All rights reserved. This material may be freely reproduced for educational and not-for-profit purposes. No reproduction by or for commercial organisations, or for commercial purposes, is allowed without the express written permission of NICE.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Introduction
This Evidence Update identifies new evidence that might reinforce or generate future change to the practice laid out in the following reference guidance:
 1
Transient loss of consciousness. NICE clinical guideline 109 (2010). Available from www.nice.org.uk/guidance/CG109
1
Transient loss of consciousness. NICE clinical guideline 109 (2010). Available from www.nice.org.uk/guidance/CG109
Approximately 1700 pieces of evidence were identified and assessed of which 26 were selected for the Evidence Update (see Appendix A for details of the evidence search and selection process). An Evidence Update Advisory Group, comprised of subject experts, reviewed the prioritised evidence and provided a commentary.
Other relevant guidance
The focus of the Evidence Update is on the guidance stated above. However, some studies make reference to the following guidance:
- Guidelines for the diagnosis and management of syncope (version 2009). European Society of Cardiology (2009). Available from www.escardio.org/guidelines-surveys/escguidelines/guidelinesdocuments/guidelines-syncope-ft.pdf
Feedback
If you have any comments you would like to make on this Evidence Update, please email ku.shn.ecnedive@sutcatnoc
Key messages
The following table summarises what the Evidence Update Advisory Group (EUAG) decided were the key messages for this Evidence Update. It also indicates the EUAG’s opinion on whether new evidence identified by the Evidence Update reinforces or has potential to generate future change to the current guidance listed in the introduction.
The relevant NICE guidance development centres have been made aware of this evidence which will be considered when guidance is reviewed. For further details of the evidence behind these key messages and the specific guidance which may be affected, please see the full commentaries.
| Effect on guidance | ||
|---|---|---|
| Key message | Potential change | No change |
| Initial assessment | ||
| ✓ | |
| ✓ | |
| ✓ | |
| ✓ | |
| ✓ | |
| ✓ | |
| Further assessment and referral | ||
| ✓ | |
| ✓ | |
| Specialist cardiovascular assessment and diagnosis | ||
| ✓ | |
| ✓ | |
| ✓ | |
| If the cause of TLoC remains uncertain | ||
| ✓ | |
1. Commentary on new evidence
These commentaries analyse the key references identified specifically for the Evidence Update, which are identified in bold text. Supporting references are also provided.
1.1. Initial assessment
Syncope and cholinesterase inhibitor-treated dementia
Cholinesterase inhibitors are used commonly for the treatment of dementia but can also cause symptomatic bradycardia and syncope. A large population-based retrospective cohort study by Gill et al. (2009) used a Canadian healthcare database to assess the relationship between cholinesterase inhibitor use and syncope-related outcomes.
A total of 19,803 community-dwelling older adults with dementia who were prescribed cholinesterase inhibitors and 61,499 controls who were not treated with cholinesterase inhibitors were included in the study.
Hospital visits for syncope were more frequent in patients taking cholinesterase inhibitors compared to the control group (31.5 vs 18.6 events per 1000 person-years; hazard ratio [HR] = 1.76, 95% confidence interval [CI] 1.57 to 1.98). In addition, the following syncope-related events were seen more frequently in patients taking cholinesterase inhibitors compared with controls: hospital visits for bradycardia (6.9 vs 4.4 events per 1000 person-years respectively; HR = 1.69, 95% CI 1.32 to 2.15), permanent pacemaker insertion (4.7 vs 3.3 events per 1000 person-years respectively; HR = 1.49, 95% CI 1.12 to 2.00) and hip fracture (22.4 vs 19.8 events per 1000 person-years respectively; HR = 1.18, 95% CI 1.04 to 1.34). Based on this observational study, the authors concluded that use of cholinesterase inhibitors is associated with increased risk of serious adverse events (that is, syncope, bradycardia, pacemaker insertion and hip fracture) in older patients with dementia.
Evidence from this study highlighted that cholinesterase inhibitors can cause syncope, which is important for clinicians to consider when assessing patients. NICE CG109 emphasises the need to assess and record current medication in the initial assessment algorithm. Diuretics are the only example listed in current guidance.
This evidence was also reviewed by the National Prescribing Centre’s MeReC Rapid Review 343.
Key reference
- Gill SG, Anderson GM, Fischer HD et al. (2009) Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: A population-based cohort study. Archives of Internal Medicine 169: 867–73. Full text: http://archinte
.ama-assn .org/cgi/content/full/169/9/867 [PubMed: 19433698]
Early symptoms and assessment of syncope in the elderly
An Italian multicentre cross-sectional observational study by Galizia et al. (2009) investigated consecutive admissions to six centres (inpatient geriatric acute care departments and outpatient clinics) and assessed the ability of specific pre-event symptoms to predict cardiac and non-cardiac syncope in 242 elderly patients (mean age 79±8 years). All participants were assessed against the European Society of Cardiology guidelines.
Multivariate regression analysis (adjusted for sex and age) was used. A diagnosis of non-cardiac syncope was made in 174 participants (75.4%) who showed the highest prevalence of symptoms (p < 0.01). The most common symptoms of this group (all of which were statistically more prevalent than in cardiac syncope [indicated by p values], and were predictive of non-cardiac syncope [indicated by relative risk, RR]) were awareness of being about to faint (p = 0.006, RR = 2.1, 95% CI 1.04 to 4.49), sweating (p = 0.002, RR = 2.8, 95% CI 1.21 to 6.89), blurred vision (p = 0.01, RR = 3.5, 95% CI 1.34 to 9.59) and nausea (p = 0.02, RR = 3.7, 95% CI 1.26 to 11.2). Breathlessness was more common in cardiac than non-cardiac syncope (p = 0.05) and was the only symptom predictive of cardiac syncope (RR = 5.5, 95% CI 1.0 to 30.2).
It is worth noting that the study only looked at cardiac and non-cardiac syncope; patients in whom the cause of syncope was unknown were excluded from the data analysis.
This study of elderly patients emphasises the importance of a detailed clinical history, and suggests that pre-event symptoms may play a useful role in distinguishing between non-cardiac and cardiac syncope, with breathlessness a potential indicator of cardiac syncope. These findings may be a consideration for future reviews of NICE CG109.
Key reference
- Galizia G, Abete P, Mussi C et al. (2009) Role of early symptoms in assessment of syncope in elderly people: Results from the Italian group for the study of syncope in the elderly. Journal of the American Geriatrics Society 57: 18–23. Abstract: www
.onlinelibrary.wiley .com/doi/10.1111/j .1532-5415.2008.02070.x/abstract [PubMed: 19054186]
Clinical decision rules
A single centre, prospective, observational study (Risk Stratification of Syncope in the Emergency Department [ROSE] study) in the UK by Reed et al. (2010) was designed to develop and validate a clinical decision rule (CDR) to predict 1-month serious outcomes and all-cause death in patients presenting to the accident and emergency department (A&E) with syncope. A CDR was developed based on 550 patients (the derivation cohort) and tested on another 550 patients (the validation cohort). All participants received care according to existing treatment protocols.
