be measured on the basis of how well they reduce excess utilization and coordinate care for a defined population of patients.v
We also anticipate that multi hospital systems would be interested in participating and could serve as the nucleus for rapid growth of organized care. In 2005, fully 30 percent of traditional Medicare enrollees hospitalized for chronic illness were treated in hospitals belonging to networks with 10 or more member facilities. Intermountain Healthcare provides a model for how hospital networks can develop into coordinated care systems. Primary care centered strategies for organized care may also emerge as part of the evolving concept of the medical home.
We recommend that an overuse penalty be imposed on providers that are extreme overusers of the acute care hospital in managing chronic illness. An overuse penalty, although limited to only a few extreme outlier hospitals, would signal Medicare’s determination to eliminate wasteful, potentially harmful overuse of hospitals in managing chronic illness, and motivate providers to participate in a shared savings program.4 Over the long run, CMS would take steps to ensure that all Americans with progressive chronic illness who are enrolled in Medicare have access to organized care systems, which would provide coordinated care over the course of illness, integrate the various components of community-based care, and avoid the overuse of acute care hospitals.
With appropriate changes in federal policy with regard to medical education and post-graduate education, the professional workforce in the United States will be increasingly suited to the needs of organized care, and increasingly competent in the skills required for community-based management of chronic illness. The care of chronic illness will become increasingly evidence-based and sensitive to patient preferences, and payment for longitudinal management of chronic care can be based on knowledge of the resources required to produce such care, provided the nation invests in clinical science. We suggest that at the end of a transition period, the demonstrated capacity to produce such care would become a condition of reimbursement by Medicare for the care of the chronically ill.
Implications for Federal Science Policy
Scientific uncertainty concerning the outcomes and value of health care plagues clinical decision-making and is a major contributor to unwarranted variation in supply-sensitive care. There is growing awareness in the policy community and the Congress that something needs to be done to fill the holes in medical knowledge, but comparative effectiveness research, as currently envisioned, is not enough to reduce unwarranted variation and the overuse of medical care. To play a significant role in health reform, we believe the comparative effectiveness research agenda must follow a clear strategy to reduce supplier-induced demand and establish cost-effective management of chronic illness. The research to address unwarranted variation in the frequency of use of supply-sensitive care for the chronically ill must be radically different from research that is primarily focused on comparing alternative treatment options. The fundamental question focuses on the value of physician visits, referrals, stays in acute care hospitals and ICUs to chronically ill patients over time. Research must first be aimed at rationalizing care processes, including the coordination of clinical responsibilities and roles in managing for care of medical specialists, primary care physicians, nurses, nurse practitioners and physician assistants and other health professionals; it must then be aimed at evaluating the cost effectiveness of alternative strategies for producing integrated care.
The research agenda should be viewed as essential to moving the nation toward organized care systems for managing chronic illness, and the ultimate goal of basing care for America’s chronically ill on good clinical science. Research grants should be targeted to health care organizations capable of redesigning care processes; making effective use of information technologies; managing clinical knowledge and skills; developing effective teams; coordinating care across patient conditions, services and settings over time; and incorporating performance and outcome measurements for improvement and accountability. Currently, only organized delivery systems exhibit these capabilities.5 Funding should be tied to a shared savings program, to soften the landing as these systems become more efficient and learn how to better match resources to patient need.
Implications for Physician Workforce Policy
The number of physicians the nation ought to produce is a topic of considerable importance, if for no other reason than the obvious implications for rising costs. Our work has shown clearly that prevalence of illness is largely uncoupled from the build-up in the supply of physicians in a given health care market. Moreover, we have shown that having more physicians per capita does not result in better care or better outcomes. Organized systems of care (group practices and integrated hospital networks) typically use less physician labor than disorganized care, particularly fewer hospital-based physicians and medical specialists.
