NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-.

PDQ Cancer Information Summaries [Internet].
Show detailsThis PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood astrocytomas. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions.
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
General Information About Childhood Astrocytomas
Primary brain tumors, including astrocytomas, are a diverse group of diseases that together constitute the most common solid tumors of childhood. Brain tumors are classified according to histology and molecular features, but tumor location and extent of spread are also important factors that affect treatment and prognosis. Immunohistochemical analysis, cytogenetic and molecular genetic findings, and measures of mitotic activity are used in tumor diagnosis and classification.
Gliomas are thought to arise from glial precursor cells that are present in the brain and spinal cord. Gliomas are named according to their presumed clinicopathologic and histologic subtype. Astrocytoma is the most commonly diagnosed type of glioma in children.
According to the World Health Organization (WHO) classification of brain tumors, gliomas are classified further as low-grade (grades I and II) or high-grade (grades III and IV) tumors. Children with low-grade tumors have a relatively favorable prognosis, especially when the tumors can be completely resected. Children with high-grade tumors generally have a less favorable prognosis, but this is somewhat dependent on subtype.
The PDQ childhood brain tumor treatment summaries are organized primarily according to the WHO classification of nervous system tumors.[1,2] For a full description of the classification of nervous system tumors and a link to the corresponding treatment summary for each type of brain tumor, refer to the PDQ summary on Childhood Brain and Spinal Cord Tumors Treatment Overview.
Anatomy
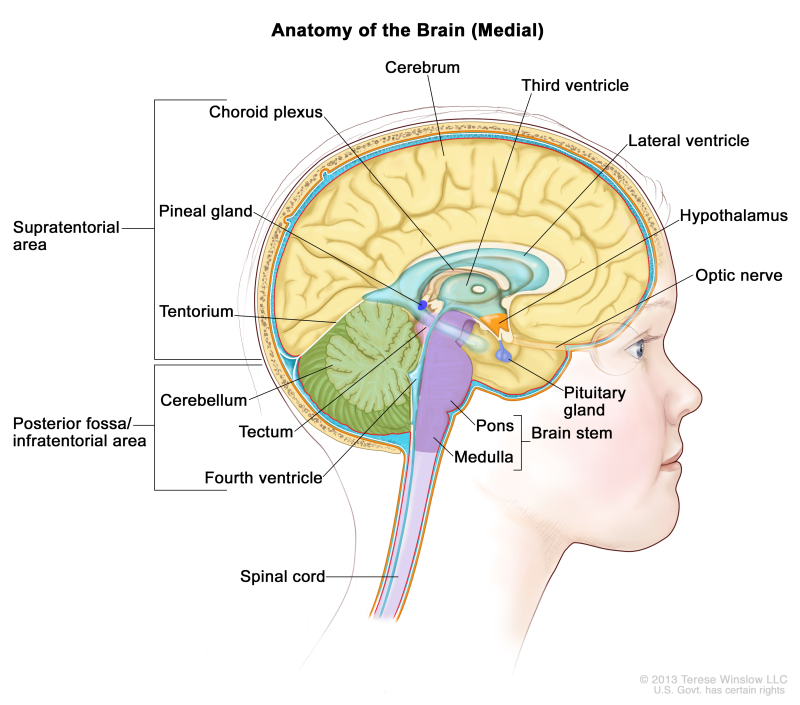
Childhood astrocytomas can occur anywhere in the central nervous system (CNS) (refer to the Figure). Refer to Table 3 for the most common CNS location for each tumor type.
Clinical Features
Presenting symptoms for childhood astrocytomas depend on the following:
- CNS location.
- Size of the tumor.
- Rate of tumor growth.
- Chronologic and developmental age of the child.
In infants and young children, low-grade astrocytomas presenting in the hypothalamus may result in diencephalic syndrome, which is manifested by failure to thrive in an emaciated, seemingly euphoric child. Such children may have little in the way of other neurologic findings, but can have macrocephaly, intermittent lethargy, and visual impairment.[3]
Diagnostic Evaluation
The diagnostic evaluation for astrocytoma includes magnetic resonance imaging (MRI) of the brain or spine. For brain primary tumors, spinal MRI is usually performed in conjunction with the initial brain MRI to exclude neuraxis metastases.
Lumbar punctures examining the cerebrospinal fluid for circulating tumor cells are not commonly performed in children with this disease.
Clinicopathologic Classification of Childhood Astrocytomas and Other Tumors of Glial Origin
The pathologic classification of pediatric brain tumors is a specialized area that is evolving. Examination of the diagnostic tissue by a neuropathologist who has particular expertise in this area is strongly recommended.
Tumor types are based on the putative glial cell type of origin, as follows:
- Astrocytomas (astrocytes).
- Oligodendroglial tumors (oligodendrocytes).
- Mixed gliomas (cell types of origin include oligodendrocytes, astrocytes, and ependymal cells).
- Mixed neuronal-glial tumors.
WHO histologic grade for astrocytic tumors
According to the WHO histologic typing of CNS tumors, childhood astrocytomas and other tumors of glial origin are classified according to clinicopathologic and histologic subtype and are graded (grade I to IV).[1]
WHO histologic grades are commonly referred to as low-grade gliomas or high-grade gliomas (refer to Table 1).
Table 1. World Health Organization (WHO) Histologic Grade and Corresponding Classification for Tumors of the Central Nervous System
| WHO Histologic Grade | Grade Classification |
|---|---|
| I | Low grade |
| II | Low grade |
| III | High grade |
| IV | High grade |
The 2016 WHO criteria began to utilize molecular data in the diagnosis of some tumors because of the accumulation of published evidence that tumor behavior is typically driven by common biological alterations (refer to Table 2). Within glial CNS tumors, this was most evident in changes in the classification of the diffuse gliomas, which were grouped together based on genetic driver mutations rather than histopathological similarities.[2] Two types of diffuse gliomas are no longer considered distinct entities: fibrillary astrocytoma and protoplasmic astrocytoma. Epithelioid glioblastoma is a new, provisionally included variant that is categorized as one subtype of IDH–wild-type glioblastoma.
Table 2. 2016 World Health Organization (WHO) Classification and Histologic Grade of Astrocytic Tumorsa
| Type | WHO Histologic Grade |
|---|---|
| Diffuse Astrocytic Tumors: | |
| —Diffuse astrocytoma, IDH-mutant | II |
| —Anaplastic astrocytoma, IDH-mutant | III |
| —Glioblastoma, IDH–wild-type | IV |
| —Glioblastoma, IDH-mutant | IV |
| —Diffuse midline glioma, H3 K27M-mutant | IV |
| Other Astrocytic Tumors: | |
| —Pilocytic astrocytoma | I |
| —Pilomyxoid astrocytoma | Grade uncertainb |
| —Pleomorphic xanthoastrocytoma | II |
| —Anaplastic pleomorphic xanthoastrocytoma | III |
| —Subependymal giant cell astrocytoma | I |
| Other Gliomas: | |
| —Angiocentric glioma | I |
| —Choroid glioma of the third ventricle | II |
| —Astroblastoma | Grade uncertain |
aAdapted from Louis et al.[2]
bIn 2007, the WHO determined that the pilomyxoid variant of pilocytic astrocytoma may be an aggressive variant that is more likely to disseminate, and it was reclassified as a grade II tumor.[1,2,4,5] In 2016, the WHO suggested not grading the pilomyxoid variant until further studies clarify its behavior.[1,2]
CNS location
Childhood astrocytomas and other tumors of glial origin can occur anywhere in the CNS, although each tumor type tends to have common CNS locations (refer to Table 3).
Table 3. Common Central Nervous System (CNS) Locations for Childhood Astrocytomas and Other Tumors of Glial Origin
| Tumor Type | Common CNS Location |
|---|---|
| Pilocytic astrocytoma | Optic nerve, optic chiasm/hypothalamus, thalamus and basal ganglia, cerebral hemispheres, cerebellum, and brain stem; and spinal cord (rare) |
| Pleomorphic xanthoastrocytoma | Superficial location in cerebrum (temporal lobe preferentially) |
| Diffuse astrocytoma | Cerebrum (frontal and temporal lobes), brain stem, spinal cord, optic nerve, optic chiasm, optic pathway, hypothalamus, and thalamus |
| Anaplastic astrocytoma, glioblastoma | Cerebrum; occasionally cerebellum, brain stem, and spinal cord |
| Diffuse midline glioma, H3 K27M-mutant | Pons, thalamus, spinal cord, and other midline structures |
Cerebellum: More than 80% of astrocytomas located in the cerebellum are low grade (pilocytic grade I) and often cystic; most of the remainder are diffuse grade II astrocytomas. Malignant astrocytomas in the cerebellum are rare.[1,2] The presence of certain histologic features (e.g., MIB-1 rate, anaplasia) has been used retrospectively to predict event-free survival for pilocytic astrocytomas arising in the cerebellum or other locations.[6-8]
Brain stem: Astrocytomas arising in the brain stem may be either high grade or low grade, with the frequency of either type being highly dependent on the location of the tumor within the brain stem.[9,10] Tumors not involving the pons are overwhelmingly low-grade gliomas (e.g., tectal gliomas of the midbrain), whereas tumors located exclusively in the pons without exophytic components are largely diffuse midline gliomas (e.g., diffuse intrinsic pontine gliomas with the H3 K27M-mutant genotype).[9,10] (Refer to the PDQ summary on Childhood Brain Stem Glioma Treatment for more information.)
Cerebrum: High-grade astrocytomas are often locally invasive and extensive and tend to occur above the tentorium in the cerebrum.[11] Spread via the subarachnoid space may occur. Metastasis outside of the CNS has been reported but is extremely infrequent until multiple local relapses have occurred.
Gliomatosis cerebri is no longer considered a distinct entity, but rather to be a growth pattern found in some diffuse astrocytic tumors and, occasionally, oligodendroglial tumors. The growth pattern encompasses widespread involvement of the cerebral hemispheres, often extending caudally to affect the brain stem, cerebellum, and/or spinal cord.[1] This pattern rarely arises in the cerebellum and spreads rostrally.[12] Patients with gliomatosis cerebri may respond to treatment initially, but overall have a poor prognosis.[13]
Neurofibromatosis type 1 (NF1)
Children with NF1 have an increased propensity to develop WHO grade I and grade II astrocytomas in the visual (optic) pathway; as many as 20% of all patients with NF1 will develop an optic pathway glioma. In these patients, the tumor may be found on screening evaluations when the child is asymptomatic or has apparent static neurologic and/or visual deficits.
Pathologic confirmation is frequently not obtained in asymptomatic patients; when biopsies have been performed, these tumors have been found to be predominantly pilocytic (grade I) rather than diffuse astrocytic tumors.[2,5,14]
In general, treatment is not required for incidental tumors found with surveillance neuroimaging. Symptomatic lesions, often causing vision impairment, or those that have radiographically progressed may require treatment.[15]
Tuberous sclerosis
Patients with tuberous sclerosis have a predilection for low-grade glioma development, especially subependymal giant cell astrocytomas. Mutations in either TSC1 or TSC2 cause pathway alterations that impact the mammalian target of rapamycin (mTOR) pathway, leading to increases in proliferation. Subependymal giant cell astrocytomas have been sensitive to targeted approaches via inhibition of the mTOR pathway.[16]
Genomic Alterations
Molecular features of low-grade gliomas
Pilocytic and diffuse astrocytomas
Genomic alterations involving activation of BRAF and the ERK/MAPK pathway are very common in sporadic cases of pilocytic astrocytoma, a type of low-grade glioma.
BRAF-KIAA1549 alterations
BRAF activation in pilocytic astrocytoma occurs most commonly through a BRAF-KIAA1549 gene fusion, producing a fusion protein that lacks the BRAF regulatory domain.[17-21] This fusion is seen in most infratentorial and midline pilocytic astrocytomas, but is present at lower frequency in supratentorial (hemispheric) tumors.[17,18,22-27]
Presence of the BRAF-KIAA1549 fusion predicted a better clinical outcome (progression-free survival [PFS] and overall survival [OS]) in one report that described children with incompletely resected low-grade gliomas.[26] However, other factors such as CDKN2A deletion, whole chromosome 7 gain, and tumor location may modify the impact of the BRAF mutation on outcome.[28]; [29][Level of evidence: 3iiiDiii] Progression to high-grade glioma is rare for pediatric low-grade glioma with the BRAF-KIAA1549 fusion.[30]
BRAF activation through the BRAF-KIAA1549 fusion has also been described in other pediatric low-grade gliomas (e.g., pilomyxoid astrocytoma).[25,26] Other genomic alterations in pilocytic astrocytomas that can activate the ERK/MAPK pathway (e.g., alternative BRAF gene fusions, RAF1 rearrangements, RAS mutations, and BRAF V600E point mutations) are less commonly observed.[18,20,21,31]
BRAF V600E mutations
BRAF V600E point mutations are occasionally observed in pilocytic astrocytoma; the mutations are also observed in nonpilocytic pediatric low-grade gliomas, including ganglioglioma,[32] desmoplastic infantile ganglioglioma, and approximately two-thirds of pleomorphic xanthoastrocytomas.[33-35]
Studies have observed the following:
- In a retrospective series of more than 400 children with low-grade gliomas, 17% of tumors were BRAF V600E mutant. The 10-year PFS rate was 27% for BRAF V600E–mutant cases, compared with 60% for cases whose tumors did not harbor that mutation. Additional factors associated with this poor prognosis included subtotal resection and CDKN2A deletion.[36] Even in patients who underwent a gross-total resection, recurrence was noted in one-third of these cases, suggesting that BRAF V600E tumors have a more invasive phenotype than do other low-grade glioma variants.
- In a similar analysis, children with diencephalic low-grade astrocytomas with a BRAF V600E mutation had a 5-year PFS rate of 22%, compared with a PFS rate of 52% in children who were BRAF wild-type.[37][Level of evidence: 3iiiDiii]
- The frequency of the BRAF V600E mutation was significantly higher in pediatric low-grade glioma that transformed to high-grade glioma (8 of 18 cases) than was the frequency of the mutation in cases that did not transform to high-grade glioma (10 of 167 cases).[30]
Other mutations
Activating mutations in FGFR1, PTPN11, and in NTRK2 fusion genes have also been identified in noncerebellar pilocytic astrocytomas.[38] In pediatric grade II diffuse astrocytomas, the most common alterations reported (up to 53% of tumors) are rearrangements in the MYB family of transcription factors.[39,40]
Angiocentric gliomas
Angiocentric gliomas typically arise in children and young adults as cerebral tumors presenting with seizures.[2]
Two reports in 2016 identified MYB gene alterations as being present in almost all cases diagnosed as angiocentric glioma, with QKI being the primary fusion partner in cases where fusion-partner testing was possible.[41,42] While angiocentric gliomas most commonly occur supratentorially, brain stem angiocentric gliomas with MYB-QKI fusions have also been reported.[43,44]
Astroblastomas
Astroblastomas are defined histologically as glial neoplasms composed of GFAP-positive cells and contain astroblastic pseudorosettes that often demonstrate sclerosis. Astroblastomas are diagnosed primarily in childhood through young adulthood.[2]
The following studies have described genomic alterations associated with astroblastoma:
- A report describing a molecular classification of CNS primitive neuroectodermal tumors (PNETs) identified an entity termed CNS high-grade neuroepithelial tumor with MN1 alteration (CNS HGNET-MN1) that was characterized by gene fusions involving MN1.[45] Most tumors with a histologic diagnosis of astroblastoma (16 of 23) belonged to this molecularly defined entity.
- A report of 27 histologically defined astroblastomas found that 10 cases had MN1 rearrangements, 7 cases had BRAF rearrangements, and 2 cases had RELA rearrangements.[46] Methylation array analysis showed that the cases with MN1 rearrangements clustered with CNS HGNET-MN1, the BRAF-mutated cases clustered with pleomorphic xanthoastrocytomas, and the RELA cases clustered with ependymomas.
