NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Saldanha IJ, Adam GP, Kanaan G, et al. Postpartum Care up to 1 Year After Pregnancy: A Systematic Review and Meta-Analysis [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2023 Jun. (Comparative Effectiveness Review, No. 261.)
Postpartum Care up to 1 Year After Pregnancy: A Systematic Review and Meta-Analysis [Internet].
Show detailsC.1. Results of Literature Searches
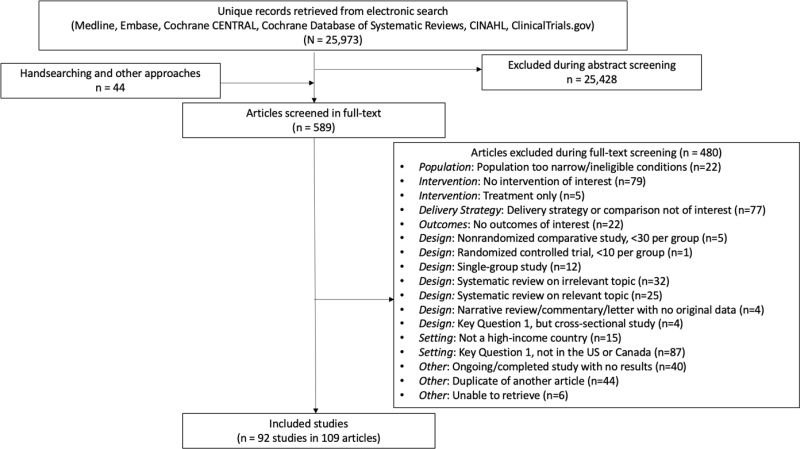
As illustrated by Figure C-1, our electronic search retrieved a combined 25,973 unique citations. Of these, 589 were deemed potentially relevant and retrieved in full text. After full-text screening, we identified 92 eligible studies that were reported in 109 articles.
C.2. Description of Included Studies
C.2.1. Overall Summary of Study Characteristics
The 92 included studies (reported in 109 articles1–84) were published between 1990 and 2022.
The studies enrolled a total of 3,967,261 participants. The 92 studies comprised 50 randomized controlled trials (RCTs) and 25 nonrandomized comparative studies (NRCSs; observational cohort studies). The 50 RCTs enrolled 477,954 participants, and the 42 NRCSs enrolled 3,489,307 participants.
Tables C-1 to C-2.2 summarize the design, arm, and baseline details of all 92 studies. Tables C-1.1 to C-1.3 address KQ 1 and Tables C-2.1 and C-2.2 address KQ 2. Eighty-three (90%) were conducted in the United States and 9 (10%) were conducted in Canada. All 9 Canadian studies addressed KQ 1 (we restricted KQ 2 to U.S.-based studies).
C.2.2. Summary of Patient Characteristics
When reported, average patient ages ranged from 17 to 34 years. When reported, average BMIs ranged from 27 to 41 kg/m2. Study participants were diverse racially; between 3 and 96 percent were White and between 2 and 89 percent were Black. Three studies selectively enrolled Black individuals and one selectively enrolled Hispanic (or Latinx) individuals.
In one study, all participants were employed; among the other studies that reported data, between 15 and 85 percent of participants were employed. No study reported on participant gender or sexual identity status. Only two studies reported on substance use disorders; 2% and 9% of participants had substance use disorders. Where reported, between 57 and 88 percent of deliveries were vaginal and between 8 and 22 percent of deliveries were preterm. Twenty-three studies explicitly reported excluding postpartum individuals with deliveries that had resulted in stillbirths, spontaneous or induced abortions, or neonatal deaths.
C.3. Risk of Bias Assessments
Tables D-1.1 to D-2.2 summarize the risk of bias assessment of all 92 studies. Tables D-1.1 to D-1.3 address KQ 1 and Tables D-2.1 and D-2.2 address KQ 2. Tables D-1 to D-4 summarize the 92 studies. Among the 50 RCTs, we rated five at low risk of bias, 25 at moderate risk, and 20 at high risk. Moderate and high-risk ratings were generally related to the lack of blinding of participants, care providers, and outcome assessors, and incomplete outcome data. Among the 42 NRCSs, we rated 28 at moderate risk of bias and 14 at high risk. Moderate ratings were related to moderate or serious risk of confounding and the lack of blinding of participants, care providers, and outcome assessors.
Table C-1.1Key Question 1: Healthcare delivery strategies – summary of design details
| Delivery Strategy Compared | Target of Intervention | Study, Publication Year, PMID, Country | Design, Direction if NRCS, (Funding) (Study Years) | Registration Number | Overall RoB | Inclusion Criteria | Exclusion Criteria | Study N |
|---|---|---|---|---|---|---|---|---|
| Where | Breastfeeding care | Lieu, 2000, 10790463, US | RCT, (Non-industry) (1996–1997) | NR | Moderate | Overall pregnant population Low medical risk | NR | 1163 |
| Where | Breastfeeding care | Gagnon, 2002, 12042545, Canada | RCT, (NR) (NR) | NR | Moderate | Gestational age ≥37 wk Overall pregnant population Breastfed at least once in hospital | Caesarean delivery, parity ≥5, multiple gestation, birth weight <2500g | 586 |
| Where | General PP care | Norr, 2003, 12716399, US | RCT, (Non-industry) (NR) | NR | Moderate |
Low-income African American or Mexican American Medicaid or state supplemental health insurance, neighborhood with high infant mortality, medically low risk, no current drug use | Current drug use | 477 |
| Where | Breastfeeding care | Escobar, 2001, 11533342, US | RCT, (Non-industry) (1998–1999) | NR | High |
Gestational age 36–42 wk Overall pregnant population Low medical and social risk |
Infant weight 2500–4600g/NICU admission Newborn hematocrit <40 or neutrophil <7000 Anticipated stay >48 hours Age ≤14 Age 15 to 17 without parent or a guardian Positive toxicology screen for drugs of abuse after admission to labor | 1014 |
| Where | General PP care | Steel O’Connor, 2003, 12675164, Canada | RCT, (Non-industry) (1997–1999) | NR | High | Primiparas, singleton infant, vaginal delivery | NR | 733 |
| Where | General PP care | McCarter, 2019, 31222789, US | RCT, (NR) (20172019) | NR | High |
Age ≥18 English-speaking | NR | 357 |
| Where | Breastfeeding care | Paul, 2012, 22064874, US | RCT, (Non-industry) (2006–2010) | NCT00360204 | High | singleton or twins born ≥34 wk gestation | ≥2night stay post vaginal delivery, ≥4night stay post Caesarean, atypical complications in hospital, newborn hyperbilirubinemia, major morbidities, and/or preexisting conditions | 1154 |
| Where | General PP care | Arias, 2022, 35331971, US | NRCS, Retrospective, (Non-industry) (2019–2019) | NR | Moderate | PP visit scheduled at institution March-June 2019 | NR | 1579 |
| Where, Who | General PP care | Dodge, 2019, 31675088, US | RCT, (Non-industry) (2014–2014) | NCT01843036 | Moderate | Overall postpartum population | Residence outside of Durham County Previously enrolled patient | 316 |
| Where, Who | Breastfeeding care | Pugh, 2002, 12000411, US | RCT, (Non-industry) (1999–2000) | NR | Moderate | Low-income women receiving financial medical assistance support | NR | 41 |
| Where, Who | General PP care | Mersky, 2021, 33078655, US | RCT, (Not funded) (NR) | NR | High | Low-income | NR | 237 |
| Where, Who | Breastfeeding care | Pugh, 2010, 19854119, US | RCT, (Non-industry) (NR) | NR | High |
Gestational age >37 wk Eligible for WIC Caesarean | Infant craniofacial abnormality, NICU admission, positive drug screen for mother/infant | 328 |
| Where, Who | Breastfeeding care | Edwards, 2013, 24187119, US | RCT, (Non-industry) (2001–2004) | NCT01925664 | High |
Age ≤21 Gestational age ≤34 wk Low-income | NR | 248 |
| Where, Who | Breastfeeding care | Gill, 2007, 17557933, US | NRCS, Prospective, (Non-industry) (NR) | NR | High |
Gestational age 2nd trimester Low-income Hispanic | Premature birth, low-birth weight, major congenital anomalies, NICU admission | 158 |
| How | General PP care | Polk, 2021, 34671758, US | RCT, (Non-industry) (2015–2016) | NR | Moderate |
Age >18 Low-income | NICU admission | 116 |
| How | General PP care | Koniak-Griffin, 2003, 12657988, US | RCT, (Non-industry) (NR) | NR | Moderate |
Age 14–19 Gestational age ≤26 wk Single, poor, underrepresented ethnicity | Dependent on narcotic or IV drugs, serious OB/medical condition | 101 |
| How, Who | General PP care | Hans, 2018, 29855838, US | RCT, (Non-industry) (2011–2015) | NCT01947244 | High |
Age 14–24 Gestational age 12–34 wk Living in high-poverty communities | NR | 312 |
| How | Contraceptive care | Haider, 2020, 31964564, US | RCT, NR, (2015–2017) | NR | Moderate | Infant ≤4.5 months, no previous LARC/sterilization, not currently pregnant | NR | 446 |
| How | General PP care | Laliberte, 2016, 26871448, Canada | RCT, (Non-industry) (NR) | NCT02043119 | Moderate |
Age ≥18 Gestational age ≥36 wk Singleton infant, no medical problems, breastfeeding | Multiple births, preterm infant | 428 |
| How | Breastfeeding care | Rozga, 2016, 27423234, US | NRCS, Prospective, (Industry) (2012–2014) | NR | Moderate | ≤185% of federal poverty level | NR | 698 |
| How | Breastfeeding care | Witt, 2021, 33956505, US | NRCS, Retrospective, (Non-industry) (2016–2019) | NR | Moderate | NR | NR | 442 |
| When | General PP care | Bernard, 2018, 29778586, US | RCT, (Industry and non-industry) (2016–2017) | NCT02769676 | Moderate |
Age 14–45 Gestational age ≥36 wk Overall pregnant population Live birth | Incarcerated, received immediate PP LARC or sterilization | 188 |
| When | General PP care | Pluym, 2021, 33785465, US | RCT, (Not funded) (2018–2020) | NCT03733405 | Moderate |
Age 18–50 Gestational age >35 wk | NR | 250 |
| When | General PP care | Chen, 2019, 30414598, US | NRCS, Retrospective, (Non-industry) (2015–2019) | NR | Moderate |
Gestational age ≥28 wk Overall pregnant population | NR | 512 |
| When | Contraceptive care | Dahlke, 2011, 21843688, US | RCT, (Not funded) (2009–2010) | NCT01088178 | Low |
Age 16–45 Overall pregnant population | Uterine or cervical neoplasia | 46 |
| When | Contraceptive care | Chen, 2010, 20966692, US | RCT, (Non-industry) (2007–2008) | NCT00476021 | Moderate |
Age ≥18 Gestational age ≥24 wk Overall pregnant population Planned vaginal delivery | Gonorrhea, chlamydia, or trichomoniasis during pregnancy | 102 |
| When | Contraceptive care | Levi, 2015, 26241250, US | RCT, (Non-industry) (2012–2014) | NCT01539759 | Moderate |
Age 18–45 Gestational age ≥24 wk Overall pregnant population Live birth, Caesarean delivery | Gonorrhea or chlamydia, cervical, uterine, or breast neoplasia, chorioamnionitis | 112 |
| When | Contraceptive care | Dempsey, 2018, N/A, US | RCT, (Industry and non-industry) (2010–2013) | NCT03585504 | Moderate |
Age 15–21 Overall pregnant population <5 days PP | Breastfeeding | 81 |
| When | Contraceptive care | Baldwin, 2019, N/A, US | RCT, (Non-industry) (2012–2014) | NCT01594476 | Moderate |
Age 18–50 Gestational age ≥32 wk | Preterm delivery, recent pregnancy with multiple gestation | 197 |
| When | Contraceptive care | Whitaker, 2014, 24457061, US | RCT, (Non-industry) (2007–2011) | NCT00635362 | High |
Age ≥18 Scheduled Caesarean delivery | Current cervical cancer or CIS | 42 |
| When | Contraceptive care | Morse, 2016, N/A, US | RCT, (Non-industry) (2013–2015) | NCT01767285 | High | Age 12–40 | NR | 59 |
| When | Contraceptive care | Chen, 2018, N/A, US | RCT, (Non-industry) (2011–2017) | NCT01463202 | High |
Age ≥18 Gestational age > 24 wk Overall pregnant population Planning to breastfeed, use DMPA for postpartum contraception | Intolerance of irregular vaginal bleeding, coagulation disorder, liver disease, contraindications to breastfeeding, history of breast cancer, reduction or augmentation surgery, history of severe clinical depression, multiple gestation | 157 |
| When | Contraceptive care | Jensen, 2019, N/A, US | RCT, (Non-industry) (2014–2017) | NCT02169869 | High |
Age 18–55 Gestational age ≥32 wk Overall pregnant population Singleton pregnancy | NR | 33 |
| Who | General PP care | Kozhimannil, 2013, 23837663, US | NRCS, Retrospective, (Non-industry) (NR) | NR | Moderate | Medicaid coverage for childbirth Singleton, live birth | NR | 52790 |
| Who | General PP care | Pan, 2020, 32437282, US | NRCS, Prospective, (NR) (2015–2017) | NR | Moderate | Social and economic risk factors | NR | 455 |
| Who | General PP care | Edwards, 1997, 9170692, Canada | RCT, (Non-industry) (NR) | NR | Low |
Gestational age ≥35 wk Overall pregnant population Primiparous, singleton birth, no congenital anomalies | NR | 788 |
| Who | Breastfeeding care | Falconi, 2022, 35812994, US | NRCS, Retrospective, (Not funded) (2014–2020) | NR | High |
Age 12−51 High risk for adverse maternal health outcomes At least one ICD-9 or ICD-10 claim Medicaid eligibility | NR | 596 |
| Who | General PP care | Buckley, 1990, 2328162, US | NRCS, Prospective, (NR) (NR) | NR | High | NR | NR | 59 |
| Who | General PP care, screening/ preventive education | Tandon, 2021, 33655429, US | RCT, (Non-industry) (2017–2019) | NCT02979444 | High |
Age ≥16 Gestational age ≤33 wk | NR | 824 |
| Who | Contraceptive care | Simmons, 2013, 23218851, US | RCT, (Non-industry) (2011–2012) | NR | Low |
Age 18–38 Medicaid insurance, English or Spanish speaking, intention to use LARC | Incarcerated at time of delivery | 49 |
| Who | Breastfeeding care | Dennis, 2002, 11800243, Canada | RCT, (Non-industry) (1997–1998) | NR | Low |
Age ≥16 Gestational age ≥37 wk Primiparous, breastfeeding | Serious illness, infant congenital abnormality, NICU admission | 256 |
| Who | Breastfeeding care | Reeder, 2014, 25092936, US | RCT, (Non-industry) (2005–2007) | NCT02120248 | Low | Low-income women/WIC participants | NR | 1885 |
| Who, IT | Breastfeeding care | Gross, 1998, 12515413, US | RCT, (Non-industry) (1992–1994) | NR | Moderate |
Gestational age <24 wk WIC eligible Singleton pregnancy | Breastfeeding contraindicated | 115 |