The nation doesn’t need more doctors, it needs better organized care. We already have enough physicians in the pipeline to take care of our needs well into the future. Efforts to increase the supply of physicians, particularly specialists, should be resisted. Congress should not increase the number of post-graduate training positions funded by Medicare. Instead, Medicare should preferentially fund post-graduate training programs that favor primary care and teach (by example) coordinated, community-based care in treating chronic illness.
Implications for cost containment
While our focus has been on improving quality and efficiency, we believe the policies we recommend will also work to contain cost. The role of supplier-induced demand for health care and the growth of the capacity of the health care sector contribute to the unsustainable rise in health care costs. Most regions of the country already have more than enough capacity to accommodate increased demand from both aging baby boomers and Americans who are currently uninsured or underinsured, and will presumably acquire coverage in the coming years. Yet in virtually every region of the country, the supply of medical specialists, ICU beds and other such medical resources as imaging machines is increasing. This increase in resource capacity is rising fastest in the regions that already overuse supply-sensitive services the most. Constraining supply in these regions will be necessary if we want to slow health care cost inflation.
Holding the line on new specialists and surgeons will dampen future cost increases that would otherwise result from excess capacity in physician workforce. Improving the scientific basis for managing chronic illness over time will also cut costs. But the most immediate and strongest impact on cost, we believe, would result from CMS’s assumption of a leadership role in promoting organized care and reducing the overuse of supply-sensitive care in acute care hospitals. This will send a powerful signal to health care providers that payers are no longer willing to pay for utilization regardless of its value.
The signal will be particularly strong if CMS follows our recommendation to impose an outlier penalty. The impact of this change in policy should ripple outward to the bond and equity markets, where investors and rating agencies have long assumed that investments in hospitals are safe, because payers always reimburse for utilization. Once this assumption is challenged, a review of practice patterns would likely become part of the bond and equity markets’ evaluation of hospitals seeking financing to increase capacity. Capital for further expansion of the acute care sector should become hard to obtain in health care markets that are overbuilt and overutilizing care.6
Understanding Preference-Sensitive Care
The Dartmouth Atlas Project also describes wide geographic variation in what we call “preference-sensitive care.” Preference-sensitive care is for conditions where legitimate treatment options exist; where the treatment options involve significant tradeoffs in the patient’s quality or length of life; and therefore the choice of treatment should be decided upon by the fully informed patient in partnership with the physician.vi
Under current practice, idiosyncratic medical opinion, or the physician’s preference, has enormous power over how likely patients are to receive several elective surgeries. In Fort Myers, Florida, for instance, 2.3 times as many Medicare enrollees per capita receive knee replacements as do recipients living in the neighboring Miami region. Doctors in Fort Myers are more likely to recommend surgical management of osteoarthritis of the knee while those in Miami favor medical management. Wide variations also exist in recommendations for surgical versus medical management of several conditions among regions served by well known academic medical centers. For instance, in the Palo Alto area, where most care is provided by Stanford University teaching hospitals, back surgery is 2.2 times greater than in San Francisco, home to the University of California, San Francisco (UCSF) Medical Center. It isn’t because UCSF physicians aren’t treating back pain, but rather that they treat it differently, relying more on conservative treatments.
In looking across the country, we see similar variation in rates of surgical options for such conditions as chronic angina (coronary bypass or angioplasty); low back pain (disc surgery or spinal fusion); arthritis of the knee or hip (joint replacement); and early stage cancer of the prostate (prostatectomy). For each of these conditions, there are multiple treatment options including surgery, drugs, life style changes, or watchful waiting.
There are two principal causes for this form of variation. First, there is the poor state of clinical science: for many conditions commonly treated by surgery, the available treatment options have not been adequately tested for efficacy. Thus, when surgeons recommend surgery, they often do so on the basis of subjective opinion, personal experience, anecdote, or an untested clinical theory that might or might not prove true, were it subjected to some actual science.
