NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-.

PDQ Cancer Information Summaries [Internet].
Show detailsThis PDQ cancer information summary has current information about breast cancer screening. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change. The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
What is screening?
Screening is looking for cancer before a person has any symptoms. This can help find cancer at an early stage. When abnormal tissue or cancer is found early, it may be easier to treat. By the time symptoms appear, cancer may have begun to spread.
Scientists are trying to better understand which people are more likely to get certain types of cancer. They also study the things we do and the things around us to see if they cause cancer. This information helps doctors recommend who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarily think you have cancer if he or she suggests a screening test. Screening tests are given when you have no cancer symptoms.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
See the following PDQ summary for more information about cancer screening:
General Information About Breast Cancer
Key Points for This Section
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast.
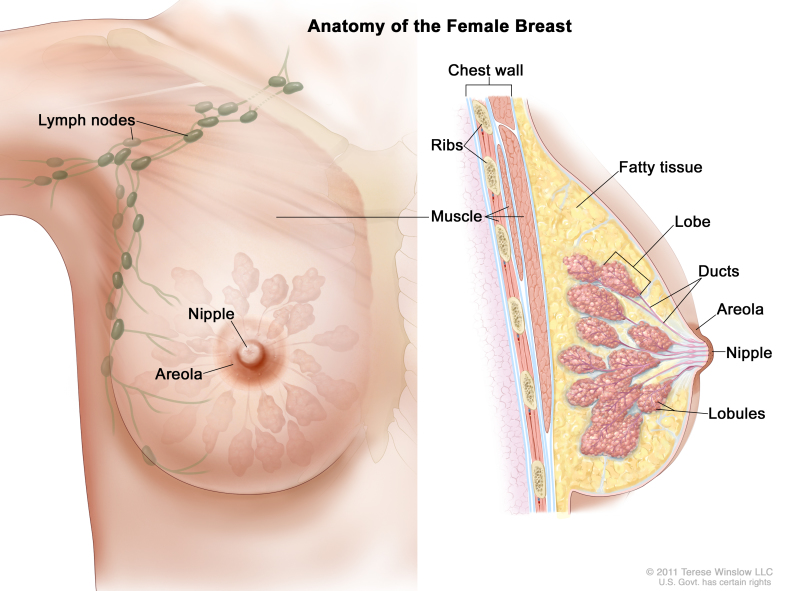
The breast is made up of lobes and ducts. Each breast has 15 to 20 sections called lobes, which have many smaller sections called lobules. Lobules end in dozens of tiny bulbs that can produce milk. The lobes, lobules, and bulbs are linked by thin tubes called ducts.
Anatomy of the female breast. The nipple and areola are shown on the outside of the breast. The lymph nodes, lobes, lobules, ducts, and other parts of the inside of the breast are also shown.
Each breast also contains blood vessels and lymph vessels. The lymph vessels carry an almost colorless fluid called lymph. Lymph vessels lead to organs called lymph nodes. Lymph nodes are small bean-shaped structures that are found throughout the body. They filter substances in lymph and help fight infection and disease. Clusters of lymph nodes are found near the breast in the axilla (under the arm), above the collarbone, and in the chest.
See the following PDQ summaries for more information about breast cancer:
Breast cancer is the second leading cause of death from cancer in American women.
Women in the United States get breast cancer more than any other type of cancer except for skin cancer. Breast cancer is second only to lung cancer as a cause of cancer death in women.
Breast cancer occurs more often in white women than in black women. However, black women are more likely than white women to die from the disease.
Breast cancer occurs in men also, but the number of cases is small.
Different factors increase or decrease the risk of breast cancer.
Anything that increases your chance of getting a disease is called a risk factor. Anything that decreases your chance of getting a disease is called a protective factor.
For information about risk factors and protective factors for breast cancer, see the PDQ summary on Breast Cancer Prevention.
Breast Cancer Screening
Key Points for This Section
Tests are used to screen for different types of cancer.
Some screening tests are used because they have been shown to be helpful both in finding cancers early and in decreasing the chance of dying from these cancers. Other tests are used because they have been shown to find cancer in some people; however, it has not been proven in clinical trials that use of these tests will decrease the risk of dying from cancer.
Scientists study screening tests to find those with the fewest risks and most benefits. Cancer screening trials also are meant to show whether early detection (finding cancer before it causes symptoms) decreases a person’s chance of dying from the disease. For some types of cancer, the chance of recovery is better if the disease is found and treated at an early stage.
Clinical trials that study cancer screening methods are taking place in many parts of the country. Information about ongoing clinical trials is available from the NCI website.