- Genomic evaluation of eight cases of astroblastoma identified four with MN1 alterations. Of the remaining four cases, two had genomic alterations consistent with high-grade glioma and two cases could not be classified on the basis of their molecular characteristics.[47]
- A study described eight cases of astroblastoma. All five cases that underwent fluorescence in situ hybridization analysis showed MN1 rearrangements.[48]
These reports suggest that the histologic diagnosis of astroblastoma encompasses a heterogeneous group of genomically defined entities; astroblastomas with MN1 fusions represent a distinctive subset of histologically diagnosed cases.[49]
Tuberous sclerosis
Most children with tuberous sclerosis have a germline mutation in one of two tuberous sclerosis genes (TSC1/hamartin or TSC2/tuberin). Either of these mutations results in activation of the mammalian target of rapamycin (mTOR) complex 1. These children are at risk of developing subependymal giant cell astrocytomas, cortical tubers, and subependymal nodules. Because subependymal giant cell astrocytomas are driven by mTOR activation, mTOR inhibitors are active agents that can induce tumor regression in children with these tumors.[50]
Molecular features of high-grade gliomas
Pediatric high-grade gliomas, especially glioblastoma multiforme, are biologically distinct from those arising in adults.[51-54]
Subgroups identified using DNA methylation patterns
Pediatric high-grade gliomas can be separated into distinct subgroups on the basis of epigenetic patterns (DNA methylation), and these subgroups show distinguishing chromosome copy number gains/losses and gene mutations in the tumor.[55-57] Particularly distinctive subtypes of pediatric high-grade gliomas are those with recurring mutations at specific amino acids in histone genes, and together these account for approximately one-half of pediatric high-grade gliomas.[57]
The following pediatric high-grade glioma subgroups were identified on the basis of their DNA methylation patterns, and they show distinctive molecular and clinical characteristics:[57]
- The histone K27 mutations: H3.3 (H3F3A) and H3.1 (HIST1H3B and, rarely, HIST1H3C) mutations at K27: The histone K27–mutated cases occur predominantly in middle childhood (median age, approximately 10 years), are almost exclusively midline (thalamus, brain stem, and spinal cord), and carry a very poor prognosis. The 2016 WHO classification groups these cancers into a single entity—diffuse midline glioma, H3 K27M–mutant—although there are clinical and biological distinctions between cases with H3.3 and H3.1 mutations, as described below.[2] These cases can be diagnosed using immunohistochemistry to identify the presence of K27M.
- H3.3K27M: H3.3K27M cases occur throughout the midline and pons, account for approximately 60% of cases in these locations, and commonly present between the ages of 5 and 10 years.[57] The prognosis for H3.3K27M patients is especially poor, with a median survival of less than 1 year; the 2-year survival is less than 5%.[57]
- H3.1K27M: H3.1K27M cases are approximately fivefold less common than H3.3K27M cases. They occur primarily in the pons and present at a younger age than other H3.3K27M cases (median age, 5 years vs. 6–10 years). These cases have a slightly more favorable prognosis than do H3.3K27M cases (median survival, 15 months vs. 11 months). Mutations in ACVR1, which is also the mutation observed in the genetic condition fibrodysplasia ossificans progressiva, are present in a high proportion of H3.1K27M cases.[57-59]
- H3.2K27M: Rarely, K27M mutations are also identified in H3.2 (HIST2H3C) cases.[57]
- H3.3 (H3F3A) mutation at G34: The H3.3G34 subtype presents in older children and young adults (median age, 14–18 years) and arises exclusively in the cerebral cortex.[55,56] H3.3G34 cases commonly have mutations in TP53 and ATRX and show widespread hypomethylation across the whole genome. Patients with H3F3A mutations are at high risk of treatment failure,[60] but the prognosis is not as poor as that of patients with histone 3.1 or 3.3 K27M mutations.[56] O-6-methylguanine-DNA methyltransferase (MGMT) methylation is observed in approximately two-thirds of cases, and aside from the IDH1-mutated subtype (see below), the H3.3G34 subtype is the only pediatric high-grade glioma subtype that demonstrates MGMT methylation rates exceeding 20%.[57]
- IDH1 mutation: IDH1-mutated cases represent a small percentage of pediatric high-grade gliomas (approximately 5%), and pediatric high-grade glioma patients whose tumors have IDH1 mutations are almost exclusively older adolescents (median age in a pediatric population, 16 years) with hemispheric tumors.[57] IDH1-mutated cases often show TP53 mutations, MGMT promoter methylation, and a glioma-CpG island methylator phenotype (G-CIMP).[55,56] Pediatric patients with IDH1 mutations show a more favorable prognosis than do other pediatric glioblastoma multiforme patients; 5-year overall survival (OS) rates exceed 60% for pediatric patients with IDH1 mutations, compared with 5-year OS rates of less than 20% for patients with wild-type IDH1.[57]
- Low-grade glioma–like: A small subset of pediatric brain tumors with the histologic appearance of high-grade gliomas show DNA methylation patterns like those of low-grade gliomas.[56,57] These cases are primarily observed in young patients (median age, 4 years); 10 of 16 infants with a glioblastoma multiforme diagnosis were in the low-grade glioma–like group.[57] The prognosis for these patients is much more favorable than for other pediatric high-grade glioma subtypes.[60] Refer below for additional discussion of glioblastoma multiforme in infants.
Other mutations
Pediatric glioblastoma multiforme high-grade glioma patients whose tumors lack both histone mutations and IDH1 mutations represent approximately 40% of pediatric glioblastoma multiforme cases.[57,61] This is a heterogeneous group, with higher rates of gene amplifications than other pediatric high-grade glioma subtypes. The most commonly amplified genes are PDGFRA, EGFR, CCND/CDK, and MYC/MYCN;[55,56] MGMT promoter methylation rates are low in this group.[61] One report divided this group into three subtypes. The subtype characterized by high rates of MYCN amplification showed the poorest prognosis, while the subtype characterized by TERT promoter mutations and EGFR amplification showed the most favorable prognosis. The third group was characterized by PDGFRA amplification.[61]
Gliomas in infants
Infants and young children with a glioblastoma multiforme diagnosis appear to have tumors with distinctive molecular characteristics when compared with tumors of older children and adults. The application of DNA methylation analysis to pediatric glioblastoma multiforme tumors identified a group of patients (representing approximately 7% of pediatric patients with a histologic diagnosis of glioblastoma multiforme) whose tumors had molecular characteristics consistent with low-grade gliomas. The median age for this group of patients was 1 year, with eight of ten infants showing a low-grade glioma–like profile.[56] The low-grade glioma–like subtype had a favorable prognosis (3-year OS rate, approximately 90%).[56,57] BRAF V600E mutations were observed in 4 of 13 low-grade glioma–like tumors and in 3 of 15 tumors from patients aged 3 years and younger.[56]
A second report investigated gene copy number gains and losses and mutation status of selected genes for glioblastoma multiforme tumors from children younger than 36 months.[62] Molecular alterations observed at appreciable rates in older children (e.g., K27M, CDKN2A loss, PDGFRA amplification, and TERT promoter mutations) were rare in the tumors of these young children, and novel abnormalities (e.g., loss of SNORD on chromosome 14q32) were observed in some cases.
The distinctive molecular characteristics of gliomas arising in infants (aged <12 months) were further defined in a study of 118 infants who had tumor tissue available for genomic characterization.[63] Approximately 75% of the cases were classified as low grade, but the diminished utility of histologic classification in this age group was illustrated by the relatively low OS rate for the low-grade cohort (71%) and the relatively favorable survival for the high-grade cohort (55%). Genomic characterization divided the infant glioma population into the following three groups:
- Group 1 tumors were receptor tyrosine kinase (RTK) driven and primarily high grade (83%). These tumors harbored lesions in ALK, ROS1, NTRK, and MET. Median age at diagnosis was 3 months, and OS rates were approximately 60%.
- Group 2 tumors were RAS/MAPK driven and were all hemispheric low-grade gliomas, representing one-fourth of hemispheric gliomas in infants. BRAF V600E was the most common alteration, followed by FGFR1 alterations and BRAF fusions. This group had a median age at presentation of 8 months and had the most favorable outcome (10-year OS rate, 93%).
- Group 3 tumors were RAS/MAPK driven with low-grade histology and midline presentation (approximately 80% optic pathway/hypothalamic gliomas). Most group 3 tumors showed either BRAF fusions or BRAF V600E. Median age at diagnosis was 7.5 months. The progression-free survival (PFS) rate at 5-years was approximately 20%, and the OS rate at 10 years was approximately 50% (far inferior to that of optic pathway/hypothalamic gliomas in children aged >1 year).
Secondary high-grade glioma
Childhood secondary high-grade glioma (high-grade glioma that is preceded by a low-grade glioma) is uncommon (2.9% in a study of 886 patients). No pediatric low-grade gliomas with the BRAF-KIAA1549 fusion transformed to a high-grade glioma, whereas low-grade gliomas with the BRAF V600E mutations were associated with increased risk of transformation. Seven of 18 patients (approximately 40%) with secondary high-grade glioma had BRAF V600E mutations, with CDKN2A alterations present in 8 of 14 cases (57%).[30]
Neurofibromatosis type 1 (NF1)
High-grade gliomas can arise in children with NF1, although low-grade gliomas are much more common. When a high-grade tumor occurs, it is most often in adulthood. Genomic characterization of 23 patients with NF1-associated high-grade gliomas (median age, 38.8 years) showed higher rates of mutations compared with NF1 patients who had low-grade gliomas (21.5 vs. 6 mutations, respectively).[64] The vast majority of patients showed NF1 germline mutations, with either loss of heterozygosity or with an inactivating mutation in the second NF1 allele. In contrast to NF1-associated low-grade gliomas, genomic alterations associated with high-grade gliomas were common (CDKN2A [58%], ATRX [38%], and TP53 [29%]).[64]
Molecular features of neuronal and mixed neuronal-glial tumors
Neuronal and mixed neuronal-glial tumors are generally low-grade tumors, with an exception of the grade III anaplastic gangliogliomas. The histologies recognized by the 2016 WHO classification include the following:[2]
- Dysembryoplastic neuroepithelial tumor.
- Gangliocytoma.
- Ganglioglioma.
- Anaplastic ganglioglioma.
- Dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease).
- Desmoplastic infantile astrocytoma and ganglioglioma.
- Papillary glioneuronal tumor.
- Rosette-forming glioneuronal tumor.
- Diffuse leptomeningeal glioneuronal tumor.
- Central neurocytoma.
- Extraventricular neurocytoma.
- Cerebellar liponeurocytoma.
- Paraganglioma.
Dysembryoplastic neuroepithelial tumor (DNET)
DNET presents in children and adults, with the median age at diagnosis in mid-to-late adolescence. It is characterized histopathologically by the presence of columns of oligodendroglial-like cells and cortical ganglion cells floating in mucin.[1] The temporal lobe is the most common location, and it is associated with drug-refractory epilepsy.[65,66]
FGFR1 alterations have been reported in 60% to 80% of DNETs, and include FGFR1 activating point mutations, internal tandem duplication of the kinase domain, and activating gene fusions.[42,67,68] BRAF mutations are uncommon in DNET.
DNET of the septum pellucidum
Septal DNET generally presents with symptoms related to obstructive hydrocephalus.[69,70] Septal DNET has an indolent clinical behavior, with most tumors not requiring treatment other than surgery. In a single-institution series that incorporated other literature-reported cases, the median age at presentation was in the adolescent age range.[71]
Mutations that are common in low-grade gliomas (e.g., BRAF V600E) and in cortical DNETs (FGFR1 mutations) are uncommon in septal DNET.[70-72] Instead, mutations in PDGFRA at the K385 residue typify most cases of septal DNET.
A report of the molecular characterization of 18 septal DNETs showed that 14 had a PDGFRA mutation, with all but one being a mutation at the K385 residue,[71] which is in the extracellular region of PDGFRA that mediates the receptor-receptor interaction required for dimerization and activation upon binding of PDGFs. Among the remaining four cases, three had FGFR1 mutations in line with those observed in cortical DNET. A second report observed PDGFRA mutations at K385 in each of four cases of septal DNET.[72] Combined, the two reports indicate that septal DNET is a distinct entity characterized by a stereotypic anatomic location and, in most cases, a PDGFRA mutation. Low-grade glioneuronal tumors with the K385 PDGFRA mutation have also been identified as arising in the corpus callosum and periventricular white matter of the lateral ventricle, leading to the proposal that myxoid glioneuronal tumor, PDGFRA p.K385-mutant be considered as a distinct central nervous system (CNS) tumor entity.[73]
Ganglioglioma
Ganglioglioma presents during childhood and into adulthood. It most commonly arises in the cerebral cortex and is associated with seizures, but also presents in other sites, including the spinal cord.[65,74]
The unifying theme for the molecular pathogenesis of ganglioglioma is genomic alterations leading to MAPK pathway activation.[42,75] BRAF alterations are observed in approximately 50% of ganglioglioma cases, with V600E being by far the most common alteration; however, other BRAF mutations and gene fusions are also observed. Other less commonly altered genes in ganglioglioma include KRAS, FGFR1/2, RAF1, NTRK2, and NF1.[42,75]
Desmoplastic infantile astrocytomas (DIA) and desmoplastic infantile gangliogliomas (DIG)
DIA and DIG most often present in the first year of life and show a characteristic imaging appearance in which a contrast-enhancing solid nodule accompanies a large cystic component.[76,77] DIG is more common than DIA,[76] and by methylation array analysis, both diagnoses cluster together.[78] Survival outcome is generally favorable with surgical resection.[76]
The most commonly observed genomic alterations in DIA and DIG are BRAF mutations involving V600; gene fusions involving kinase genes are observed less frequently.
- Among 16 cases confirmed by histology and DNA methylation profiling to be DIA and DIG, BRAF mutations were observed in seven cases (43.8%): four BRAF V600E mutations and three BRAF V600D mutations. One additional case had an EML4-ALK fusion. BRAF mutations were present in 4 of 12 (25%) DIG cases (with 3 of 4 mutated cases having BRAF V600D) and in 3 of 4 (75%) DIA cases (all 3 mutated cases with BRAF V600E).
- A study of seven DIG cases found MAPK pathway alterations in four (57%).[79] Three alterations involved BRAF (V600E, V600D, and one deletion/insertion centered at V600) and one was a TPM3-NTRK1 in-frame fusion. Notably, the variant allele frequency was low (8%–27%), suggesting that DIG is characterized by a prominent nonneoplastic component resulting in low clonal driver mutation allele frequencies.
- Another report also described the BRAF V600D mutation in a DIG case.[80] As the V600D mutation is far less common than V600E in other cancers, its detection in multiple DIG cases suggests an association between the mutation and DIG.
Papillary glioneuronal tumor
Papillary glioneuronal tumor is a low-grade biphasic neoplasm with astrocytic and neuronal differentiation that primarily arises in the supratentorial compartment.[2] The median age at presentation is in the early 20s, but it can be observed during childhood through adulthood.
The primary genomic alteration associated with papillary glioneuronal tumor is a gene fusion, SLC44A1-PRKCA, that is associated with the t(9:17)(q31;q24) translocation.[81,82] In one study of 28 cases diagnosed histologically as papillary glioneuronal tumor using methylation arrays, 11 of the cases clustered in a distinctive methylation class, while the remaining cases showed methylation profiles typical for other tumor entities. Molecular analysis of the cases in the distinctive methylation cluster showed that all of them had the SLC44A1-PRKCA gene fusion except for a single case with a NOTCH1-PRKCA gene fusion.[83] This suggests that molecular methods for identifying the presence of a PRKCA fusion are less susceptible to misclassification in diagnosing papillary glioneuronal tumor than are morphology-based methods.
Rosette-forming glioneuronal tumor (RGNT)
RGNT presents in adolescents and adults, with tumors generally located infratentorially, although tumors can arise in mesencephalic or diencephalic regions.[84] The typical histological appearance shows both a glial component and a neurocytic component arranged in rosettes or perivascular pseudorosettes.[2] Outcome for patients with RGNT is generally favorable, consistent with the WHO grade I designation.[84]
DNA methylation profiling shows that RGNT has a distinct epigenetic profile that distinguishes it from other low-grade glial/glioneuronal tumor entities.[84] A study of 30 cases of RGNT observed FGFR1 hotspot mutations in all analyzed tumors.[84] In addition, PIK3CA activating mutations were concurrently observed in 19 of 30 cases (63%). Missense or damaging mutations in NF1 were identified in 10 of 30 cases (33%), with 7 tumors having mutations in FGFR1, PIK3CA, and NF1. The co-occurrence of mutations that activate both the MAPK pathway and the PI3K pathway makes the mutation profile of RGNT distinctive among astrocytic and glioneuronal tumors.