| Who | Breastfeeding care | Anderson, 2005, 16143742, US | RCT, (Non-industry) (2003–2004) | NR | Moderate |
Age ≥18 Gestational age ≤32 wk Low-income Term delivery | Diabetes, hypertension, HIV/AIDS, using illegal drugs | 135 |
| Who | Breastfeeding care | Chapman, 2004, 15351756, US | RCT, (Non-industry) (2000–2003) | NR | High |
Age ≥18 Gestational age ≤26 wk Low-income Healthy, full-term singleton infants | HIV, infant congenital anomalies | 165 |
| Who | Breastfeeding care | Wambach, 2011, 20876551, US | RCT, (Non-industry) (2003–2007) | NR | High |
Age 15–18 Gestational age 2nd trimester Pregnant with first child, planning to keep newborn, Englishspeaking, phone access | Multiple-gestation, preterm labor, infant cleft lip/palate, heart defect, Down’s syndrome, neural tube defects, NICU admission | 390 |
| Who | Breastfeeding care | Chapman, 2013, 23209111, US | RCT, (Non-industry) (2006–2009) | NCT01338727 | High |
Age ≥18 Gestational age ≤36 wk Income ≤185% federal poverty level Pre-pregnancy BMI ≥27.0 Breastfeeding, singleton pregnancy, no conditions interfering with breastfeeding | NR | 154 |
| Who | Breastfeeding care | Srinivas, 2015, 25193602, US | RCT, (Non-industry) (2011–2012) | NR | High |
Age ≥18 Gestational age ≥28 wk | Non-English, contraindication to breastfeeding | 103 |
| Who, IT | Breastfeeding care, screening/preventive education | Kerver, 2019, N/A, US | RCT, (Non-industry) (2017–2018) | NCT03480048 | High |
Age 18–55 With obesity African American | High-risk pregnancy | 53 |
| Who | Breastfeeding care | Porteous, 2000, 11155608, Canada | RCT, (Non-industry) (NR) | NR | Moderate | Overall pregnant population Singleton pregnancy, vaginal delivery | NR | 51 |
| Who | Breastfeeding care | Rasmussen, 2011, 20958105, US | RCT, (Non-industry) (2006–2007) | NR | Moderate |
Age ≥19 Gestational age ≤35 wk With obesity Singleton pregnancy | NR | 40 |
| Who, Provider Interventio ns | Breastfeeding care | Bonuck, 2014a, 24354834, US | RCT, (Non-industry) (2008–2013) | NCT00619632 | Moderate |
Age ≥18 Gestational age 1st or 2nd trimester Overall pregnant population | High risk of prematurity/NICU, use of illicit drugs | 628 |
| Who, Provider Interventio ns | Breastfeeding care | Bonuck, 2014b, 24354834, US | RCT, (Non-industry) (2008–2013) | NCT00643253 | Moderate |
Age ≥18 Gestational age 12–30 wk Overall pregnant population | Multiple gestation | 262 |
| Who, IT | Breastfeeding care | Uscher-Pines, 2020, 31629118, US | RCT, (Non-industry) (2016–2018) | NCT02870413 | High |
Age 18–46 Gestational age ≥35 wk Singleton birth, initiated breastfeeding | Infant cardiac defect, infant ventilator dependence, NICU admission, HIV+ | 187 |
| Coordination/management | General PP care | Rutledge, 2016, 27350389, US | NRCS, Retrospective, (NR) (2008–2010) | NR | Moderate | Medicaid eligibility | Not eligible for Medicaid | 7120 |
| Coordination/management | General PP care | Tsai, 2011, 21365543, US | NRCS, Retrospective, (NR) (2006–2008) | NR | High | Overall pregnant population | NR | 221 |
| Coordination/management | Screening | Mendez-Figueroa, 2014, 24481876, US | NRCS, Retrospective, (Non-industry) (2011–2012) | NR | High | Gestational diabetes | NR | 388 |
| Coordination/management, Provider Interventio ns | Screening | Clark, 2009, 19268878, Canada | RCT, (Non-industry) (2002–2005) | NCT00212914 | Moderate |
Gestational diabetes Attended High-Risk Obstetrical Unit | No family physician Family physician had other patient(s) enrolled Previously enrolled patient Delivered outside of Ottawa Hospital Stillbirth | 223 |
| Coordination/management, IT | Screening | Shea, 2011, 21466755, Canada | NRCS, Prospective, (Non-industry) (2007–2008) | NR | Moderate | Gestational diabetes | NR | 262 |
| IT | Breastfeeding care | Martinez-Brockman, 2018, 29325660, US | RCT, (Non-industry) (2014–2016) | NCT02214849 | Moderate |
Age ≥18 Gestational age ≤28 wk Low-income women in WIC BFPC program Singleton, intention to breastfeed | Withdrawal from BFPC program, multiple gestation, premature birth, history of miscarriage, medication given to mother or baby prior to BF, >3d NICU infant weight <5 lb | 174 |
| IT | Breastfeeding care | Abbass-Dick, 2020, 32739716, Canada | RCT, (Non-industry) (2018–2020) | NCT03492411 | Moderate |
Age ≥18 Gestational age >25 wk Overall pregnant population Primiparous, not previously breastfed, singleton birth | NR | 217 |
| IT | Breastfeeding care | Bender, 2022, 36201773, US | RCT, (NR), (2020–2021) | NCT04108533 | Moderate |
Age ≥18 Gestational age 34–36 wk English-speaking Singleton gestation | Contraindication to breastfeeding Preterm delivery or NICU admission | 216 |
| IT | Breastfeeding care | Ahmed, 2016, 26779838, US | RCT, (Non-industry) (NR) | NR | High |
Age ≥18 Gestational age ≥37 wk | HIV | 106 |
| Provider Interventions | Screening | Domingo, 2022, 35237835, US | NRCS, Retrospective, (NR), (2016–2020) | NR | Moderate | Gestational diabetes | History of pregestational diabetes | 246 |
Table C-1.2Key Question 1: Healthcare delivery strategies – summary of arm details
| Delivery Strategy Compared | Study, Publication Year, PMID | Target | Location | Facility Volume, Type, Academic Status, Level (Only if Reported) | Arm N | Arm Name | Delivery Strategy: Where, How, Who, Coordination, IT (as Relevant) | Delivery Strategy: When: AP, In Hosp, After Discharge (as Relevant) |
|---|---|---|---|---|---|---|---|---|
| Where | Lieu, 2000, 10790463 | BF care | NR | NR | 580 | Home visit by nurse on day 3 or 4 PP |
Where: Home How: Home visit Who: Nurse | After discharge: 1 time; 1–1.5 hr; day 3 or 4 |
| . | . | . | . | 583 | Pediatric clinic visit on day 3 or 4 PP |
Where: Clinic, How: As part of well-child visit, Who: Pediatrician, nurse practitioner | After discharge: 1 time; 20 min; day 3 or 4 | |
| Where | Gagnon, 2002, 12042545 | BF care | Urban | NR | 292 | Home visit by community nurse |
Where: Home How: Dedicated PP visit Who: Nurse |
In hosp: 1 time; 2 d After discharge: 1 time; 1 hr; 3–4 d after discharge |
| . | . | . | . | 294 | Hospital visit with nurse |
Where: Hospital How: Dedicated PP visit Who: Nurse |
In hosp: 1 time; 2 d After discharge: 1 time; 1 hr; 3–4 d after discharge | |
| Where | Norr, 2003, 12716399 | General PP care | Urban | Academic, community | 258 | Home visits by nurse-led community worker team |
Where: Clinic, Home How: Dedicated PP visit, as part of well-child visit, home visit Who: Nurse, community health worker | After discharge: 12 times; monthly |
| . | . | . | . | 219 | Routine PP and well-baby visits with current provider |
Where: Clinic How: Dedicated PP visit, as part of well-child visit, Who: Pediatrician, provider of mother’s choice | After discharge: 1 time; PP visit | |
| Where | Escobar, 2001, 11533342 | BF care | Urban | NR | 506 | Home visit by nurse on day 3 or 4 PP |
Where: Home How: Dedicated newborn and BF visit Who: Nurse | After discharge: 1 time; 1–1.5 hr; day 3 or 4 PP |
| . | . | . | . | 508 | Hospital visit on day 3 or 4 PP |
Where: Hospital, How: Dedicated newborn and BF visit Who: Nurse | After discharge: 1 time; 1.5–2 hr; day 3 or 4 PP | |
| Where | Steel O’Connor, 2003, 12675164 | General PP care | Urban | Tertiary | 380 | Telephone visit by public health nurse |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: Nurse IT: Phone visits | After discharge: 1 time; 1st working d post-discharge |
| . | . | . | . | 353 | Home visit by public health nurse |
Where: Home How: Home visit Who: Nurse | After discharge: 2 times; 1st working d post-discharge & ≤10 d post-discharge | |
| Where | McCarter, 2019, 31222789 | General PP care | Urban | Community/Pri mary | 190 | Telephone-based nursing care |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: Nurse IT: Phone visits, Smartphone or computer applications |
AP: N/A In Hospital: N/A, After Discharge: Total 104 times, 4x/wk for 26 wks. |
| . | . | . | . | 167 | Usual care |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: Nurse IT: Phone visits |
AP: In Hospital: After Discharge: One time within PP 2 wks | |
| Where | Paul, 2012, 22064874 | BF care | NR | NR | 576 | First PP visit at home |
Where: Home How: Home newborn and BF visit Who: Nurse | After discharge: 1 time; 3–5 d after delivery |
| . | . | . | . | 578 | First PP visit in clinic |
Where: Clinic How: Dedicated newborn and BF visit Who: OB/GYN | After discharge: 1 time; 3–5 d after delivery | |
| Where | Arias, 2022, 35331971 | General PP care | Urban | Academic | 799 | Virtual visits |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: Obstetrics provider through telehealth. IT: Bidirectional telemedicine/virtual tele-visits |
AP: N/A In Hospital: N/A After Discharge: N/A |
| . | . | . | . | 780 | In-person visits |
Where; Hospital How: Dedicated PP visit Who: obstetrics provider IT: Primarily in-person |
AP: N/A, In Hospital: N/A, After Discharge: N/A | |
| Where, Who | Dodge, 2019, 31675088 | General PP care | Urban | Academic | 158 | Nurse home visitation through Family Connects (FC) Program |
Where: Home How: Home visit Who: Nurse, Community Agency-Administered Nurse. Coordination: Child preventive service and family support IT: Primarily in-person |
AP: N/A In Hospital: In-hospital support After Discharge: 1–3 home visits |
| . | . | . | . | 158 | Usual care |
Where: NR How: NR Who: NR Coordination: NR IT: NR |
AP: NR In Hospital: NR After Discharge: NR | |
| Where, Who | Pugh, 2002, 12000411 | Breastfeeding care | NR | High large, Academic | 21 | Home visits by peer counselors |
Where: Hospital, Home, Telehealth/e-Health, How: Home visit, Telehealth/virtual visit Who: Nurse, peer counselor IT: Phone visits |
AP: N/A In Hospital: N/A After Discharge: at least 3 times for 6 months, week 1, 2, 4, and at teams discretion. |
| . | . | . | . | 20 | Usual care |
Where: Hospital How: N/A Who: Nurse IT: N/A |
AP: NR In Hospital: 1 time After Discharge: NR | |
| Where, Who | Mersky, 2021, 33078655 | General PP care | Urban | N/A | 72 | Home visits by human service professions through the Healthy Families American Program |
Where: Home How: Home visit Who: Human service professionals | After discharge: 24 times; 1 hr; 6 mo; wkly |
| . | . | . | . | 65 | Home visits by public health nurses through the Prenatal Care and Coordination Program |
Where: Home How: Home visit Who: Nurse | After discharge: 4 times; 1 hr; 2 mo; bi-wkly | |
| . | . | . | . | 100 | No home visits | N/A | N/A | |
| Where, Who | Pugh, 2010, 19854119 | BF care | Urban | Public | 168 | BF support team inpatient and home visits and pager access |
Where: Hospital, home, telehealth/e-health How: Dedicated PP visit, home visit, telehealth/virtual visit Who: Nurse, peer IT: Primarily in-person, phone visits |
In hosp: unlimited After discharge: 3 home (45–60 min each; 2 within 1 wk and third at 4 wk), 12 phone (20 min each; biwkly) |
| . | . | . | . | 160 | Inpatient visits by lactation consultant and home telephone access |
Where: Hospital, Telehealth/e-Health, How: Dedicated PP visit, Telehealth/virtual visit, Who: Lactation consultant IT: Primarily in-person, phone visits |
In hosp: unlimited After discharge: unlimited | |
| Where, Who | Edwards, 2013, 24187119 | BF care | Urban | Community/ | 124 | Home visits by doulas |
Where: Clinic, home How: Home visit Who: Doula |
AP: 10 times; 3rd trimester; wkly In hosp: 1 time After discharge: 12 times; 3 mo; wkly |
| . | . | . | . | 124 | Standard care without home visits by doulas |
Where: Clinic How: Dedicated PP visit | NR | |
| Where, Who | Gill, 2007, 17557933 | BF care | Urban | Low-volume, academic | 79 | Telephone calls from research team and as needed lactation consultant home visits |
Where: Clinic, Home, Telephone How: Dedicated PP visit, Telephone Who: Lactation consultant, research staff IT: Primarily in-person, Telephone |
AP: 2 times In hosp: NR After discharge: 9 calls; 4 d, 2 wk, 3 wk, 4 wk, 6 wk, 3 mo, 4 mo, 5 mo, 6 mo |
| . | . | . | . | 79 | Standard BF education in clinic and/or WIC site |
Where: Clinic, WIC Program office/site, How: Dedicated PP visit, WIC site, Who: Research staff | NR | |
| How | Polk, 2021, 34671758 | General PP care | Urban | Tertiary | 58 | Combined PP/well-child visit at 4 wk |
Where: Clinic How: As part of well-child visit Who: OB/GYN, pediatrician | After discharge: 1 time; 4 wk |
| . | . | . | . | 58 | Separate PP and well-child visits |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time | |
| How | Koniak-Griffin, 2003, 12657988 | General PP care | NR | Academic, tertiary | 56 | Early Intervention Program |
Where: Home, telephone How: Home visit Who: Public health nurse |
AP: 2 times; 1.5–2 hr In hosp: NR After discharge: 15 times; 1.5–2 hr; wk 1, 4, 6 & mo 2–12 |
| . | . | . | . | 45 | Traditional Public Health Nursing Care |
Where: Home, telephone How: Home visit Who: Public health nurse |
AP: 2 times In hosp: NR After discharge: 1 time | |