One-month serious outcome or all-cause death occurred in 40 (7.3%) patients in the derivation cohort; independent predictors were a brain natriuretic peptide (BNP) concentration of 300 picograms or more, positive faecal occult blood, haemoglobin levels of 90 g/l or less, oxygen saturation of 94% or less and Q-wave on the presenting electrocardiogram (ECG). One-month serious outcome or all-cause death occurred in 39 (7.1%) patients in the validation cohort. The CDR (the ‘ROSE rule’) had a sensitivity and specificity of 87.2% and 65.5%, respectively. An elevated BNP concentration was the single major predictor of serious cardiovascular outcomes (36%; 8 of 22 events) and all-cause death (89%, 8 of 9 deaths).
The use of BNP in the decision process appeared to add significantly to the clinical assessment that was already undertaken. BNP increased the sensitivity of ‘standard’ processes, although it is unclear what these were in the current study.
BNP testing currently has insufficient evidence for it to affect current practice in the assessment of patients after transient loss of consciousness (TLoC). The simplicity of the ROSE rule is appealing at a practical level and could be adopted easily by junior doctors. However, further validation may be needed.
Evidence from Reed et al. (2010) is unlikely to affect NICE CG109. However, it highlighted BNP as a potential diagnostic tool, although the transferability needs to be confirmed with further research.
A systematic review by Serrano et al. (2010) assessed the methodological quality and prognostic accuracy of CDRs in syncope patients in the accident and emergency department. Six electronic databases were searched, conference abstracts were scanned for unpublished studies and experts were consulted for additional potential references; a total of 18 eligible studies (comprising 10,944 patients) that derived or validated CDRs were identified and included in the review.
The most frequent methodological weaknesses were deficiencies in outcome and inter-rater reliability assessment. Meta-analyses of the San Francisco Syncope rule showed sensitivity of 86% (95% CI 83 to 89%) and specificity of 49% (95% CI 48 to 51%); a sensitivity of 95% (95% CI 88 to 98%) and specificity of 31% (95% CI 29 to 34%) was recorded for the Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL) risk score. Differences in study design and ECG interpretation were considered plausible explanations for the variable prognostic performance of the San Francisco Syncope rule.
This review of CDRs included those looked at during the development of NICE CG109 and acknowledged similar issues as those noted in the NICE process (such as low patient numbers in studies). The conclusions are unlikely to affect NICE CG109, and reinforce current recommendations that clinicians should not rely solely on CDRs when assessing syncope patients in the accident and emergency department.
A retrospective Canadian study by Thiruganasambandamoorthy et al. (2010) validated the San Francisco Syncope rule in a non-US healthcare setting and included patients aged 16 years or older who fulfilled the definition of syncope (transient loss of consciousness with complete recovery) and presented to a tertiary care A&E during an 18-month period. The study used largely the same design as the San Francisco Syncope rule study (Quinn et al. [2004]) in order to prevent anomalous results.
Patient characteristics, five predictors for the San Francisco Syncope rule (history of congestive heart failure, haematocrit level under 30%, abnormal ECG characteristics, shortness of breath, and triage systolic blood pressure under 90 mmHg), and outcomes (as per the original study) were reviewed. Of 915 visits screened, 505 were included; 49 (9.7%) visits were associated with serious outcomes.
The rule showed sensitivity of 90% (44 of 49 outcomes, 95% CI 79 to 96%) and specificity of 33% (95% CI 32 to 34%). Inclusion of ECG to monitor abnormalities could improve sensitivity to 96% (47 of 49 outcomes, 95% CI 87 to 99%). Two deaths were not predicted by physicians; however, the rule would have predicted all three deaths that occurred after A&E discharge. Implementing the rule in the Canadian setting would increase admission rates from 12.3 to 69.5%.
The San Francisco Syncope Rule performed with comparable sensitivity but significantly poorer specificity than previously reported, indicating that further refinement and testing of the rule is required. The authors concluded that implementation of the rule would significantly increase admission rates.
Evidence from this study confirms previously reviewed data and is unlikely to affect NICE CG109. However, it highlights the need for more research to refine the San Francisco Syncope Rule or to develop a new CDR.
A prospective cohort single centre study by Romme et al. (2009) evaluated the Calgary Syncope Symptom Score, which was designed to distinguish vasovagal syncope from other causes of syncope by history taking.
A total of 380 patients presenting with TLoC were evaluated; diagnoses of vasovagal syncope based on the Calgary Score were compared with final diagnoses obtained after additional testing and 2-year follow-up. The sensitivity of the Calgary Score was 87% (95% CI 82 to 91%) and specificity 32% (95% CI 24 to 40%). The sensitivity of the Calgary Score was comparable with that reported in the original study used to develop the score (Sheldon et al. 2006), but specificity was much lower. Misdiagnosis of patients with syncope as vasovagal was most common in patients with psychogenic pseudosyncope (specificity 21%) and was also noted in patients with cardiac syncope (specificity 32%).
The low sensitivity may lead to misdiagnosis of TLoC and suggests poor utility of the Calgary Score in clinical practice. Further, the maximum duration stated in the definition of TLoC that was used (< 1 hour) may not be universal; NICE CG109 does not specify a time duration.
Evidence from this study has no impact on NICE CG109, although the prominence of functional illness presenting as TLoC was notable. This evidence is important in highlighting the limitations of the Calgary Syncope Symptom Score. Awareness-raising is needed to ensure that A&E settings do not use this score in patient triage pathways.
Key references
- Reed MJ, Newby DE, Coull AJ et al. (2010) The ROSE (Risk Stratification of Syncope in the Emergency Department) Study. Journal of the American College of Cardiology 55: 713–21. Full text: www
.content.onlinejacc .org/cgi/reprint/55/8/713.pdf [PubMed: 20170806] - Romme JJCM, van Dijk N, Boer KR et al. (2009) Diagnosing vasovagal syncope based on quantitative history-taking: Validation of the Calgary Syncope Symptom Score. European Heart Journal 30: 2888–96. Full text: www
.eurheartj.oxfordjournals .org/content/30/23/2888.full.pdf [PubMed: 19687157] - Serrano LA, Hess EP, Bellolio MF et al. (2010) Accuracy and quality of clinical decision rules for syncope in the emergency department: A systematic review and meta-analysis. Annals of Emergency Medicine 56 : 362–73. Abstract: www
.annemergmed.com/article /S0196-0644%2810%2900482-8 /abstract [PMC free article: PMC2946941] [PubMed: 20868906] - Thiruganasambandamoorthy V, Hess EP, Alreesi A. et al. (2010) External validation of the San Francisco Syncope Rule in the Canadian setting. Annals of Emergency Medicine 55: 464–72. Abstract: www
.annemergmed.com/article /S0196-0644%2809%2901619-9 /abstract [PubMed: 19944489]
Supporting references
- Quinn JV, Stiell IG, McDermott DA et al. (2004) Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Annals Emergency Medicine 43: 224–32. Abstract: www
.annemergmed.com/article /S0196-0644(03)00823-0/abstract [PubMed: 14747812] - Sheldon R, Rose S, Connolly S, Ritchie D, Koshman ML, Frenneaux M. (2006) Diagnostic criteria for vasovagal syncope based on a quantitative history. European Heart Journal 27: 344–50. Full text: www
.eurheartj.oxfordjournals .org/content/27/3/344.long [PubMed: 16223744]
Predictors for mortality and re-hospitalisation in syncope
A single centre observational study by Sule et al. (2010) looked at aetiologies for syncope and risk factors for mortality and re-hospitalisation (based on review of patients’ medical records) over a 27-month follow-up of 325 patients (mean age 66 years) hospitalised for syncope. No patients were lost to follow-up.