Diffuse leptomeningeal glioneuronal tumor (DLGNT)
DLGNT is a rare CNS tumor that has been characterized radiographically by leptomeningeal enhancement on magnetic resonance imaging (MRI) that may involve the posterior fossa, brain stem region, and spinal cord.[85] Intraparenchymal lesions, when present, typically involve the spinal cord;[85] localized intramedullary glioneuronal tumors without leptomeningeal dissemination and with histomorphologic, immunophenotypic, and genomic characteristics similar to DLGNT have been reported.[86]
DLGNT showed a distinctive epigenetic profile on DNA methylation arrays, and unsupervised clustering of array data applied to 30 cases defined two subclasses of DLGNT: methylation class (MC)-1 (n = 17) and MC-2 (n = 13).[85] Of note, many of the array-defined cases had originally been diagnosed as other entities (e.g., primitive neuroectodermal tumors, pilocytic astrocytoma, and anaplastic astrocytoma). Patients with DLGNT-MC-1 were diagnosed at an earlier age than were patients with DLGNT-MC-2 (5 years vs. 14 years, respectively). The 5-year overall survival rate was higher for patients with DLGNT-MC-1 than for those with DLGNT-MC-2 (100% vs. 43%, respectively). Genomic findings from the 30 methylation array–defined DLGNT cases are provided below:
- All 30 cases showed loss of chromosome 1p, but only 6 of 17 DLGNT-MC-1 cases showed additional gain of chromosome 1q, compared with all cases of DLGNT-MC-2.[85] A separate report found that chromosome 1q gain was an adverse prognostic factor in patients with DLGNT (including cases with localized disease),[87] which is consistent with the inferior outcome for patients with DLGNT-MC-2.
- Co-deletions of 1p/19q were more frequent in the DLGNT-MC-1 group (7 of 13, 54%) than in the DLGNT-MC-2 group (2 of 13, 15%). In contrast to oligodendroglioma, mutations of IDH1 and IDH2 were not identified.[85]
- MAPK pathway activation is common in DLGNT cases.[85] The KIAA1549-BRAF fusion was present in 11 of 15 DLGNT-MC-1 cases (65%) and in 9 of 13 DLGNT-MC-2 cases (69%). Fusions involving NTRK1/2/3 were present in one case each, and another case had a TRIM33-RAF1 fusion.
Extraventricular neurocytoma
Extraventricular neurocytoma is histologically similar to central neurocytoma, consisting of small uniform cells that demonstrate neuronal differentiation, but it arises in the brain parenchyma rather than in association with the ventricular system.[2] It presents during childhood through adulthood.
In a study of 40 tumors histologically classified as extraventricular neurocytoma and subjected to methylation array analysis, only 26 formed a separate cluster distinctive from reference tumors of other histologies.[88] Among cases with an extraventricular neurocytoma methylation array classification for which genomic characterization could be performed, 11 of 15 (73%) showed rearrangements affecting members of the FGFR family, with FGFR1-TACC1 being the most common alteration.[88]
Prognosis
Low-grade astrocytomas
Low-grade astrocytomas (grade I [pilocytic] and grade II) have a relatively favorable prognosis, particularly for well-circumscribed lesions where complete excision may be possible.[11,89-92] Tumor spread, when it occurs, is usually by contiguous extension; dissemination to other CNS sites is uncommon, but does occur.[93,94] Although metastasis is uncommon, tumors may be of multifocal origin, especially when associated with NF1.
Unfavorable prognostic features for childhood low-grade astrocytomas include the following:[95-98]
- Young age.[98]
- Diffuse histology, especially IDH mutant.
- Inability to obtain a complete resection.
- Diencephalic syndrome.[98]
- Metastases. When metastasis does occur, it is associated with a poorer long-term outcome.[99] However, it is increasingly evident that prognosis is largely dependent on specific molecular features integrated with standard pathological grouping.
In patients with pilocytic astrocytoma, elevated MIB-1 labeling index, a marker of cellular proliferative activity, is associated with shortened PFS.[8] A BRAF-KIAA1549 fusion, found in pilocytic tumors, confers a better clinical outcome.[26]
In children with tumors of the visual pathway, outcome is not only assessed by radiographic disease control or survival but also by visual outcome. Children with isolated optic nerve tumors have a better prognosis than do children with lesions that involve the chiasm or that extend along the optic pathway.[100,101]; [102][Level of evidence: 3iiC] Children with NF1 also have a better prognosis, especially when the tumor is found in asymptomatic patients at the time of screening.[103] Better visual acuity at diagnosis, older age at diagnosis, and presence of NF1 are associated with better visual outcomes.[104]
High-grade astrocytomas
Although high-grade astrocytomas generally carry a poor prognosis in younger patients, those with anaplastic astrocytomas in whom a gross-total resection is possible may fare better,[90,105,106] as well as those with non-H3 K27M–mutant tumors.
Molecular subtypes of pediatric glioblastoma multiforme show prognostic significance.[56] Patients whose tumors have histone K27M mutations have the poorest prognosis, with 3-year survival rates below 5%. In the thalamus, wild-type high-grade gliomas have a somewhat better prognosis than do those harboring an H3.3 mutation. For high-grade gliomas in the thalamus, patients with H3 wild-type tumors have a somewhat better prognosis (2-year overall survival [OS], 71%) than do patients who harbor H3 K27M mutations (2-year OS, 13%).[107] Patients whose tumors have IDH1 mutations appear to have the most favorable prognosis among pediatric glioblastoma multiforme cases, while those with histone G34 mutations and those lacking both histone and IDH1 mutations have an intermediate prognosis (3-year OS, approximately 30%). In a multivariate analysis that included both molecular and clinical factors, the presence of gene amplifications and K27M mutations were associated with a poorer prognosis, while the presence of IDH1 mutations was associated with a more favorable prognosis.[56]
References
- Louis DN, Ohgaki H, Wiestler OD: WHO Classification of Tumours of the Central Nervous System. 4th rev.ed. Lyon, France: IARC Press, 2016.
- Louis DN, Perry A, Reifenberger G, et al.: The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131 (6): 803-20, 2016. [PubMed: 27157931]
- Kilday JP, Bartels U, Huang A, et al.: Favorable survival and metabolic outcome for children with diencephalic syndrome using a radiation-sparing approach. J Neurooncol 116 (1): 195-204, 2014. [PubMed: 24218181]
- Louis DN, Ohgaki H, Wiestler OD, et al., eds.: WHO Classification of Tumours of the Central Nervous System. 4th ed. Lyon, France: IARC Press, 2007.
- Komotar RJ, Burger PC, Carson BS, et al.: Pilocytic and pilomyxoid hypothalamic/chiasmatic astrocytomas. Neurosurgery 54 (1): 72-9; discussion 79-80, 2004. [PubMed: 14683543]
- Tibbetts KM, Emnett RJ, Gao F, et al.: Histopathologic predictors of pilocytic astrocytoma event-free survival. Acta Neuropathol 117 (6): 657-65, 2009. [PubMed: 19271226]
- Rodriguez FJ, Scheithauer BW, Burger PC, et al.: Anaplasia in pilocytic astrocytoma predicts aggressive behavior. Am J Surg Pathol 34 (2): 147-60, 2010. [PubMed: 20061938]
- Margraf LR, Gargan L, Butt Y, et al.: Proliferative and metabolic markers in incompletely excised pediatric pilocytic astrocytomas--an assessment of 3 new variables in predicting clinical outcome. Neuro Oncol 13 (7): 767-74, 2011. [PMC free article: PMC3129272] [PubMed: 21653594]
- Fried I, Hawkins C, Scheinemann K, et al.: Favorable outcome with conservative treatment for children with low grade brainstem tumors. Pediatr Blood Cancer 58 (4): 556-60, 2012. [PubMed: 21618421]
- Fisher PG, Breiter SN, Carson BS, et al.: A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as distinct entities. Cancer 89 (7): 1569-76, 2000. [PubMed: 11013373]
- Pfister S, Witt O: Pediatric gliomas. Recent Results Cancer Res 171: 67-81, 2009. [PubMed: 19322538]
- Rorke-Adams LB, Portnoy H: Long-term survival of an infant with gliomatosis cerebelli. J Neurosurg Pediatr 2 (5): 346-50, 2008. [PubMed: 18976105]
- Armstrong GT, Phillips PC, Rorke-Adams LB, et al.: Gliomatosis cerebri: 20 years of experience at the Children's Hospital of Philadelphia. Cancer 107 (7): 1597-606, 2006. [PubMed: 16955507]
- Allen JC: Initial management of children with hypothalamic and thalamic tumors and the modifying role of neurofibromatosis-1. Pediatr Neurosurg 32 (3): 154-62, 2000. [PubMed: 10867564]
- Molloy PT, Bilaniuk LT, Vaughan SN, et al.: Brainstem tumors in patients with neurofibromatosis type 1: a distinct clinical entity. Neurology 45 (10): 1897-902, 1995. [PubMed: 7477989]
- Franz DN, Weiss BD: Molecular therapies for tuberous sclerosis and neurofibromatosis. Curr Neurol Neurosci Rep 12 (3): 294-301, 2012. [PubMed: 22544507]
- Bar EE, Lin A, Tihan T, et al.: Frequent gains at chromosome 7q34 involving BRAF in pilocytic astrocytoma. J Neuropathol Exp Neurol 67 (9): 878-87, 2008. [PubMed: 18716556]
- Forshew T, Tatevossian RG, Lawson AR, et al.: Activation of the ERK/MAPK pathway: a signature genetic defect in posterior fossa pilocytic astrocytomas. J Pathol 218 (2): 172-81, 2009. [PubMed: 19373855]
- Jones DT, Kocialkowski S, Liu L, et al.: Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res 68 (21): 8673-7, 2008. [PMC free article: PMC2577184] [PubMed: 18974108]
- Jones DT, Kocialkowski S, Liu L, et al.: Oncogenic RAF1 rearrangement and a novel BRAF mutation as alternatives to KIAA1549:BRAF fusion in activating the MAPK pathway in pilocytic astrocytoma. Oncogene 28 (20): 2119-23, 2009. [PMC free article: PMC2685777] [PubMed: 19363522]
- Pfister S, Janzarik WG, Remke M, et al.: BRAF gene duplication constitutes a mechanism of MAPK pathway activation in low-grade astrocytomas. J Clin Invest 118 (5): 1739-49, 2008. [PMC free article: PMC2289793] [PubMed: 18398503]
- Korshunov A, Meyer J, Capper D, et al.: Combined molecular analysis of BRAF and IDH1 distinguishes pilocytic astrocytoma from diffuse astrocytoma. Acta Neuropathol 118 (3): 401-5, 2009. [PubMed: 19543740]
- Horbinski C, Hamilton RL, Nikiforov Y, et al.: Association of molecular alterations, including BRAF, with biology and outcome in pilocytic astrocytomas. Acta Neuropathol 119 (5): 641-9, 2010. [PMC free article: PMC5859320] [PubMed: 20044755]
- Yu J, Deshmukh H, Gutmann RJ, et al.: Alterations of BRAF and HIPK2 loci predominate in sporadic pilocytic astrocytoma. Neurology 73 (19): 1526-31, 2009. [PMC free article: PMC2777068] [PubMed: 19794125]
- Lin A, Rodriguez FJ, Karajannis MA, et al.: BRAF alterations in primary glial and glioneuronal neoplasms of the central nervous system with identification of 2 novel KIAA1549:BRAF fusion variants. J Neuropathol Exp Neurol 71 (1): 66-72, 2012. [PMC free article: PMC4629834] [PubMed: 22157620]
- Hawkins C, Walker E, Mohamed N, et al.: BRAF-KIAA1549 fusion predicts better clinical outcome in pediatric low-grade astrocytoma. Clin Cancer Res 17 (14): 4790-8, 2011. [PubMed: 21610142]
- Becker AP, Scapulatempo-Neto C, Carloni AC, et al.: KIAA1549: BRAF Gene Fusion and FGFR1 Hotspot Mutations Are Prognostic Factors in Pilocytic Astrocytomas. J Neuropathol Exp Neurol 74 (7): 743-54, 2015. [PMC free article: PMC4470527] [PubMed: 26083571]
- Horbinski C, Nikiforova MN, Hagenkord JM, et al.: Interplay among BRAF, p16, p53, and MIB1 in pediatric low-grade gliomas. Neuro Oncol 14 (6): 777-89, 2012. [PMC free article: PMC3367847] [PubMed: 22492957]
- Roth JJ, Fierst TM, Waanders AJ, et al.: Whole Chromosome 7 Gain Predicts Higher Risk of Recurrence in Pediatric Pilocytic Astrocytomas Independently From KIAA1549-BRAF Fusion Status. J Neuropathol Exp Neurol 75 (4): 306-15, 2016. [PMC free article: PMC5009478] [PubMed: 26945035]
- Mistry M, Zhukova N, Merico D, et al.: BRAF mutation and CDKN2A deletion define a clinically distinct subgroup of childhood secondary high-grade glioma. J Clin Oncol 33 (9): 1015-22, 2015. [PMC free article: PMC4356711] [PubMed: 25667294]
- Janzarik WG, Kratz CP, Loges NT, et al.: Further evidence for a somatic KRAS mutation in a pilocytic astrocytoma. Neuropediatrics 38 (2): 61-3, 2007. [PubMed: 17712732]
- López GY, Van Ziffle J, Onodera C, et al.: The genetic landscape of gliomas arising after therapeutic radiation. Acta Neuropathol 137 (1): 139-150, 2019. [PMC free article: PMC6589431] [PubMed: 30196423]
- Dougherty MJ, Santi M, Brose MS, et al.: Activating mutations in BRAF characterize a spectrum of pediatric low-grade gliomas. Neuro Oncol 12 (7): 621-30, 2010. [PMC free article: PMC2940652] [PubMed: 20156809]
- Dias-Santagata D, Lam Q, Vernovsky K, et al.: BRAF V600E mutations are common in pleomorphic xanthoastrocytoma: diagnostic and therapeutic implications. PLoS One 6 (3): e17948, 2011. [PMC free article: PMC3066220] [PubMed: 21479234]
- Schindler G, Capper D, Meyer J, et al.: Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol 121 (3): 397-405, 2011. [PubMed: 21274720]
- Lassaletta A, Zapotocky M, Mistry M, et al.: Therapeutic and Prognostic Implications of BRAF V600E in Pediatric Low-Grade Gliomas. J Clin Oncol 35 (25): 2934-2941, 2017. [PMC free article: PMC5791837] [PubMed: 28727518]
- Ho CY, Mobley BC, Gordish-Dressman H, et al.: A clinicopathologic study of diencephalic pediatric low-grade gliomas with BRAF V600 mutation. Acta Neuropathol 130 (4): 575-85, 2015. [PubMed: 26264609]
- Jones DT, Hutter B, Jäger N, et al.: Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nat Genet 45 (8): 927-32, 2013. [PMC free article: PMC3951336] [PubMed: 23817572]
- Zhang J, Wu G, Miller CP, et al.: Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet 45 (6): 602-12, 2013. [PMC free article: PMC3727232] [PubMed: 23583981]
- Ramkissoon LA, Horowitz PM, Craig JM, et al.: Genomic analysis of diffuse pediatric low-grade gliomas identifies recurrent oncogenic truncating rearrangements in the transcription factor MYBL1. Proc Natl Acad Sci U S A 110 (20): 8188-93, 2013. [PMC free article: PMC3657784] [PubMed: 23633565]
- Bandopadhayay P, Ramkissoon LA, Jain P, et al.: MYB-QKI rearrangements in angiocentric glioma drive tumorigenicity through a tripartite mechanism. Nat Genet 48 (3): 273-82, 2016. [PMC free article: PMC4767685] [PubMed: 26829751]
- Qaddoumi I, Orisme W, Wen J, et al.: Genetic alterations in uncommon low-grade neuroepithelial tumors: BRAF, FGFR1, and MYB mutations occur at high frequency and align with morphology. Acta Neuropathol 131 (6): 833-45, 2016. [PMC free article: PMC4866893] [PubMed: 26810070]
- D'Aronco L, Rouleau C, Gayden T, et al.: Brainstem angiocentric gliomas with MYB-QKI rearrangements. Acta Neuropathol 134 (4): 667-669, 2017. [PMC free article: PMC6556888] [PubMed: 28803398]