| How, Who | Hans, 2018, 29855838 | General PP care | Urban | NR | 156 | Home visits by doulas and hospital support for childbirth preparation and childbirth |
Where: Hospital, home How: Home visit, hospital Who: Doula, lay support worker |
AP: weekly In hosp: NR After discharge: weekly |
| . | . | . | . | 156 | Case management by community case managers or social service providers |
Where: Community site/center How: Community center Who: Case manager |
AP: 2 times In hosp: NR After discharge: 2 times | |
| How | Haider, 2020, 31964564 | Contraceptive care | Urban | NR | 231 | Contraceptive counseling at well-baby visit |
Where: Clinic How: As part of well-child visit Who: OB/GYN, nurse midwife IT: Primarily in-person | After discharge: 1 time |
| . | . | . | . | 215 | Contraceptive counseling at routine PP visit |
Where: Clinic How: Dedicated PP visit Who: OB/GYN IT: Primarily in-person | After discharge: 1 time | |
| How | Laliberte, 2016, 26871448 | General PP care | NR | Public, community | 294 | Multidisciplinary clinic within 48 hr PP with additional visits as indicated |
Where: Clinic How: Dedicated PP visit Who: Family physician, nurse, lactation consultant | After discharge: 1 time |
| . | . | . | . | 134 | Standard Care |
Where: Clinic How: Dedicated PP visit, Who: Family physician | NR | |
| How | Rozga, 2016, 27423234 | BF care | NR | Public, academic, tertiary | 472 | Home visits, phone calls, and WIC clinical support from peer counselors as part of the BF Initiative Program |
Where: Hospital, Home, Telehealth/e-Health, WIC Program office/site How: Group visit, Home visit, Telehealth/virtual visit, Who: Peer IT: Phone visits |
AP: monthly phone calls until delivery After discharge: wkly phonecalls in first mo, monthly thereafter |
| . | . | . | . | 226 | Standard home visit, phone calls, and hospital contact with peer counselors |
Where: Hospital, Home, Telehealth/e-Health, How: Home visit, Telehealth/virtual visit Who: Peer IT: Phone visits |
AP: one home visit, monthly phone calls until delivery After discharge: wkly phonecalls in first mo, monthly thereafter | |
| How | Witt, 2021, 33956505 | BF care | Urban | NR | 197 | Before integration of lactation consultant and primary care provider care |
Where: Clinic How: Dedicated PP visit Who: Family physician | N/A |
| . | . | . | . | 245 | After integration of lactation consultant and primary care provider care |
Where: Clinic How: Dedicated PP visit Who: Family physician, lactation consultant | After discharge: ≥1 time; 40 min | |
| When | Bernard, 2018, 29778586 | General PP care | Urban, Rural | Public | 93 | Two PP visits (3 & 6 wk) |
Where: Clinic How: Dedicated PP visit Who: Resident, nurse practitioner | After discharge: 2 times; 3 & 6 wk |
| . | . | . | . | 95 | One PP visit (6 wk) |
Where: Clinic How: Dedicated PP visit Who: Resident, nurse practitioner | After discharge: 1 time; 6 wk | |
| When | Pluym, 2021, 33785465 | General PP care | NR | Academic, tertiary | NR | Two PP visits (2 & 6 wk) |
Where: Clinic, How: Dedicated PP visit Who: OB/GYN | After discharge: 2 times; 2 wk & 6 wk |
| . | . | . | . | NR | One PP visit (6 wk) |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 6 wk | |
| When | Chen, 2019, 30414598 | General PP care | Urban | High-volume, public, non-academic | 256 | One PP visit (2–3 wk) |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 2–3 wk |
| . | . | Urban | . | 256 | One PP visit (6 wk) |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 6 wk | |
| When | Dahlke, 2011, 21843688 | Contraceptive care | Urban | High-volume | 15 | Immediate PP levonorgestrel IUD within 10 min after delivery |
Where: Birth center How: After delivery Who: OB/GYN | In hosp: 1 time; ≤10 min after delivery |
| . | . | . | . | 15 | PP levonorgestrel IUD 10 min-48 hr after delivery |
Where: Birth center How: After delivery Who: OB/GYN | In hosp: 1 time; 10 min-48 hr after delivery | |
| . | . | . | . | 16 | PP levonorgestrel IUD at 6 wk PP |
Where: Clinic, How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 6 wk | |
| When | Chen, 2010, 20966692 | Contraceptive care | Urban | NR | 51 | Immediate PP levonorgestrel IUD placement after delivery |
Where: Hospital How: Hospital Who: NR | In hosp: 1 time; before discharge |
| . | . | . | . | 51 | Levonorgestrel IUD placement at 6–8 wk PP visit |
Where: Clinic How: Dedicated PP visit Who: NR | After discharge: 1 time; 6–8 wk | |
| When | Levi, 2015, 26241250 | Contraceptive care | NR | NR | 56 | Immediate PP levonorgestrel or copper IUD after delivery |
Where: Hospital How: After delivery Who: OB/GYN | In hosp: 1 time; after delivery |
| . | . | . | . | 56 | Levonorgestrel or copper IUD at ≥6 wk PP |
Where: Clinic, How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; ≥6 wk | |
| When | Dempsey, 2018, N/A | Contraceptive care | Urban | Non-academic | 41 | Etonogestrel insertion before discharge |
Where: Hospital How: Hospital Who: OB/GYN | In hosp: 1 time; before discharge |
| . | . | . | . | 40 | Etonogestrel insertion at 6 wk PP visit |
Where: Clinic How: Dedicated PP visit | After discharge: 1 time; 6 wk | |
| When | Baldwin, 2019, N/A | Contraceptive care | Urban | Academic, tertiary | 100 | Levonorgestrel IUD placement at 3 wk PP |
Where: Clinic How: Dedicated PP visit | After discharge: 1 time; 3 wk |
| . | . | . | . | 97 | Levonorgestrel IUD placement at 6 wk PP |
Where: Clinic How: Dedicated PP visit | After discharge: 1 time; 6 wk | |
| When | Whitaker, 2014, 24457061 | Contraceptive care | NR | NR | 20 | Immediate levonorgestrel IUD placement after delivery |
Where: Hospital How: After delivery Who: OB/GYN | In hosp: 1 time; after delivery |
| . | . | . | . | 22 | Levonorgestrel IUD placement at 4–8 wk PP visit |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 4–8 wk | |
| When | Morse, 2016, N/A | Contraceptive care | Urban | NR | 29 | Etonogestrel implant before discharge | Where: Hospital | In hosp: 1 time; before discharge |
| . | . | . | . | 30 | Etonogestrel implant at 6 wk PP |
Where: Clinic How: Dedicated PP visit | After discharge: 1 time; 6 wk | |
| When | Chen, 2018, N/A | Contraceptive care | Urban | High-volume, public, non-academic | 79 | PP DMPA administration before discharge |
Where: Hospital How: Hospital Who: OB/GYN | In hosp: 1 time; after delivery |
| . | . | . | . | 78 | PP DMPA administration 4–6 wk PP |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 4–6 wk | |
| When | Jensen, 2019, N/A | Contraceptive care | Urban | Academic | 17 | Immediate PP levonorgestrel IUD placement |
Where: Hospital How: Hospital | In hosp: 1 time; ≤1 hr after delivery |
| . | . | . | . | 16 | Levonorgestrel IUD placement at 6 wk PP visit |
Where: Clinic How: Dedicated PP visit Who: OB/GYN | After discharge: 1 time; 6 wk | |
| Who | Kozhimannil, 2013, 23837663 | General PP care | Suburban | High-volume, public, non-academic, community | 1069 | Doula support through the Everyday Miracles Program |
How: Dedicated PP visit, Who: Doula | NR |
| . | . | . | . | 51721 | No doula supported care | N/A | N/A | |
| Who | Pan, 2020, 32437282 | General PP care | NR | Academic, tertiary | 353 | Home visits by community health worker and referral to social worker through the Baby Love Program |
Where: Home visit How: Home visit Who: Community health worker, social worker | NR |
| . | . | . | . | 102 | Standard care without the Baby Love Program | NR | NR | |
| Who | Edwards, 1997, 9170692 | General PP care | Urban | Public | 279 | Public Health Nurse Telephone Visit |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: Nurse IT: Phone visits | After discharge: 1 time; 1–2 wk after discharge |
| . | . | . | . | 218 | Health Department Clerk Call |
Where: Telehealth/e-Health How: Telehealth/virtual visit, Who: Public health department clerk IT: Phone visits | After discharge: 1 time; 5 wk after discharge | |
| . | . | . | . | 291 | Postpartum education package |
Where: Mail How: Mail | NR | |
| Who | Falconi, 2022, 35812994 | General PP care | NR | NR | 298 | Doula support |
Where: Hospital, How: Dedicated PP visit, Prenatal visit and inhospital labor. Who: OB/GYN, Midwife, Doula. Coordination: integrating doula into maternity care networks. |
AP: at least 4 Prenatal visits In Hospital: supporting during labor and birth. After Discharge: 4 PP visits |
| . | . | . | . | 298 | No doula support |
Where: Hospital How: NR Who: NR Coordination: NR |
AP: NR In Hospital: NR After Discharge: NR | |
| Who | Buckley, 1990, 2328162 | General PP care | Urban | Academic | 34 | PP visit and phone call by nurse practitioner |
Where: Clinic, Telehealth/e-Health How: Dedicated PP visit, telehealth/virtual visit Who: Nurse practitioner IT: Primarily in-person, Phone visits |
In hosp: 1 time; 15 min After discharge: 1 time; 15 min; 1 wk |
| . | . | Urban | . | 25 | No PP visit and phone call by NP | Where: Clinic | N/A | |
| Who | Tandon, 2021, 33655429 | General PP care | Urban | NR | 293 | Home visits by mental health professionals through the Mothers and Babies (MB) Program |
Where: Home, How: Home visit Who: Mental health professional | After discharge: 6 times; 1.5 hr; wkly |
| . | . | . | . | 382 | Home visits by community health workers through the Mothers and Babies (MB) Program |
Where: Home, How: Home visit Who: Community health worker | After discharge: 6 times; 1.5 hr; wkly | |
| . | . | . | . | 149 | Usual home visits (visitor type unspecified) |
Where: Home, How: Home visit | NR | |
| Who | Simmons, 2013, 23218851 | Contraceptive care | Urban | Academic | 25 | Contraceptive Counselor phone calls at 2 wk and clinic visit at 6 wk |
Where: Clinic, Telehealth/e-Health How: Telehealth/virtual visit Who: Contraceptive counselor IT: Phone visits | After discharge: 2 times; 2 wk & 6 wk |
| . | . | . | . | 24 | Clinic visit at 6 wk |
Where: Clinic How: Dedicated PP visit How: Nurse midwife | After discharge: 1 time; 6 wk | |
| Who | Dennis, 2002, 11800243 | BF care | Urban | N/A | 132 | BF peer support and standard care |
Where: Hospital, clinic, community site/center, telephone support How: Telephone, hospital Who: OB/GYN, pediatrician, nurse, lactation consultant, peer IT: Primarily in-person, telephone | NR |
| . | . | . | . | 124 | BF standard care only |
Where: Hospital, clinic, telephone support How: Dedicated PP visit Who: OB/GYN, pediatrician, nurse, lactation consultant IT: Primarily in-person, telephone | NR | |
| Who | Reeder, 2014, 25092936 | BF care | Urban and rural | NR | 1250 | Peer counseling with 4–8 telephone calls and WIC Program |
Where: Telehealth/e-Health How: WIC Program office/site, telehealth/virtual visit Who: Peer |
AP: 2 times; initial assessment and 2 wk before due date After discharge: 2–6 times; 1 wk, 2 wk, 1 mo, 2 mo, 3 mo, & 4 mo |
| . | . | . | . | 635 | WIC Program but no peer counseling |
Where: WIC office/site How: WIC Program Who: WIC staff | NR | |
| Who, IT | Gross, 1998, 12515413 | BF care | NR | NR | 35 | Video and peer counselor BF education |
Where: Telehealth/e-Health, WIC Program office/site Who: Peer IT: Videos |
AP: 9 times; 8 videos, 1 peer visit In hosp: 1 time; 2–5 min video, 1 hr visit After discharge: 1 time; 1hr |
| . | . | . | . | 32 | Peer counselor BF education |
Where: WIC Program office/site Who: Peer |
In hosp: 1 time; 1 hr After discharge: wkly up to 16 wk PP | |
| . | . | . | . | 33 | Video BF education |
Where: Telehealth/e-Health How: Telehealth/virtual visit IT: Videos | AP: 8 times; 2–5 min videos | |
| . | . | . | . | 15 | Standard WIC BF education |
Where: WIC Program office/site Who: WIC staff | NR | |
| Who | Anderson, 2005, 16143742 | BF care | Urban | Academic | 63 | Peer counselor BF support and conventional support from clinic staff |
Where: Hospital, Clinic, Home, How: Home visit Who: Nurse, lactation consultant, peer IT: Primarily in-person, phone visits |
AP: 3 times In hosp: ≥1 time/day After discharge: 9 times; 3 in 1st wk, 2 in 2nd wk, & 1 per wk in wk 3–6 |
| . | . | . | . | 72 | Conventional BF support from clinic staff only |
Where: Clinic, dedicated PP visit How: Part of prenatal, perinatal and after discharge care, dedicated PP visit Who: Nurse, lactation consultant IT: Primarily in-person, phone visits |
AP: 1 time In hosp: ≥1 time/day After discharge: As needed | |
| Who | Chapman, 2004, 15351756 | BF care | Urban | Academic, tertiary | 90 | Heritage and Pride peer counseling program |
Where: Hospital, home How: Dedicated PP visit, home visit Who: Nurse, peer |
AP: 1 time In hosp: ≥1 time daily After discharge: 3 times |
| . | . | . | . | 75 | Routine BF education |
Where: Hospital How: Dedicated PP visit Who: Nurse | NR | |
| Who | Wambach, 2011, 20876551 | BF care | Urban | Academic | 128 | Lactation consultantpeer counselor team support |
Where: Clinic, How: Dedicated PP visit, Telehealth/virtual visit, Who: Lactation consultant, peer IT: Primarily in-person, phone visits |