Three tests are used by health care providers to screen for breast cancer:
Mammogram
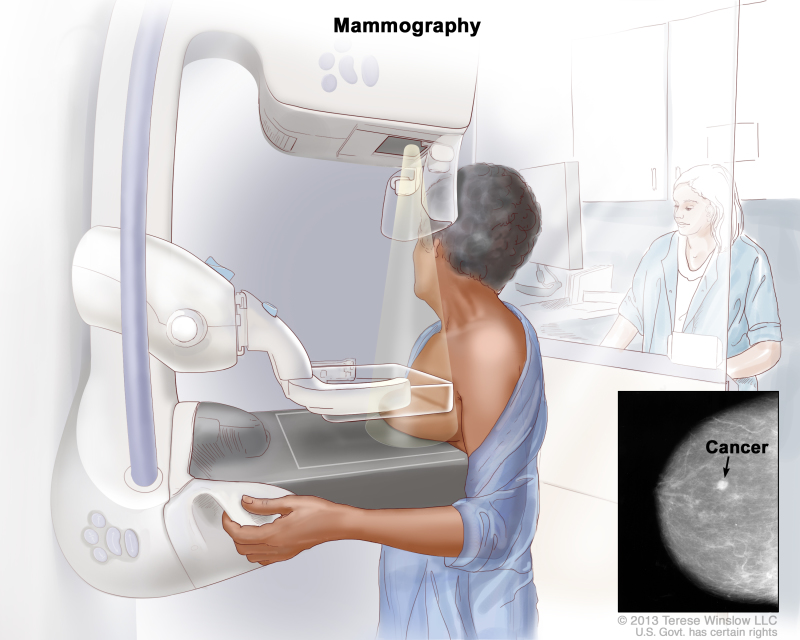
Mammography is the most common screening test for breast cancer. A mammogram is an x-ray of the breast. This test may find tumors that are too small to feel. A mammogram may also find ductal carcinoma in situ (DCIS). In DCIS, there are abnormal cells in the lining of a breast duct, which may become invasive cancer in some women.
Mammograms are less likely to find breast tumors in women younger than 50 years than in older women. This may be because younger women have denser breast tissue that appears white on a mammogram. Because tumors also appear white on a mammogram, they can be harder to find when there is dense breast tissue.
Mammography. The breast is pressed between two plates. X-rays are used to take pictures of breast tissue.
The following may affect whether a mammogram is able to detect (find) breast cancer:
- The size of the tumor.
- How dense the breast tissue is.
- The skill of the radiologist.
Women aged 40 to 74 years who have screening mammograms have a lower chance of dying from breast cancer than women who do not have screening mammograms.
Clinical breast exam (CBE)
A clinical breast exam is an exam of the breast by a doctor or other health professional. The doctor will carefully feel the breasts and under the arms for lumps or anything else that seems unusual. It is not known if having clinical breast exams decreases the chance of dying from breast cancer.
Breast self-exams may be done by women or men to check their breasts for lumps or other changes. It is important to know how your breasts usually look and feel. If you feel any lumps or notice any other changes, talk to your doctor. Doing breast self-exams has not been shown to decrease the chance of dying from breast cancer.
MRI (magnetic resonance imaging) in women with a high risk of breast cancer
MRI is a procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). MRI does not use any x-rays.
MRI is used as a screening test for women who have one or more of the following:
- Certain gene changes, such as in the BRCA1 or BRCA2 genes.
- A family history (first degree relative, such as a mother, daughter or sister) with breast cancer.
MRIs find breast cancer more often than mammograms do, but it is common for MRI results to appear abnormal even when there isn't any cancer.
Other screening tests are being studied in clinical trials.
Thermography
Thermography is a procedure in which a special camera that senses heat is used to record the temperature of the skin that covers the breasts. A computer makes a map of the breast showing the changes in temperature. Tumors can cause temperature changes that may show up on the thermogram.
There have been no clinical trials of thermography to find out how well it detects breast cancer or if having the procedure decreases the risk of dying from breast cancer.
Tissue sampling
Breast tissue sampling is taking cells from breast tissue to check under a microscope. Abnormal cells in breast fluid have been linked to an increased risk of breast cancer in some studies. Scientists are studying whether breast tissue sampling can be used to find breast cancer at an early stage or predict the risk of developing breast cancer. Three ways of taking tissue samples are being studied:
- Fine-needle aspiration: A thin needle is inserted into the breast tissue around the areola (darkened area around the nipple) to take out a sample of cells and fluid.
- Nipple aspiration: The use of gentle suction to collect fluid through the nipple. This is done with a device similar to the breast pumps used by women who are breast-feeding.
- Ductal lavage: A hair-size catheter (tube) is inserted into the nipple and a small amount of salt water is released into the duct. The water picks up breast cells and is removed.
Risks of Breast Cancer Screening
Key Points for This Section
Screening tests have risks.
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying from cancer.
The risks of breast cancer screening tests include the following:
Finding breast cancer may not improve health or help a woman live longer.
Screening may not help you if you have fast-growing breast cancer or if it has already spread to other places in your body. Also, some breast cancers found on a screening mammogram may never cause symptoms or become life-threatening. Finding these cancers is called overdiagnosis. When such cancers are found, treatment would not help you live longer and may instead cause serious side effects. At this time, it is not possible to be sure which breast cancers found by screening will cause problems and which ones will not.
False-negative test results can occur.
Screening test results may appear to be normal even though breast cancer is present. A woman who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if she has symptoms.
One in 5 cancers may be missed by mammography. False-negative results occur more often in younger women than in older women because the breast tissue of younger women is more dense. The chance of a false-negative result is also affected by the following:
- The size of the tumor.