Causes of syncope were diagnosed in 241 of 325 patients (74%). Thirteen (4%) patients were re-hospitalised for syncope and 38 (12%) died. Independent risk factors for re-hospitalisation for syncope were diabetes (odds ratio [OR] = 5.7, 95% CI 1.6 to 20.4), atrial fibrillation (OR = 4.0, 95% CI 1.0 to 15.6) and smoking (OR = 4.6, 95% CI 1.3 to 16.8). Independent risk factors for time to mortality were diabetes (HR = 2.7, 95% CI 1.4 to 5.2), coronary artery bypass graft surgery (HR = 2.9, 95% CI 1.3 to 6.5), history of malignancy (HR = 2.5, 95% CI 1.2 to 5.2), use of narcotics (HR = 4.0, 95% CI 1.7 to 9.8), smoking (HR = 2.8, 95% CI 1.4 to 5.5), atrial fibrillation (HR = 2.4, 95% CI 1.0 to 5.4) and volume depletion (HR = 2.8, 95% CI 1.4 to 5.8).
In this study, characterisation as high risk by the OESIL risk score or San Francisco Syncope rule was not significantly associated with re-hospitalisation or long-term mortality; the authors concluded that these scores were designed to identify short-term risks and guide the admission and management of syncope patients in the A&E.
Further studies are needed to confirm the relationship between these risk factors and syncope, as the identified factors could also be considered as general risk factors for hospitalisation and mortality. In addition, the study was in a single centre with a low number of patients in each group, potentially limiting the transferability of findings.
Evidence from this study is unlikely to affect NICE CG109. However, it highlights the need for further research to develop long-term risk prediction tools for patients with syncope.
Key reference
- Sule S, Palaniswamy C, Aronow WS et al. (2011) Etiology of syncope in patients hospitalized with syncope and predictors of mortality and rehospitalization for syncope at 27-month follow-up. Clinical Cardiology 34: 35–8. Full text: www
.onlinelibrary.wiley .com/doi/10.1002/clc.20872/pdf [PMC free article: PMC6652658] [PubMed: 21259276]
Aetiology and outcomes in high-risk patients
A prospective, observational cohort study by Grossman et al. (2011) evaluated outcomes for high-risk patients diagnosed with benign causes of syncope after standard A&E assessments. A&E assessments varied from patient to patient, but all had a complete history, physical examination and ECG (although testing was not mandatory in the study). Eligible patients (aged ≥ 18 years) were followed up to 30 days to identify adverse outcomes. Benign aetiology was defined as vasovagal syncope or dehydration.
Benign causes were established in 164 of 293 (56%, 95% CI 50 to 62%) cases (among the benign cases, 40% of syncope was dehydration-related, and 60% was vasovagal syncope); but pathological conditions were identified during A&E evaluation in 11 of these 164 (7%, 95% CI 3 to 11%) cases, all of whom were admitted to hospital. The remaining 153 patients with benign presentations and a normal A&E assessment had no adverse outcomes at 30 days, while 57 of 129 (44%) patients considered to have non-benign aetiologies had adverse outcomes in the hospital or within 30 days. The authors concluded that patients classified as having a benign cause of syncope (vasovagal or dehydration) on the basis of a standard A&E assessment receive no benefit from hospital admission.
This study defined vasovagal syncope as interchangeable with neurocardiogenic, neurally mediated, vasodepressor and situational syncope, whereas NICE CG109 separates vasovagal syncope, carotid sinus syncope and situational syncope and includes these within the broader definition of ‘neurally mediated syncope’.
Evidence from this study addresses formal clinical recognition of dehydration as a contributing cause of syncope and reinforces the importance of history-taking, and the need to record current medications (particularly diuretics, which may cause or contribute to dehydration) as recommended by NICE CG109. Current recommendations already encourage early discharge for uncomplicated vasovagal syncope, situational syncope and orthostatic hypotension. Since dehydration is likely to provoke syncope predominantly by causing orthostatic hypotension and/or triggering vasovagal syncope, the main message from this study is that dehydration, and drug therapy causing dehydration, should be recognised as potentially reversible causes of these mechanisms for syncope as part of the initial assessments recommended by CG109. Once corrected, dehydration alone can be regarded as a benign cause of syncope. However, failure to recognise and treat dehydration effectively may not have a benign outcome.
Key reference
- Grossman SA, Fischer C, Kancharia A et al. (2011) Can benign etiologies predict benign outcomes in high-risk syncope patients? Journal of Emergency Medicine 40: 592–97. Abstract: www
.jem-journal.com/article /S0736-4679%2809%2900788-4 /abstract [PubMed: 19926429]
D-dimer
A prospective cohort study by Stockley et al. (2009) was undertaken as a sub-study of the ROSE study (Reed et al. [2010]; see ‘Clinical decision rules’ in section 1.1 for more details) and aimed to establish whether D-dimer is an independent predictor of 1-month serious outcomes and all-cause death in patients presenting to the A&E with syncope.
D-dimer concentrations were determined from citrated plasma collected at presentation to the A&E; 205 of 237 patients enrolled into the study had suitable plasma samples. Seventeen patients had a serious outcome or death at 1 month (including three patients with a pulmonary embolism and eight with a serious cardiovascular outcome). Ninety-four patients (46%) had a plasma D-dimer concentration above the upper limit of normal, ten of whom had a serious outcome or death at 1 month. However, receiver-operator characteristic curve analysis showed no relationship between plasma D-dimer concentration and serious outcome or death at 1 month. The authors concluded that there is no role for the routine measurement of D-dimer in the management of patients presenting to the A&E with syncope.
This study highlighted the mortality and morbidity associated with TLoC. However, the studied patient group was relatively old (median age 71 years) and unlikely to be representative of the general population with TLoC, which tends to be younger. The question of false positives was raised, and a hypothesis regarding potential elevation of D-dimer as a result of soft tissue injury resulting from a collapse was also raised but not further addressed.
Evidence from this study has no impact on NICE CG109.
Key reference
- Stockley CJ, Reed MJ, Newby DE et al. (2009) The utility of routine D-dimer measurement in syncope. European Journal of Emergency Medicine 16: 256–60. Abstract: www
.journals.lww.com /euro-emergencymed/Abstract /2009/10000/The _utility_of_routine _D_dimer_measurement_in.5.aspx [PubMed: 19902561]
1.2. Further assessment and referral
Orthostatic and neurally mediated syncope
A retrospective study by Cooke et al. (2011) reviewed referrals to a tertiary syncope unit to determine the changing prevalence of orthostatic and ‘neurocardiogenic’ syncope (NCS) with increasing patient age.
