NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Signs, symptoms and risk factors indicating suitability for transfer to a regional vascular service
Review question
Which signs, symptoms, risk factors (or combinations of these) and prognostic risk assessment tools are most accurate in indicating a patient’s suitability for transfer?
Introduction
People who present at emergency departments with suspected or confirmed ruptured abdominal aortic aneurysm (AAA), or with a symptomatic, unruptured AAA often need urgent specialist care, however this is not always available at all hospitals. This review question aims to determine which signs, symptoms and risk factors are useful in deciding which people are stable enough to survive transfer to a regional vascular service.
PICO
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual. Methods specific to this review question are described in the review protocol in Appendix A.
Declarations of interest were recorded according to NICE’s 2014 conflicts of interest policy.
A single broad search was used to identify all studies that examine the diagnosis, surveillance or monitoring of AAAs. This was a ‘bulk’ search that addressed multiple review questions. The database was sifted to identify all studies that met the criteria detailed in Table 1. The relevant review protocol can be found in Appendix A.
Table 1
Inclusion criteria.
Prospective observational studies that used multivariate analysis to explore factors associated with patient survival during transfer to regional vascular services, were considered for inclusion. No sample size restrictions were made.
Studies were excluded if they:
- were case-controls or cross-sectional studies
- were not in English
- were not full reports of the study (for example, published only as an abstract)
- were not peer-reviewed.
Clinical evidence
Included studies
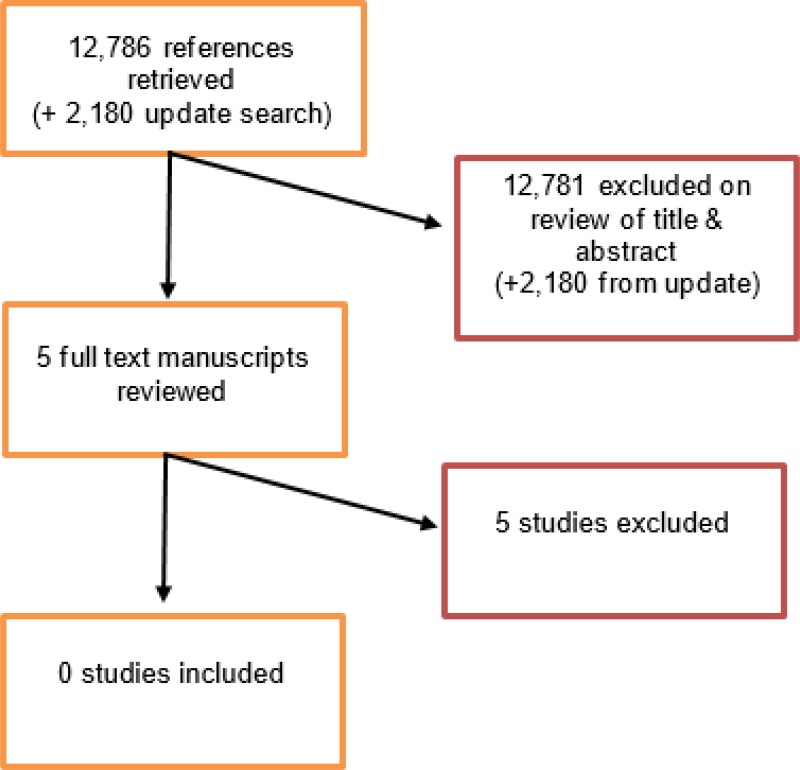
From an initial database of 16,274 abstracts, 5 were identified as being potentially relevant. Following full-text review of these articles, 0 studies were included in this review.
An update search was conducted in December 2017, to identify any relevant studies published during guideline development. The search found 2,180 abstracts; all of which were not considered relevant to this review question. As a result no additional studies were included.
Excluded studies
The list of the papers excluded at full-text review, with reasons, is given in Appendix E.
Summary of clinical studies included in the evidence review
No studies were included following full text review
Quality assessment of clinical studies included in the evidence review
No studies were included following full text review.
Economic evidence
Included studies
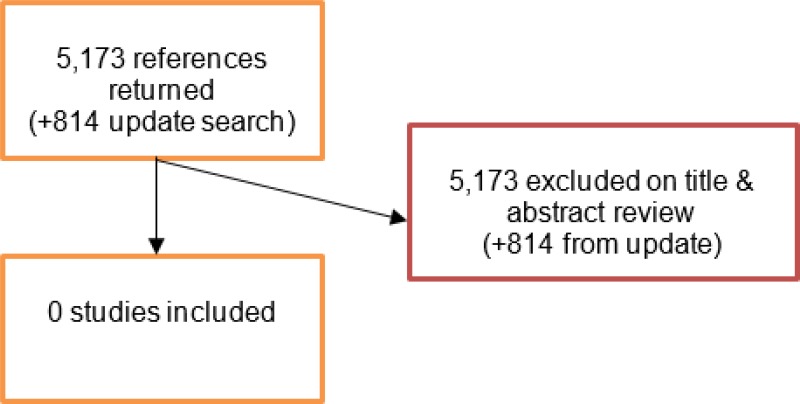
A literature search was conducted jointly for all review questions by applying standard health economic filters to a clinical search for AAA. This search returned a total of 5,173 citations. Following review of all titles and abstracts, 0 studies were identified as being potentially relevant to this review question. No full text manuscripts were retrieved, and 0 studies were included as economic evidence.