- The rate of tumor growth.
- The skill of the radiologist.
False-positive test results can occur.
Screening test results may appear to be abnormal even though no cancer is present. A false-positive test result (one that shows there is cancer when there really isn’t) is usually followed by more tests (such as biopsy), which also have risks.
When a breast biopsy result is abnormal, getting a second opinion from a different pathologist may improve the accuracy of a breast cancer diagnosis.
Most abnormal test results turn out not to be cancer. False-positive results are more common in the following:
- Younger women.
- Women who have had previous breast biopsies.
- Women with a family history of breast cancer.
- Women who take hormones, such as estrogen and progestin.
False-positive results are more likely the first time a screening mammogram is done than with later screenings. Being able to compare a current mammogram with a past mammogram lowers the risk of a false-positive result.
The skill of the radiologist also can affect the chance of a false-positive result.
Anxiety from additional testing may result from false positive results.
False-positive results from screening mammograms are usually followed by more testing that can lead to anxiety. In one study, women who had a false-positive screening mammogram followed by more testing reported feeling anxiety 3 months later, even though cancer was not diagnosed. However, several studies show that women who feel anxiety after false-positive test results are more likely to schedule regular breast screening exams in the future.
Mammograms expose the breast to radiation.
Being exposed to radiation is a risk factor for breast cancer. The risk of breast cancer from radiation exposure is higher in women who received radiation before age 30 and at high doses. For women older than 40 years, the benefits of an annual screening mammogram may be greater than the risks from radiation exposure.
There may be pain or discomfort during a mammogram.
During a mammogram, the breast is placed between 2 plates that are pressed together. Pressing the breast helps to get a better x-ray of the breast. Some women have pain or discomfort during a mammogram.
The risks and benefits of screening for breast cancer may be different in different age groups.
The benefits of breast cancer screening may vary among age groups:
- In women who are expected to live 5 years or fewer, finding and treating early stage breast cancer may reduce their quality of life without helping them live longer.
- As with other women, in women older than 65 years, the results of a screening test may lead to more diagnostic tests and anxiety while waiting for the test results. Also, the breast cancers found are usually not life-threatening.
- It has not been shown that women with an average risk of developing breast cancer benefit from starting screening mammography before age 40.
Women who have had radiation treatment to the chest, especially at a young age, are advised to have routine breast cancer screening. Yearly MRI screening may begin 8 years after treatment or by age 25 years, whichever is later. The benefits and risks of mammograms and MRIs for these women have not been studied.
There is no information on the benefits or risks of breast cancer screening in men.
No matter how old you are, if you have risk factors for breast cancer you should ask for medical advice about when to begin having breast cancer screening tests and how often to have them.
Talk to your doctor about your risk of breast cancer and your need for screening tests.
Talk to your doctor or other health care provider about your risk of breast cancer, whether a screening test is right for you, and the benefits and harms of the screening test. You should take part in the decision about whether you want to have a screening test, based on what is best for you. (See the PDQ summary on Cancer Screening Overview for more information.)
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about breast cancer screening. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials are listed in PDQ and can be found online at NCI's website. Many cancer doctors who take part in clinical trials are also listed in PDQ. For more information, call the Cancer Information Service 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Breast Cancer Screening. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/breast/patient/breast-screening-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389160]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 2,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
- Review Breast Cancer Prevention (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Breast Cancer Prevention (PDQ®): Patient Version.PDQ Screening and Prevention Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Neuroblastoma Screening (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Neuroblastoma Screening (PDQ®): Patient Version.PDQ Screening and Prevention Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Thyroid Cancer Screening (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Thyroid Cancer Screening (PDQ®): Patient Version.PDQ Screening and Prevention Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Prostate Cancer Screening (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Prostate Cancer Screening (PDQ®): Patient Version.PDQ Screening and Prevention Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Colorectal Cancer Screening (PDQ®): Patient Version.[PDQ Cancer Information Summari...]Review Colorectal Cancer Screening (PDQ®): Patient Version.PDQ Screening and Prevention Editorial Board. PDQ Cancer Information Summaries. 2002
- Breast Cancer Screening (PDQ®) - PDQ Cancer Information SummariesBreast Cancer Screening (PDQ®) - PDQ Cancer Information Summaries
- Ovarian, Fallopian Tube, and Primary Peritoneal Cancer Screening (PDQ®) - PDQ Ca...Ovarian, Fallopian Tube, and Primary Peritoneal Cancer Screening (PDQ®) - PDQ Cancer Information Summaries
- Prostate Cancer Treatment (PDQ®) - PDQ Cancer Information SummariesProstate Cancer Treatment (PDQ®) - PDQ Cancer Information Summaries
- Laetrile/Amygdalin (PDQ®) - PDQ Cancer Information SummariesLaetrile/Amygdalin (PDQ®) - PDQ Cancer Information Summaries
- Childhood Bladder Cancer Treatment - PDQ Cancer Information SummariesChildhood Bladder Cancer Treatment - PDQ Cancer Information Summaries
Your browsing activity is empty.
Activity recording is turned off.
See more...