The study included all consecutive patients (n = 3002, 1914 females and 1088 males) referred to a tertiary referral syncope unit with recurrent falls or orthostatic intolerance over a 10-year period. Patient age ranged from 11 to 91 years with a median (interquartile range; IQR) of 75 (62–81) years.
The most common abnormality was orthostatic hypotension (test positivity of 60.3%); affected patients had a median (IQR) age of 78 (71–83) years and symptomatic patients were significantly younger than asymptomatic (p = 0.03). NCS demonstrated a bimodal age distribution. The median age (IQR) was 77 (68–82) years for the 194 patients with carotid sinus hypersensitivity and 30 (19–44) years for the 80 patients with vasovagal syncope. Patients with isolated postural orthostatic tachycardia syndrome (n = 57, 75% females) had a median (IQR) age of 23 (17–29) years. The authors concluded that the aetiology of syncope changes with age, with the greatest burden of disease in the elderly.
The retrospective nature of the study limits the conclusions that can be drawn; a prospective community-based study is needed.
Although using age to aid diagnosis is of interest, it lacks specificity. Evidence from this study is not expected to alter patient pathways or service commissioning and is unlikely to affect NICE CG109. However, it does offer some insight into the aetiology of TLoC and its variation with age.
Another retrospective study by Ojha et al. (2010) used an autonomic laboratory database of 3700 patients to assess the frequency of syncope in patients with different orthostatic syndromes (postural tachycardia syndrome and orthostatic hypotension).
A total of 810 patients were referred for postural tachycardia syndrome, of which 185 met criteria for postural orthostatic tachycardia syndrome (POTS) and another 328 had orthostatic hypotension.
A significantly higher proportion of patients with POTS had syncope on head-up tilt compared with patients with orthostatic hypotension (38% vs 22%, p < 0.0001). Further, in the POTS group, 90% of those with syncope on head-up tilt had a clinical history of syncope, whereas only 30% of those who did not experience syncope on head-up tilt had a clinical history of syncope (p < 0.0001). The presence or absence of syncope on head-up tilt was not associated with a clinical history of syncope in the orthostatic hypotension group (41% vs 36%, p = 0.49). The authors concluded that syncope occurs more commonly in patients with POTS than in patients with orthostatic hypotension.
The study was limited in being a single-centre retrospective electronic patient record review which used healthy controls from the literature, without matching baseline characteristics precisely to their own study population.
The incidence of POTS is not reported in this publication and this condition may apply to only a small proportion of patients; however, this does not change the significance of these findings.
Evidence from this study is unlikely to affect NICE CG109. However, it may be helpful in raising awareness of POTS, as specialist referral may be needed to ensure optimal management of these patients. Further research is needed to establish the incidence and prevalence of POTS.
Key references
- Cooke J, Carew S, Costelloe A et al. (2011) The changing face of orthostatic and neurocardiogenic syncope with age. QJM 104: 689–95. Abstract: www
.qjmed.oxfordjournals .org/content/104/8/689.short?rss=1 [PubMed: 21382922] - Ojha A, McNeeley K, Heller E et al. (2010) Orthostatic syndromes differ in syncope frequency. The American Journal of Medicine 123: 245–49. Abstract: www
.amjmed.com/article /S0002-9343%2809%2900948-6/abstract [PubMed: 20193833]
Psychogenic non-epileptic seizures
A large cohort study by Duncan et al. (2011) involved patients referred to a first seizure clinic with suspected psychogenic non-epileptic seizures and prospectively identified 68 cases (54 confirmed by video or ECG) of first presentations of psychogenic non-epileptic seizures from a Scottish population of 367,566 over a 3-year period, implying an annual incidence of 4.9 per 100,000.
The identified patient group had high rates of psychological morbidity, including self harm and history of abuse, but half (27 of 54 patients) were free of attacks at 3 months. However, the authors found a high risk of relapse. Patients were referred to a neuropsychologist, but the details of treatment were not provided.
This study has identified a highly complex group of patients that are associated with high A&E re-admission rates and for whom a gap in treatment pathways currently exists.
This evidence emphasises that psychogenic non-epileptic seizures are a common cause of TLoC, and implies that addressing the diagnostic and treatment issues in this group may be a consideration in an update to NICE CG109.
A retrospective study by Song et al. (2010) compared the clinical characteristics of patients with neurally mediated (reflex) syncope who experience ‘seizure-like’ symptoms during a head-up tilt test (HUT) with those who do not display such activity.
Medical records from 226 (of 1383 reviewed) patients with a positive HUT were included in the study. Thirteen (5.75%) patients showed ‘seizure-like’ activities (five [2.21%] with multifocal myoclonic jerky movements, five [2.21%] with focal ‘seizure-like’ activity involving one extremity, and three [1.33%] with upward deviation of the eye balls). There were no significant differences in clinical variables and hemodynamic parameters during HUT between patients with and those without ‘seizure-like’ activity.
The study was limited by being retrospective and based on HUT test reports only and did not review the patient’s general record. Therefore it was not possible to compare ‘seizure-like’ activity during HUT and observed behaviour during syncopal episodes.
These data confirmed that neurally mediated syncope can produce convulsive movements, which can be misinterpreted as epilepsy due to the presence of myoclonic jerky movements during syncope, and does not warrant any change to the recommendations in NICE CG109 for suspected epilepsy.
Key references
- Duncan R, Razvi S, Mulhern S (2011) Newly presenting psychogenic nonepileptic seizures: Incidence, population characteristics, and early outcome from a prospective audit of a first seizure clinic. Epilepsy and Behavior 20: 308–11. Abstract: www
.sciencedirect.com /science/article/pii/S1525505010006694 [PubMed: 21195031] - Song PS, Kim JS, Park J et al. (2010) Seizure-like activities during head-up tilt test-induced syncope. Yonsei Medical Journal 51: 77–81. Full text: www
.eymj.org/Synapse /Data/PDFData/0069YMJ/ymj-51-77.pdf [PMC free article: PMC2799981] [PubMed: 20046517]
Inpatient management
A single centre prospective observational cohort study by Tattersall et al. (2010) involved 540 patients and assessed inpatient management (based on length of hospital stay and investigations performed) of patients with syncope admitted to hospital from a UK A&E.
The median and mean length of stay was 1 day (IQR 1–4) and 6.3 days (standard deviation 15.5), respectively. A total of 392 (73%) patients were admitted to general or acute medicine, 39 (7%) to cardiology, 35 (7%) to medicine of the elderly, 33 (6%) to surgical specialities and the rest to other specialities. A diagnosis was made in 342 (63%) patients (including 33 [85%] of 39 patients admitted to cardiology and 239 [61%] of the 392 patients admitted to general/acute medicine). Application of diagnostic tests varied between specialities; more intensive investigations (including the exercise tolerance test and angiography) were undertaken in patients admitted to cardiology.
The differing levels of diagnosis and variety of diagnostic testing between specialities identified by the study suggest that current inpatient management of syncope may be suboptimal and speciality-dependent.