An update search was conducted in December 2017, to identify any relevant health economic analyses published during guideline development. The search found 814 abstracts; all of which were not considered relevant to this review question. As a result no additional studies were included.
Excluded studies
No studies were retrieved for full-text review.
Evidence statements
No evidence was identified for this review question.
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
The committee agreed that the outcome that matters most is survival during and following transfer.
The quality of the evidence
The committee noted that, although there is a lack of evidence relating to factors which could be used to determine if a person with a ruptured AAA is likely to survive transfer to a regional vascular service, non-evidence-based guidelines are available across NHS trusts.
Benefits and harms
The committee agreed that their clinical experience could be used to outline important considerations when deciding whether someone should be transferred. It was agreed that an important problem, encountered in practice, is a subgroup of people with ruptured AAA were being transferred to regional vascular services when there was little prospect that they would survive surgery. This population comprises people who have had a cardiac arrest and/or have a persistent loss of consciousness as a result of a ruptured AAA. Evidence relating to these populations can be found the evidence review on risk factors that predict survival after rupture.
The committee were mindful that in some circumstances non-experts may have to decide whether to transfer a person with a suspected or confirmed ruptured AAA, and that their decision could be influenced by misplaced preconceptions about the likelihood of survival. The committee noted that they had previously recommended that all symptomatic or suspected ruptured AAAs should be discussed with a regional vascular service in the evidence review evaluating diagnostic imaging techniques (Evidence review B). With this in mind, it was agreed that specialist input would inform the decision to transfer and operate, precluding any inappropriate decisions being made by non-specialists.
The committee felt that the recommendations on assessing people for transfer are unlikely to incur any patient harm. The recommendations are intended to raise awareness so that appropriate transfer decisions can be made. This, in turn, should reduce patient and family suffering. The committee were mindful that guidance is needed for situations in which the decision has been made not to transfer or operate on a person with a ruptured AAA. They recognised the importance of empathy, effective communication and the need to alleviate pain or discomfort in people during their last moments of life. The committee noted that recommendations have been drafted in the NICE guideline on care of dying adults in the last days of life, and considered it appropriate to cross-refer to this guideline.
Cost effectiveness and resource use
The committee believed that the recommendations could improve resource use and reduce costs associated with inappropriate transfers to regional vascular services.
Other factors the committee took into account
The committee discussed whether it was possible to draft a recommendation about which patient characteristics would prompt paramedics to immediately transfer people with suspected ruptured AAA from the community to a specialist vascular service, bypassing local emergency departments. It was agreed that it would not be possible to specify patient characteristics because some ambulance services may not have prompt access to patient records in community settings. As a result, no recommendations were made.
Appendices
Appendix A. Review protocols
Review protocol for risk factors indicating suitability for transfer to a regional vascular service
| Review question 16 | Which signs, symptoms, risk factors (or combinations of these) and prognostic risk assessment tools are most accurate in indicating a patient’s suitability for transfer? |
|---|---|
| Objectives | To determine which signs, symptoms and risk factors are useful in deciding which people are stable enough to survive transfer to a regional vascular service. |
| Type of review | Prognostic |
| Language | English only |
| Study design | Prospective observational studies using multivariate analysis |
| Status |
Published papers only (full text) No date restrictions |
| Population | People with a suspected or confirmed ruptured or symptomatic unruptured abdominal aortic aneurysm who need to be transferred to a regional vascular service |
| Index test / factors of interest |
Respiratory failure Intubation Cardiac arrest Myocardial ischaemia (on electrocardiogram) Hypoxia Hypotension Altered consciousness Glasgow aneurysm score Hardman index |
| Endpoint |
Arrival at the regional vascular service Cardiac arrest in transit Mortality |
| Other criteria for inclusion / exclusion of studies |
Exclusion: Non-English language Abstract/non-published (i only) |
| Baseline characteristics to be extracted in evidence tables |
Age Sex Size of aneurysm Comorbidities |
| Search strategies | See Appendix B |
| Review strategies |
Double-sifting of randomly selected 20%. Appropriate NICE Methodology Checklists, depending on study designs, will be used as a guide to appraise the quality of individual studies. 20% will be appraised by a second reviewer. Data on all included studies will be extracted into evidence tables. Where statistically possible, a meta-analytic approach will be used to give an overall summary effect. All key findings from evidence will be presented in GRADE profiles and further summarised in evidence statements. |
| Key papers | None identified |
Appendix B. Literature search strategies
Clinical search literature search strategy
Main searches
Bibliographic databases searched for the guideline
- Cumulative Index to Nursing and Allied Health Literature - CINAHL (EBSCO)
- Cochrane Database of Systematic Reviews – CDSR (Wiley)
- Cochrane Central Register of Controlled Trials – CENTRAL (Wiley)
- Database of Abstracts of Reviews of Effects – DARE (Wiley)
- Health Technology Assessment Database – HTA (Wiley)
- EMBASE (Ovid)
- MEDLINE (Ovid)
- MEDLINE Epub Ahead of Print (Ovid)
- MEDLINE In-Process (Ovid)
Identification of evidence for review questions
The searches were conducted between November 2015 and October 2017 for 31 review questions (RQ). In collaboration with Cochrane, the evidence for several review questions was identified by an update of an existing Cochrane review. Review questions in this category are indicated below. Where review questions had a broader scope, supplement searches were undertaken by NICE.