The other explanation for unwarranted variation in rates of surgery is a flaw in the medical decision process itself. Even when evidence exists as to outcomes, surgery rates can vary dramatically from place to place. This is the case in early stage breast cancer. Mastectomy and lumpectomy have equal outcomes. Yet in an early Dartmouth Atlas study (1992-93), we found regions in which virtually no Medicare women underwent lumpectomy, while in another, nearly half did. Sometimes, adjoining regions had strikingly different rates. For example, in the Elyria, Ohio hospital referral region, 48 percent of Medicare women had breast-sparing surgery for early stage breast cancer, while in Cleveland 23 percent did, and in Columbus less than 12 percent did.vii
Such extreme variation arises because patients commonly delegate decision-making to physicians, under the assumption that not only does the doctor know best, he or she can also accurately diagnose the patient’s treatment preference. Physicians often assume the same. Yet studies show that when patients are fully informed about their options, they often choose very differently from their physicians. Moreover, we have learned the importance of distinguishing between medical necessity, or appropriateness based on evidence, and necessity as defined by the patient. This first became clear in studies of treatment choice for an enlarged prostate. Only about 20 percent of patients who were eligible for surgery actually wanted surgery when they were fully informed about their options.
Under delegated decision-making, even surgeons who base their decision to operate on up-to-date, evidence-based appropriateness guidelines are at risk of operating on the wrong patient—that is, on a patient whose values are such that he or she would not have wanted the surgery, had he or she been adequately informed. The right rate for discretionary surgery in any particular market is the demand for treatments that would emerge were all patients fully informed about the trade offs inherent in any treatment choice, and encouraged to choose according to their own values and preferences.
For example, a patient with early stage breast cancer, for whom mastectomy and lumpectomy are options, would be informed about the advantages and disadvantages of each approach. She might use a patient decision aid, a video or interactive computer program, which helps her both to understand the trade offs and to reach a decision that reflects her personal preferences and values.
The result of this process, applied to all such women, would be rates for lumpectomy and mastectomy that reflect the “true demand” of patients with early stage breast cancer—demand based on informed patient choice. We might still observe geographic variation in rates of mastectomy versus lumpectomy, but that variation would be based on true differences in preferences among patients living in different regions.
Research conducted over the past decade has produced tools that are essential for helping patients make informed choices, including patient decision aids, and methods for monitoring the quality of their decisions. With few exceptions, clinical trials have found that the use of patient decision aids results in a lower demand for surgery compared to control groups given usual care.viii Implementing shared decision-making will enable patients who want surgery to get it, and those who don’t to avoid it.
Moreover, the results indicate that the true demand for expensive, discretionary surgery may be lower than current utilization rates under supplier-induced demand, in some cases dramatically so.
Reducing Unwarranted Variation in Preference-Sensitive Care
Reducing unwarranted variation in preference-sensitive care and establishing the right rate of demand for discretionary treatments require improvements in clinical science and fundamental changes in the ethical standards that govern the way patients are informed. Delegated decision-making should be replaced by shared decision-making, and the doctrine of informed patient consent replaced by informed patient choice.
We recommend three strategies for achieving these goals. First, we urge state legislatures to redraft informed consent laws to promote informed patient choice for preference-sensitive treatments. Second, CMS should take the lead among payers to bring about reform. It should undertake pilot projects to develop implementation models for shared-decision-making in various practice settings and then work to extend successful models throughout the nation, ultimately reimbursing hospitals and surgical centers for elective surgery only if they support a high quality shared decision-making process. Third, the Administration should implement informed patient choice as the standard of practice in the Veterans Health Administration delivery system and the military health care systems.
Establishing Informed Patient Choice as the Legal Standard
Current legal concepts of informed consent are at odds with both modern medical practice and individual autonomy.ix In about half of states, informed consent laws follow a physician-based standard; the rest follow a patient-based standard. The physician-based standard requires physicians to inform patients as a “reasonably prudent practitioner” would do. The fundamental assumption is that physicians agree on both the best treatment option and the information patients need in order to give informed consent—thus codifying the agency role of the physician.