The median length of stay in hospital of 1 day emphasises the fact that many patients can be managed more effectively in observational medicine (for example, clinical decision units) without the need for formal admission to hospital. Identification of diagnostic yields of the tests undertaken would have been useful in this study. The study also emphasised the need for a standardised approach (for example, the use of diagnostic algorithms) for the investigation and inpatient management of syncope.
Evidence from this study is unlikely to affect NICE CG109. However, it emphasises the need for a study to determine the extent to which NICE CG109 is being used within the NHS and use of an audit tool (reports relating to the uptake of NICE guidance are stored on the Evaluation and Review of NICE Implementation Evidence database [ERNIE] database). In addition, the adoption of NICE CG109 audit support may serve to increase awareness of the guideline among practitioners.
Key reference
- Tattersall LC, Reed MJ. (2010) The inpatient management of syncope. Emergency Medicine Journal 27: 870–72. Abstract: www
.emj.bmj.com/content/27/11/870 .abstract [PubMed: 20682959]
Supporting reference
- NICE clinical guideline 109: audit support. Available from: www
.guidance.nice.org .uk/CG109/AuditSupport/doc/English.
1.3. Specialist cardiovascular assessment and diagnosis
Tilt table testing
A single centre prospective cohort study by Furukawa et al. (2011) involved 380 patients who had previously undergone tilt table testing and aimed to determine a possible relationship between clinical triggers of syncope on responses to head-up tilt, using glyceryl trinitrate (nitroglycerin) or clomipramine provocation.
Glyceryl trinitrate or clomipramine were used as a provocative agent during tilt table tests in non-randomised, sequential cohorts of 252 and 128 patients, respectively. Tilt testing was done either as a diagnostic test for suspected reflex syncope or for biofeedback in definite cases. Definite cases were used to estimate the true sensitivity of tilt testing. A specificity calculation was not possible because no participants definitely did not have reflex syncope.
Syncope was triggered by emotional distress (central trigger), specific situations or prolonged standing (peripheral trigger) and occurred without any detectable trigger in 66, 161 and 153 patients, respectively. Clinical triggers (central versus peripheral versus none) of reflex syncope were compared with type of response to tilt testing and to sensitivity of provocation by glyceryl trinitrate or clomipramine.
In patients with central triggers for reflex syncope, clomipramine challenge had greater sensitivity than glyceryl trinitrate, ‘positive’ responses were more common and cardioinhibitory responses were more likely. In patients with peripheral triggers, glyceryl trinitrate challenge was more sensitive than clomipramine; mixed and vasodepressor responses were more commonly induced in patients by glyceryl trinitrate (41%) compared with clomipramine (24%).
Clomipramine infusion was associated with anticholinergic symptoms (sweating, dry mouth, nausea, heat rash and vomiting) in 23 (18%) patients, ‘neurologic’ symptoms (dizziness, fatigue and headache) in 11 (9%) patients and ‘psychic’ symptoms (sleepiness, confusion and dyskinesia) in 5 (4%) patients. These adverse effects associated with clomipramine infusion suggest that it should not be routinely used. In contrast, the only side effect that was associated with glyceryl trinitrate was transient headache.
Although evidence from this study is relevant to NICE CG109, it is unlikely to affect current guidance. The authors suggested that clomipramine challenge may be better than glyceryl trinitrate in identifying patients for pacemaker therapy, but that further research is needed.
Key reference
- Furukawa T, Maggi R, Solano A et al. (2011) Effect of clinical triggers on positive responses to tilt-table testing potentiated with nitroglycerin or clomipramine. American Journal of Cardiology 107: 1693–97. Abstract: www
.ajconline.org/article /S0002-9149%2811%2900470-X/abstract [PubMed: 21420055]
Computed tomography scans
A prospective study by Al-Nsoor & Mhearat (2010) assessed the use of computed tomography (CT) scans of the head as routine diagnostic tests for patients presenting with syncope.
A total of 292 patients with TLoC presenting to a clinic in Jordan were evaluated; 254 (86.9%) patients underwent CT scan of the head, which is not included as part of the standard investigation for TLoC recommended in NICE CG109. The study identified ten (3.9%) patients with CT abnormalities related to TLoC and 39 (15.3%) with abnormalities unrelated to TLoC.
The authors concluded that routine use of CT head scans as a diagnostic tool for syncope is unjustifiable; however, it is difficult to state this definitively in the absence of a more in-depth analysis of the abnormal cases and what if anything the scan contributed to the subsequent management of these cases. Although the CT scan did not appear to contribute to the diagnosis of TLoC in most cases, the total percentage of patients identified as having abnormalities (19.2%) suggests that CT scans may be justifiable as a screening tool in this apparently high-risk population.
This study would need to be repeated in a UK setting before drawing any firm conclusions about its applicability to the NHS.
Evidence from this study confirms the diagnostic approach taken in NICE CG109, which does not include CT scans.
Key reference
- Al-Nsoor NM, Mhearat AS (2010) Brain computed tomography in patients with syncope. Neurosciences 15: 105–9. Full text: www
.neurosciencesjournal .org/PDFFiles/Apr10/Brain.pdf [PubMed: 20672498]
Implantable event recorders
A prospective multicentre observational study by Edvardsson et al. (2011) assessed the use of the Reveal implantable event recorder (IER) and its effectiveness in the diagnosis of unexplained syncope.
Enrolled patients had syncope or pre-syncope; many patients had numerous non-diagnostic investigations and specialist consultations before IER implantation. Of the recurrent events in 218 of 570 patients analysed (650 patients recruited), IER was reported to be diagnostic in 170 and may have contributed to diagnosis in 13. Diagnosis was not guided by IER in 23 patients and data were inconclusive in 12.
In most patients experiencing recurrent syncope, this occurred more than 30 days after IER implantation and the numbers of people with recurrence increased progressively over 2 years.
This study did not compare different diagnostic strategies for people with unexplained syncope, so is of limited benefit in directing evidence-based clinical guidelines.
Nevertheless the data are consistent with the recommendations in NICE CG109 in discouraging early use of many investigations and discouraging neurology referral for unexplained TLoC, and encouraging early use of an IER in those in whom initial clinical assessment and 12-lead ECG fail to identify a likely cause and in whom the frequency of recurrent events is unlikely to allow documentation with an external event recorder. It should also be noted that pre-publication information from this study was available to the GDG when NICE CG109 was developed.
Use of IERs is constrained by the limited memory, sensing artefacts and necessary manual memory download associated with currently available devices, but may be improved by remote monitoring technology that has capacity for automatic data transfer. A prospective, non-randomised single centre study by Arrocha et al. (2010) assessed the effectiveness of new IER device with wireless technology, by determining the effect of direct IER transmission to a central ECG monitoring centre on the burden of data reviewed by the physician.
Forty patients with unexplained syncope were implanted with a new IER and followed for 8.5±5.1 months; the transmitted recordings underwent a 2-step review process (initial algorithmic filtering followed by human overread at a monitoring centre). A total of 223,226 ECG recordings were transmitted at a rate of approximately 660 recordings per patient per month. Initial algorithmic filtering eliminated 191,305 ECGs as artefact (89%), with monitoring centre overread required for 31,921 ECGs. A total of 117 ECGs needed further evaluation by the physician (0.0053%).