AP: 2 times; 1.5–2 hr In hosp: NR After discharge: 5 times; 4, 7, 11, 18, 28 d |
| . | . | . | . | 128 | Advanced-practice nurse and peer counselor attention control |
Where: Clinic How: Dedicated PP visit, telehealth/virtual visit Who: Nurse, peer IT: Primarily in-person, phone visits |
AP: 2 times; 1.5–2 hr In hosp: NR After discharge: 5 times; 4, 7, 11, 18, 28 d | |
| . | . | . | . | 134 | Usual care at clinic |
Where: Clinic How: Dedicated PP visit | NR | |
| Who | Chapman, 2013, 23209111 | BF care | Urban | N/A | 76 | Specialized BF peer counseling |
Where: Hospital, home How: Dedicated PP visit, home visit Who: Nurse, peer |
AP: 2 times; 1 hr In hosp: 3 times; 1.5 hr After discharge: 5 times |
| . | . | . | . | 78 | Standard BF care by BF: Heritage and Pride peer counselors |
Where: Hospital, home How: Dedicated PP visit, home visit Who: Nurse, peer |
In hosp: 2 times; 0.5 hr After discharge: NR | |
| Who | Srinivas, 2015, 25193602 | BF care | Urban | NR | 50 | BF counseling by peer and non-peer counselors |
Where: Clinic, How: Dedicated PP visit, Telehealth/virtual visit, Who: Pediatrician, lactation consultant, peer, WIC nutritionist IT: Primarily in-person, Phone visits |
AP: 28 wk gestation-1 wk pre-delivery In hosp: NR After discharge: 9 times; at 3–5d, wkly for 1 mo, biwkly up to 3 mo, once at 4 mo |
| . | . | . | . | 53 | BF counseling by non-peer counselors only |
Where: Clinic How: Dedicated PP visit Who: Pediatrician, lactation consultant, WIC nutritionist | NR | |
| Who, IT | Kerver, 2019, N/A | BF care, General PP/risk counseling | Urban | High-volume, academic, community | 28 | In-person, phone, and online support by peer counselors and smart phone-based weight control program |
Where: Clinic, Home Telehealth/e-Health How: Home visit, Telehealth/virtual visit Who: Peer IT: Smartphone/computer applications | NR |
| . | . | . | . | 25 | Support by prenatal care provider |
Where: Clinic How: Dedicated PP visit Who: OB/GYN IT: Primarily in-person | NR | |
| Who | Porteous, 2000, 11155608 | BF care | Urban | Academic | 26 | Hospital visits by midwife and telephone access through 1 mo PP |
Where: Hospital, telehealth/e-Health How: Dedicated PP visit Telehealth/virtual visit Who: Midwife IT: Primarily in-person, Phone visits |
In hosp: Daily After discharge: 4 times; 4 wk; 10–15 min; wkly |
| . | . | . | . | 25 | Conventional nursing care group |
Where: Hospital How: Dedicated PP visit Who: Nurse | NR | |
| Who | Rasmussen, 2011, 20958105 | BF care | Rural | Academic | 20 | Additional BF support by a lactation consultant |
Where: Clinic, Telehealth/e-Health How: Dedicated PP visit, telehealth/virtual visit Who: Nurse, lactation consultant IT: Primarily in-person, phone visits |
AP: 1 time In hosp: Multiple times; 8 hrly After discharge: 2 times; 1–3 d |
| . | . | . | . | 20 | Standard BF support without a lactation consultant |
Where: Clinic, How: Dedicated PP visit, Telehealth/virtual visit, Who: Nurse |
AP: 1 time In hosp: Multiple times; ~8-hourly After discharge: NR | |
| Who, Provider Interventions | Bonuck, 2014a, 24354834 | BF care | Urban | Community | 129 | Electronic prompts for provider and lactation consultant for patients |
Where: Clinic, telehealth/e-Health How: Dedicated PP visit, Telehealth/virtual visit Who: OB/GYN, lactation consultant IT: Primarily in-person, phone visits |
AP: 7 times; 1 hr each In hosp: 1 time; 45 min After discharge: >1 hr; 3 mo or until BF cessation |
| . | . | . | . | 133 | Standard BF support | N/A | N/A | |
| Who, Provider Interventions | Bonuck, 2014b, 24354834 | BF care | Urban | Academic | 238 | Electronic prompts for provider and lactation consultant for patients |
Where: Clinic, Telehealth/e-Health How: Dedicated PP visit, Telehealth/virtual visit Who: OB/GYN, lactation consultant |
AP: 7 times; 1 hr each In hosp: 1 time; 45 min After discharge: >1 hr; 3 mo or until BF cessation |
| . | . | . | . | 77 | Only lactation consultant for patients |
Where: Clinic How: Dedicated PP visit Who: Lactation consultant |
AP: 2 times; 1 hr each In hosp: 1 time; 45 min After discharge: >1 hr; 3 mo or until BF cessation | |
| . | . | . | . | 236 | Only electronic prompts for provider |
Where: Telehealth/e-Health How: Telehealth/virtual visit Who: OB/GYN | AP: 5 times; 1 hr each | |
| . | . | . | . | 77 | Standard BF support | N/A | N/A | |
| Who, IT | Uscher-Pines, 2020, 31629118 | BF care | Rural | Academic | 94 | Unlimited on-demand video BF support by lactation consultant through Telelactation app and standard in-hospital BF support |
Where: Hospital, Telehealth/e-Health, How: Dedicated PP visit, Telehealth/virtual visit, Who: OB/GYN, Pediatrician, nurse, lactation consultant IT: Bidirectional telemedicine/virtual televisits, smartphone/computer applications | After discharge: Unlimited; 3 mo; 24 hr/d |
| . | . | . | . | 93 | Standard in-hospital BF support only |
Where: Hospital, How: Dedicated PP visit, Who: OB/GYN, pediatrician, nurse | NR | |
| Coordination/management | Rutledge, 2016, 27350389 | General PP care | NR | NR | 1709 | Case management and referral through Maternity Care Coordination (MCC) programs |
Where: Clinic, Home How: Home visit, Who: Nurse, Social worker Combination of people at different time-points: NR Coordination: case management and referral services |
AP: NR In Hospital: NR After Discharge: NR |
| . | . | . | . | 4848 | Usual care |
Where: NR How: NR Who: NR Coordination: NR |
AP: NR In Hospital: NR After Discharge: NR | |
| Coordination/management | Tsai, 2011, 21365543 | General PP care | Urban | Public, academic | 106 | Before initiative to provide patient PP appointment information in the hospital and a photo of patient and baby at PP visit |
Where: Clinic How: Dedicated PP visit Who: Clinic staff | N/A |
| . | . | . | . | 115 | After initiative to provide patient PP appointment information in the hospital and a photo of patient and baby at PP visit |
Where: Clinic How: Dedicated PP visit Who: Clinic staff |
In hosp: 1 time; pre-discharge After discharge: 1 time; PP visit | |
| Coordination/management | Mendez-Figueroa, 2014, 24481876 | Screening | Urban | Public, Academic, Tertiary | 207 | Telephone reminders for diabetes screening |
Where: Clinic How: Dedicated PP visit. Scheduled appointment for OGTT. Who: Nurse. Combination of people at different time-points: Bilingual outreach worker worked with patient and community-based provider. Coordination: Other: Scheduling an appointment for PP OGTT, issuing reminders, phone call 1 week prior to the OGTT. IT: Primarily in-person. Issuing reminders, phone call 1 week prior to the scheduled OGTT. |
AP: NR In Hospital: PP in-hospital stay visit follow-up and scheduling an appointment for PP OGTT After Discharge: Scheduled OGTT at 4–6 weeks PP, reminder 1 week before the appointment by phone call, 3 testing appointments were made for patients failing to attend. |
| . | . | . | . | 181 | No telephone reminders for diabetes screening |
Where: Clinic. How: NR Who: NR IT: N/A (Primarily in-person) |
AP: NR, In Hospital: NR After Discharge: NR | |
| Coordination/ management, Provider Interventions | Clark, 2009, 19268878 | Screening care | Urban | High (Provides services to 750000, perform 8000 deliveries per yr), Public, Academic, Tertiary | 81 | Provider and patient mail reminders for diabetes screening |
Where: Postal How: Postal reminders Coordination: Reminder for the screening of GMD for both. When reminders were sent to both the patient and the physician, the physician reminder was modified to inform the physician that the patient had received a requisition for the recommended screening test. IT: Postal reminders |
AP: N/A In Hospital: N/A After Discharge: Once for 3 months |
| . | . | . | . | 31 | Provider reminder for diabetes screening |
Where: Postal How: Postal reminders IT: Postal reminders. |
AP: N/A In Hospital: N/A After Discharge: Once for 3 months | |
| . | . | . | . | 76 | Patient mail reminder for diabetes screening |
Where: Postal How: Postal reminders IT: Postal reminders |
AP: N/A In Hospital: N/A After Discharge: Once for 3 months. | |
| . | . | . | . | 35 | No reminders for diabetes screening |
Where: N/A How: N/A IT: N/A |
AP: N/A In Hospital: N/A After Discharge: N/A | |
| Coordination/ management, IT | Shea, 2011, 21466755 | Screening | NR | Public, academic, tertiary | 55 | Mail and/or phone reminder for diabetes screening |
Where: Telehealth/e-Health, How: Mail, Telehealth/virtual visit, mail, Coordination: Strategy to facilitate access to appointments/scheduling, IT: Phone visits | After discharge: 1 time; 3 mo |
| . | . | . | . | 90 | Mail reminder only for diabetes screening |
How: Mail, Coordination: Strategy to facilitate access to appointments/scheduling | After discharge: 1 time; 3 mo | |
| . | . | . | . | 117 | No mail/phone reminder for diabetes screening | N/A | N/A | |
| IT | Martinez-Brockman, 2018, 29325660 | BF care | Urban | N/A | 94 | Text messaging of the benefits of BF and BF peer counselors |
Where: Telehealth/e-Health, WIC office/site How: Telehealth/virtual visit, WIC program Who: Lactation consultant, peer, WIC staff IT: Bidirectional texting | After discharge: ≤3 mo |
| . | . | . | . | 80 | BF peer counselors only |
Where: WIC Program office/site How: WIC program Who: Lactation consultant, peer, WIC staff | NR | |
| IT | Abbass-Dick, 2020, 32739716 | BF care | Urban | Tertiary | 106 | eHealth BF co-parenting website |
Where: Telehealth/e-Health How: Telehealth/virtual visit IT: Smartphone/computer applications | After discharge: NR |
| . | . | . | . | 111 | Available community resources only | Where: Community site/center | After discharge: NR | |
| IT | Bender, 2022, 36201773 | Breastfeeding care | Urban | Academic ,Tertiary | 106 | Text message-based BF support |
Where: Text-based support. In the rare instance that issues could not be remedied by text message, referrals for telehealth or in-person visits with lactation specialists or other health care professionals were made How: Text-based breastfeeding support. In the rare instance that issues could not be remedied by text message, referrals for telehealth or in-person visits with lactation specialists or other health care professionals were made Who: OB/GYN, Other: In the rare instance that issues could not be remedied by text message, referrals for telehealth or in-person visits with lactation specialists or other health care professionals were made Coordination: In the rare instance that issues could not be remedied by text message, referrals for telehealth or in-person visits with lactation specialists or other health care professionals were made IT: Bidirectional texting, Other: Text-based support via the Way to Health platform |
AP: N/A In Hospital: N/A After Discharge: Follow-up: 2/wk for first 4 wk PP, and once/wk thereafter for the remaining 2wks PP (The first 6 wks there are the supportive texts) |
| . | . | . | . | 110 | Usual care |
Where; NR How: Women in this group will be directed to their physician with any questions or concerns during the study period Who: Women in this group will be directed to their physician with any questions or concerns during the study period Coordination: Women in this group will be directed to their physician with any questions or concerns during the study period. IT: NR |
AP: NR In Hospital: NR After Discharge: NR | |
| IT | Ahmed, 2016, 26779838 | BF care | Urban | Academic | 49 | Interactive web-based BF monitoring and usual care |
Where: Hospital How: Telehealth/e-Health, phone visit, telehealth/virtual visit Who: Lactation consultant IT: Smartphone/computer applications |
AP: NR In hosp: 1 time After discharge: Daily, 1 mo |
| . | . | . | . | 57 | Usual BF support |
Where: Hospital How: Phone visit Who: Lactation consultant IT: Phone visits |
AP: NR In hosp: 1 time After discharge: 1 time, ≤1 wk | |
| Provider Interventions | Domingo, 2022, 35237835 | Screening | Suburban | NR | 133 | EMR reminder for providers for OGTT testing |
Where: Clinic, How: Dedicated PP visit Who: Electronic medical record |
AP: N/A, In Hospital: N/A After Discharge: N/A |
| . | . | . | . | 113 | No EMR reminder for providers for OGTT testing |
Where: Clinic How: Dedicated PP visit Who: Electronic medical record. |
AP: N/A In Hospital: N/A After Discharge: N/A |
Abbreviations: AP = antepartum, BF = breastfeeding, d = day, DMPA = depot-medroxyprogesterone acetate, EMR = electronic medical record, hosp = hospital, hr = hour, GDM = gestational diabetes mellitus, IT =information technology, IUD = intrauterine device, LARC = long-acting reversible contraceptive, min = minute, mo = month, N/A = not applicable, NR = not reported, OB/GYN = obstetrics and gynecology, PMID = PubMed ID, PP = postpartum, wk = week
Studies did not report on titrations or unplanned modifications to delivery strategies.