The patient-based standard requires that physicians provide all information that a “reasonable patient” would want to know. This standard also assumes that physicians are good diagnosticians of patient preferences, and that reasonable patients all need the same information about risks and benefits. The flaws in both standards are evident in the wide geographic variation in rates of elective surgeries and tests, and in clinical trials of shared decision-making showing that patients are less likely to choose invasive interventions when fully informed.
A substantial overhaul of the current informed consent system is needed to balance patient autonomy with physician expertise and beneficence. The Washington State legislature has already enacted a law that begins this process.x It explicitly endorses informed patient choice as the preferred standard of practice and grants physicians who use patient decision aids greater immunity from failure-to-inform malpractice suits than is currently provided under informed consent provisions. Moreover, it called for demonstration projects to provide models for implementing shared decision-making in various clinical settings.
Changing the Standard for Payer Determination of Medical Necessity
The medical necessity of an elective treatment has traditionally been determined by payers, who first decide whether to cover a given procedure as part of the benefit package (often in the absence of evidence on comparative effectiveness). Next, payers, using peer review, determine whether the procedure is appropriate, or necessary for a given patient. For preference-sensitive treatments, this is a flawed strategy, because informed patients often want less invasive treatments.
Payers should support the transition to a new standard for determining medical necessity. Under this new model, the payer would still be responsible for determining what procedures to cover, (and experts would continue to create the guidelines for clinical appropriateness), but the determination of which “clinically appropriate” treatment option is medically necessary for an individual patient would be based on what the informed patient chooses.
We recommended that the transition to informed patient choice be led by CMS.xi CMS should extend its pay-for-performance program, now widely used to remedy underuse of effective care, to reward hospitals for providing a shared decision-making process. As the initial target, CMS should concentrate on 10 common conditions, which together account for about 40 percent of Medicare’s spending for inpatient surgery (see Table 1). CMS should implement this program in two phases, after which shared decision-making would be required in order for hospitals to receive reimbursement:
Table 1.
Ten Common Conditions with Widely Varying Use of Discretionary Surgery
Phase I:
During the first phase, providers would compete for funds from a federal grant-in-aid program to test shared decision-making models. Special attention would be given to funding pilot projects in states that enact statutes establishing informed patient choice as the standard of practice, particularly those like Washington state, where the legislature has called for demonstration projects.
During Phase I, the program would also support key research and development tasks that are essential for Phase II, including an analysis of the costs associated with developing and implementing a shared decision-making process, and a process for certifying patient decision aids.
Phase II:
CMS would initiate a program to change the standard for defining medical necessity. On a voluntary basis, group practices, hospitals, ambulatory surgery centers, and primary care physicians practicing in organized medical homes would be encouraged to implement shared decision-making and participate in CMS’s pay-for-performance program. All U.S. hospitals and surgical centers that provide discretionary surgery for one or more of the 10 conditions would be eligible to participate, and would be compensated for the costs of maintaining a shared decision-making process for conditions involving discretionary surgery.7 Participating providers should be eligible for a bonus over estimated real costs, depending upon the extent to which, compared to other participating hospitals, they achieve high quality shared decision-making, as measured by scores on decision quality instruments and success in enrolling eligible patients.
At the end of Phase II, CMS would take the final step to assure that all Medicare patients have access to shared decision-making: it would no longer reimburse hospitals for surgery if they fail to comply with the new standard for defining medical necessity.
Establishing Informed Patient Choice in Federal Health Care Systems
The federal government should establish informed patient choice as the standard of practice by implementing shared decision-making best practices in the Veteran’s Administration delivery system and in military hospitals and clinics. We recommend a phased introduction, beginning with a pilot phase to try different models, followed by implementation of successful models throughout the military and Veterans Administration delivery systems.
Implications for Science Policy
The transition to informed patient choice requires an expansion of research priorities. Research is needed to improve the scientific basis for policy as well as clinical decisions. Policymakers need to better understand and predict demand for expensive preference-sensitive treatments; experts responsible for defining which treatments should be included in benefit packages need better information on effectiveness of care; and patients and providers facing decisions need both up-to-date information on the risks and benefits of various treatment options and an understanding of the importance of patient preference in guiding choice. Here, we emphasize three research areas that should be part of the nation’s comparative effectiveness agenda.