This study found use of the automatic IER with wireless technology to be a feasible option for remote ECG monitoring by IERs; however, there were problems with excessive ECG burden from the recording. The choice of IER used would be determined by the individual clinician.
The cost-effectiveness of the device was not discussed in this publication. Section 4.5 (‘Cost effectiveness of implantable event recorders in people with TLoC’) of NICE CG109 recommends that patients with infrequent TLoC episodes (every 1–2 weeks or less) in whom a cardiac cause is suspected be offered an implantable event recorder. However, the guideline also states that the cost-effectiveness of this approach remains unclear. Further research is needed.
Evidence from this study has no impact on NICE CG109, as the use of IERs is already recommended in patients with infrequent TLoC. However, it shows that there is a possible option for remote ECG monitoring from IERs.
Key references
- Arrocha A, Klein GJ, Benditt DG et al. (2010) Remote electrocardiographic monitoring with a wireless implantable loop recorder: minimizing the data review burden. Pacing & Clinical Electrophysiology 33: 1347–52. Abstract: www
.onlinelibrary.wiley .com/doi/10.1111/j .1540-8159.2010.02857.x/abstract [PubMed: 20727097] - Edvardsson N, Frykman V, van Mechelen R et al. (2011) Use of an implantable loop recorder to increase the diagnostic yield in unexplained syncope: Results from the PICTURE registry. Europace 13: 262–9. Full text: www
.europace.oxfordjournals .org/content/13/2/262 .full.pdf+html [PMC free article: PMC3024039] [PubMed: 21097478]
Structural heart disease
A prospective cohort study by Sheldon et al. (2010) developed a simple evidence-based point-score to distinguish vasovagal syncope (VVS) from ventricular tachycardia (VT) in patients with structural heart disease. The point score was derived from logistic regression analysis of the contribution of symptoms to diagnoses. A 118-item questionnaire was used to assess symptoms, which was developed with expert input from medical staff at the syncope clinic and arrhythmia consultants, and subsequent testing.
A total of 134 patients with syncope and structural heart disease were included in the study, which involved completion of the 118-item questionnaire as well as non-invasive and invasive diagnostic tests. Twenty-one patients had tilt-positive VVS, 78 had clinically declared or inducible VT and 35 had unexplained syncope. The following factors predicted VT: male sex and age at onset of 35 years or more. The following factors predicted VVS: prolonged sitting or standing. The point score correctly classified 92% of patients, and diagnosed VT with 99% sensitivity and 68% specificity.
The authors concluded that the causes of syncope in patients with structural heart disease, and their clinical outcomes can be estimated accurately based on the clinical history, which can be used to rule out VT as the basis for syncope.
The developed point-score can be used at the bedside and is a cheaper method of testing than many of the other methods available. The study is limited by the number of patients and in addition, the applicability of scoring systems varies according to patient population, necessitating a high level of validation.
Evidence from this study emphasises the need for taking a good clinical history in patients with syncope, which is already highlighted in NICE CG109. However, the scoring system and its relevance to assessment of patients may need to be evaluated further.
Key reference
- Sheldon R, Hersi A, Ritchie D et al. (2010) Syncope and structural heart disease: Historical criteria for vasovagal syncope and ventricular tachycardia. Journal of Cardiovascular Electrophysiology 21: 1358–64. Abstract: www
.onlinelibrary.wiley .com/doi/10.1111/j .1540-8167.2010.01835.x/abstract [PubMed: 20586825]
Standardised diagnostic evaluation
Mitro et al. (2011) described a prospective, observational study to evaluate the aetiology and diagnostic yield of a standardised diagnostic work-up, in a selected group of patients, in a syncope unit.
It should be noted that although the study approach is reportedly based on European Society of Cardiology guidelines, the paper refers to guidelines that were published after study recruitment was completed.
A total of 501 patients (mean age 65 years) were evaluated prospectively and underwent initial evaluation (history, physical evaluation and a 12-lead ECG) and specific tests based on the suspected aetiology. There were some inconsistencies in methodology (for example, diagnosis of orthostatic hypotension required a symptomatic fall in blood pressure but diagnosis of carotid sinus syncope apparently did not require induction of symptoms during testing).
Echocardiography was used in 55% of people, with a diagnostic yield of only 2%, providing support for the NICE CG109 recommendation that echocardiography should be used only with clinical or ECG suspicion of structural heart disease.
Thirty-nine of 139 patients with ‘organic heart disease’ had reflex syncope, supporting the emphasis in NICE CG109 that orthostatic hypotension and reflex syncope should be considered in those with structural heart disease. However, tilt testing was used more than would be expected if NICE CG109 had been followed.
This evidence does not affect NICE CG109. However, it highlights a need to clarify in large randomised trials the place of tilt testing in the diagnosis and selection of patients with severe vasovagal syncope for cardiac pacing.
Key reference
- Mitro P, Kirsch P, Valocik G et al. (2011) A prospective study of the standardized diagnostic evaluation of syncope. Europace 13: 566–71. Abstract: www
.europace.oxfordjournals .org/content/early /2011/02/10/europace .eur014.abstract [PubMed: 21317150]
Bundle branch block
A prospective, observational, multi-centre study by Moya et al. (2011) assessed outcomes in patients with syncope and bundle branch block.
A total of 323 patients (left ventricular ejection fraction 56 ± 12%) were evaluated. A 3-phase diagnostic strategy was followed (phase 1: clinical + ECG + echocardiography + also Holter or in-patient ECG monitoring ‘recommended’; phase 2: electrophysiology study; phase 3: IER), providing what was regarded as ‘diagnostic’ evidence in 32%, 35% and 16%, respectively (after exclusion of 24% mainly for deviation from protocol).
Aetiological diagnoses were established in 267 (82.7%) patients. A pacemaker was implanted in 220 (68.1%) patients, an implantable cardioverter defibrillator in 19 (5.8%), and radiofrequency catheter ablation was undertaken in three patients. Twenty patients (6%) died at an average follow-up of 19.2 ± 8.2 months, which was considered by the authors as a low mortality rate.
The study lacked some methodological consistency (for example, sustained VT or rapid supraventricular VT were to be considered diagnostic for the cause of previous syncope even when the documented events were asymptomatic). No comparisons were made with any other possible diagnostic/therapeutic strategies in these patients.
This paper is unlikely to affect NICE CG109, which identifies complete right or left bundle branch block as a ‘red flag’ that should result in clinical assessment, ECG, Holter monitoring and echocardiography in these patients, with subsequent investigation and treatment dictated by specialist cardiovascular assessment in individual patients.
Key reference
- Moya A, Garcia-Civera R, Croci F et al. (2011) Diagnosis, management, and outcomes of patients with syncope and bundle branch block. European Heart Journal 32: 1535–41. Full text: www
.eurheartj.oxfordjournals .org/content /early/2011/03/27/eurheartj .ehr071.full.pdf [PMC free article: PMC3114095] [PubMed: 21444367]
Predicting the cause of syncope from clinical history
Although risk factors and outcome scores to predict prognosis in patients with syncope have been established and correlate with morbidity and mortality in patients, their association with the aetiology of syncope has yet to be determined. This retrospective study by Sud et al. (2009) characterised clinical predictors of primary bradycardia in a cohort of 52 patients undergoing prolonged monitoring for unexplained syncope.