Table C-1.3Key Question 1: Healthcare delivery strategies – summary of sample details
| Study, Publication Year, PMID | Age in Years, Mean (SD) or as Specified | BMI, Mean (SD) or as Specified | Race | Educational Attainment in Years, Mean (SD) or as Specified | Employment Status | SES | Miscellane ous | SUDs | Chronic Conditions | Delivery Type | Offspring Characteristics |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lieu, 2000, 10790463 | 27.9 (6.1) | NR |
W: 708 (60.9) B: 83 (7.1) H: 145 (12.5) O1: 227 (19.5) | Less than HS degree: 85 (7.3) HS degree or more: 1078 (92.7) | NR | At or below federal poverty level: 80 (6.9) 101%–200% of federal poverty level: 234 (20.1) >200% of federal poverty level: 802 (69) | NR | NR | NR | V: 1163 (100) |
Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 |
| Gagnon, 2002, 12042545 | 30 (4.8) | NR | NR | Up to graduate education: 522 (89.1) Attended postgraduate studies: 64 (10.9) | NR | NR | Born outside of Canada: 312 (53.2) | NR | NR | V: 586 (100) | NR |
| Norr, 2003, 12716399 | <20: 190 (39.8) ≥20: 287 (60.2) | NR |
B: 323 (67.7) H: 154 (32.3) | Some HS or less: 235 (49.3) HS graduate: 242 (50.7) | NR | NR | Medicaid: 477 (100) | OUD: 0 | NR | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 |
| Escobar, 2001, 11533342 | 29.1 (5.6) Median 29 | NR |
W: 480 (47.3) B: 27 (2.7) H: 207 (20.4) O1: 300 (29.6) | HS graduate or less: 263 (25.9) Some college/ technical school: 325 (32.1) College graduate or more: 426 (42) | NR |
≤$20000: 76 (7.5) $20001–$40000: 176 (17.4) $40001–$60000: 193 (19) $60000: 477 (47) | NR |
OUD: 0 Other: 0 | NR | V: 1014 (100) |
Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Steel O’Connor, 2003, 12675164 | 27.4 (5.3) | NR | NR |
Less than HS: 97 (13.8) Completed HS: 64 (9.1) Some post-secondary: 83 (11.9) Completed post-secondary: 458 (65.2) | NR | NR | NR | NR | NR | V: 702 (100) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 |
| McCarter, 2019, 31222789 | 29.6 (NR) | NR |
W: 306 (85.7) B: 51 (14.3) H: 29 (8.1) | High school or less 80 (22.4) Some college 117 (32.8) College degree or higher 162 (45.4) | NR | NR | WIC: 131 (36.7) | NR | NR |
V: 283 (79.3) C: 74 (20.7) | NR |
| Paul, 2012, 22064874 | 29 (5.5) <20: 49 (4.2) ≥20: 1105 (95.8) | NR |
W: 971 (84.4) B: 63 (5.5) A: 50 (4.3) H: 57 (5) O1: 10 (0.9) |
Some HS: 31 (2.7) HS graduate: 171 (14.9) Some college and/or technical school: 287 (25) College graduate: 427 (37.1) Postgraduate training: 234 (20.3) | NR |
Annual income <$5,000: 98 (8.5) Annual income $5,000-$49,999: 210 (18.2) Annual income $50,000-$74,999: 251 (21.8) Annual income $75,000-$99,999: 222 (19.2) Annual income ≥$100,000: 244 (21.1) Missing data/refused/unknown: 129 (11.2) |
Medicaid insurance: 153 (13.4) WIC participation : 197 (17.1) | NR |
PE: 49 (4.3) HTN: 101 (8.8) DM: 62 (5.4) |
V: 794 (68.9) C: 361 (31.1) |
Multiple births: 15 (1.3) Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Arias, 2022, 35331971 |
Median 30.2 IQR (25.47–34.29) | NR |
W: 399 (25.3) B: 966 (61.2) A: 132 (8.4) O1: 66 (4.2) |
Less than high school 159 (10) High School Diploma/ GED degree 743 (47.1) Advanced degree 648 (41) Unknown 28 (1.8) | NR | NR | NR | NR |
HDP: 483 (30.6) HTN: (Chronic) 129 (8.2) GD: 104 (6.6) DM: Pregestational DM 42 (2.7) CVD: Cardiomyopathy 5 (0.3) |
V: 1078 (68.3) C: 501 (31.7) |
Multiple births 42 (2.7) NICU: 217 (13.7) Neonatal death: 24 (1.5) |
| Dodge, 2019, 31675088 |
29.4 (6.2) Adolescent mother: 21 (6.6) | NR |
W: 178 (56.3) B: 120 (40) H: 90 (28.5) O1: 18 (5.7) | NR | NR | NR | Medicaid: Medicaid or no insurance: 197 (62.3) | NR | NR |
V: 230 (72.8) C: 86 (27.2) | Multiple births 15 (7.4) |
| Pugh, 2002, 12000411 | 21.6 (4.38) | NR |
W: 7.3 B: 92.7 | >12yr/high school 35 (84.9) | NR | Low income 41 (100) | NR | NR | NR | NR | NR |
| Mersky, 2021, 33078655 | 26.8 (6.1) | NR |
B: 112 (47.3) H: 96 (40.5) O1: 29 (12.2) |
Up to secondary education: 182 (76.8) Postsecondary education: 55 (23.2) | NR | Low-income: 237 (100) | NR | NR | NR | NR | NR |
| Pugh, 2010, 19854119 |
23.1 (5.3) 13–17: 33 (10.1) 18–19: 56 (17.1) 20–24: 137 (41.8) 25–34: 91 (27.7) 35–43: 11 (3.4) | NR |
W: 15 (4.6) B: 286 (87.2) H: 13 (4) O1: 14 (4.3) |
Below HS: 87 (26.5) HS/GED: 121 (36.9) Some College: 83 (25.3) College Grad/Grad Degree: 37 (11.3) |
Employed, in school: 72 (22) Employed, not in school: 139 (42.4) Unemployed, in school: 60 (18.3) Unemployed, not in school: 57 (17.4) | Low income: 328 (100) | WIC: 328 (100) | NR | NR |
V: 241 (73.5) C: 87 (26.5) | NR |
| Edwards, 2013, 24187119 | 18.1 (1.7) | NR | B: 248 (100) |
10.8 (1.5) Not in school: 113 (45.6) In school: 135 (54.4) |
Unemployed: 211 (85.1) Employed: 37 (14.9) | NR | Medicaid: 233 (93.8) | NR | NR | NR | Neonatal death: 2 (0.8) |
| Gill, 2007, 17557933 | NR | NR | H: 158 (100) | NR | NR | NR | WIC: 158 (100) | NR | NR | NR |
Preterm birth: 0 NICU: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Polk, 2021, 34671758 | 27.7 (6) | NR |
W: 8 (6.9) B: 11 (9.5) H: 94 (81) O1: 3 (2.6) |
≤6th Grade: 32 (27.6) 7th to 12th Grade: 38 (31.9) HS or GED: 32 (27.6) Some college: 5 (4.3) College: 8 (6.9) | NR | NR | Medicaid: 23 (19.8) | NR |
PE: 1 (0.9) GD: 10 (8.6) | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 4 (3.4) NICU: 0 Neonatal death: 0 |
| Koniak-Griffin, 2003, 12657988 | 16.8 (1.1) | NR |
W: 19 (19) B: 11 (11) H: 65 (64) O1: 7 (6) |
Enrolled, attending HS: 50 (49.5) Enrolled, not attending: 13 (12.9) Dropped out: 27 (26.7) Graduated HS/GED: 8 (7.9) Other: 3 (3) |
Employed: 15 (15) Unemployed: 87 (85) | NR | Medicaid: 86 (84) | OUD: 0 | NR | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 NICU: 25 (25) |
| Hans, 2018, 29855838 | 18.4 (1.8) | NR |
W: 26 (8.3) B: 140 (44.9) H: 117 (37.5) O1: 29 (9.3) |
10.9 (1.5) Not in school: 148 (47.4) In school: 164 (52.6) | NR | NR |
Medicaid: 278 (91.1) WIC: 268 (85.9) | NR | NR |
V: 248 (79.5) C: 64 (20.5) |
Preterm birth: 22 (7.1) NICU: 44 (14.1) |
| Haider, 2020, 31964564 |
<20: 42 (9.4) 20–24: 128 (28.7) 25–29: 125 (28) 30–34: 97 (21.8) ≥35: 54 (12.1) | NR |
W: 52 (11.7) B: 256 (57.4) A: 19 (4.3) H: 102 (22.9) O1: 16 (3.6) |
<HS/ in HS: 32 (7.2) HS, graduate: 126 (28.3) Some college/ 2yr degree: 180 (40.4) Bachelor’s degree or higher: 108 (24.2) |
Full-time: 54 (12.1) Part-time: 23 (5.2) Maternity leave: 185 (41.5) Unemployed: 182 (40.8) | NR | NR | NR | NR |
V: 324 (72.6) C: 116 (26) | NR |
| Laliberte, 2016, 26871448 |
15–19: 2 (0.4) 20–24: 22 (5.1) 25–29: 95 (22.2) 30–34: 165 (38.5) 35–39: 108 (25.3) ≥40: 26 (6) Missing: 10 | NR | NR |
Up to some HS: 1 (0.25) Completed HS: 33 (7.7) Vocational/technical training after HS: 67 (15.7) Completed university: 316 (73.8) Missing: 11 (2.6) | NR | NR | NR | NR | NR |
V: 339 (71.8) C: 133 (28.2) | Multiple births: 0 |
| Rozga, 2016, 27423234 |
<20: 91 (13.1) 20–29: 483 (69.2) ≥30: 124 (17.7) | NR |
W: 512 (74.3) B: 87 (12.5) H: 80 (11.4) O1: 13 (1.9) |
<HS Diploma: 143 (20.5) HS Diploma or equivalent: 555 (79.5) | NR | NR | WIC: 667 (95.6) | NR | NR | NR | Preterm birth: 50 (7.2) |
| Witt, 2021, 33956505 | 27 (16–43) | NR |
W: 297 (67.2) B: 104 (23.6) H: 145 (32.7) | NR | NR | NR | NR | NR | NR |
V: 349 (79) C: 93 (21) |
Preterm birth: 119 (27) NICU: 18 (4.1) |
| Bernard, 2018, 29778586 | 25.7 (5) | NR |
W: 15 (8) B: 168 (89.4) O1: 5 (2.7) |
Less than HS: 28 (14.9) HS/GED: 82 (43.6) Some college/associate’s degree: 63 (33.5) Vocational/technical school: 9 (4.8) College degree: 6 (3.2) |
Working full-time: 61 (32.4) Working part-time: 31 (16.5) Unemployed: 62 (33) Disabled/sick leave/other: 23 (12.2) Full-time student: 11 (5.9) | NR | NR | NR | NR |
V: 125 (66.5) C: 63 (33.5) |
Stillbirth: 0 Spontaneous or induced abortion: 0 NICU: 0 |
| Pluym, 2021, 33785465 | 30.4 (5.95) | With obesity at consent (PP): 133 (53.2) |
W: 28 (11.2) B: 24 (9.6) A: 24 (9.6) H: 140 (56) O1: 34 (13.6) |
<9 yr: 4 (1.6) 9−11 yr: 16 (6.4) 12−16 yr: 1 (0.4) >16 yr: 39 (15.6) | NR | NR | NR | NR |
HTN: 41 (16.4) DM: 74 (29.6) CVD: 6 (2.4) |
V: 176 (70.4) C: 74 (29.6) |
Multiple births: 6 (2.4) NICU: 26 (10.4) |
| Chen, 2019, 30414598 |
29.5 (5.4) <30: 247 (48.2) ≥30: 265 (51.8) | NR |
W: 340 (66.4) B: 51 (10) A: 66 (12.9) H: 145 (28.3) O1: 21 (4.4) O2: 34 (6.6) |
HS or less: 111 (21.7) Some college: 155 (30.3) College graduate: 136 (26.6) Graduate school: 110 (21.5) |
Employed full-time: 251 (49) Employed part-time: 69 (13.5) Unemployed: 71 (13.9) Homemaker: 91 (17.8) Full-time student: 30 (5.9) | NR | NR | NR | NR | V: 360 (70.3) | Preterm birth: 40 (7.8) |
| Dahlke, 2011, 21843688 | 25.6 | NR |
W: 30 (65.2) B: 11 (23.9) H: 5 (10.9) | NR | NR | NR | NR | NR | NR | V: 46 (100) | NR |
| Chen, 2010, 20966692 |
25.1 (5.3) ≤18: 0 18–65: 102 (100) ≥65: 0 | NR |
W: 51 (50) B: 45 (44.1) H: 5 (4.9) O1: 6 (5.9) | NR | NR | NR | Government insurance: 75 (73.5) | NR | NR | V: 102 (100) | NR |
| Levi, 2015, 26241250 | 28.5 (5.4) | NR |
W: 48 (42.9) B: 28 (25) A: 2 (1.8) H: 31 (27.7) O1: 3 (2.7) |
HS or less: 53 (47.3) Some college: 46 (41.1) Graduate education: 13 (11.6) | NR |
Income ≤$250/mo: 6 (5.4) Income $251-$500/mo: 7 (6.3) Income $501-$1000/mo: 10 (8.9) Income $1001-$2000/mo: 33 (29.5) Income $2001-$3000/mo: 12 (10.7) Income ≥3000/mo: 33 (29.5) Refuse to answer: 11 (9.8) | Language Discordance: 0 | NR | NR | C: 112 (100) |
Stillbirth: 0 Spontaneous or induced abortion: 0 |
| Dempsey, 2018, N/A |
Median 19.2 SD (1.4) | NR |
W: 15 (18.5) B: 61 (75.3) A: 1 (1.2) O1: 4 (4.9) | NR | NR | NR | NR | NR | NR | NR | NR |
| Baldwin, 2019, N/A | 28.4 (6.3) | NR | H: 27 (13.7) |
Up to HS/GED: 54 (27.4) More than HS: 143 (72.6) | NR | NR | Public Insurance: 95 (48.2) | NR | NR |
V: 146 (74.1) C: 51 (25.9) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 |
| Whitaker, 2014, 24457061 | 27.8 (5.8) | NR |
W: 8 (19.1) B: 29 (69.1) H: 3 (7.1) O1: 2 (4.8) | NR | NR |
Income <$10,000/yr: 13 (31) Income $10,000–$30,000/yr: 13 (31) Income >$30,000/yr: 16 (38) | Medicaid: 30 (71.4) | NR | NR | C: 42 (100) | NR |
| Morse, 2016, N/A | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Chen, 2018, NCT01463202 | 24.1 (4.8) | NR |
W: 20 (12.7) B: 122 (77.7) H: 9 (5.7) O1: 15 (9.6) | NR | NR | NR | Language Discordance: 0 | NR | NR | NR | Multiple births: 0 |