- Chan E, Bollen AW, Sirohi D, et al.: Angiocentric glioma with MYB-QKI fusion located in the brainstem, rather than cerebral cortex. Acta Neuropathol 134 (4): 671-673, 2017. [PMC free article: PMC5693679] [PubMed: 28776091]
- Sturm D, Orr BA, Toprak UH, et al.: New Brain Tumor Entities Emerge from Molecular Classification of CNS-PNETs. Cell 164 (5): 1060-72, 2016. [PMC free article: PMC5139621] [PubMed: 26919435]
- Lehman NL, Usubalieva A, Lin T, et al.: Genomic analysis demonstrates that histologically-defined astroblastomas are molecularly heterogeneous and that tumors with MN1 rearrangement exhibit the most favorable prognosis. Acta Neuropathol Commun 7 (1): 42, 2019. [PMC free article: PMC6419470] [PubMed: 30876455]
- Wood MD, Tihan T, Perry A, et al.: Multimodal molecular analysis of astroblastoma enables reclassification of most cases into more specific molecular entities. Brain Pathol 28 (2): 192-202, 2018. [PMC free article: PMC5843525] [PubMed: 28960623]
- Hirose T, Nobusawa S, Sugiyama K, et al.: Astroblastoma: a distinct tumor entity characterized by alterations of the X chromosome and MN1 rearrangement. Brain Pathol 28 (5): 684-694, 2018. [PMC free article: PMC8028274] [PubMed: 28990708]
- Lucas CG, Solomon DA, Perry A: A review of recently described genetic alterations in central nervous system tumors. Hum Pathol 96: 56-66, 2020. [PubMed: 31678207]
- Franz DN, Belousova E, Sparagana S, et al.: Efficacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 381 (9861): 125-32, 2013. [PubMed: 23158522]
- Paugh BS, Qu C, Jones C, et al.: Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J Clin Oncol 28 (18): 3061-8, 2010. [PMC free article: PMC2903336] [PubMed: 20479398]
- Bax DA, Mackay A, Little SE, et al.: A distinct spectrum of copy number aberrations in pediatric high-grade gliomas. Clin Cancer Res 16 (13): 3368-77, 2010. [PMC free article: PMC2896553] [PubMed: 20570930]
- Ward SJ, Karakoula K, Phipps KP, et al.: Cytogenetic analysis of paediatric astrocytoma using comparative genomic hybridisation and fluorescence in-situ hybridisation. J Neurooncol 98 (3): 305-18, 2010. [PubMed: 20052518]
- Pollack IF, Hamilton RL, Sobol RW, et al.: IDH1 mutations are common in malignant gliomas arising in adolescents: a report from the Children's Oncology Group. Childs Nerv Syst 27 (1): 87-94, 2011. [PMC free article: PMC3014378] [PubMed: 20725730]
- Sturm D, Witt H, Hovestadt V, et al.: Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22 (4): 425-37, 2012. [PubMed: 23079654]
- Korshunov A, Ryzhova M, Hovestadt V, et al.: Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Acta Neuropathol 129 (5): 669-78, 2015. [PubMed: 25752754]
- Mackay A, Burford A, Carvalho D, et al.: Integrated Molecular Meta-Analysis of 1,000 Pediatric High-Grade and Diffuse Intrinsic Pontine Glioma. Cancer Cell 32 (4): 520-537.e5, 2017. [PMC free article: PMC5637314] [PubMed: 28966033]
- Buczkowicz P, Hoeman C, Rakopoulos P, et al.: Genomic analysis of diffuse intrinsic pontine gliomas identifies three molecular subgroups and recurrent activating ACVR1 mutations. Nat Genet 46 (5): 451-6, 2014. [PMC free article: PMC3997489] [PubMed: 24705254]
- Taylor KR, Mackay A, Truffaux N, et al.: Recurrent activating ACVR1 mutations in diffuse intrinsic pontine glioma. Nat Genet 46 (5): 457-61, 2014. [PMC free article: PMC4018681] [PubMed: 24705252]
- Mackay A, Burford A, Molinari V, et al.: Molecular, Pathological, Radiological, and Immune Profiling of Non-brainstem Pediatric High-Grade Glioma from the HERBY Phase II Randomized Trial. Cancer Cell 33 (5): 829-842.e5, 2018. [PMC free article: PMC5956280] [PubMed: 29763623]
- Korshunov A, Schrimpf D, Ryzhova M, et al.: H3-/IDH-wild type pediatric glioblastoma is comprised of molecularly and prognostically distinct subtypes with associated oncogenic drivers. Acta Neuropathol 134 (3): 507-516, 2017. [PubMed: 28401334]
- Gielen GH, Gessi M, Buttarelli FR, et al.: Genetic Analysis of Diffuse High-Grade Astrocytomas in Infancy Defines a Novel Molecular Entity. Brain Pathol 25 (4): 409-17, 2015. [PMC free article: PMC8029085] [PubMed: 25231549]
- Guerreiro Stucklin AS, Ryall S, Fukuoka K, et al.: Alterations in ALK/ROS1/NTRK/MET drive a group of infantile hemispheric gliomas. Nat Commun 10 (1): 4343, 2019. [PMC free article: PMC6761184] [PubMed: 31554817]
- D'Angelo F, Ceccarelli M, Tala, et al.: The molecular landscape of glioma in patients with Neurofibromatosis 1. Nat Med 25 (1): 176-187, 2019. [PMC free article: PMC6857804] [PubMed: 30531922]
- Blumcke I, Spreafico R, Haaker G, et al.: Histopathological Findings in Brain Tissue Obtained during Epilepsy Surgery. N Engl J Med 377 (17): 1648-1656, 2017. [PubMed: 29069555]
- Stone TJ, Keeley A, Virasami A, et al.: Comprehensive molecular characterisation of epilepsy-associated glioneuronal tumours. Acta Neuropathol 135 (1): 115-129, 2018. [PMC free article: PMC5756244] [PubMed: 29058119]
- Rivera B, Gayden T, Carrot-Zhang J, et al.: Germline and somatic FGFR1 abnormalities in dysembryoplastic neuroepithelial tumors. Acta Neuropathol 131 (6): 847-63, 2016. [PMC free article: PMC5039033] [PubMed: 26920151]
- Matsumura N, Nobusawa S, Ito J, et al.: Multiplex ligation-dependent probe amplification analysis is useful for detecting a copy number gain of the FGFR1 tyrosine kinase domain in dysembryoplastic neuroepithelial tumors. J Neurooncol 143 (1): 27-33, 2019. [PubMed: 30825062]
- Baisden BL, Brat DJ, Melhem ER, et al.: Dysembryoplastic neuroepithelial tumor-like neoplasm of the septum pellucidum: a lesion often misdiagnosed as glioma: report of 10 cases. Am J Surg Pathol 25 (4): 494-9, 2001. [PubMed: 11257624]
- Gessi M, Hattingen E, Dörner E, et al.: Dysembryoplastic Neuroepithelial Tumor of the Septum Pellucidum and the Supratentorial Midline: Histopathologic, Neuroradiologic, and Molecular Features of 7 Cases. Am J Surg Pathol 40 (6): 806-11, 2016. [PubMed: 26796505]
- Chiang JCH, Harreld JH, Tanaka R, et al.: Septal dysembryoplastic neuroepithelial tumor: a comprehensive clinical, imaging, histopathologic, and molecular analysis. Neuro Oncol 21 (6): 800-808, 2019. [PMC free article: PMC6556860] [PubMed: 30726976]
- Solomon DA, Korshunov A, Sill M, et al.: Myxoid glioneuronal tumor of the septum pellucidum and lateral ventricle is defined by a recurrent PDGFRA p.K385 mutation and DNT-like methylation profile. Acta Neuropathol 136 (2): 339-343, 2018. [PMC free article: PMC7787982] [PubMed: 30006677]
- Lucas CG, Villanueva-Meyer JE, Whipple N, et al.: Myxoid glioneuronal tumor, PDGFRA p.K385-mutant: clinical, radiologic, and histopathologic features. Brain Pathol 30 (3): 479-494, 2020. [PMC free article: PMC7780370] [PubMed: 31609499]
- Becker AJ: Ganglioglioma. In: Louis DN, Ohgaki H, Wiestler OD: WHO Classification of Tumours of the Central Nervous System. 4th rev.ed. Lyon, France: IARC Press, 2016, pp 138-41.
- Pekmezci M, Villanueva-Meyer JE, Goode B, et al.: The genetic landscape of ganglioglioma. Acta Neuropathol Commun 6 (1): 47, 2018. [PMC free article: PMC5992851] [PubMed: 29880043]
- Bianchi F, Tamburrini G, Massimi L, et al.: Supratentorial tumors typical of the infantile age: desmoplastic infantile ganglioglioma (DIG) and astrocytoma (DIA). A review. Childs Nerv Syst 32 (10): 1833-8, 2016. [PubMed: 27659826]
- Trehan G, Bruge H, Vinchon M, et al.: MR imaging in the diagnosis of desmoplastic infantile tumor: retrospective study of six cases. AJNR Am J Neuroradiol 25 (6): 1028-33, 2004 Jun-Jul. [PMC free article: PMC7975656] [PubMed: 15205142]
- Wang AC, Jones DTW, Abecassis IJ, et al.: Desmoplastic Infantile Ganglioglioma/Astrocytoma (DIG/DIA) Are Distinct Entities with Frequent BRAFV600 Mutations. Mol Cancer Res 16 (10): 1491-1498, 2018. [PMC free article: PMC7269191] [PubMed: 30006355]
- Blessing MM, Blackburn PR, Krishnan C, et al.: Desmoplastic Infantile Ganglioglioma: A MAPK Pathway-Driven and Microglia/Macrophage-Rich Neuroepithelial Tumor. J Neuropathol Exp Neurol 78 (11): 1011-1021, 2019. [PubMed: 31562743]
- Greer A, Foreman NK, Donson A, et al.: Desmoplastic infantile astrocytoma/ganglioglioma with rare BRAF V600D mutation. Pediatr Blood Cancer 64 (6): , 2017. [PMC free article: PMC5589269] [PubMed: 27860162]
- Pages M, Lacroix L, Tauziede-Espariat A, et al.: Papillary glioneuronal tumors: histological and molecular characteristics and diagnostic value of SLC44A1-PRKCA fusion. Acta Neuropathol Commun 3: 85, 2015. [PMC free article: PMC4681033] [PubMed: 26671581]
- Bridge JA, Liu XQ, Sumegi J, et al.: Identification of a novel, recurrent SLC44A1-PRKCA fusion in papillary glioneuronal tumor. Brain Pathol 23 (2): 121-8, 2013. [PMC free article: PMC8029478] [PubMed: 22725730]
- Hou Y, Pinheiro J, Sahm F, et al.: Papillary glioneuronal tumor (PGNT) exhibits a characteristic methylation profile and fusions involving PRKCA. Acta Neuropathol 137 (5): 837-846, 2019. [PubMed: 30759284]
- Sievers P, Appay R, Schrimpf D, et al.: Rosette-forming glioneuronal tumors share a distinct DNA methylation profile and mutations in FGFR1, with recurrent co-mutation of PIK3CA and NF1. Acta Neuropathol 138 (3): 497-504, 2019. [PubMed: 31250151]
- Deng MY, Sill M, Chiang J, et al.: Molecularly defined diffuse leptomeningeal glioneuronal tumor (DLGNT) comprises two subgroups with distinct clinical and genetic features. Acta Neuropathol 136 (2): 239-253, 2018. [PubMed: 29766299]
- Chiang JCH, Harreld JH, Orr BA, et al.: Low-grade spinal glioneuronal tumors with BRAF gene fusion and 1p deletion but without leptomeningeal dissemination. Acta Neuropathol 134 (1): 159-162, 2017. [PMC free article: PMC5848506] [PubMed: 28547128]
- Chiang J, Dalton J, Upadhyaya SA, et al.: Chromosome arm 1q gain is an adverse prognostic factor in localized and diffuse leptomeningeal glioneuronal tumors with BRAF gene fusion and 1p deletion. Acta Neuropathol 137 (1): 179-181, 2019. [PubMed: 30465258]
- Sievers P, Stichel D, Schrimpf D, et al.: FGFR1:TACC1 fusion is a frequent event in molecularly defined extraventricular neurocytoma. Acta Neuropathol 136 (2): 293-302, 2018. [PubMed: 29978331]
- Fisher PG, Tihan T, Goldthwaite PT, et al.: Outcome analysis of childhood low-grade astrocytomas. Pediatr Blood Cancer 51 (2): 245-50, 2008. [PubMed: 18386785]
- Qaddoumi I, Sultan I, Gajjar A: Outcome and prognostic features in pediatric gliomas: a review of 6212 cases from the Surveillance, Epidemiology, and End Results database. Cancer 115 (24): 5761-70, 2009. [PMC free article: PMC2794938] [PubMed: 19813274]
- Wisoff JH, Sanford RA, Heier LA, et al.: Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children's Oncology Group. Neurosurgery 68 (6): 1548-54; discussion 1554-5, 2011. [PubMed: 21368693]
- Bandopadhayay P, Bergthold G, London WB, et al.: Long-term outcome of 4,040 children diagnosed with pediatric low-grade gliomas: an analysis of the Surveillance Epidemiology and End Results (SEER) database. Pediatr Blood Cancer 61 (7): 1173-9, 2014. [PMC free article: PMC4657506] [PubMed: 24482038]
- von Hornstein S, Kortmann RD, Pietsch T, et al.: Impact of chemotherapy on disseminated low-grade glioma in children and adolescents: report from the HIT-LGG 1996 trial. Pediatr Blood Cancer 56 (7): 1046-54, 2011. [PubMed: 21319282]
- Mazloom A, Hodges JC, Teh BS, et al.: Outcome of patients with pilocytic astrocytoma and leptomeningeal dissemination. Int J Radiat Oncol Biol Phys 84 (2): 350-4, 2012. [PubMed: 22401918]
- Stokland T, Liu JF, Ironside JW, et al.: A multivariate analysis of factors determining tumor progression in childhood low-grade glioma: a population-based cohort study (CCLG CNS9702). Neuro Oncol 12 (12): 1257-68, 2010. [PMC free article: PMC3018938] [PubMed: 20861086]
- Mirow C, Pietsch T, Berkefeld S, et al.: Children <1 year show an inferior outcome when treated according to the traditional LGG treatment strategy: a report from the German multicenter trial HIT-LGG 1996 for children with low grade glioma (LGG). Pediatr Blood Cancer 61 (3): 457-63, 2014. [PubMed: 24039013]
- Rakotonjanahary J, De Carli E, Delion M, et al.: Mortality in Children with Optic Pathway Glioma Treated with Up-Front BB-SFOP Chemotherapy. PLoS One 10 (6): e0127676, 2015. [PMC free article: PMC4476571] [PubMed: 26098902]
- Gnekow AK, Walker DA, Kandels D, et al.: A European randomised controlled trial of the addition of etoposide to standard vincristine and carboplatin induction as part of an 18-month treatment programme for childhood (≤16 years) low grade glioma - A final report. Eur J Cancer 81: 206-225, 2017. [PMC free article: PMC5517338] [PubMed: 28649001]
- Chamdine O, Broniscer A, Wu S, et al.: Metastatic Low-Grade Gliomas in Children: 20 Years' Experience at St. Jude Children's Research Hospital. Pediatr Blood Cancer 63 (1): 62-70, 2016. [PMC free article: PMC5122937] [PubMed: 26312767]
- Due-Tønnessen BJ, Helseth E, Scheie D, et al.: Long-term outcome after resection of benign cerebellar astrocytomas in children and young adults (0-19 years): report of 110 consecutive cases. Pediatr Neurosurg 37 (2): 71-80, 2002. [PubMed: 12145515]
- Massimi L, Tufo T, Di Rocco C: Management of optic-hypothalamic gliomas in children: still a challenging problem. Expert Rev Anticancer Ther 7 (11): 1591-610, 2007. [PubMed: 18020927]
- Campagna M, Opocher E, Viscardi E, et al.: Optic pathway glioma: long-term visual outcome in children without neurofibromatosis type-1. Pediatr Blood Cancer 55 (6): 1083-8, 2010. [PubMed: 20979170]
- Hernáiz Driever P, von Hornstein S, Pietsch T, et al.: Natural history and management of low-grade glioma in NF-1 children. J Neurooncol 100 (2): 199-207, 2010. [PubMed: 20352473]
- Falzon K, Drimtzias E, Picton S, et al.: Visual outcomes after chemotherapy for optic pathway glioma in children with and without neurofibromatosis type 1: results of the International Society of Paediatric Oncology (SIOP) Low-Grade Glioma 2004 trial UK cohort. Br J Ophthalmol 102 (10): 1367-1371, 2018. [PubMed: 29343527]
- Finlay JL, Boyett JM, Yates AJ, et al.: Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen. Childrens Cancer Group. J Clin Oncol 13 (1): 112-23, 1995. [PubMed: 7799011]
- Villano JL, Seery TE, Bressler LR: Temozolomide in malignant gliomas: current use and future targets. Cancer Chemother Pharmacol 64 (4): 647-55, 2009. [PubMed: 19543728]
- Karremann M, Gielen GH, Hoffmann M, et al.: Diffuse high-grade gliomas with H3 K27M mutations carry a dismal prognosis independent of tumor location. Neuro Oncol 20 (1): 123-131, 2018. [PMC free article: PMC5761525] [PubMed: 29016894]
Stage Information for Childhood Astrocytomas
There is no recognized staging system for childhood astrocytomas. For the purposes of this summary, the treatment of childhood astrocytomas will be described using the following classifications:
- Low-grade astrocytoma—grades I and II (e.g., pilocytic astrocytomas and diffuse astrocytomas).
- -
Newly diagnosed.
- -
Progressive/recurrent.
- High-grade astrocytoma—grades III and IV (anaplastic astrocytomas and glioblastoma).
- -
Newly diagnosed.