Of 52 patients with recurrent syncope, 20 patients were categorised as having primary arrhythmia and 32 as having non-arrhythmic syncope. Evidence from this study suggested that a history of syncope without prodrome, abnormal ECG and structural heart disease were all predictors of spontaneous primary arrhythmia.
Evidence from this study is limited by the number patients, which the authors noted was insufficient to establish specificity of baseline ECG features for primary arrhythmia, and some variables (for example, family history) were not used as they were not recorded at baseline.
All of the predictors from patients’ clinical history are already covered in NICE CG109 to help decide on the need for cardiovascular assessment. A post-hoc analysis using the OESIL risk score found that (based on a small sample) it independently predicted primary arrhythmia after adjustment for age, baseline ejection fraction, and gender (adjusted OR = 4.63 per one point increase in OESIL score, 95% CI 1.84 to 11.65, p =0.001); this scoring system was discussed during the development of NICE CG109 but may warrant further consideration. Information from this study is unlikely to affect NICE CG109.
Key reference
- Sud S, Klein GJ, Skanes AC et al. (2009) Predicting the cause of syncope from clinical history in patients undergoing prolonged monitoring. Heart Rhythm 6: 238–43. Abstract: www
.heartrhythmjournal .com/article/S1547-5271 %2808%2901071-0/abstract [PubMed: 19187918]
1.4. If the cause of TLoC remains uncertain
Psychological profiling
A Canadian prospective study by D’Antono et al. (2009) was designed to determine the psychological profile of patients with recurrent syncope before and after diagnostic HUT, and whether it can be used to predict recurrence of syncope.
A total of 116 patients (73 women and 43 men; mean age 48 years) referred for HUT were enrolled. Patients’ psychological status (based on the Psychiatric Symptom Index, the Anxiety Sensitivity Index and the Fear of Blood Injury Subscale) and mood or anxiety disorders (based on Primary Care Evaluation of Mental Disorders) were assessed 1 month before and 6 months after HUT; follow-up data were collected for 83 patients.
Clinically meaningful levels of distress were observed in 60% of patients at baseline. However, patients with ‘unexplained syncope’ (negative HUT) had a five-fold greater risk of experiencing depressive or anxiety disorders compared to VVS (positive HUT).
There were no significant changes in distress levels during the 6-month follow-up, however, psychiatric morbidity decreased from 33% to 22% (p = 0.049). Recurrence of syncope was predicted by increased levels of baseline psychological distress (OR = 1.544, p = 0.013).
Overall, this study identified patients with ‘unexplained syncope’ with high risk of psychological morbidity. However, the authors did not specifically comment on this group and the recommendations remained general.
This study had a number of limitations, the first being the small patient sample. In addition, the exclusion criteria, which excluded patients with epilepsy, were not fully explained, and the profile of patients lost to follow-up and any potential significance (for example, whether more ‘unexplained syncope’ than VVS patients) was unclear.
Evidence from this study is unlikely to affect NICE CG109. However, non-epileptic attack disorder accounts for 15–20% of people with a label of ‘epilepsy’, who may overlap with the ‘unexplained syncope’ group described in this study – this group is likely to have a high level of unmet need and are invariably high users of NHS resources.
In addition, evidence from this study also highlights areas for further research (for example, to determine the form of therapy that is most effective in treating psychological morbidity).
Furthermore, data from this study suggest that changes to the treatment pathway to highlight the availability of Increasing Access to Psychological Therapies (IAPT) may be warranted.
Key reference
- D’Antono B, Dupuis G, St-Jean K et al. (2009) Prospective evaluation of psychological distress and psychiatric morbidity in recurrent vasovagal and unexplained syncope. Journal of Psychosomatic Research 67: 213–22. Abstract: www
.sciencedirect.com /science/article/pii/S0022399909000968 [PubMed: 19686877]
1.5. Information for people with TLoC
No new key evidence was found for this section.
1.6. Areas currently not covered by NICE guidance
Genetic aspects of vasovagal syncope
Understanding the aetiology of VVS is of value in determining diagnostic and treatment options. A systematic review of MEDLINE and EMBASE databases by Olde Nordkamp et al. (2009) was designed to provide an overview of the current knowledge of the genetics of VVS.
Nineteen studies (comprising case reports, case-series, case-control studies and cohort studies) of 3552 patients evaluated hereditary aspects of VVS. Across eight studies (1752 patients), a positive family history was observed in 19–90% of the VVS patients; however, this rate of a positive family history is not higher than the cumulative incidence of VVS in the general population (a lifetime cumulative incidence in people up to 65 of 35–39%). Such an incidence among the general population means it is almost inevitable that most individuals will have a family history, although they may not be aware of it. Genetic polymorphisms associated with VVS were assessed in 4 studies (316 patients); only the Gly389 allele was recorded more commonly in VVS patients with a positive HUT test.
The authors found that the quantity and quality of studies in this area was generally poor, and thus no firm conclusions could be drawn. Included studies also had small sample sizes and heterogeneous phenotype definitions, preventing meta-analysis. Although the authors commented on the need for further studies, it is unclear if this is warranted as an impact on clinical practice appears unlikely.
Data from this systematic literature review did not find strong evidence for a genetic basis for vasovagal syncope and has no impact on NICE CG109.
Key reference
- Olde Nordkamp LRA, Wieling W, Zwinderman A H et al. (2009) Genetic aspects of vasovagal syncope: a systematic review of current evidence. Europace 11: 414–20. Full text: www
.europace.oxfordjournals .org/content/11/4/414.full.pdf [PubMed: 19153089]
2. New evidence uncertainties
No new evidence uncertainties were identified during the Evidence Update process, however current uncertainties for transient loss of consciousness can be found at www.library.nhs.uk/duets/ and in the NICE research recommendations database at www.nice.org.uk/research/index.jsp?action=rr
DUETs has been established in the UK to publish uncertainties about the effects of treatment that cannot currently be answered by referring to reliable up-to-date systematic reviews of existing research evidence.
Appendix A. Methodology
Scope
The scope of this Evidence Update is taken from the scope of the reference guidance:
- Transient loss of consciousness. NICE clinical guideline 109 (2010). Available from www.nice.org.uk/guidance/CG109
Searches
The literature was searched to identify studies and reviews relevant to the scope. Searches were conducted of the following databases, covering the dates 02 November 2009 (the end of the search period of the most recent Annual Evidence Update) to 04 October 2011:
- CINAHL
- Cochrane Database of Systematic Reviews
- Embase
- MEDLINE
- PsycINFO
Table 1 provides details of the MEDLINE search strategy used, which was adapted to search the other databases listed above. Given the breadth of the topic, it was necessary to adapt the search strategy used in the reference guidance and the previous Annual Evidence Update. The search strategy was used in conjunction with validated Scottish Intercollegiate Guidelines Network search filters for RCTs, systematic reviews and observational studies (www.sign.ac.uk/methodology/filters.html).