- Ongoing, up-to-date assessment of treatment optionsRational decision-making requires an accurate assessment of the outcomes of care that matter to patients. An organized research agenda is needed for the continuous evaluation of the clinical theories and supporting evidence that justify the range of interventions offered. We believe the experiences of the Patient Outcomes Research Team approach funded under the medical effectiveness initiative of the Agency for Health Care Policy and Research provides a firm basis for the design of a contemporary research strategy for achieving this goal.
- Practical tools for decision supportOver the past decade, patient decision aids have become increasingly available for a number of clinical conditions. Their effectiveness has been tested in more than 50 clinical trials. These studies confirm that decision aids work to facilitate shared decision-making: they increase a patient’s knowledge of what is at stake; promote active engagement in decision-making; reduce uncertainty on the part of the patient about which treatment to choose; and improve the agreement between the patient’s values or preferences and the treatment option that is actually chosen. The availability of a growing library of patient decision aids makes feasible the broad implementation of shared decision-making into everyday practice. To facilitate the transition to informed patient choice, the comparative effectiveness research agenda should fund work to advance the art and science for constructing decision aids, decision quality measures, and other tools for supporting shared decision-making.
- Studies of patient demand for preference-sensitive careThe research agenda should include a focus on understanding the implications of the shift from delegated decision-making to informed patient choice on the health care economy. The first priority should be to understand and predict the demand for elective surgery under informed patient choice, focusing on the conditions for which surgery is one of at least two clinically appropriate options. The research should also address the effects of co-payment and other forms of patient cost-sharing on patient preferences for the more expensive treatment option. This research is essential if rising patient demand for expensive, invasive treatments requires cost-sharing as a means of reducing costs.
Implications for Physician Workforce Policy
Primary care practices are well situated to ensure that utilization rates for preference-sensitive treatments approximate true demand based on informed patient choice. Unlike specialists, primary care physicians have no financial stake in a patient’s decision among treatment options. Primary care physicians can identify patients who meet evidence-based guidelines for appropriateness and then, through shared decision-making, help patients learn which treatment they want. CMS should give special priority to Phase I projects aimed at developing the role of primary care physicians as professional advocates for informed patient choice and the medical home as the site for implementing shared decision-making.
Implications for Cost Containment
We believe the policies we recommend for shifting from delegated decision-making to shared decision-making could result in lower costs. Most clinical trials show that patients who engage in shared decision-making are less likely to choose surgery when compared to patients who are informed through usual practice. Extrapolations from these trials predict a substantial reduction in per capita Medicare spending for surgery and as much as a 30 percent decline in utilization rates. This suggests that improving the quality of patient decision-making may also be good news for cost containment.
However, cost containment is not certain. If cost containment objectives are not achieved solely through implementing informed patient choice, policymakers have the option to adjust the proportion of the cost borne by patients who choose more expensive treatments. This is why we suggest that studies of demand for preference-sensitive surgery under different cost-sharing options be included in the medical effectiveness research agenda.
Implications for Extending Coverage to America’s Uninsured
This white paper does not deal directly with priorities and strategies for fixing the problem of America’s uninsured. However, supply-induced demand has two significant implications for the design of payment reform. The first is the opportunity for addressing the issue of geographic inequity that occurs because patients in regions served by relatively efficient providers are subsidizing less efficient providers in other regions. Our data make it possible to adjust premiums to the true per capita cost of care in regional markets. Moreover, making this geographic inequity transparent could increase the motivation on the part of companies, patients, and payers to reduce unwarranted growth in health care spending.