- -
Recurrent.
Treatment Option Overview for Childhood Astrocytomas
Dramatic improvements in survival have been achieved for children and adolescents with cancer. Between 1975 and 2010, childhood cancer mortality decreased by more than 50%.[1] Many of the improvements in survival in childhood cancer have been made as a result of clinical trials that have attempted to improve on the best available, accepted therapy. Clinical trials in pediatrics are designed to compare new therapy with therapy that is currently accepted as standard. This comparison may be done in a randomized study of two treatment arms or by evaluating a single new treatment and comparing the results with previously obtained results that assessed an existing therapy. Because of the relative rarity of cancer in children, all patients with brain tumors should be considered for entry into a clinical trial. Information about ongoing National Cancer Institute (NCI)–supported clinical trials is available from the NCI website.
To determine and implement optimal treatment, planning by a multidisciplinary team of cancer specialists who have experience treating childhood brain tumors is required. Irradiation of pediatric brain tumors is technically very demanding and should be carried out in centers that have experience in that area to ensure optimal results.
Long-term management of patients with brain tumors is complex and requires a multidisciplinary approach. (Refer to the PDQ summary on Late Effects of Treatment for Childhood Cancer for specific information about the incidence, type, and monitoring of late effects in childhood and adolescent cancer survivors.)
Table 4 describes the standard treatment options for low-grade and high-grade childhood astrocytomas.
Table 4. Standard Treatment Options for Childhood Astrocytomas
| Treatment Group | Standard Treatment Options | |
|---|---|---|
| Childhood low-grade astrocytomas: | ||
| Newly diagnosed childhood low-grade astrocytomas | Observation without intervention | |
| Surgery | ||
| Adjuvant therapy (for tumors that are incompletely resected): | ||
| —Observation after surgery | ||
| —Chemotherapy | ||
| —Radiation therapy | ||
| —Targeted therapy | ||
| Progressive/recurrent childhood low-grade astrocytomas | Second surgery | |
| Radiation therapy | ||
| Chemotherapy | ||
| Targeted therapy with or without chemotherapy | ||
| Childhood high-grade astrocytomas: | ||
| Newly diagnosed childhood high-grade astrocytomas | Surgery | |
| Adjuvant therapy: | ||
| —Radiation therapy | ||
| —Chemotherapy | ||
| Recurrent childhood high-grade astrocytomas | Surgery (not considered standard treatment) | |
| High-dose chemotherapy with stem cell transplant (SCT) (not considered standard treatment) | ||
| Radiation therapy (not considered standard treatment) | ||
| Targeted therapy with a BRAF inhibitor, for patients with a BRAF V600E mutation (not considered standard treatment) | ||
References
- Smith MA, Altekruse SF, Adamson PC, et al.: Declining childhood and adolescent cancer mortality. Cancer 120 (16): 2497-506, 2014. [PMC free article: PMC4136455] [PubMed: 24853691]
Treatment of Childhood Low-Grade Astrocytomas
To determine and implement optimal management, treatment is often guided by a multidisciplinary team of cancer specialists who have experience treating childhood brain tumors.
For children with low-grade optic pathway astrocytomas, treatment options should be considered not only to improve survival but also to stabilize visual function.[1,2]
Standard treatment options for newly diagnosed childhood low-grade astrocytomas include the following:
- Adjuvant therapy (for tumors that are incompletely resected).
Observation without intervention
Observation, in the absence of any intervention, is an option for patients with neurofibromatosis type 1 (NF1) or incidentally found, asymptomatic masses.[3] Spontaneous regressions of optic pathway gliomas have been reported in children with and without NF1.[4,5]
Surgery
Surgical resection is the primary treatment for childhood low-grade astrocytoma [6,7] and surgical feasibility is determined by tumor location. In infants and young children, low-grade astrocytomas presenting in the optic chiasm/hypothalamus make surgery difficult; consequently, biopsies are not always done. This is especially true in patients with NF1.[6] When associated with NF1, tumors may be of multifocal origin. Diffuse astrocytomas (World Health Organization [WHO] grade II) may be less amenable to total resection, and this may contribute to a poorer outcome in these patients.
- Cerebellum: Complete or near-complete removal can be obtained in 90% to 95% of patients with pilocytic tumors that occur in the cerebellum.[7]
- Optic nerve: For children with isolated optic nerve lesions and progressive symptoms, complete surgical resection, while curative, generally results in blindness in the affected eye. In the absence of retained vision in the affected eye, complete surgical resection may be considered when cosmesis related to proptosis is of concern.
- Midline structures (hypothalamus, thalamus, brain stem, and spinal cord): Low-grade astrocytomas that occur in midline structures can sometimes be aggressively resected, with resultant long-term disease control.[4,8,9]; [10][Level of evidence: 3iiiA] Despite the increasing surgical accessibility of these tumors, such resection may result in significant neurologic sequelae, especially in children younger than 2 years at diagnosis.[11][Level of evidence: 3iC] Because of the infiltrative nature of some deep-seated lesions, extensive surgical resection may not be appropriate and biopsy only should be considered.[12][Level of evidence: 3iiiDiii]
- Cerebrum: Circumscribed, grade I hemispheric tumors are often amenable to complete surgical resection.
After resection, immediate (within 48 hours of resection per Children’s Oncology Group [COG] criteria) postoperative magnetic resonance imaging is obtained. Surveillance scans are then obtained periodically for completely resected tumors, although the value following the initial 3- to 6-month postoperative period is uncertain.[13]; [14][Level of evidence: 3iiDiii]
Factors related to outcome for children with low-grade gliomas treated with surgery followed by observation were identified in a COG study that included 518 evaluable patients.[7] Overall outcome for the entire group was a 78% progression-free survival (PFS) rate at 8 years and 96% overall survival (OS) rate at 8 years. The following factors were related to prognosis:[7]
- Tumor location: Children with cerebellar and cerebral tumors showed a higher PFS rate at 8 years compared with patients with midline and chiasmatic tumors (84% ± 1.9% vs. 51% ± 5.9%, respectively).
- Histology: Approximately three-fourths of patients had pilocytic astrocytoma; PFS and OS were superior for these patients when compared with children with nonpilocytic tumors.
- Extent of resection: Patients with gross-total resection had 8-year PFS rates exceeding 90% and OS rates of 99%. By comparison, approximately one-half of patients with any degree of residual tumor (as assessed by operative report and by postoperative imaging) showed disease progression by 8 years, although OS rates exceeded 90%.[7]
- Age: Younger children (age <5 years) showed higher rates of tumor progression but there was no significant age effect for OS in multivariate analysis. In a retrospective review of a different series of pediatric patients, children younger than 1 year with low-grade glioma demonstrated an inferior PFS compared with children aged 1 year and older.[15]
The long-term functional outcome of cerebellar pilocytic astrocytomas is relatively favorable. Full-scale mean intelligence quotients (IQs) of patients with low-grade gliomas treated with surgery alone are close to the normative population. However, long-term medical, psychological, and educational deficits may be present in these patients.[16]; [17,18][Level of evidence: 3iiiC]
Adjuvant therapy
Adjuvant therapy following complete resection of a low-grade glioma is generally not required unless there is a subsequent recurrence of disease. Treatment options for patients with incompletely resected tumor must be individualized and may include one or more of the following:
- Targeted therapy (for subependymal giant cell astrocytomas).
A shunt or other cerebrospinal fluid diversion procedure may be needed.
Observation after surgery
In patients in whom a portion of the tumor has been resected, the patient may be observed without further disease-directed treatment, particularly if the pace of tumor regrowth is anticipated to be very slow. Approximately 50% of patients with less-than-gross total resection may have disease that remains progression-free at 5 to 8 years, supporting the observation strategy in selected patients.[7]
Chemotherapy
Given the long-term side effects associated with radiation therapy, postoperative chemotherapy may be initially recommended.
Chemotherapy may result in objective tumor shrinkage and delay the need for radiation therapy in most patients.[19-22] Chemotherapy is also an option that may delay or avoid radiation therapy in adolescents with optic nerve pathway gliomas.[23][Level of evidence: 3iiDii] Chemotherapy has been shown to shrink tumors in children with hypothalamic gliomas and the diencephalic syndrome, resulting in weight gain in those who respond to treatment.[24]
The most widely used regimens to treat tumor progression or symptomatic nonresectable, low-grade gliomas are the following:
- Combination of thioguanine, procarbazine, lomustine, and vincristine (TPCV).[22]; [27][Level of evidence: 1iiA]
The COG reported the results of a randomized phase III trial (COG-A9952) that treated children younger than 10 years with low-grade chiasmatic/hypothalamic gliomas without NF1 using one of two regimens: carboplatin and vincristine (CV) or TPCV. The 5-year event-free survival (EFS) rate was 39% (± 4%) for the CV regimen and 52% (± 5%) for the TPCV regimen. Toxicity rates between the two regimens were relatively comparable.[27] In the same study, children with NF1 were nonrandomly assigned to receive treatment with CV. The 5-year EFS rate for children with NF1 was markedly better, at 69% (± 4%), than it was for children without NF1 who received CV. In multivariate analysis, NF1 was an independent predictor of better EFS but not OS.[28]
A multicenter, prospective, randomized trial that compared treatment with vincristine/carboplatin with vincristine/carboplatin plus etoposide in children with low-grade glioma failed to demonstrate a difference in PFS and OS between the two regimens.[29][Level of evidence: 1iiD]
Other chemotherapy approaches have been employed to treat children with progressive or symptomatic nonresectable, low-grade astrocytomas, including the following:
- Multiagent, platinum-based regimens.[20,21,30]; [31][Level of evidence: 2Diii]; [32][Level of evidence: 3iiiB] Reported 5-year PFS rates have ranged from approximately 35% to 60% for children receiving platinum-based chemotherapy for optic pathway gliomas,[20,21] but most patients ultimately require further treatment. This is particularly true for children who initially present with hypothalamic/chiasmatic gliomas that have neuraxis dissemination.[33][Level of evidence: 3iiiDiii]
Among children receiving chemotherapy for optic pathway gliomas, those without NF1 have higher rates of disease progression than those with NF1, and infants have higher rates of disease progression than do children older than 1 year.[20,21,30,35] Visual status (including acuity and field) is an important measure of outcome and improvement after treatment, and it is variable even in patients with radiographic responses. Children with sporadic visual pathway gliomas have poorer visual outcomes than do children with NF1.[35]; [38,39][Level of evidence: 3iiiC] Better initial visual acuity, older age, and absence of postchiasmatic involvement are associated with improved or stable vision after chemotherapy.[40]
Radiation therapy
Radiation therapy is usually reserved until progressive disease is documented [41,42] and may be further delayed through the use of chemotherapy.[19,20]
For children with low-grade gliomas for whom radiation therapy is indicated, approaches that contour the radiation distribution to the tumor and avoid normal brain tissue (3-D conformal radiation therapy, intensity-modulated radiation therapy, stereotactic radiation therapy, and proton radiation therapy [charged-particle radiation therapy]) all appear effective and may potentially reduce the acute and long-term toxicities associated with these modalities.[43,44]; [45][Level of evidence: 3iDiii] Radiation doses of 54 Gy in 1.8 Gy fractions are typically used.[46,47]
Subsequent to radiation administration, care must be taken in distinguishing radiation-induced imaging changes from disease progression, which usually occurs during the first year after radiation, but may occur even after the first year, especially in patients with pilocytic astrocytomas.[48-51]; [52][Level of evidence: 2A]; [53][Level of evidence: 2C]; [54][Level of evidence: 3iiiDi]; [55][Level of evidence: 3iiiDii]; [12,56][Level of evidence: 3iiiDiii]
Radiation therapy results in long-term disease control for most children with chiasmatic and posterior pathway chiasmatic gliomas, but may also result in substantial intellectual and endocrinologic sequelae, cerebrovascular damage, late death, and possibly an increased risk of secondary tumors.[57-59]; [53][Level of evidence: 2C] A population-based study identified radiation therapy as the most significant risk factor associated with late mortality, although the patients who required radiation therapy may have reflected a higher-risk population.[59]
Children with NF1 may be at higher risk of radiation-associated secondary tumors and morbidity resulting from vascular changes. Radiation therapy and alkylating agents are used as last resorts for these patients, given the theoretically heightened risk of inducing neurologic toxic effects and second malignancy.[60]
Targeted therapy
For children with symptomatic subependymal giant cell astrocytomas (SEGAs), agents that inhibit mammalian target of rapamycin (mTOR) (e.g., everolimus and sirolimus) have been studied.
Evidence (treatment of SEGA with an mTOR inhibitor):
- Small series have shown significant reductions in the size of these tumors after administration of everolimus or sirolimus, often eliminating the need for surgery.[61]; [62][Level of evidence: 2C]; [63][Level of evidence: 3iiDiv]; [64][Level of evidence: 3iiiC]
- A multicenter, phase III, placebo-controlled trial of 117 patients confirmed these earlier findings.[65][Level of evidence: 1iDiv]
- 35% of the patients in the everolimus group had at least a 50% reduction in the size of the SEGA, versus no reduction in the placebo group.
- In a study of patients who were treated with everolimus for 5 years, the following results were observed:[66]
- A reduction in the size of the mass was observed in about 50% of patients; in many cases, the reduction was sustained.
- These patients also had a reduction in seizure frequency.
Treatment options under clinical evaluation
Early-phase therapeutic trials may be available for selected patients. These trials may be available via the COG, the Pediatric Brain Tumor Consortium, or other entities. Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- NCT02684058 (Phase II Pediatric Study With Dabrafenib in Combination With Trametinib in Patients With High-Grade Gliomas and Low-Grade Gliomas): The purpose of this study is to investigate the activity of dabrafenib in combination with trametinib in children and adolescent patients with BRAF V600 mutation–positive low-grade gliomas or relapsed or refractory high-grade gliomas.
- NCT03871257 (A Study of the Drugs Selumetinib Versus Carboplatin/Vincristine in Patients With NF1 and Low-Grade Glioma): This phase III trial investigates the use of selumetinib compared with the standard treatment of CV for treating patients with NF1-associated low-grade gliomas, and improving vision in patients with low-grade gliomas of the optic pathway (vision nerves).