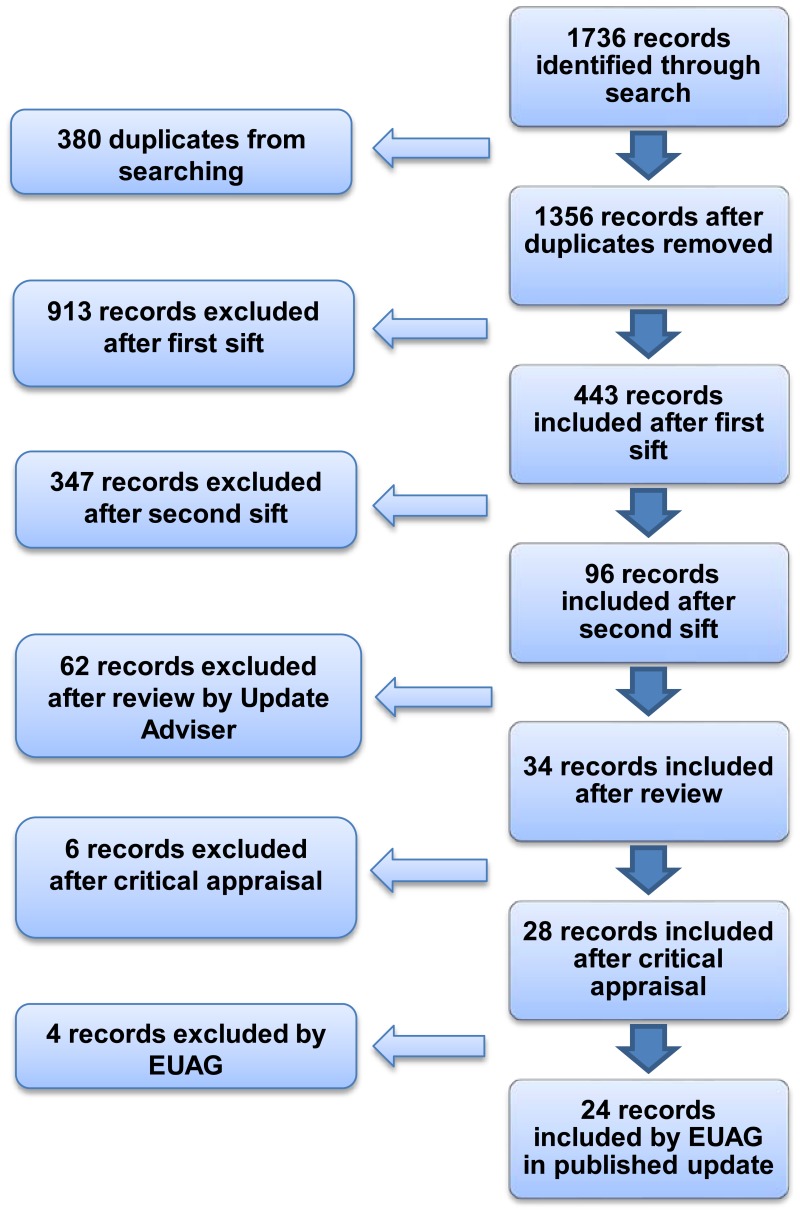
Figure 1 provides details of the evidence selection process. The long list of evidence excluded after review by the Update Adviser (the chair of the EUAG), and the full search strategies, are available on request from ku.shn.ecnedive@sutcatnoc
Table 1MEDLINE search strategy (adapted for individual databases)
| 1 | unconsciousness/ |
| 2 | black?out$.ti,ab. |
| 3 | (pass$ adj out).ti,ab. |
| 4 | (tloc or t-loc).ti,ab. |
| 5 | ((transient or temporary or short or brief or paroxysmal) adj3 (los$ adj2 conscious$)).ti,ab. |
| 6 | or/1-5 |
| 7 | exp syncope/ |
| 8 | pre?syncop$.ti,ab. |
| 9 | syncop$.ti,ab. |
| 10 | or/7-9 |
| 11 | neurally mediated hypotension.mp. |
| 12 | reflex anoxic seizure$.mp. |
| 13 | complex faint$.mp. |
| 14 | ((psychogenic or non?epilep$ or hysteri$ or pseudo or doxogenic) adj (black?out$ or attack$ or seizure$)).mp. |
| 15 | ((hyster$ or pseudo) adj epilep$).mp. |
| 16 | pseudo?seizure$.mp. |
| 17 | hysteroepilep$.mp. |
| 18 | pseudoepilep$.mp. |
| 19 | conversion fit$.mp. |
| 20 | or/11-19 |
| 21 | 6 or 10 or 20 |
Appendix B. The Evidence Update Advisory Group and NHS Evidence project team
Evidence Update Advisory Group
The Evidence Update Advisory Group is a group of subject experts who review the prioritised evidence obtained from the literature search and provide the commentary for the Evidence Update.
- Professor Tom Quinn – ChairProfessor of Clinical Practice, Faculty of Health and Medical Sciences, University of Surrey and Clinical Lead, NHS Evidence
- Dr Robin BealConsultant in Emergency Medicine, St Mary’s Hospital, Newport, Isle of Wight
- Dr Richard GrünewaldConsultant Neurologist, Royal Hallamshire Hospital, Sheffield
- Dr David PitcherConsultant Cardiologist, Worcestershire Royal Hospital
- Ms Alison PottleCardiology Nurse Consultant, Harefield Hospital
- Dr Greg RogersGeneral Practitioner with a Special Interest in Epilepsy for Eastern and Coastal Kent Primary Care Trust
- Mr Garry SwannEmergency Care Nurse Consultant, Heart of England Foundation Trust in Birmingham
- Dr Denise WilliamsConsultant Clinical Geneticist, Birmingham Women’s NHS Foundation Trust and Specialist Adviser, NHS Evidence
NHS Evidence project team
- Alan LovellEvidence Hub Manager
- Elly O’BrienInformation Specialist
- Justina Orleans-LindsayEditor
Footnotes
- 1
NICE-accredited guidance is denoted by the Accreditation Mark

Evidence Updates provide a regular, often annual, summary of selected new evidence published since the literature search was last conducted for the accredited guidance they update. They reduce the need for individuals, managers and commissioners to search for new evidence and inform guidance developers of new evidence in their field. In particular, Evidence Updates highlight any new evidence that might reinforce or generate future change to the practice described in the most recent, accredited guidance, and provide a commentary on the potential impact. Any new evidence that may impact current guidance will be notified to the appropriate NICE guidance development centres. For contextual information, Evidence Updates should be read in conjunction with the relevant clinical guideline, available from (www.nice.org.uk/guidance/CG109). NHS Evidence is a service provided by NICE to improve use of, and access to, evidence-based information about health and social care.
Evidence Updates do not replace current accredited guidance and do not provide formal practice recommendations.
National Institute for Health and Clinical Excellence
Level 1A
City Tower
Piccadilly Plaza
Manchester M1 4BT
- Transient loss of consciousnessTransient loss of consciousness
Your browsing activity is empty.
Activity recording is turned off.
See more...