Geographic Equity and Regional Markets
We recommend that legislation intended to extend coverage to the uninsured adjust the dollar amount of premiums to reflect the cost of delivery in regional health care markets. Today’s insurance market is ill-equipped to drive providers toward organized systems, in part because the price of insurance premiums is not closely linked to the actual cost of medical care in a given market. As a consequence, there is little feedback in the form of differential premium price that reflects differences in utilization rates, and thus cost of health care delivery at the local and regional level.
This is true of both private and public payers. Medicare doesn’t adjust premiums or tax contributions to regional spending patterns. As a result, there are long-standing transfer payments from more efficient, low-spending regions of the country to less efficient, high-spending regions. The transfer payments, accumulated over the life time of Medicare enrollees, can amount to tens of thousands of dollars per capita.
The pricing of private insurance is also associated with transfer payments. For example, federal employees make the same contribution to insurance pools, no matter where they live; auto workers in Iowa help pay for auto workers in Michigan; and California teachers pay the same premium and experience the same deduction from wages, whether they live in a high- or low-cost region of the state. Why should those living in low-cost, more efficient health care markets subsidize providers in high-cost markets, when the reason for high costs isn’t illness but inefficient care?
The problem isn’t just one of equity. If the cost of medical coverage reflected differences in local and region market spending, then the problems of disorganized care, underuse, misuse, and overuse would become more transparent to local opinion leaders and decision makers. The realization that health care delivery relates to capacity, and capacity relates to costs, would begin to emerge as a local issue—something that local leaders might do something about. It would become apparent that decisions to increase capacity of acute care hospitals by building beds, buying new imaging equipment, or hiring new surgeons or other specialists would have a direct impact on local utilization, and thus the local price of insurance. Further, if accompanied by routine reports such as those available on the Dartmouth Atlas web site, which compare per capita supply of medical resources, utilization and spending among local providers and across regional markets, the stage might be set for serious debate over whether more care is better, and efforts to increase local capacity might be viewed with some skepticism.
For these reasons, we recommend that legislative initiatives to extend coverage contain a provision to establish boundaries around regional markets, empirically defined according to patterns of use of health care. Premiums and taxation could then be set according to (price- and illness- adjusted) differences in regional per capita utilization and costs. We also urge that coverage reform legislation contain provisions for extending the routine monitoring of regional health care markets and their constituent providers to include data from all payers, not just traditional Medicare.
Likely Effects of Increasing Coverage on the Overall Costs of Care
Most analyses of coverage reform predict that we will spend more as a nation on health care once the uninsured gain coverage and begin consuming more care. But we predict that covering everyone will have a much smaller impact on the trend in overall costs of health care delivery than is commonly assumed, provided that capacity is not increased. Our understanding of the nature of the disequilibrium between the supply of medical resources and utilization predicts that increasing the patient population (by increasing the number of people who are insured) will decrease the overall per capita utilization and per capita costs of medical care, as long as supply is held constant. More patients will receive care, but each patient will receive less. Thus, overall spending will not rise as much as predicted—as long as supply is held constant and providers are not permitted to raise prices.
Our studies and the Massachusetts experience predict that expanding coverage will draw attention to the difficulties patients have in accessing care, particularly when they need to find a primary care physician, or see a doctor because of an acute problem. This will occur with greater frequency in high cost regions. But this is more a symptom of the payment system and disorganized, chaotic care than a real problem in scarcity of resources. We believe these considerations underline the importance of the federal government taking the lead in promoting reform of the delivery system along the lines discussed in this paper.
Summary
The United States now faces the worst recession in decades. While the immediate cause of the current crisis is the failure of banks and Wall Street, over the long term the most important threat to the nation’s fiscal health is rising health care costs.xii According to Congressional Budget Office projections, total spending on health care is expected to rise from 16 percent of GDP in 2007 to 25 percent in 2025 and 49 percent by 2082.xiii These projections will have an impact not only on the federal budget, but also the capacity of American companies to compete in the global marketplacexiv and the American worker to enjoy the fruits of his labor in the form of increasing income. Since 1988, wages have been virtually stagnant, as productivity has been siphoned off in part into rising health care premiums.xv xvi The need to reduce inefficiency and costs in health care has never been more pressing.