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Nicolin G, Parkin P, Mabbott D, et al.: Natural history and outcome of optic pathway gliomas in children. Pediatr Blood Cancer 53 (7): 1231-7, 2009. [PubMed: 19621457]
- Kramm CM, Butenhoff S, Rausche U, et al.: Thalamic high-grade gliomas in children: a distinct clinical subset? Neuro Oncol 13 (6): 680-9, 2011. [PMC free article: PMC3107103] [PubMed: 21636712]
- Listernick R, Ferner RE, Liu GT, et al.: Optic pathway gliomas in neurofibromatosis-1: controversies and recommendations. Ann Neurol 61 (3): 189-98, 2007. [PMC free article: PMC5908242] [PubMed: 17387725]
- Albright AL: Feasibility and advisability of resections of thalamic tumors in pediatric patients. J Neurosurg 100 (5 Suppl Pediatrics): 468-72, 2004. [PubMed: 15287457]
- Piccirilli M, Lenzi J, Delfinis C, et al.: Spontaneous regression of optic pathways gliomas in three patients with neurofibromatosis type I and critical review of the literature. Childs Nerv Syst 22 (10): 1332-7, 2006. [PubMed: 16639629]
- Due-Tønnessen BJ, Helseth E, Scheie D, et al.: Long-term outcome after resection of benign cerebellar astrocytomas in children and young adults (0-19 years): report of 110 consecutive cases. Pediatr Neurosurg 37 (2): 71-80, 2002. [PubMed: 12145515]
- Wisoff JH, Sanford RA, Heier LA, et al.: Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children's Oncology Group. Neurosurgery 68 (6): 1548-54; discussion 1554-5, 2011. [PubMed: 21368693]
- Tseng JH, Tseng MY: Survival analysis of 81 children with primary spinal gliomas: a population-based study. Pediatr Neurosurg 42 (6): 347-53, 2006. [PubMed: 17047414]
- Ahmed R, Menezes AH, Torner JC: Role of resection and adjuvant therapy in long-term disease outcomes for low-grade pediatric intramedullary spinal cord tumors. J Neurosurg Pediatr 18 (5): 594-601, 2016. [PubMed: 27420482]
- Milano MT, Johnson MD, Sul J, et al.: Primary spinal cord glioma: a Surveillance, Epidemiology, and End Results database study. J Neurooncol 98 (1): 83-92, 2010. [PubMed: 19898743]
- Scheinemann K, Bartels U, Huang A, et al.: Survival and functional outcome of childhood spinal cord low-grade gliomas. Clinical article. J Neurosurg Pediatr 4 (3): 254-61, 2009. [PubMed: 19772410]
- Sawamura Y, Kamada K, Kamoshima Y, et al.: Role of surgery for optic pathway/hypothalamic astrocytomas in children. Neuro Oncol 10 (5): 725-33, 2008. [PMC free article: PMC2666249] [PubMed: 18612049]
- Sutton LN, Cnaan A, Klatt L, et al.: Postoperative surveillance imaging in children with cerebellar astrocytomas. J Neurosurg 84 (5): 721-5, 1996. [PubMed: 8622142]
- Dorward IG, Luo J, Perry A, et al.: Postoperative imaging surveillance in pediatric pilocytic astrocytomas. J Neurosurg Pediatr 6 (4): 346-52, 2010. [PubMed: 20887107]
- Mirow C, Pietsch T, Berkefeld S, et al.: Children <1 year show an inferior outcome when treated according to the traditional LGG treatment strategy: a report from the German multicenter trial HIT-LGG 1996 for children with low grade glioma (LGG). Pediatr Blood Cancer 61 (3): 457-63, 2014. [PubMed: 24039013]
- Beebe DW, Ris MD, Armstrong FD, et al.: Cognitive and adaptive outcome in low-grade pediatric cerebellar astrocytomas: evidence of diminished cognitive and adaptive functioning in National Collaborative Research Studies (CCG 9891/POG 9130). J Clin Oncol 23 (22): 5198-204, 2005. [PubMed: 16051961]
- Turner CD, Chordas CA, Liptak CC, et al.: Medical, psychological, cognitive and educational late-effects in pediatric low-grade glioma survivors treated with surgery only. Pediatr Blood Cancer 53 (3): 417-23, 2009. [PubMed: 19479971]
- Daszkiewicz P, Maryniak A, Roszkowski M, et al.: Long-term functional outcome of surgical treatment of juvenile pilocytic astrocytoma of the cerebellum in children. Childs Nerv Syst 25 (7): 855-60, 2009. [PubMed: 19418058]
- Packer RJ, Ater J, Allen J, et al.: Carboplatin and vincristine chemotherapy for children with newly diagnosed progressive low-grade gliomas. J Neurosurg 86 (5): 747-54, 1997. [PubMed: 9126887]
- Gnekow AK, Falkenstein F, von Hornstein S, et al.: Long-term follow-up of the multicenter, multidisciplinary treatment study HIT-LGG-1996 for low-grade glioma in children and adolescents of the German Speaking Society of Pediatric Oncology and Hematology. Neuro Oncol 14 (10): 1265-84, 2012. [PMC free article: PMC3452343] [PubMed: 22942186]
- Laithier V, Grill J, Le Deley MC, et al.: Progression-free survival in children with optic pathway tumors: dependence on age and the quality of the response to chemotherapy--results of the first French prospective study for the French Society of Pediatric Oncology. J Clin Oncol 21 (24): 4572-8, 2003. [PubMed: 14673044]
- Prados MD, Edwards MS, Rabbitt J, et al.: Treatment of pediatric low-grade gliomas with a nitrosourea-based multiagent chemotherapy regimen. J Neurooncol 32 (3): 235-41, 1997. [PubMed: 9049885]
- Chong AL, Pole JD, Scheinemann K, et al.: Optic pathway gliomas in adolescence--time to challenge treatment choices? Neuro Oncol 15 (3): 391-400, 2013. [PMC free article: PMC3578487] [PubMed: 23295772]
- Gropman AL, Packer RJ, Nicholson HS, et al.: Treatment of diencephalic syndrome with chemotherapy: growth, tumor response, and long term control. Cancer 83 (1): 166-72, 1998. [PubMed: 9655307]
- Gururangan S, Cavazos CM, Ashley D, et al.: Phase II study of carboplatin in children with progressive low-grade gliomas. J Clin Oncol 20 (13): 2951-8, 2002. [PubMed: 12089224]
- Dodgshun AJ, Maixner WJ, Heath JA, et al.: Single agent carboplatin for pediatric low-grade glioma: A retrospective analysis shows equivalent efficacy to multiagent chemotherapy. Int J Cancer 138 (2): 481-8, 2016. [PubMed: 26235348]
- Ater JL, Zhou T, Holmes E, et al.: Randomized study of two chemotherapy regimens for treatment of low-grade glioma in young children: a report from the Children's Oncology Group. J Clin Oncol 30 (21): 2641-7, 2012. [PMC free article: PMC3413276] [PubMed: 22665535]
- Ater JL, Xia C, Mazewski CM, et al.: Nonrandomized comparison of neurofibromatosis type 1 and non-neurofibromatosis type 1 children who received carboplatin and vincristine for progressive low-grade glioma: A report from the Children's Oncology Group. Cancer 122 (12): 1928-36, 2016. [PMC free article: PMC4892942] [PubMed: 27061921]
- Gnekow AK, Walker DA, Kandels D, et al.: A European randomised controlled trial of the addition of etoposide to standard vincristine and carboplatin induction as part of an 18-month treatment programme for childhood (≤16 years) low grade glioma - A final report. Eur J Cancer 81: 206-225, 2017. [PMC free article: PMC5517338] [PubMed: 28649001]
- Massimino M, Spreafico F, Cefalo G, et al.: High response rate to cisplatin/etoposide regimen in childhood low-grade glioma. J Clin Oncol 20 (20): 4209-16, 2002. [PubMed: 12377964]
- Massimino M, Spreafico F, Riva D, et al.: A lower-dose, lower-toxicity cisplatin-etoposide regimen for childhood progressive low-grade glioma. J Neurooncol 100 (1): 65-71, 2010. [PubMed: 20151174]
- Mora J, Perez-Jaume S, Cruz O: Treatment of childhood astrocytomas with irinotecan and cisplatin. Clin Transl Oncol 20 (4): 500-507, 2018. [PubMed: 28828715]
- von Hornstein S, Kortmann RD, Pietsch T, et al.: Impact of chemotherapy on disseminated low-grade glioma in children and adolescents: report from the HIT-LGG 1996 trial. Pediatr Blood Cancer 56 (7): 1046-54, 2011. [PubMed: 21319282]
- Bouffet E, Jakacki R, Goldman S, et al.: Phase II study of weekly vinblastine in recurrent or refractory pediatric low-grade glioma. J Clin Oncol 30 (12): 1358-63, 2012. [PubMed: 22393086]
- Lassaletta A, Scheinemann K, Zelcer SM, et al.: Phase II Weekly Vinblastine for Chemotherapy-Naïve Children With Progressive Low-Grade Glioma: A Canadian Pediatric Brain Tumor Consortium Study. J Clin Oncol 34 (29): 3537-3543, 2016. [PubMed: 27573663]
- Gururangan S, Fisher MJ, Allen JC, et al.: Temozolomide in children with progressive low-grade glioma. Neuro Oncol 9 (2): 161-8, 2007. [PMC free article: PMC1871667] [PubMed: 17347491]
- Khaw SL, Coleman LT, Downie PA, et al.: Temozolomide in pediatric low-grade glioma. Pediatr Blood Cancer 49 (6): 808-11, 2007. [PubMed: 17588234]
- Moreno L, Bautista F, Ashley S, et al.: Does chemotherapy affect the visual outcome in children with optic pathway glioma? A systematic review of the evidence. Eur J Cancer 46 (12): 2253-9, 2010. [PubMed: 20400294]
- Shofty B, Ben-Sira L, Freedman S, et al.: Visual outcome following chemotherapy for progressive optic pathway gliomas. Pediatr Blood Cancer 57 (3): 481-5, 2011. [PubMed: 21241008]
- Falzon K, Drimtzias E, Picton S, et al.: Visual outcomes after chemotherapy for optic pathway glioma in children with and without neurofibromatosis type 1: results of the International Society of Paediatric Oncology (SIOP) Low-Grade Glioma 2004 trial UK cohort. Br J Ophthalmol 102 (10): 1367-1371, 2018. [PubMed: 29343527]
- Fisher BJ, Leighton CC, Vujovic O, et al.: Results of a policy of surveillance alone after surgical management of pediatric low grade gliomas. Int J Radiat Oncol Biol Phys 51 (3): 704-10, 2001. [PubMed: 11597812]
- Tsang DS, Murphy ES, Merchant TE: Radiation Therapy for Optic Pathway and Hypothalamic Low-Grade Gliomas in Children. Int J Radiat Oncol Biol Phys 99 (3): 642-651, 2017. [PubMed: 29280458]
- Greenberger BA, Pulsifer MB, Ebb DH, et al.: Clinical outcomes and late endocrine, neurocognitive, and visual profiles of proton radiation for pediatric low-grade gliomas. Int J Radiat Oncol Biol Phys 89 (5): 1060-8, 2014. [PubMed: 25035209]
- Paulino AC, Mazloom A, Terashima K, et al.: Intensity-modulated radiotherapy (IMRT) in pediatric low-grade glioma. Cancer 119 (14): 2654-9, 2013. [PubMed: 23633429]
- Müller K, Gnekow A, Falkenstein F, et al.: Radiotherapy in pediatric pilocytic astrocytomas. A subgroup analysis within the prospective multicenter study HIT-LGG 1996 by the German Society of Pediatric Oncology and Hematology (GPOH). Strahlenther Onkol 189 (8): 647-55, 2013. [PubMed: 23831852]
- Bitterman DS, MacDonald SM, Yock TI, et al.: Revisiting the Role of Radiation Therapy for Pediatric Low-Grade Glioma. J Clin Oncol 37 (35): 3335-3339, 2019. [PMC free article: PMC9798905] [PubMed: 31498029]
- Cherlow JM, Shaw DWW, Margraf LR, et al.: Conformal Radiation Therapy for Pediatric Patients with Low-Grade Glioma: Results from the Children's Oncology Group Phase 2 Study ACNS0221. Int J Radiat Oncol Biol Phys 103 (4): 861-868, 2019. [PMC free article: PMC6548322] [PubMed: 30419305]
- Chawla S, Korones DN, Milano MT, et al.: Spurious progression in pediatric brain tumors. J Neurooncol 107 (3): 651-7, 2012. [PubMed: 22237949]
- Marcus KJ, Goumnerova L, Billett AL, et al.: Stereotactic radiotherapy for localized low-grade gliomas in children: final results of a prospective trial. Int J Radiat Oncol Biol Phys 61 (2): 374-9, 2005. [PubMed: 15667955]
- Combs SE, Schulz-Ertner D, Moschos D, et al.: Fractionated stereotactic radiotherapy of optic pathway gliomas: tolerance and long-term outcome. Int J Radiat Oncol Biol Phys 62 (3): 814-9, 2005. [PubMed: 15936565]
- Naftel RP, Pollack IF, Zuccoli G, et al.: Pseudoprogression of low-grade gliomas after radiotherapy. Pediatr Blood Cancer 62 (1): 35-9, 2015. [PubMed: 25213668]
- Merchant TE, Kun LE, Wu S, et al.: Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol 27 (22): 3598-604, 2009. [PMC free article: PMC3525947] [PubMed: 19581536]
- Merchant TE, Conklin HM, Wu S, et al.: Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol 27 (22): 3691-7, 2009. [PMC free article: PMC2799064] [PubMed: 19581535]
- Kano H, Niranjan A, Kondziolka D, et al.: Stereotactic radiosurgery for pilocytic astrocytomas part 2: outcomes in pediatric patients. J Neurooncol 95 (2): 219-29, 2009. [PubMed: 19468692]
- Hallemeier CL, Pollock BE, Schomberg PJ, et al.: Stereotactic radiosurgery for recurrent or unresectable pilocytic astrocytoma. Int J Radiat Oncol Biol Phys 83 (1): 107-12, 2012. [PubMed: 22019245]
- Mansur DB, Rubin JB, Kidd EA, et al.: Radiation therapy for pilocytic astrocytomas of childhood. Int J Radiat Oncol Biol Phys 79 (3): 829-34, 2011. [PubMed: 20421157]
- Jenkin D, Angyalfi S, Becker L, et al.: Optic glioma in children: surveillance, resection, or irradiation? Int J Radiat Oncol Biol Phys 25 (2): 215-25, 1993. [PubMed: 8420869]
- Khafaga Y, Hassounah M, Kandil A, et al.: Optic gliomas: a retrospective analysis of 50 cases. Int J Radiat Oncol Biol Phys 56 (3): 807-12, 2003. [PubMed: 12788189]
- Krishnatry R, Zhukova N, Guerreiro Stucklin AS, et al.: Clinical and treatment factors determining long-term outcomes for adult survivors of childhood low-grade glioma: A population-based study. Cancer 122 (8): 1261-9, 2016. [PubMed: 26970559]
- Grill J, Couanet D, Cappelli C, et al.: Radiation-induced cerebral vasculopathy in children with neurofibromatosis and optic pathway glioma. Ann Neurol 45 (3): 393-6, 1999. [PubMed: 10072056]
- Franz DN, Agricola KD, Tudor CA, et al.: Everolimus for tumor recurrence after surgical resection for subependymal giant cell astrocytoma associated with tuberous sclerosis complex. J Child Neurol 28 (5): 602-7, 2013. [PubMed: 22805244]
- Krueger DA, Care MM, Holland K, et al.: Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. N Engl J Med 363 (19): 1801-11, 2010. [PubMed: 21047224]
- Weidman DR, Pole JD, Bouffet E, et al.: Dose-level response rates of mTor inhibition in tuberous sclerosis complex (TSC) related subependymal giant cell astrocytoma (SEGA). Pediatr Blood Cancer 62 (10): 1754-60, 2015. [PubMed: 25929843]
- Franz DN, Leonard J, Tudor C, et al.: Rapamycin causes regression of astrocytomas in tuberous sclerosis complex. Ann Neurol 59 (3): 490-8, 2006. [PubMed: 16453317]
- Franz DN, Belousova E, Sparagana S, et al.: Efficacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 381 (9861): 125-32, 2013. [PubMed: 23158522]
- Franz DN, Agricola K, Mays M, et al.: Everolimus for subependymal giant cell astrocytoma: 5-year final analysis. Ann Neurol 78 (6): 929-38, 2015. [PMC free article: PMC5063160] [PubMed: 26381530]
Treatment of Progressive/Recurrent Childhood Low-Grade Astrocytomas
To determine and implement optimal management, treatment is often guided by a multidisciplinary team of cancer specialists who have experience treating childhood brain tumors.
For children with low-grade optic pathway astrocytomas, treatment options should be considered not only to improve survival but also to stabilize visual function.[1,2]
Childhood low-grade astrocytomas may progress or recur many years after initial presentation and treatment.
An individual plan needs to be tailored on the basis of the following:
- Patient age.
- Tumor location.
- Prior treatment.
Recurrent disease is usually at the primary tumor site, although multifocal or widely disseminated disease to other intracranial sites and to the spinal leptomeninges has been documented.[3,4] Most children whose low-grade diffuse fibrillary astrocytomas recur will harbor low-grade lesions; however, transformation into a higher grade tumor is possible. Surveillance imaging will frequently identify asymptomatic recurrences.[5] At the time of recurrence, a complete evaluation to determine the extent of the relapse is indicated.
Standard treatment options for progressive/recurrent childhood low-grade astrocytomas include the following:
Second surgery
Patients with low-grade astrocytomas who relapse after being treated with surgery alone may be candidates for another surgical resection.[6] The need for surgical intervention must be individualized on the basis of the following:
- Initial tumor type.
- Length of time between initial treatment and the reappearance of the mass lesion.
- Clinical picture.
Utility of second surgery is impacted by site of recurrence and the probability of obtaining a near-total resection/gross-total resection without significant neurologic injury.[7]
Radiation therapy
The rationale for the use of radiation therapy is essentially the same when utilized as first-line therapy or at the time of recurrence (refer to the Radiation therapy subsection of the Treatment of Childhood Low-Grade Astrocytomas section of this summary). If the child has never received radiation therapy, local radiation therapy may be a treatment option, although chemotherapy in lieu of radiation may be considered, depending on the child's age and the extent and location of the tumor.[8][Level of evidence: 3iA]; [9][Level of evidence: 3iiiDi]
For children with low-grade gliomas for whom radiation therapy is indicated, conformal radiation therapy approaches appear effective and offer the potential for reducing the acute and long-term toxicities associated with this modality.[10-13]
Chemotherapy
If there is recurrence at an unresectable site, chemotherapy should be considered.
Chemotherapy may result in relatively long-term disease control.[14,15] The choice of regimen depends on whether previous chemotherapy has been utilized. Numerous options can be considered, including carboplatin and vincristine (CV); thioguanine, procarbazine, lomustine, and vincristine (TPCV); vinblastine alone; temozolomide alone; or temozolomide in combination with carboplatin and vincristine.[14-17]
Targeted therapy with or without chemotherapy
Antitumor activity has also been observed for bevacizumab given in combination with irinotecan, which, in some cases, also results in clinical or visual improvement.[18]
Evidence (targeted therapy [bevacizumab]):
- In a phase II study of bevacizumab plus irinotecan for children with recurrent low-grade gliomas, the following results were observed:[19]
- Sustained partial responses were observed in only two patients (5.7%).
