NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Slaughter-Acey J, Behrens K, Claussen AM, et al. Social and Structural Determinants of Maternal Morbidity and Mortality: An Evidence Map [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2023 Dec. (Comparative Effectiveness Review, No. 264.)
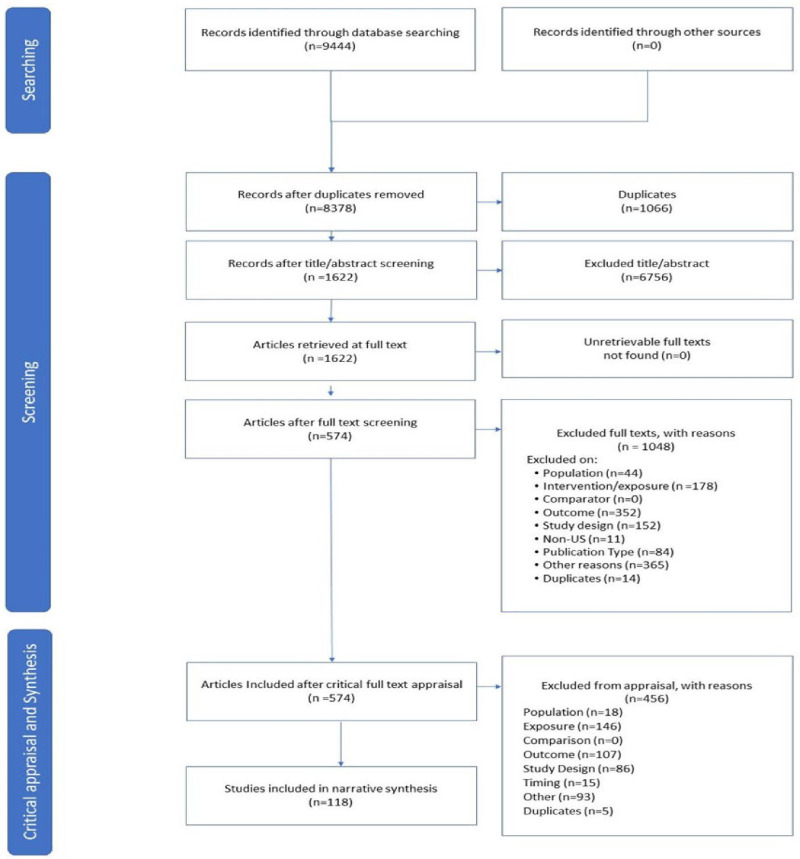
Our search identified 8,378 unique publications for screening. Based on inclusion criteria, we identified 118 eligible studies. We list all studies excluded at full text appraisal, by exclusion category, in Appendix B. Exclusions captured under “other reasons” are varied and overlapping, so often not easily placed into a more singular category. For example, an “other reasons” exclude might have been for both study quality and a challenging interpretation on whether the risk factors were interpersonal in nature. See Figure 3.1 for details of the screening process.
The 118 included studies were published between 2000 and 2022. The studies contained 221 specifically named exposures or factors of interest. While many of these exposures or factors of interest are comparable or overlap, studies used various language and operational definitions for them. Using the named exposures, we categorized the studies into 11 broad exposure domains based on the main social-structural determinant of health. Table 3.1 presents the number of included studies by Key Question and exposure domain. The exposure domains are illustrated by example named exposure or factor of interest. Some studies used data that focused on particular populations, such as Black, Hispanic, or military veterans. As shown in Table 3.1, these populations represent only a subset of the many potential populations of interest.
Table 3.2 presents the number of included studies by Key Qquestion, outcome domain, and special populations for those outcomes. The outcome domains are illustrated by examples of named outcome variables from included studies.
As shown in Table 3.3, included data varied widely in sample size and source. Sample sizes ranged from as small as 16 women whose deaths were examined for potential preventability, to several million pregnant or birthing people. Categories of data sources are provided in Table 3.3. Nine studies used Pregnancy Risk Assessment Monitoring System data.