We believe that controlling costs and improving the efficiency of our health care system require strategies that go beyond the current prescriptions for reform. Comparative effectiveness has been hailed as a means toward increasing efficiency and reducing the misuse and overuse of care. While this is necessary, it is not sufficient. Electronic health records have been shown to reduce medication error and duplication of diagnostic tests; help physicians manage complex cases, particularly those of the chronically ill; and improve coordination of care among different physicians. But these gains in efficiency have been seen for the most part in organized group practice settings, which are uniquely prepared to use the information gained from health information technology to improve care. Congress, CMS, and the Administration should focus a significant part of reform efforts on expanding organized care. This is the fastest way to achieve the goals of increased efficiency, higher quality, and better outcomes. We urge the Congress and the new administration to push forward with a coordinated, multi-pronged strategy for health care reform that includes the methods outlined here for reducing unwarranted variation, expanding organized care systems, and improving quality. The wealth and health of the nation depend upon it.
Footnotes
- 1
Here we are referring to Dartmouth Atlas Hospital Referral Regions (HRRs), which are geographic areas about the size of a typical county that represent natural health care markets: the majority of residents in an HRR get the majority of their care at one or more hospitals within that region. There are 306 different HRRs in the U.S. For details, please visit DartmouthAtlas
.org - 2
By efficiency, we do not mean production efficiency, but rather the best outcomes and highest quality for the lowest utilization and cost.
- 3
In 2005, for acute and chronic medical conditions, the per capita days spent in hospital in the Sacramento region were 45% less than Los Angeles; They were 71% lower for inpatient physician visits.
- 4
The outlier penalty can be calculated on a hospital-specific basis using Medicare claims.
- 5
The Institute of Medicine’s landmark report, Crossing the Quality Chasm, set out these basic requirements for conducting such research.
- 6
We recommend the overuse penalty be used sparingly at first, more as a strategy for stimulating provider participation in the shared savings program than as a method for directly controlling costs. However, if providers do not reduce overuse, the same method for calculating the overuse penalty can be used to set a ceiling for reimbursements to providers. A population-based global budgeting approach will force providers to reduce supply-sensitive care, thus requiring hospitals and their associated providers in high cost regions to alter the practice patterns.
- 7
Certain diagnostic screening exams, such as the Prostate Specific Antigen Test, could also be included.
References
- i.
- Alan M. Garber, and Jonathan Skinner. 2008. “Is American Health Care Uniquely Inefficient?” Journal of Economic Perspectives, 22(4): 27–50. [PMC free article: PMC2659297] [PubMed: 19305645]
- ii.
- Elliott S. Fisher, David E. Wennberg, Thérèse A. Stukel, Daniel J. Gottlieb, F. L. Lucas, and Etoile L. Pinder, “The implications of regional variations in Medicare spending: Part 1. Utilization of services and the quality of care.” Annals of Internal Medicine 2003;138:273-287. Elliott S. Fisher, David E. Wennberg, Thérèse A. Stukel, Daniel J. Gottlieb, F. L. Lucas, and Etoile L. Pinder, “The implications of regional variations in Medicare spending: Part 2. Health outcomes and satisfaction with care,” Annals of Internal Medicine 2003;138:288-298. [PubMed: 12585826]
- iii.
- To Err Is Human: Building a Safer Health System, KohnL.T., CorriganJ.M., DonaldsonM.S., eds. (Committee on Quality of Health Care in America, Institute of Medicine), National Academies Press, Washington, DC 1999. [PubMed: 25077248]
- iv.
- John E. Wennberg, Elliott S. Fisher, Jonathan S. Skinner, and Kristen K. Bronner, “Extending The P4P Agenda, Part 2: How Medicare Can Reduce Waste And Improve The Care Of The Chronically Ill” Health Affairs, November/December 2007; 26(6): 1575-1585. [PMC free article: PMC2213719] [PubMed: 17978378]
- v.