- The 6-month progression-free survival (PFS) rate was 85.4% (standard error [SE] ± 5.96%).
- The 2-year PFS rate was 47.8% (SE ± 9.27%).
- A pilot study of 14 patients with recurrent low-grade gliomas also evaluated bevacizumab-based therapies and observed the following:[20][Level of evidence: 3iiDi]; [21][Level of evidence: 3iiiDiv]
- Objective responses were seen in 12 patients (86%).
- No patients progressed on therapy (median treatment duration, 12 months), but 13 of 14 progressed after stopping bevacizumab at a median of 5 months.
- Bevacizumab has also been employed for children with low-grade gliomas and symptomatic radiation-induced tumor enlargement.[22]
- Treatment with bevacizumab produced radiographic improvement (five of five patients) and allowed weaning off steroids (four of four patients).
With the identification of BRAF mutations driving a significant proportion of low-grade gliomas, inhibition of various elements of this molecular pathway (e.g., MEK and BRAF) are actively being tested in ongoing clinical trials, with early reports suggesting substantial activity. While first-generation BRAF inhibitors like vemurafenib and dabrafenib are active against BRAF V600E–mutated tumors, they are contraindicated for tumors with BRAF gene fusions because of the potential for paradoxical activation of the MAPK pathway.[23,24]
Studies of BRAF and MEK inhibitors include the following:
- For patients whose tumors have BRAF V600E mutations, the focus of clinical research efforts is on the evaluation of BRAF inhibitors in combination with MEK inhibitors. Such combinations are approved for the treatment of adult cancers with BRAF V600E mutations and are more effective than either BRAF inhibitors or MEK inhibitors used as single agents.[25]
- Early results on the use of the BRAF V600E inhibitor dabrafenib, presented in abstract, demonstrated a 41% overall response rate (two complete responses and 11 partial responses) by central review in children with BRAF V600–mutated relapsed or refractory low-grade gliomas.[26]
- The MEK inhibitor selumetinib has been studied in a phase I/II clinical trial for children with low-grade gliomas (PBTC-029 [NCT01089101]).
- The phase I component of the PBTC-029 trial showed the following results:[32]
- Selumetinib was tolerated at a daily dose of 25 mg/m2.
- The most common adverse events leading to patient discontinuation of treatment were rash, paronychia, and asymptomatic creatine phosphokinase (CPK) elevation.
- Stratum 1 of the phase II component of this trial was for patients with BRAF genomic alterations.[33]
- Eight of 25 patients (32%) achieved a partial response, with responses occurring for both BRAF V600E patients and for patients with BRAF gene fusions.
- The 2-year PFS was 66% for stratum 1 patients.
- Stratum 3 of the phase II component of this trial was for patients with NF1-associated low-grade gliomas.[33]
- The 2-year event-free survival rate for this group was 96%.
- 10 of 25 patients (40%) achieved partial responses.
The most common toxicities across all strata were grade 1 and grade 2 CPK elevation, diarrhea, hypoalbuminemia, elevated aspartate aminotransferase (AST), and rash. Rare grade 3 and grade 4 toxicities included elevated CPK, rash, neutropenia, emesis, and paronychia.
Treatment options under clinical evaluation
Early-phase therapeutic trials may be available for selected patients. These trials may be available via the COG, the Pediatric Brain Tumor Consortium, or other entities. Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- APEC1621 (NCT03155620) (Pediatric MATCH: Targeted Therapy Directed by Genetic Testing in Treating Pediatric Patients with Relapsed or Refractory Advanced Solid Tumors, Non-Hodgkin Lymphomas, or Histiocytic Disorders): NCI-COG Pediatric Molecular Analysis for Therapeutic Choice (MATCH), referred to as Pediatric MATCH, will match targeted agents with specific molecular changes identified using a next-generation sequencing targeted assay of more than 4,000 different mutations across more than 160 genes in refractory and recurrent solid tumors. Children and adolescents aged 1 to 21 years are eligible for the trial.Tumor tissue from progressive or recurrent disease must be available for molecular characterization. Patients with tumors that have molecular variants addressed by treatment arms included in the trial will be offered treatment on Pediatric MATCH. Additional information can be obtained on the NCI website and ClinicalTrials.gov website.
- PBTC-029B (NCT01089101) (Selumetinib in Treating Young Patients With Recurrent or Refractory Low-Grade Glioma): This is a clinical trial to determine the side effects and the best dose of the MEK inhibitor selumetinib in children with low-grade astrocytoma (phase I component). Based on activity observed in the phase I component (now completed), the study has been modified to include phase II expansion cohorts for patients with pilocytic astrocytoma and other low-grade astrocytomas with BRAF genomic alterations and for NF1 patients with recurrent low-grade astrocytomas.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Nicolin G, Parkin P, Mabbott D, et al.: Natural history and outcome of optic pathway gliomas in children. Pediatr Blood Cancer 53 (7): 1231-7, 2009. [PubMed: 19621457]
- Kramm CM, Butenhoff S, Rausche U, et al.: Thalamic high-grade gliomas in children: a distinct clinical subset? Neuro Oncol 13 (6): 680-9, 2011. [PMC free article: PMC3107103] [PubMed: 21636712]
- Perilongo G, Carollo C, Salviati L, et al.: Diencephalic syndrome and disseminated juvenile pilocytic astrocytomas of the hypothalamic-optic chiasm region. Cancer 80 (1): 142-6, 1997. [PubMed: 9210720]
- Leibel SA, Sheline GE, Wara WM, et al.: The role of radiation therapy in the treatment of astrocytomas. Cancer 35 (6): 1551-7, 1975. [PubMed: 1148989]
- Udaka YT, Yeh-Nayre LA, Amene CS, et al.: Recurrent pediatric central nervous system low-grade gliomas: the role of surveillance neuroimaging in asymptomatic children. J Neurosurg Pediatr 11 (2): 119-26, 2013. [PubMed: 23157391]
- Austin EJ, Alvord EC: Recurrences of cerebellar astrocytomas: a violation of Collins' law. J Neurosurg 68 (1): 41-7, 1988. [PubMed: 3335911]
- Bowers DC, Krause TP, Aronson LJ, et al.: Second surgery for recurrent pilocytic astrocytoma in children. Pediatr Neurosurg 34 (5): 229-34, 2001. [PubMed: 11423771]
- Scheinemann K, Bartels U, Tsangaris E, et al.: Feasibility and efficacy of repeated chemotherapy for progressive pediatric low-grade gliomas. Pediatr Blood Cancer 57 (1): 84-8, 2011. [PubMed: 21557457]
- de Haas V, Grill J, Raquin MA, et al.: Relapses of optic pathway tumors after first-line chemotherapy. Pediatr Blood Cancer 52 (5): 575-80, 2009. [PubMed: 19148944]
- Merchant TE, Conklin HM, Wu S, et al.: Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol 27 (22): 3691-7, 2009. [PMC free article: PMC2799064] [PubMed: 19581535]
- Marcus KJ, Goumnerova L, Billett AL, et al.: Stereotactic radiotherapy for localized low-grade gliomas in children: final results of a prospective trial. Int J Radiat Oncol Biol Phys 61 (2): 374-9, 2005. [PubMed: 15667955]
- Bitterman DS, MacDonald SM, Yock TI, et al.: Revisiting the Role of Radiation Therapy for Pediatric Low-Grade Glioma. J Clin Oncol 37 (35): 3335-3339, 2019. [PMC free article: PMC9798905] [PubMed: 31498029]
- Cherlow JM, Shaw DWW, Margraf LR, et al.: Conformal Radiation Therapy for Pediatric Patients with Low-Grade Glioma: Results from the Children's Oncology Group Phase 2 Study ACNS0221. Int J Radiat Oncol Biol Phys 103 (4): 861-868, 2019. [PMC free article: PMC6548322] [PubMed: 30419305]
- Packer RJ, Lange B, Ater J, et al.: Carboplatin and vincristine for recurrent and newly diagnosed low-grade gliomas of childhood. J Clin Oncol 11 (5): 850-6, 1993. [PubMed: 8487049]
- Gnekow AK, Falkenstein F, von Hornstein S, et al.: Long-term follow-up of the multicenter, multidisciplinary treatment study HIT-LGG-1996 for low-grade glioma in children and adolescents of the German Speaking Society of Pediatric Oncology and Hematology. Neuro Oncol 14 (10): 1265-84, 2012. [PMC free article: PMC3452343] [PubMed: 22942186]
- Gururangan S, Fisher MJ, Allen JC, et al.: Temozolomide in children with progressive low-grade glioma. Neuro Oncol 9 (2): 161-8, 2007. [PMC free article: PMC1871667] [PubMed: 17347491]
- Lassaletta A, Scheinemann K, Zelcer SM, et al.: Phase II Weekly Vinblastine for Chemotherapy-Naïve Children With Progressive Low-Grade Glioma: A Canadian Pediatric Brain Tumor Consortium Study. J Clin Oncol 34 (29): 3537-3543, 2016. [PubMed: 27573663]
- Avery RA, Hwang EI, Jakacki RI, et al.: Marked recovery of vision in children with optic pathway gliomas treated with bevacizumab. JAMA Ophthalmol 132 (1): 111-4, 2014. [PubMed: 24232489]
- Gururangan S, Fangusaro J, Poussaint TY, et al.: Efficacy of bevacizumab plus irinotecan in children with recurrent low-grade gliomas--a Pediatric Brain Tumor Consortium study. Neuro Oncol 16 (2): 310-7, 2014. [PMC free article: PMC3895377] [PubMed: 24311632]
- Hwang EI, Jakacki RI, Fisher MJ, et al.: Long-term efficacy and toxicity of bevacizumab-based therapy in children with recurrent low-grade gliomas. Pediatr Blood Cancer 60 (5): 776-82, 2013. [PubMed: 22976922]
- Packer RJ, Jakacki R, Horn M, et al.: Objective response of multiply recurrent low-grade gliomas to bevacizumab and irinotecan. Pediatr Blood Cancer 52 (7): 791-5, 2009. [PubMed: 19165892]
- Foster KA, Ares WJ, Pollack IF, et al.: Bevacizumab for symptomatic radiation-induced tumor enlargement in pediatric low grade gliomas. Pediatr Blood Cancer 62 (2): 240-245, 2015. [PubMed: 25382690]
- Sievert AJ, Lang SS, Boucher KL, et al.: Paradoxical activation and RAF inhibitor resistance of BRAF protein kinase fusions characterizing pediatric astrocytomas. Proc Natl Acad Sci U S A 110 (15): 5957-62, 2013. [PMC free article: PMC3625308] [PubMed: 23533272]
- Karajannis MA, Legault G, Fisher MJ, et al.: Phase II study of sorafenib in children with recurrent or progressive low-grade astrocytomas. Neuro Oncol 16 (10): 1408-16, 2014. [PMC free article: PMC4165419] [PubMed: 24803676]
- Odogwu L, Mathieu L, Blumenthal G, et al.: FDA Approval Summary: Dabrafenib and Trametinib for the Treatment of Metastatic Non-Small Cell Lung Cancers Harboring BRAF V600E Mutations. Oncologist 23 (6): 740-745, 2018. [PMC free article: PMC6067947] [PubMed: 29438093]
- Kieran MW, Bouffet E, Tabori U, et al.: The first study of dabrafenib in pediatric patients with BRAF V600–mutant relapsed or refractory low-grade gliomas. [Abstract] Ann Oncol 27 (Suppl 6): A-LBA19 PR, 2016.
- Rush S, Foreman N, Liu A: Brainstem ganglioglioma successfully treated with vemurafenib. J Clin Oncol 31 (10): e159-60, 2013. [PubMed: 23358987]
- del Bufalo F, Carai A, Figà-Talamanca L, et al.: Response of recurrent BRAFV600E mutated ganglioglioma to Vemurafenib as single agent. J Transl Med 12: 356, 2014. [PMC free article: PMC4279809] [PubMed: 25524464]
- Aguilera D, Janss A, Mazewski C, et al.: Successful Retreatment of a Child with a Refractory Brainstem Ganglioglioma with Vemurafenib. Pediatr Blood Cancer 63 (3): 541-3, 2016. [PubMed: 26579623]
- Marks AM, Bindra RS, DiLuna ML, et al.: Response to the BRAF/MEK inhibitors dabrafenib/trametinib in an adolescent with a BRAF V600E mutated anaplastic ganglioglioma intolerant to vemurafenib. Pediatr Blood Cancer 65 (5): e26969, 2018. [PubMed: 29380516]
- Touat M, Gratieux J, Condette Auliac S, et al.: Vemurafenib and cobimetinib overcome resistance to vemurafenib in BRAF-mutant ganglioglioma. Neurology 91 (11): 523-525, 2018. [PMC free article: PMC9694795] [PubMed: 30120137]
- Banerjee A, Jakacki RI, Onar-Thomas A, et al.: A phase I trial of the MEK inhibitor selumetinib (AZD6244) in pediatric patients with recurrent or refractory low-grade glioma: a Pediatric Brain Tumor Consortium (PBTC) study. Neuro Oncol 19 (8): 1135-1144, 2017. [PMC free article: PMC5570236] [PubMed: 28339824]
- Fangusaro JR, Onar-Thomas A, Young-Poussaint T, et al.: A phase II prospective study of selumetinib in children with recurrent or refractory low-grade glioma (LGG): a Pediatric Brain Tumor Consortium (PBTC) study. [Abstract] J Clin Oncol 35 (Suppl 15): A-10504, 2017. Also available online. Last accessed June 26, 2020.
Treatment of Childhood High-Grade Astrocytomas
To determine and implement optimal management, treatment of childhood high-grade astrocytomas should be guided by a multidisciplinary team of cancer specialists who have experience treating childhood brain tumors.
Outcomes in high-grade gliomas occurring in childhood are often more favorable than that in adults. It is not clear whether this difference is caused by biologic variations in tumor characteristics, therapies used, tumor resectability, or other factors.
The therapy for both children and adults with supratentorial high-grade astrocytoma includes surgery, radiation therapy, and chemotherapy.
Standard treatment options for newly diagnosed childhood high-grade astrocytomas include the following:
Surgery
The ability to obtain a complete resection is associated with a better prognosis.[1,2] Among patients treated with surgery, radiation therapy, and nitrosourea (lomustine)-based chemotherapy, the 5-year progression-free survival rate was 19% (± 3%); the survival rate was 40% in those who had total resections.[3] Similarly, in a trial of multiagent chemoradiation therapy and adjuvant chemotherapy in addition to valproic acid, the overall 5-year event-free survival (EFS) rate was 13%, but for children with a complete resection of their tumor, the EFS rate was 48%.[4][Level of evidence: 2A]
Adjuvant therapy
Radiation therapy
Radiation therapy is routinely administered to a field that widely encompasses the entire tumor. The radiation therapy dose to the tumor bed is usually at least 54 Gy. Despite such therapy, overall survival (OS) rates remain poor. Similarly poor survival is seen in children with spinal cord primaries and children with thalamic high-grade gliomas (i.e., diffuse midline gliomas, H3 K27M-mutant tumors) treated with radiation therapy.[5,6]; [7,8][Level of evidence: 3iiiA]
Chemotherapy
In one trial, children with glioblastoma who were treated on a prospective randomized trial with adjuvant lomustine, vincristine, and prednisone fared better than children treated with radiation therapy alone.[9] Furthermore, children who received lomustine in addition to temozolomide for subtotally-resected tumors, especially glioblastoma with methylated O-6-methylguanine-DNA-methyltransferase (MGMT) overexpression, had a slightly improved outcome.[10] Patients with IDH1 mutations had an improved 1-year OS rate (100%) when compared with IDH1–wild-type tumors (1-year OS rate, 81%), highlighting the potential importance of underlying biological characteristics.[11]
The use of temozolomide to treat glioblastoma was initially investigated in adults. In this population, the addition of temozolomide during and after radiation therapy resulted in improved 2-year EFS compared with treatment with radiation therapy alone. Adult patients with glioblastoma with an MGMT promoter benefitted from temozolomide, whereas those who did not have a methylated MGMT promoter did not.[12,13] The role of temozolomide given concurrently with radiation therapy for children with supratentorial high-grade glioma appears comparable to the outcome seen in children treated with nitrosourea-based therapy [14] and again demonstrated an EFS advantage for those children without MGMT overexpression.