Tables
Table 3.1Identified eligible studies by major exposure domain
| Key Question, Number of Studies | Exposure Domain | Special Populations |
|---|---|---|
|
KQ1 – 27 studies KQ2 – 11 studies |
Identity and Discrimination Race or Ethnicity, Including Nativity, and Acculturation Reported racial discrimination Spatial polarization (segregation) Rural/urban Socioeconomic factors Disparities in care Gender or sexual minority Patterns of SDOH |
Black African American White Hispanic Asian Immigrants 2nd or 3rd generation immigration status |
|
KQ1 – 9 studies KQ2 – 3 studies |
Socioeconomic status Maternity leave Household income Public insurance State income inequality Unstable housing Homelessness Food insecurity (in combination) |
Low-income Homeless |
| KQ1 – 12 studies |
Violence Intimate Partner Violence Domestic Violence |
Latina Low-income Urban |
| KQ1 – 4 studies |
Trauma Childhood Trauma/ACEs Lifetime trauma exposure Reported racial discrimination Military sexual trauma |
African American Veterans |
| KQ1 – 3 studies |
Psychosocial Stress Stressful life events Partner-related stress PTSD | None |
|
KQ1 – 17 studies KQ2 – 11 studies |
Structural/Institutional Obstetrical unit closure Maternity care deserts Payment policies Neighborhood physical disorders Food deserts Incarceration Municipal expenditures |
Rural Urban Medicaid |
|
KQ1 – 3 studies KQ2 – 3 studies | Rural/Urban |
Rural Urban |
| KQ1 – 6 studies |
Environmental Green factors Pollution Heat exposure | Urban |
|
KQ1 – 2 studies KQ2 – 1 study |
Comorbidities Pre-existing psychopathy Substance use HIV SARS-CoV-2 | Women living with HIV |
| KQ2 – 4 studies |
Hospital Quality of care Safety-net burden Teaching affiliation |
Rural Medicaid |
|
KQ1 – 1 study KQ2 – 1 study |
Healthcare Use Access to healthcare Late entry to prenatal care | Rural/Urban |
Abbreviations: KQ=Key Question; N=number; ACEs=adverse childhood events; PTSD=post-traumatic stress disorder; SDOH=social determinants of health
Table 3.2Identified eligible studies by outcome domain
| Key Question, Number of Studies | Outcome Domain | Special Populations |
|---|---|---|
|
KQ1 – 4 KQ2 - 5 |
Cost/Healthcare Use Postpartum Emergency Department use Postpartum readmission Maternal Intensive Care Unit admission Cost Maternal hospital stay length |
African American Urban Homeless |
|
KQ1 - 37 KQ2 - 1 |
Depression Postpartum depressive symptoms Depressed mood Depressive disorder |
Black White Arabic descent Immigrants Women living with HIV US & foreign-born Latinas Veterans Mexican descent Women who worked during pregnancy |
|
KQ1 - 7 KQ2 - 1 |
Diabetes Gestational diabetes |
Medicaid insured women Hispanic Non-Hispanic White |
|
KQ1 - 18 KQ2 - 3 |
Hypertensive Disorders Hypertension Pregnancy-induced hypertension Hypertensive disorders Preeclampsia |
Non-Hispanic Black women Urban Medicaid insured |
|
KQ1 - 10 KQ2 - 6 |
Maternal Mortality Pregnancy-related death Preventable in-hospital mortality In-hospital death |
Black White Rural Low-income |
| KQ1 - 10 |
Other Mental Health or Substance Use PTSD Suicidal ideation Substance use Anxiety Stress | Latina |
|
KQ1 - 23 KQ2 - 23 |
Severe Maternal Morbidity Blood transfusion Postpartum hemorrhage Major laceration Major puerperal infection Obstetric complications |
Black African American White Indigenous Somali immigrants Sexual or gender minority US military, active or veteran Women experiencing loss of nearest obstetric unit |
| KQ1 - 4 |
Weathering * Epstein-Barr virus reactivation Chronic placental inflammation Excess heart age |
African American Caucasian White |
|
KQ1 – 2 KQ2 - 1 |
Cardio/metabolic-Disorders Peripartum cardiomyopathy Cardiometabolic disorders |
Low-income African American White Hispanic |
- *
Weathering is the physiological effect of premature aging caused by chronic stressful experiences
Abbreviations: KQ=Key Question; N=number; ACEs=adverse childhood events; PTSD=post-traumatic stress disorder
Table 3.3Data sources, number of studies, and sample size ranges
| Data Source Categories | N Studies | Sample Size Range |
|---|---|---|
| Clinic | 5 | 115 – 498 |
| Single Hospital | 11 | 100 – 34,383 |
| Hospital System | 5 | 16 – 675,553 |
| Programs | 25 | 56 – 10,038 |
| City | 6 | 191,947 – 591,455 |
| State (4 PRAMS) | 33 | 118 – 3,020,525 |
| Multi-State (5 PRAMS) | 11 | 1,717 – 6,879,332 |
| Regional | 2 | 301 – 38,915 |
| National (3 PRAMS) | 16 | 501 – 138,311,788 |
| Secondary analysis of Randomized Controlled Trial data | 5 | 930 – 5,759 |
Abbreviations: PRAMS=Pregnancy Risk Assessment Monitoring System