| Jensen, 2019, N/A | NR | NR | NR | NR | NR | NR | Language Discordance: 0 | NR | NR | NR | Multiple births: 0 |
| Kozhimannil, 2013, 23837663 | NR | NR |
W: (56.8) B: (9.3) A: (0.6) H: (14.9) O1: (9.5) O2: (14.2) O3: (5.7) | NR | NR | NR | Medicaid: 52790 (100) | NR | NR | NR |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 |
| Pan, 2020, 32437282 | NR | NR | NR | NR | NR | NR | Medicaid: 410 (90.1) | NR | NR | NR |
Preterm birth: 62 (13.6) NICU: 76 (16.7) |
| Edwards, 1997, 9170692 |
≤25: 125 (16) >25: 662 (84) | NR | NR |
Less than HS: 197 (25) At least HS: 591 (75) | NR |
Household income <$20,000: 79 (10) Household income ≥$20,000: 709 (90) | NR | NR | NR | NR | Multiple births: 0 |
| Falconi, 2022, 35812994 | 28.4 (5.4) | NR |
W: 221 (37.1) B: 204 (34.2) A: 26 (4.4) H: 98 (16.4) O1: 47 (7.9) | NR | NR |
Q1 (worst) 240 (40.3) Q2 144 (24.2) Q3 134 (22.5) Q4 (best) 42 (7) Missing/unknown 36 (6) | NR | Substance use disorder: 13 (2.2) |
HDP: Gestational HTN 30 (5) HTN: 21 (3.5) GD: 31 (5.2) |
V: 512 (85.9) C: 84 (14.1) | Preterm birth 42 (7) |
| Buckley, 1990, 2328162 | 18 (16–36) | NR |
W: 47 (79.7) B: 5 (8.5) H: 7 (11.9) | NR | NR | NR | Medicaid: 44 (74.6) | NR | NR |
V: 52.0 (88.1) C: 7 (11.9) | NR |
| Tandon, 2021, 33655429 | 26.3 (5.83) | NR |
W: 245 (29.7) O1: 579 (70.3) |
HS graduate or less: 493 (59.8) Some college: 331 (40.2) |
Unknown: 14 (1.7) Unemployed: 520 (63.1) Employed part-time: 167 (20.3) Employed fulltime: 123 (14.9) |
Income ≤$25,000/yr: 584 (70.9) Income $25,000–$49,999/yr: 151 (18.3) Income $50,000–$74,999/yr: 32 (3.9) Income $75,000–$99,999/yr: 13 (1.6) Income ≥$100,000/yr: 12 (1.5) Unknown: 32 (3.9) | Born outside US: 97 (11.8) | NR | NR | NR | NR |
| Simmons, 2013, 23218851 |
25.3 (4.8) (18–38) <25: 26 (53.1) ≥25: 23 (46.9) | NR |
W: 34 (69.4) O1: 15 (30.6) |
HS or less: 24 (49) Some college or higher: 25 (51) | NR | Low-income: 49 (100) | Oregon Medicaid: 49 (100) | NR | NR |
V: 33 (67.4) C: 16 (32.6) | NR |
| Dennis, 2002, 11800243 |
16–24: 35 (13.7) 25–34: 191 (74.6) ≥35: 30 (11.7) | NR | NR |
Some HS: 65 (25.4) Some college: 165 (64.5) Some postgraduate: 26 (10.2) | NR |
Income ≤$39999/yr: 41 (16) Income $40000–$79999/yr: 101 (39.5) Income ≥$80000/yr: 98 (38.3) | Not born in North America: 35 (13.7) | NR | NR |
V: 197 (77) C: 59 (23) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Reeder, 2014, 25092936 | 27.2 | NR |
W: (54.7) H: (93.7) O1: (6.3) |
No or some HS: (41.7) At least HS graduate: (58.3) | NR | NR | WIC eligible: 1885 (100) | NR | NR |
V: 1338 (71) C: 547 (29) | NR |
| Gross, 1998, 12515413 | 22.1 (5.7) | NR | B: 115 (100) |
Less than HS diploma: 84 (73) HS diploma: 18 (15.7) More than HS diploma: 13 (11.3) | Employed before pregnancy: 26 (22.6) | NR | WIC eligible: 115 (100) | NR | NR | NR | Multiple births: 0 |
| Anderson, 2005, 16143742 |
<20: 18 (13.3) 20–30: 91 (67.4) ≥30: 26 (19.3) | NR |
W: 10 (7.4) B: 24 (17.8) H: 97 (71.9) O1: 4 (3) |
Less than or some HS: 47 (34.8) HS graduate: 45 (33.3) More than HS: 43 (31.9) |
Unemployed: 85 (63) Employed part-time: 36 (26.7) Employed fulltime: 14 (10.4) | NR | WIC participation : 122 (90.4) | OUD: 0 |
HDP: 0 HTN: 0 GD:0 DM: 0 CVD: 0 | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 |
| Chapman, 2004, 15351756 | 24.8 (5.8) | NR |
W: (3.6) B: (8.5) H: (80) O1: (7.9) | 11.6 (2.7) |
Full-time: (15.9) Part-time: (22) Unemployed: (62.2) | NR | WIC participation: (72.1) | NR | NR |
V: (75.6) C: (24.4) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Wambach, 2011, 20876551 | 17 (0.9) (15–18) | NR | B: (61) |
In school: (71) Not in school: (29) |
Unemployed: (81.8) Employed part-time: (13.2) Employed full-time: (5) |
Family income <$25,000/yr: (75) Family income ≥$25,000/yr: (25) | NR | NR | NR | NR |
Multiple births: 0 Spontaneous or induced abortion: 0 NICU: 0 |
| Chapman, 2013, 23209111 | Median 24 (21–31) | Median 31.8 (28.5–37.0) |
W: 8 (5.2) B: 16 (10.4) H: 126 (81.8) O1: 4 (2.6) | Median 12 (10–12) |
Employed prenatally: 50 (32.5) Not employed prenatally: 104 (67.5) | NR |
Not born in the US/Puerto Rico: 67 (43.5) Receiving SNAP: 68 (44.2) Receiving WIC: 134 (87) | NR | NR |
V: 94 (61) C: 60 (39) |
Multiple births: 0 Stillbirth: 0 Preterm birth: 0 |
| Srinivas, 2015, 25193602 | NR | NR |
W: 44 (42.7) B: 28 (27.2) H: 27 (26.2) O1: 7 (6.8) |
Did not complete HS or GED: 61 (59.2) Completed HS or GED: 42 (40.8) |
Unemployed: 64 (38.1) Employed: 39 (61.9) | NR | Public insurance: 87 (84.5) | NR | NR | NR | NR |
| Kerver, 2019, N/A | NR | NR | B: 53 (100) | NR | NR | NR | WIC: 53 (100) | NR | NR | NR | NR |
| Porteous, 2000, 11155608 | NR | NR |
W: 49 (96.1) O1: 2 (3.9) |
HS or less: 19 (37.3) Beyond HS: 32 (62.7) | NR | NR | NR | NR | NR | V: 51 (100) | NR |
| Rasmussen, 2011, 20958105 | 27 (8.9) | 40.7 (6.8) Peripartum | NR | NR | NR | NR | WIC and/ or PCAP participation: 21 (53) | NR | NR |
V: 26 (65) C: 14 (35) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 |
| Bonuck, 2014a, 24354834 | 28.1 (5.7) |
<25: 104 (39.7) 25–29.9: 77 (29.4) ≥30: 81 (30.9) |
W: 13 (5) B: 75 (28.6) A: 7 (2.7) H: 146 (55.7) O1: 21 (8) |
No or some HS: 32 (12.2) HS graduate: 230 (87.8) | NR | NR |
Non-US born: 10 6 (40.5) WIC: 103 (39.3) | NR | NR |
V: 174 (66.4) C: 88 (33.6) |
Multiple births: 0 NICU: 0 |
| Bonuck, 2014b, 24354834 | 27.7 (6) |
<25: 199 (31.7) 25–29.9: 164 (26.1) ≥30: 241 (38.3) |
W: 28 (4.5) B: 179 (28.5) A: 12 (1.9) H: 357 (56.8) O1: 52 (8.3) |
No or some HS: 145 (23.1) HS graduate: 483 (76.9) | NR | NR |
Non-US born: 188 (29.9) WIC: 376 (59.9) | NR | NR |
V: 387 (61.6) C: 241 (38.4) |
Multiple births: 0 NICU: 0 |
| Uscher-Pines, 2020, 31629118 | 26.5 (5.1) |
<30: 177 (94.7) ≥30: 10 (5.3) |
W: 180 (96.3) H: 3 (1.6) |
No or some HS: 84 (44.9) HS graduate: 103 (55.1) | NR |
Income ≤$14,999/yr: 30 (16.4) Income $15,000∓$24,999/yr: 21 (11.2) Income $25,000∓$39,999/yr: 24 (12.8) Income $40,000∓$54,999/yr: 28 (15) Income 55,000∓$79,999/yr: 35 (18.7) Income ≥$80,000/yr: 28 (15) | Public insurance: 92 (49.2) | NR |
HTN: 10 (5.3) DM: 2 (1.1) |
V: 106 (56.7) C: 81 (43.3) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 26 (13.9) NICU: 0 |
| Rutledge, 2016, 27350389 |
<18: 800 (12.2) 18–35: 5331 (81.3) >35: 426 (6.5) | NR |
W: 3862 (58.9) B: 2406 (36.7) A: 118 (1.8) H: 898 (13.7) |
High school or less: 29 (44.9) Missing data: 2400 (36.6) | NR | NR | NR | Substance use disorder: 564 (8.6) | NR | NR |
Multiple births 0 (0) Stillbirth 0 (0) |
| Tsai, 2011, 21365543 | 26.3 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Mendez-Figueroa, 2014, 24481876 | 29.8 (6.2) | 29.9 (7.7) |
W: 101 (26) B: 55 (14.2) A: 37 (9.5) H: 156 (40.2) O1: 36 (9.3) | NR | NR | NR | Language discordance with provider: (Different primary languages): 134 (34.5) Medicaid: Public funding 288 (74.2) | NR | GD: GDM 388 (100) | NR | Multiple births: 6 (1.5) |
| Clark, 2009, 19268878 | ≥ 30 y: 173 (77.6) | ≥ 30 (kg/m2): 73 (32.7) | W: 137 (61.4) | Postsecondary 182 (81.6) | NR | NR | NR | NR | GD: 223 (100) |
V: 61.4 C: 38.6 |
Stillbirth 0 (0) Preterm birth 27 (12.1) |
| Shea, 2011, 21466755 | 33.7 (5) | 27.1 (6.3) Antepartum Unknown: 28 (10.7) Normal: 104 (39.7) Overweight: 64 (24.4) With obesity: 66 (25.2) | NR | NR | NR |
Missing: 3 (1.1) SES1 (lowest): 67 (25.6) SES 2: 44 (16.8) SES 3: 57 (21.8) SES 4: 51 (19.5) SES 5 (highest): 40 (15.3) | NR | NR |
HDP: 20 (7.6) GD: 262 (100) PE: 13 (5) |
V: 165 (63) C: 97 (37) | Multiple births: 8 (3.1) |
| Martinez-Brockman, 2018, 29325660 | 26.8 (5.6) | 28 (7.4) Antepartum |
H: 127 (74.7) O1: 43 (25.3) |
Less than or some HS: 22 (15.3) HS graduate: 62 (43.1) More than HS: 60 (41.7) | NR |
Income ≤$1,000/mo: 41 (24.1) Income ≥$1,000/mo: 35 (20.6) Don’t know/refused: 94 (55.3) |
SNAP: 81 (47.9) WIC: 174 (100) | NR | NR | NR |
Multiple births: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 |
| Abbass-Dick, 2020, 32739716 |
18–30: 82 (37.8) ≥31: 135 (62.2) | NR | NR |
Did not attend university: 55 (25) Attended university: 162 (75) | NR |
Household income (CAD/yr): CAD ≤60,000: (14.2) CAD >60,000: (85.8) | Not born in Canada: 54 (24.9) | NR | NR |
V: 79 (69.9) C: 34 (30.1) | Multiple births: 0 |
| Bender, 2022, 36201773 | 31.6 (5.8) | Median 32.2 (26.3–38.0) |
W: 66 (30.6) B: 114 (52.8) A: 17 (7.9) H: 15 (6.9) O1: 6 (2.8) | NR | NR | NR | Language discordance with provider (unable to communicat e using English-language text messages) 0 (0) Irregular access to the internet: (unable to access a personal cellular telephone with unlimited text messaging) 0 (0) Medicaid: Public or uninsured 98 (45.4) | NR |
HDP (Severe PE) 10 (4.6) HTN: (Chronic) 8 (3.7) DM: 33 (15.2) |
V: 147 (68.1) C: 69 (31.9) |
Multiple births: 0 (0) Stillbirth: 0 (0) Spontaneous or induced abortion: 0 (0) Preterm birth: 0 (0) NICU: 0 (0) Congenital anomalies: 0 (0) |
| Ahmed, 2016, 26779838 | 29.6 (6.4) <20: 8 (7.5) 20–29: 42 (39.6) ≥30: 56 (52.8) | NR |
W: 72 (67.9) B: 24 (22.6) A: 3 (2.8) H: 4 (3.8) O1: 3 (2.8) |
Less than or HS graduate: 34 (32.1) Associate’s degree: 12 (11.3) Bachelor’s degree: 35 (33) Graduate degree: 25 (23.6) | NR |
Income ($/yr): <10,000: 15 (14.2) 10,000-$24,999: 15 (14.2) $25,000-$49,999: 14 (13.2) ≥$50,000: 62 (58.5) | NR | NR | NR |
V: 78 (73.6) C: 28 (26.4) |
Multiple births: 0 Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 0 NICU: 0 |
| Domingo, 2022, 35237835 | 32.6 (5.84) | 34.7 (5.81) |
W: 8 (3.3) B: 37 (15) A: 29 (11.8) H: 172 (69.9) | NR |
Employed: 67 (27.2) Unemployed: 179 (72.8) | NR |
Medicaid: Enrolled 228 (92.7) WIC: Enrolled 183 (74.4) | NR | GD: Diagnosed 246 (100) |
V: 159 (64.6) C: 87 (35.3) | NR |
Abbreviations: A = Asian, B = Black, BMI = body mass index, C = Cesarean delivery, CVD = cardiovascular disorders, DM = diabetes mellitus, GD = gestational diabetes, H = Hispanic, HS = high school, HDP = hypertensive disorders of pregnancy, HTN = hypertension, NICU = Neonatal intensive care unit, O = Other, OUD = opioid use disorder, PCAP = Prenatal Care Assistance Program, PE = Preeclampsia, PMID = PubMed ID, PP = Postpartum, SD = standard deviation, SES = socioeconomic status, SNAP = Supplemental Nutrition Assistance Program, SUD = substance use disorder, V = vaginal delivery, W = White, WIC= women, Infants, and Children
No studies reported on sexual/gender identity status of participants.