The use of adjuvant bevacizumab after radiation therapy did not prolong OS or progression-free survival in pediatric patients with newly diagnosed high-grade gliomas.[15]
Younger children may benefit from chemotherapy or consolidation with high-dose chemotherapy to delay, modify, or, in selected cases, obviate the need for radiation therapy.[16-18]
Treatment options under clinical evaluation
Early-phase therapeutic trials may be available for selected patients. These trials may be available via the Children’s Oncology Group (COG), the Pediatric Brain Tumor Consortium, or other entities. Information about National Cancer Institute (NCI)–supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- ACNS1721 (NCT03581292) (Veliparib, Radiation Therapy, and Temozolomide in Treating Participants With Newly Diagnosed Malignant Glioma Without H3 K27M or BRAF V600E Mutations): This phase II trial investigates the use of veliparib, radiation therapy, and temozolomide in treating patients with newly diagnosed malignant glioma without H3 K27M or BRAF V600E mutations.
- ACNS1723 (NCT03919071) (Dabrafenib Combined With Trametinib After Radiation Therapy in Treating Patients With Newly-Diagnosed High-Grade Glioma): This phase II trial investigates the use of the combination of dabrafenib and trametinib after radiation therapy in children and young adults with high-grade gliomas who have a BRAF V600 mutation.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Wisoff JH, Boyett JM, Berger MS, et al.: Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children's Cancer Group trial no. CCG-945. J Neurosurg 89 (1): 52-9, 1998. [PubMed: 9647172]
- Yang T, Temkin N, Barber J, et al.: Gross total resection correlates with long-term survival in pediatric patients with glioblastoma. World Neurosurg 79 (3-4): 537-44, 2013 Mar-Apr. [PubMed: 23017588]
- Fouladi M, Hunt DL, Pollack IF, et al.: Outcome of children with centrally reviewed low-grade gliomas treated with chemotherapy with or without radiotherapy on Children's Cancer Group high-grade glioma study CCG-945. Cancer 98 (6): 1243-52, 2003. [PubMed: 12973849]
- Wolff JE, Driever PH, Erdlenbruch B, et al.: Intensive chemotherapy improves survival in pediatric high-grade glioma after gross total resection: results of the HIT-GBM-C protocol. Cancer 116 (3): 705-12, 2010. [PubMed: 19957326]
- Kramm CM, Butenhoff S, Rausche U, et al.: Thalamic high-grade gliomas in children: a distinct clinical subset? Neuro Oncol 13 (6): 680-9, 2011. [PMC free article: PMC3107103] [PubMed: 21636712]
- Tendulkar RD, Pai Panandiker AS, Wu S, et al.: Irradiation of pediatric high-grade spinal cord tumors. Int J Radiat Oncol Biol Phys 78 (5): 1451-6, 2010. [PMC free article: PMC5095924] [PubMed: 20346593]
- Wolff B, Ng A, Roth D, et al.: Pediatric high grade glioma of the spinal cord: results of the HIT-GBM database. J Neurooncol 107 (1): 139-46, 2012. [PubMed: 21964697]
- Ononiwu C, Mehta V, Bettegowda C, et al.: Pediatric spinal glioblastoma multiforme: current treatment strategies and possible predictors of survival. Childs Nerv Syst 28 (5): 715-20, 2012. [PubMed: 22307824]
- Sposto R, Ertel IJ, Jenkin RD, et al.: The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: results of a randomized trial. A report from the Childrens Cancer Study Group. J Neurooncol 7 (2): 165-77, 1989. [PubMed: 2550594]
- Jakacki RI, Cohen KJ, Buxton A, et al.: Phase 2 study of concurrent radiotherapy and temozolomide followed by temozolomide and lomustine in the treatment of children with high-grade glioma: a report of the Children's Oncology Group ACNS0423 study. Neuro Oncol 18 (10): 1442-50, 2016. [PMC free article: PMC5035517] [PubMed: 27006176]
- Pollack IF, Hamilton RL, Sobol RW, et al.: IDH1 mutations are common in malignant gliomas arising in adolescents: a report from the Children's Oncology Group. Childs Nerv Syst 27 (1): 87-94, 2011. [PMC free article: PMC3014378] [PubMed: 20725730]
- Stupp R, Mason WP, van den Bent MJ, et al.: Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352 (10): 987-96, 2005. [PubMed: 15758009]
- Hegi ME, Diserens AC, Gorlia T, et al.: MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352 (10): 997-1003, 2005. [PubMed: 15758010]
- Cohen KJ, Pollack IF, Zhou T, et al.: Temozolomide in the treatment of high-grade gliomas in children: a report from the Children's Oncology Group. Neuro Oncol 13 (3): 317-23, 2011. [PMC free article: PMC3064602] [PubMed: 21339192]
- Grill J, Massimino M, Bouffet E, et al.: Phase II, Open-Label, Randomized, Multicenter Trial (HERBY) of Bevacizumab in Pediatric Patients With Newly Diagnosed High-Grade Glioma. J Clin Oncol 36 (10): 951-958, 2018. [PubMed: 29412784]
- Duffner PK, Horowitz ME, Krischer JP, et al.: Postoperative chemotherapy and delayed radiation in children less than three years of age with malignant brain tumors. N Engl J Med 328 (24): 1725-31, 1993. [PubMed: 8388548]
- Dufour C, Grill J, Lellouch-Tubiana A, et al.: High-grade glioma in children under 5 years of age: a chemotherapy only approach with the BBSFOP protocol. Eur J Cancer 42 (17): 2939-45, 2006. [PubMed: 16962317]
- Espinoza JC, Haley K, Patel N, et al.: Outcome of young children with high-grade glioma treated with irradiation-avoiding intensive chemotherapy regimens: Final report of the Head Start II and III trials. Pediatr Blood Cancer 63 (10): 1806-13, 2016. [PMC free article: PMC5598351] [PubMed: 27332770]
Treatment of Recurrent Childhood High-Grade Astrocytomas
To determine and implement optimal management, treatment of childhood high-grade astrocytomas should be guided by a multidisciplinary team of cancer specialists who have experience treating childhood brain tumors.
Most patients with high-grade astrocytomas or gliomas will eventually have tumor recurrence. Recurrences usually occur within 3 years of original diagnosis, but some patients recur many years after initial treatment. Disease may recur at the primary tumor site, at the margin of the resection/radiation bed, or at noncontiguous central nervous system sites. Systemic relapse rarely occurs.
At the time of recurrence, a complete evaluation for extent of relapse is indicated for all malignant tumors. Biopsy or surgical resection may be necessary for confirmation of relapse because other entities, such as secondary tumor and treatment-related brain necrosis, may be clinically indistinguishable from tumor recurrence.
Treatment options for recurrent childhood high-grade astrocytomas include the following:
- Targeted therapy with a BRAF inhibitor, for patients with a BRAF V600E mutation.
Surgery
The utility of surgical intervention must be individualized on the basis of the following:
- Initial tumor type.
- Length of time between initial treatment and the reappearance of the mass lesion.
- Location of the recurrent tumor.
- Consideration of therapeutics based on the requirement for fresh tumor tissue or to deliver therapy to the operative bed.
High-dose chemotherapy with SCT
High-dose, marrow-ablative chemotherapy with hematopoietic SCT may be effective in a highly selected subset of patients with minimal residual disease at time of recurrence.[1][Level of evidence: 3iiiA] However, the results of previous clinical trials that tested various targeted and combination chemotherapies have largely failed to demonstrate convincing benefits for enrolled patients.[2-4]
Radiation therapy
Radiation therapy is appropriate for patients who have not previously been irradiated. Radiation doses and volumes are similar to those used for newly diagnosed patients. Generally, this is limited to young children initially treated with radiation-avoiding strategies.
For previously irradiated patients, reirradiation has been used, although the data demonstrating benefit are sparse. Stereotactic radiosurgery (SRS) or stereotactic radiation therapy (SRT) techniques using either hypofractionated radiation therapy or standard fraction sizes may be considered. For small volume distinct lesions, SRS allows for maximum sparing of normal tissues. For more infiltrative lesions, fractionated radiation therapy may better spare normal tissues.[5]
Targeted therapy
Molecular targets for recurrent high-grade gliomas are limited. BRAF V600E mutations are present in a small subset of these patients, and a small number of cases have responded to BRAF inhibitors.
A case report documented a complete response to the BRAF inhibitor vemurafenib in a patient with recurrent BRAF V600–mutated glioblastoma.[6] A phase I study reported in an abstract that eight children with progressive BRAF V600E high-grade gliomas were treated with dabrafenib and demonstrated three complete responses, three partial responses, and two progressive disease responses.[7]
Treatment options under clinical evaluation
The role of immune checkpoint inhibition in the treatment of children with recurrent high-grade astrocytoma is currently under study. Children with biallelic mismatch repair deficiency have a very high mutational burden and neoantigen expression and are at risk of developing a variety of cancers, including hematologic malignancies, gastrointestinal cancers, and brain tumors. The high mutation and neoantigen load has been correlated with improved response to immune checkpoint inhibition. Early case reports have demonstrated clinical and radiographic responses in children who are treated with an anti–programmed death-1 (anti–PD-1) inhibitor.[8]
Patients for whom initial treatment fails may benefit from additional treatment, including entry into clinical trials of novel therapeutic approaches.[9] Early-phase therapeutic trials may be available for selected patients. These trials may be available via the Children's Oncology Group (COG), the Pediatric Brain Tumor Consortium, or other entities. Information about NCI-supported clinical trials can be found on the NCI website. For information about clinical trials sponsored by other organizations, refer to the ClinicalTrials.gov website.
The following are examples of national and/or institutional clinical trials that are currently being conducted:
- APEC1621 (NCT03155620) (Pediatric MATCH: Targeted Therapy Directed by Genetic Testing in Treating Pediatric Patients with Relapsed or Refractory Advanced Solid Tumors, Non-Hodgkin Lymphomas, or Histiocytic Disorders): NCI-COG Pediatric Molecular Analysis for Therapeutic Choice (MATCH), referred to as Pediatric MATCH, will match targeted agents with specific molecular changes identified using a next-generation sequencing targeted assay of more than 4,000 different mutations across more than 160 genes in refractory and recurrent solid tumors. Children and adolescents aged 1 to 21 years are eligible for the trial.Tumor tissue from progressive or recurrent disease must be available for molecular characterization. Patients with tumors that have molecular variants addressed by treatment arms included in the trial will be offered treatment on Pediatric MATCH. Additional information can be obtained on the NCI website and ClinicalTrials.gov website.
- NCT02684058 (Phase II Pediatric Study With Dabrafenib in Combination With Trametinib in Patients With High-Grade Gliomas and Low-Grade Gliomas): The purpose of this study is to investigate the activity of dabrafenib in combination with trametinib in children and adolescent patients with BRAF V600 mutation–positive low-grade gliomas or relapsed or refractory high-grade gliomas.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Finlay JL, Dhall G, Boyett JM, et al.: Myeloablative chemotherapy with autologous bone marrow rescue in children and adolescents with recurrent malignant astrocytoma: outcome compared with conventional chemotherapy: a report from the Children's Oncology Group. Pediatr Blood Cancer 51 (6): 806-11, 2008. [PMC free article: PMC2844080] [PubMed: 18802947]
- Fouladi M, Nicholson HS, Zhou T, et al.: A phase II study of the farnesyl transferase inhibitor, tipifarnib, in children with recurrent or progressive high-grade glioma, medulloblastoma/primitive neuroectodermal tumor, or brainstem glioma: a Children's Oncology Group study. Cancer 110 (11): 2535-41, 2007. [PubMed: 17932894]
- Nicholson HS, Kretschmar CS, Krailo M, et al.: Phase 2 study of temozolomide in children and adolescents with recurrent central nervous system tumors: a report from the Children's Oncology Group. Cancer 110 (7): 1542-50, 2007. [PubMed: 17705175]
- Wetmore C, Daryani VM, Billups CA, et al.: Phase II evaluation of sunitinib in the treatment of recurrent or refractory high-grade glioma or ependymoma in children: a children's Oncology Group Study ACNS1021. Cancer Med 5 (7): 1416-24, 2016. [PMC free article: PMC4944867] [PubMed: 27109549]
- Tsang DS, Oliveira C, Bouffet E, et al.: Repeat irradiation for children with supratentorial high-grade glioma. Pediatr Blood Cancer 66 (9): e27881, 2019. [PubMed: 31207154]
- Robinson GW, Orr BA, Gajjar A: Complete clinical regression of a BRAF V600E-mutant pediatric glioblastoma multiforme after BRAF inhibitor therapy. BMC Cancer 14: 258, 2014. [PMC free article: PMC3996187] [PubMed: 24725538]
- Kieran MW, Hargrave DR, Cohen KJ, et al.: Phase 1 study of dabrafenib in pediatric patients (pts) with relapsed or refractory BRAF V600E high- and low-grade gliomas (HGG, LGG), Langerhans cell histiocytosis (LCH), and other solid tumors (OST). [Abstract] J Clin Oncol 33 (15 Suppl): A-10004, 2015.
- Bouffet E, Larouche V, Campbell BB, et al.: Immune Checkpoint Inhibition for Hypermutant Glioblastoma Multiforme Resulting From Germline Biallelic Mismatch Repair Deficiency. J Clin Oncol 34 (19): 2206-11, 2016. [PubMed: 27001570]
- Warren KE, Gururangan S, Geyer JR, et al.: A phase II study of O6-benzylguanine and temozolomide in pediatric patients with recurrent or progressive high-grade gliomas and brainstem gliomas: a Pediatric Brain Tumor Consortium study. J Neurooncol 106 (3): 643-9, 2012. [PMC free article: PMC3518022] [PubMed: 21968943]
Changes to this Summary (07/06/2020)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
This summary was reformatted.
This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® - NCI's Comprehensive Cancer Database pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the treatment of childhood astrocytomas. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Childhood Astrocytomas Treatment are:
- Kenneth J. Cohen, MD, MBA (Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Hospital)
- Louis S. Constine, MD (James P. Wilmot Cancer Center at University of Rochester Medical Center)
- Karen J. Marcus, MD, FACR (Dana-Farber Cancer Institute/Boston Children's Hospital)
- Roger J. Packer, MD (Children's National Health System)
- D. Williams Parsons, MD, PhD
- Malcolm A. Smith, MD, PhD (National Cancer Institute)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Astrocytomas Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/brain/hp/child-astrocytoma-treament-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389382]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
Based on the strength of the available evidence, treatment options may be described as either “standard” or “under clinical evaluation.” These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.
- General Information About Childhood Astrocytomas
- Stage Information for Childhood Astrocytomas
- Treatment Option Overview for Childhood Astrocytomas
- Treatment of Childhood Low-Grade Astrocytomas
- Treatment of Progressive/Recurrent Childhood Low-Grade Astrocytomas
- Treatment of Childhood High-Grade Astrocytomas
- Treatment of Recurrent Childhood High-Grade Astrocytomas
- Changes to this Summary (07/06/2020)
- About This PDQ Summary
- Review Childhood Astrocytomas Treatment: Patient Version.[PDQ Cancer Information Summari...]Review Childhood Astrocytomas Treatment: Patient Version.. PDQ Cancer Information Summaries. 2002
- Review Childhood Brain Stem Glioma Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Brain Stem Glioma Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Brain and Spinal Cord Tumors Summary Index (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Brain and Spinal Cord Tumors Summary Index (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Craniopharyngioma Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Craniopharyngioma Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Review Childhood Ependymoma Treatment (PDQ®): Health Professional Version.[PDQ Cancer Information Summari...]Review Childhood Ependymoma Treatment (PDQ®): Health Professional Version.PDQ Pediatric Treatment Editorial Board. PDQ Cancer Information Summaries. 2002
- Childhood Astrocytomas Treatment (PDQ®) - PDQ Cancer Information SummariesChildhood Astrocytomas Treatment (PDQ®) - PDQ Cancer Information Summaries
- Homo sapiens paired immunoglobin like type 2 receptor alpha (PILRA), transcript ...Homo sapiens paired immunoglobin like type 2 receptor alpha (PILRA), transcript variant 1, mRNAgi|1520687840|ref|NM_013439.3|Nucleotide
- RecName: Full=Phosphoribosyl pyrophosphate synthase-associated protein 1; Short=...RecName: Full=Phosphoribosyl pyrophosphate synthase-associated protein 1; Short=PRPP synthase-associated protein 1; AltName: Full=39 kDa phosphoribosypyrophosphate synthase-associated protein; Short=PAP39gi|24418495|sp|Q14558.2|KPRA_HUMANProtein
- Homo sapiens annexin A2 (ANXA2), transcript variant 2, mRNAHomo sapiens annexin A2 (ANXA2), transcript variant 2, mRNAgi|50845385|ref|NM_001002857.1|Nucleotide
Your browsing activity is empty.
Activity recording is turned off.
See more...