- Elliott S. Fisher, Douglas O. Staiger, Julie P.W. Bynum, and Daniel J. Gottlieb “Creating Accountable Care Organizations: The Extended Hospital Medical Staff” Health Affairs, January/February 2007; 26(1): w44-w57. [PMC free article: PMC2131738] [PubMed: 17148490]
- vi.
- Annette M. O’Connor, John E. Wennberg, France Legare, Hilary A. Llewellyn-Thomas, Benjamin W. Moulton, Karen R. Sepucha, Andrea G. Sodano, and Jaime S. King “Toward The ‘Tipping Point’: Decision Aids And Informed Patient Choice” Health Affairs, May/June 2007; 26(3): 716-725. [PubMed: 17485749]
- vii.
- John E. Wennberg and Megan McAndrew Cooper, eds., The Dartmouth Atlas of Health Care in the United States, American Hospital Publishing, Inc., Chicago, IL 1996. [PubMed: 36264872]
- viii.
- Annette M. O’Connor et al., “Decision Aids for People Facing Health Treatment or Screening Decisions,” Cochrane Review, in The Cochrane Library, Issue 4 (Chichester, U.K.: John Wiley and Sons Ltd. 2006).
- ix.
- Jaime Staples King and Benjamin W. Moulton, “Rethinking Informed Consent: The Case for Shared Medical Decision-Making,” American Journal of Law and Medicine 32 (2006): 429-501. [PubMed: 17240730]
- x.
- For more information on Engrossed Second Substitute Senate Bill (E2SSB) 5930, Chap. 259, Laws of 2007, see Red Orbit News, “Washington Becomes First State to Endorse Shared Medical Decision Making,” Press Release, 2 May 2007, http://www
.redorbit.com /news/display/?id=922404 (accessed 08 December 2008); and Washington State Legislature, “SB 5930—2007–08,” http://apps .leg.wa.gov/billinfo/summary .aspx?year =2007&bill=5930 (accessed 08 December 2008). - xi.
- John E. Wennberg, Annette M. O’Connor, E. Dale Collins, and James N. Weinstein, “Extending The P4P Agenda, Part 1: How Medicare Can Improve Patient Decision-making And Reduce Unnecessary Care” Health Affairs, November/December 2007; 26(6): 1564-1574. [PMC free article: PMC2213717] [PubMed: 17978377]
- xii.
- Congressional Budget Office, The Long-Term Outlook for Health Care Spending (November 2007).
- xiii.
- Len Nichols and Sarah Axeen, “Employer Health Costs In a Global Economy: A Competitive Disadvantage For U.S. Firms” Policy Paper, New America Foundation May 2008 http://www
.newamerica .net/publications/policy /employer_health _costs_global_economy - xiv.
- The 2008 Kaiser/Health Research and Educational Trust Employer Health Benefits Survey Chart Pack p. 2 http://www
.kff.org/insurance /7672/upload/7693.pdf - xv.
- Dean Baker “The Productivity to Paycheck Gap: What the Data Show” Center for Economic Policy and Research Report, April 2007 http://www
.cepr.net/documents /publications /growth_failure_2007_04.pdf - xvi.
- Congressional Budget Office, Evidence on the Costs and Benefits of Health Information Technology (May 2008).
- Preface
- Executive Summary
- The Problem of Unwarranted Variation in Medical Practice
- Understanding Supply-Sensitive Care
- Reducing Overuse of Supply-Sensitive Care and Promoting Organized Care
- Understanding Preference-Sensitive Care
- Reducing Unwarranted Variation in Preference-Sensitive Care
- Implications for Extending Coverage to America’s Uninsured
- Summary
- References
- NLM CatalogRelated NLM Catalog Entries
- PMCPubMed Central citations
- PubMedLinks to PubMed
- An Agenda for ChangeAn Agenda for Change
Your browsing activity is empty.
Activity recording is turned off.
See more...