Table C-2.1Key Question 2: Extension of healthcare or insurance coverage - summary of design and arm details
| Author, Year, PMID | State(s) | Funding (Study Years) | Overall RoB | Inclusion Criteria | Exclusion Criteria | Study N | Focus of Study | Arm | Arm N | Arm Description |
|---|---|---|---|---|---|---|---|---|---|---|
| Arora, 2018, 29490290 | OH | Non-industry (2012–2014) | High | Sterilization as the documented contraceptive plan | Sterilized before study or died | 1184 | Contraceptive care | More comprehensive insurance | 154 | Private insurance |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 1030 | Medicaid insurance | |
| Austin, 2022, 34974107 | 20 states | Non-industry (2009–2018) | Modera te | Age>18yr Income <138% FPL | NR | 82728 | General PP care | More comprehensive insurance coverage | 51200 | Medicaid expansion states |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance coverage | 31528 | Medicaid non-expansion states | |
| Brant, 2021, 34619694 | OH | Non-industry (2015–2019) | Modera te | Gestational age >20wk | Birth outcome not a liveborn neon ate | 8516 | Contraceptive care | More comprehensive access to care | 2129 | Law that required hospitals to offer LARC placement after delivery (2017–2019) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive access to care | 6387 | No law that required hospitals to offer after delivery (2015–2017) | |
| Caudillo, 2022, 35488950 | 16 states | Non-industry (2012–2017) | Modera te | NR | NR | 47109 | Contraceptive care | More comprehensive insurance | 2504 | Delaware (After Delaware Contraceptive Access Now (DelCAN) initiative) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 44605 | 15 other states (no Delaware Contraceptive Access Now (DelCAN) initiative) | |
| Cilenti, 2015, 25627330 | NC | Non-industry (2009–2010) | Modera te | Delivery covered by NC Medicaid | NR | 1969 | General PP care | More comprehensive insurance | 1007 | Before change in Medicaid policy reducing reimbursement rates for maternity care coordination by 19% |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 962 | After change in Medicaid policy reducing reimbursement rates for maternity care coordination by 19% | |
| DeSisto, 2020, 32335806 | Wl | Non-industry (2011–2015) | Modera te | Live births. Medicaid. | NR | 105718 | General PP care | More comprehensive insurance | 79172 | Continuous Medicaid eligibility |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 26546 | Pregnancy-only Medicaid eligibility | |
| Dunlop, 2020, 32958368 | OH | Non-industry (2011–2015) | Modera te | Age 20–44 yr Medicaid | Medicaid eligibility based on disability | 138426 | Contraceptive care | More comprehensive insurance | 54477 | After Medicaid expansion (2014–2015) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 83949 | Before Medicaid expansion (2011–2013) | |
| Eliason, 2021, 34870677 | 15 states | Non-industry (2011–2018) | Modera te | Age>18yr Income 100%-138% of FPL | NR | 5034 | General PP care | More comprehensive insurance | 3389 | Medicaid expansion states |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 1645 | Medicaid non-expansion states | |
| Eliason, 2022, 35259409 | 11 states | Non-industry (2012–2019) | Modera te | Age>18yr Income <138% FPL | NR | 34598 | General PP care | More comprehensive insurance | 25781 | Medicaid expansion states |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 8817 | Medicaid non-expansion states | |
| Gordon, 2020, 31905073 | CO, UT | Non-industry (2013–2015) | Modera te | Age>19yr Live birth | NR | 66672 | General PP care | More comprehensive insurance | 42144 | CO (after Medicaid expansion) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 24528 | UT (no Medicaid expansion) | |
| Koch, 2022, 35588793 | MO | NR(2017–2019) | ▪ | Gestational age >24wk | NR | 6233 | Contraceptive care | More comprehensive insurance | 3128 | After policy change for separate LARC reimbursement |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 3105 | Before policy change for separate LARC reimbursement | |
| Kozhimannil 2011, 21485419 | MA | Non-industry (2001–2007) | Modera te | NR | NR | 2509 | General/ Overall PP care | More comprehensive insurance | 2280 | Full coverage of AP and PP care, no cost sharing beyond office visit and hospitalization copayments. Out-patient visit copayments $5-$25 (median $15). Hospitalization copayments $0-$1000 (median $250). |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 229 | Annual deductible $500-$2000 for individuals and $1000-$4000 for families. Out-of-pocket maximum $2000-$4000 for individuals and $4000-$8000 for families. | |
| Kramer, 2021, 33849768 | Wl | Non-industry (2016–2017) | Modera te | Overall/general PP/ pregnant population Medicaid | NR | 45200 | Contraceptive care | More comprehensive insurance | 22405 | After unbundling (separate or additional reimbursement for immediate PP LARC) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 22795 | Before unbundling (no separate or additional reimbursement for immediate PP LARC) | |
| Liberty, 2020, 31846612 | SC | Non-industry (2010–2017) | Modera te | Gestational age ≥ 23 wk Singleton pregnancy | Births covered by Emergency Medicaid | 164004 | Contraceptive care | More comprehensive insurance | 108430 | After policy covering immediate PP LARC (2013–2017) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 55574 | Before policy covering immediate PP LARC (2010–2012) | |
| Margerison, 2021, 34606358 | 18 states | Non-industry (2012–2018) | Modera te | Age>18yr Household income <137%of FPL | NR | 56965 | General/ Overall PP care | More comprehensive insurance | NR | Medicaid expansion states |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | NR | Medicaid non-expansion states | |
| Myerson, 2020, 33136489 | 13 states | NR(2011–2017) | Modera te | Household income <138%of FPL Live birth | NR | 15059 | Contraceptive care | More comprehensive insurance | 9135 | Medicaid expansion states |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 5924 | Medicaid non-expansion states | |
| Okoroh, 2018, 29530670 | I A, LA | NR(2013–2015) | Modera te | Medicaid | NR | 57894 | Contraceptive care | More comprehensive insurance | NR | After Medicaid expansion (2014–2015) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | NR | Before Medicaid expansion (2013–2014) | |
| Pace, 2022, 34908011 | MA, ME | Non-industry (2009–2015) | High | Age 13–45 yr Medicaid insurance | NR | 776853 | General PP care | More comprehensive insurance | 691867 | Massachusetts (after Medicaid expansion) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 84986 | Maine (after Medicaid contraction) | |
| Redd, 2019, 30484739 | OK, Wl, MD, MN, MO, NY, OR, PA, WA | Non-industry (2007–2013) | Modera te | Live birth | NR | 75082 | Contraceptive care | More comprehensive insurance | 19882 | Transition from the Medicaid 1115 waiver, which allowed states to expand eligibility to some individuals otherwise ineligible Medicaid coverage, to the State Plan Amendment, which provides contraceptive care to all |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 55200 | Maintenance of the Medicaid 1115 waiver, which allowed states to expand eligibility to some individuals otherwise ineligible Medicaid coverage | |
| Rodriguez, 2008, 18692614 | OR | NR (2000–2006) | Modera te | Convenience sample based on available billing data | NR | 11526 | Contraceptive care | More comprehensive insurance | 7832 | Before policy requiring undocumented immigrants and legal immigrants within 5 years of immigration with Emergency Medicaid to pay for sterilization following vaginal delivery |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 3694 | After policy requiring undocumented immigrants and legal immigrants within 5 years of immigration with Emergency Medicaid to pay for sterilization following vaginal delivery | |
| Rodriguez, 2021, 34910148 | OR, SC | Non-industry (2014–2019) | Modera te | Age 15–44 yr Low-income, noncitizen, Emergency Medicaid. | LARC | 27667 | General PP care | More comprehensive insurance | 15465 | Oregon (after Medicaid expansion) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | General PP care | Less comprehensive insurance | 12202 | South Carolina (no Medicaid expansion) | |
| Schuster, 2022, 34670222 | MO, NE, OK, UT, WY | Non-industry (2012–2015) | Modera te | Family income <100%or>400% of FPL | Uninsured for pregnancy | 9472 | General/ Overall PP care | More comprehensive insurance | 4797 | After Medicaid expansion (2014–2015) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 4675 | Before Medicaid expansion (2012–2013) | |
| Smith, 2021, 34109490 | GA | NR(2015–2017) | Modera te | Age <44 yr | NR | 5648 | Contraceptive care | More comprehensive insurance | 3683 | After Medicaid policy covering inpatient LARC (2016–2017) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 1965 | Before Medicaid policy covering inpatient LARC (2015) | |
| Steenland, 2021a, 33523747 | SC | Non-industry (2010–2014) | Modera te | Age 12–50 yr Births covered by South Carolina Medicaid | NR | 154163 | Contraceptive care | More comprehensive insurance | NR | After Medicaid policy of payment for immediate PP LARC (Feb 2012–2014) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | NR | Before Medicaid policy of payment for immediate PP LARC (2011-Jan 2012) | |
| Steenland, 2021 b, 35977301 | AR | Industry (2013–2015) | High | Age>19yr | NR | 50364 | General PP care | More comprehensive insurance | 40785 | After Medicaid expansion (2014–2015) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 9579 | Before Medicaid expansion (2013) | |
| Symum, 2022, 35628011 | FL | Not funded (2010–2017) | Modera te | Hospital delivery | NR | 1454699 | General PP care | More comprehensive insurance | 662981 | After Statewide Mandatory Medicaid Managed Care (2014–2017) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 791718 | Before Statewide Mandatory Medicaid Managed Care (2010–2014) | |
| Taylor, 2020, 31397625 | NC | Non-industry (2014–2015) | Modera te | Age>18yr Gestational age <42wk Live birth | Insurance not commercial, Medicaid, or uninsured | 9613 | General/ Overall PP care | Commercial insurance | 4441 | NR |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Medicaid insurance | 4990 | NR | |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | No insurance | 182 | NR | |
| Wang, 2022, 35592081 | TX | NR(2019–2020) | High | Age 14–48 yr Singleton pregnancy | NR | 8876 | General PP care | More comprehensive insurance | 5411 | After Families First Coronavirus Response Act (2020) |
| ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | ▪ | Less comprehensive insurance | 3465 | Before Families First Coronavirus Response Act (2019) |
Abbreviations: AP = antepartum, FPL = federal poverty limit, LARC = long-acting reversible contraception, NR = not reported, PMID = PubMed ID, PP = postpartum, RoB = risk of bias
All studies were retrospective nonrandomized comparative studies (NRCSs).
Table C-2.2Key Question 2: Extension of healthcare or insurance coverage – summary of sample details
| Author, Year, PMID | Age in Years, Mean (SD) or as Specified | BMI, Mean (SD) or as Specified | Race, N (%) | Educational Attainment in Years, Mean (SD) or as Specified | Employment Status | SES | Miscellaneous N (%) | Chronic Conditions | Delivery Type | Offspring Characteristics |
|---|---|---|---|---|---|---|---|---|---|---|
| Arora, 2018, 29490290 | 30 (5.4) | NR |
W: 363 (30.7) B: 592 (50.0) A: 10 (0.9) H: 186 (15.7) O: 33 (2.8) |
No college: 785 (66.3) Some college: 399 (33.7) | NR | NR | Medicaid: 1030 (87) | NR |
V: 698 (59.0) C: 486 (41.0) | Preterm birth: 234 (19.8) |
| Austin, 2022, 34974107 |
18–24: (44.8) 25–29: (28.3) 30–34: (16.9) >35: (9.9) | NR |
W: (43.2) B: (20.5) H: (28.9) O1: (7.5) |
Less than HS (26.5) HS diploma or GED (38.9) Some college (28.1) College degree or more (6.5) | NR | NR | Medicaid: (74.2) | NR | NR | NR |
| Brant, 2021, 34619694 | 30.3 (5.5) | 32.6 (6.8) |
W: 5526 (64.5) B:1592 (18.7) H: 459 (5.4) O: 939 (11.4) | NR | NR | NR | Medicaid: 2840 (33.3) | HTN: 768 (9) |
V: 5902 (69.3) C: 2614 (30.7) |
Stillbirth: 0 Spontaneous or induced abortion: 0 Preterm birth: 695 (8.2) Neonatal death: 0 |
| Caudillo, 2022, 35488950 |
<20: (5.9) 20–24: (20.7) 25–29: (30.5) 30–34: (28.3) ≥35: (14.4) | NR |
W: (61.9) B: (13.2) A: (4.6) H: (16.3) O1: (4.0) |
<HS (13.3) HS (23.6) Some college (28.8) Bachelors or more (34.3) | NR | NR | Medicaid: (42.8) | NR |
V: (67.9) C: (32.1) | NR |
| Cilenti, 2015, 25627330 | NR | NR | NR | NR | NR | NR |
Medicaid: NC Medicaid: 1969 (100) | NR | NR | NR |
| DeSisto, 2020, 32335806 |
<20: (11) 20–24: (31.7) 25–29: (29.6) 30–34: (18.5) >35: (9.3) | NR |
W: (55.6) B: (17.4) A: (13.4) H: (13.7) |
<High school/GED (19.8) High school diploma/GED (38.9) >High school/GED (40.8) Unknown (0.6) | NR | NR | Medicaid: (100) |
HDP: Gestational HTN (5.3) HTN: Prepregnancy HNT (2.3) GD: (6.6) DM: Prepregnancy diabetes (1.2) |
V: (74.4) C: (25.6) |
Multiple births (1.2) Stillbirth (0) Spontaneous or induced abortion (0) Preterm birth (9.3) |
| Dunlop, 2020, 32958368 |
20–24: 61270 (44.3) 25–34: 67255 (48.6) 35–44: 9901 (7.1) | NR |
W: 87855 (63.5) B: 41313 (29.8) H: 6121 (4.4) O: 3151 (2.3) |
Unknown: 1252 (0.9) College graduate: 6663 (4.8) Some college: 54028 (39) HS graduate: 52157 (37.5) Less than HS graduate: 24326 (17.8) | NR | NR |
Medicaid: Ohio Medicaid: NR (100) | NR | NR | NR |
| Eliason, 2021, 34870677 |
18–24: 1862 (37) 25–30: 1483 (29.5) 30–34: 1066 (21.2) 35–39: 479 (9.5) ≥40: 143 (2.8) | NR |
W: 2413 (47.9) B: 730 (14.5) A: 144 (2.8) H: 973 (19.3) O1: 315 (6.3) |
HS or less 2472 (49.1) More than HS 2494 (49.5) Missing 68 (1.4) | NR | NR | NR | NR | NR | NR |
| Eliason, 2022, 35259409 |
18–24: (49.6) 25–29: (28.9) 30–34: (14.3) 35–39: (5.6) ≥40: (1.6) | NR |
W: (65.5) B: (14.7) A: (1.5) H: (12.8) O1: (4.6) |
HS or less (56.1) More than HS (42.8) NR (1.1) | NR | NR | NR | NR | NR | NR |
| Gordon, 2020, 31905073 |
19–24: 27395 (41.1) 25–39: 38125 (57.2) 40–53: 1152 (1.7) | NR | NR | NR | NR | NR | Medicaid: 66672 (100) | NR | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 Neonatal death: 0 |
| Koch, 2022, 35588793 | 27.6 (5.9) |
BMI ≤30: 2910 (46.7) BMI ≤30: 3323 (53.3) |
W: 2014 (32.3) B: 3351 (53.8) A: 233 (3.7) H: 265 (4.3) | NR | NR | NR | Medicaid: 3902 (62.6) | NR |
V: 3858 (61.9) C: 2354 (37.8) | NR |
| Kozhimannil, 2011, 21485419 | 33.0 (95% CI 32.8, 33.2) | NR | NR | NR | Employed: 2509 (100) |
Low*: 417 (16.6) Not low*: 2092 (83.4) | Medicaid: 0 (0) | GD: 99 (4) |
V: 1658 (66.1) C: 851 (33.9) | Preterm birth: 233 (9.3) |
| Kramer, 2021, 33849768 |
<20: 3803 (8.4) 20–24: 12876 (28.5) 25–29: 14639 (32.4) 30–34: 9201 (20.4) ≥35: 4681 (10.4) | NR |
W: 22562 (49.9) B: 10517 (23.3) H: 7696 (17) O: 4425 (9.8) | NR | NR | NR | Medicaid: 45200 (100) | NR | NR | NR |
| Liberty, 2020, 31846612 | 25.0 (5.4) | NR |
W: 83788 (44.7) B: 86869 (46.3) H: 6780 (3.6) O1: 1769 (0.9) | NR | NR | NR | Medicaid: 164004 (100) |
HDP: 12354 (6.6) HTN: Chronic HTN 5586 (3) GD: 10072 (5.4) DM: Prepregnancy diabetes 1958 (1) |
V: 124451 (66.4) C: 63064 (33.6) |
Multiple births: (0) Preterm birth 20447 (10.9) |
| Margerison, 2021, 34606358 | NR | NR |
W: 27970 (49.1) B: 9969 (17.5) A: 1196 (2.1) H: 13890 (24.4) O1: 1709 (3) O2: 2507 (4.4) | NR | NR | NR | Medicaid: 31957 (56.1) | NR | NR | NR |
| Myerson, 2020, 33136489 |
20–24: 5680 (37.7) 25–29: 4888 (32.5) 30–34: 2900 (19.3) 35–39: 1226 (8.1) 40+: 326 (2.2) | NR |
W: 7524 (50) B: 2608 (17.3) A: 1469 (9.8) H: 3459 (23) |
<12 years: 3392 (22.5) 12 years: 5605 (37.2) 13–15 years: 4799 (31.9) ≥16 years: 1480 (9.8) | NR | NR | NR | NR | NR |
Stillbirth: 0 Neonatal death: 0 Congenital anomalies: 0 |
| Okoroh, 2018, 29530670 | NR | NR | NR | NR | NR | NR | Medicaid: 57894 (100) | NR | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 Neonatal death: 0 |
| Pace, 2022, 34908011 | NR | NR | NR | NR | NR | NR | Medicaid: (100) | NR | NR | NR |
| Redd, 2019, 30484739 |
≤20: 6365 (9) 20–24: 16390 (22) 25–34: 39223 (52) ≥35: 13097 (17) | NR |
W: 44084 (59) B: 12631 (17) A: 5357 (7) O1: 12329 (17) O2: NR |
Some HS: 12274 (16) HS graduate: 18465 (25) Some college: 20787 (28) College graduate: 23108 (31) | NR | NR |
Medicaid: 13862 (18) WIC during pregnancy: 35942 (48) | NR | NR | NR |
| Rodriguez, 2008, 18692614 | 26 (NR) | NR | NR | NR | NR | NR | Immigrants on Emergency Medicaid: 6286 (54.5) | NR |
V: 8520 (73.9) C: 3006 (26.1) | NR |
| Rodriguez, 2021, 34910148 | 29.4 (6) <20: 1172 (4.2) 20–34: 20449 (73.9) ≥35: 6046 (21.9) | NR |
W: 1005 (3.6) B: 473 (1.7) A: 1367 (4.9) H: 18408 (66.5) O1: 5759 (20.8) O2: 70 (0.3) O3: 585 (2.1) | NR | NR | NR |
Immigrant: noncitizens 27667 (100) Medicaid: Emergency Medicaid Coverage 27667 (100) | NR |
V: 20043 (72.4) C: 7624 (27.6) | Preterm birth 2165 (7.8) |
| Schuster, 2022, 34670222 |
<25: 2341 (24.5) 25–34: 6 (65.2) ≥35: 1086 (10.3) | NR |
W: 20382 (82.7) B: 536 (5.2) O: 1741 (12) |
<HS: 614 (5.1) HS: 1997 (18.8) Some college: 3691 (41.1) At least Bachelor’s degree: 3060 (35) | NR |
Household income 100–250% Of federal poverty: 6984 (73) Household income 251–400% Of federal poverty: 2488 (27) | Medicaid: 2082 (20.6) |
HTN: 449 (3.6) DM: 243 (2) | NR | NICU: 2207 (11.8) |
| Smith, 2021, 34109490 | NR | NR | NR | NR | NR | NR | Medicaid: 4417 (78.2) | NR | NR | NR |
| Steenland, 2021a, 33523747 |
24.9 (5.5) 12–19: 23778 (15.4) 20–50: 13 (84.6) | NR |
W: 65770 (42.8) B: 65958 (42.9) H: 15584 (10.1) O: 6335 (4.1) | NR | NR | NR | Medicaid: 154163 (100) | NR | NR | NR |
| Steenland, 2021b, 35977301 |
27.1 19–24: (44.5) 25–30: (35.5) 31–35: (12.3) 36–50: (8.7) | NR |
W: (62.3) B: (24.3) H: (8.6) O1: (4.8) |
Less than college (88.2) College or higher (11.8) | NR | NR | NR | NR |
V: (66.7) C: (33.3) | NR |
| Symum, 2022, 35628011 |
Median (28) <18: 27026 (1.8) 18–30: 858875 (57.2) 30–40: 566371 (37.8) >40: 47722 (3.2) | NR |
W: 724174 (48.3) B: 347720 (23.2) H: 329438 (22.9) O1: 79979 (5.3) | NR | NR | NR | Medicaid beneficiaries (54.6) | NR |
V: 915390 (61.1) C: 584604 (38.9) | Preterm birth 122566 (8.1) |
| Taylor, 2020, 31397625 |
18–24: 2088 (21.7) 25–34: 5698 (59.3) ≥35: 1827 (19) |
Under-weight: 94 (1.0) Normal: 3586 (37.3) Overweig ht: 2897 (30.1) With obesity: 2400 (25.0) With severe obesity: 636 (6.6) |
W: 2709 (28.2) B: 2593 (27.0) H: 2881 (30.0) O: 1430 (14.9) | NR | NR | NR | Medicaid: 4990 (51.9) |
HTN: 269 (2.8) DM: 120 (1.2) | NR |
Stillbirth: 0 Spontaneous or induced abortion: 0 Neonatal death: 0 |
| Wang, 2022, 35592081 |
26.9 (5.5) 14–24: 3107 (35) 25–34: 4704 (53) 35–48: 1065 (12) | NR | NR | NR | NR | NR | NR |
HTN: 440 (5) DM: 204 (2.3) Asthma 661 (7.4) | NR |
Multiple births: (0) Preterm birth 1934 (21.8) |
Abbreviations: A = Asian, B = Black, BMI = body mass index, C = Cesarean delivery, CV = cardiovascular, DM = diabetes mellitus, GD = gestational diabetes, H = Hispanic, HS = high school, HTN = hypertension, O = Other, PMID = PubMed ID, SD = standard deviation, SES = socioeconomic status, V = vaginal delivery, W = White, WIC= women, Infants, and Children
- *
Defined as living in a census tract with either >25% of adults having less than a HS education or >10% of households living below the poverty level.
No studies reported on sexual/gender identities or substance use disorders.
- Results: Design, Arm, and Sample Details - Postpartum Care up to 1 Year After Pr...Results: Design, Arm, and Sample Details - Postpartum Care up to 1 Year After Pregnancy: A Systematic Review and Meta-Analysis
- Appendix References - Partial Breast Irradiation for Breast CancerAppendix References - Partial Breast Irradiation for Breast Cancer
- Sensitivity Analysis - Partial Breast Irradiation for Breast CancerSensitivity Analysis - Partial Breast Irradiation for Breast Cancer
- Preface - Serum Free Light Chain Analysis for the Diagnosis, Management, and Pro...Preface - Serum Free Light Chain Analysis for the Diagnosis, Management, and Prognosis of Plasma Cell Dyscrasias
- Quality Table - Interventional Treatments for Acute and Chronic Pain: Systematic...Quality Table - Interventional Treatments for Acute and Chronic Pain: Systematic Review
Your browsing activity is empty.
Activity recording is turned off.
See more...