Searches were re-run in December 2017.
Where appropriate, study design filters (either designed in-house or by McMaster) were used to limit the retrieval to, for example, randomised controlled trials. Details of the study design filters used can be found in section 4.
Search strategy review question 16
Medline Strategy, searched 29th September 2016 Database: 1946 to September Week 3 2016 Search Strategy: |
|---|
| 1 Aortic Aneurysm, Abdominal/ |
| 2 Aortic Rupture/ |
| 3 (aneurysm* adj4 (abdom* or thoracoabdom* or thoraco-abdom* or aort* or spontan* or juxtarenal* or juxta-renal* or juxta renal* or paraerenal* or para-renal* or para renal* or suprarenal* or supra renal* or supra-renal* or short neck* or short-neck* or shortneck* or visceral aortic segment*)).tw. |
| 4 or/1–3 |
| 5 prognosis.sh. |
| 6 diagnosed.tw. |
| 7 cohort.mp. |
| 8 predictor:.tw. |
| 9 death.tw. |
| 10 exp models, statistical/ |
| 11 or/5–10 |
| 12 (sensitiv: or predictive value:).mp. or accurac:.tw. |
| 13 11 or 12 |
| 14 “signs and symptoms”/ |
| 15 ((sign or signs) adj5 symptom*).tw. |
| 16 Risk Factors/ |
| 17 factor*.tw. |
| 18 predict*.tw. |
| 19 or/14–18 |
| 20 13 or 19 |
| 21 4 and 20 |
| 22 animals/ not humans/ |
| 23 21 not 22 (12444) |
| 24 limit 23 to english language |
Health Economics literature search strategy
Sources searched to identify economic evaluations
- NHS Economic Evaluation Database – NHS EED (Wiley) last updated Dec 2014
- Health Technology Assessment Database – HTA (Wiley) last updated Oct 2016
- Embase (Ovid)
- MEDLINE (Ovid)
- MEDLINE In-Process (Ovid)
Search filters to retrieve economic evaluations and quality of life papers were appended to the population and intervention terms to identify relevant evidence. Searches were not undertaken for qualitative RQs. For social care topic questions additional terms were added. Searches were re-run in September 2017 where the filters were added to the population terms.
Health economics search strategy
| Medline Strategy |
|---|
| Economic evaluations |
| 1 Economics/ |
| 2 exp “Costs and Cost Analysis”/ |
| 3 Economics, Dental/ |
| 4 exp Economics, Hospital/ |
| 5 exp Economics, Medical/ |
| 6 Economics, Nursing/ |
| 7 Economics, Pharmaceutical/ |
| 8 Budgets/ |
| 9 exp Models, Economic/ |
| 10 Markov Chains/ |
| 11 Monte Carlo Method/ |
| 12 Decision Trees/ |
| 13 econom*.tw. |
| 14 cba.tw. |
| 15 cea.tw. |
| 16 cua.tw. |
| 17 markov*.tw. |
| 18 (monte adj carlo).tw. |
| 19 (decision adj3 (tree* or analys*)).tw. |
| 20 (cost or costs or costing* or costly or costed).tw. |
| 21 (price* or pricing*).tw. |
| 22 budget*.tw. |
| 23 expenditure*.tw. |
| 24 (value adj3 (money or monetary)).tw. |
| 25 (pharmacoeconomic* or (pharmaco adj economic*)).tw. |
| 26 or/1–25 |
| Quality of life |
| 1 “Quality of Life”/ |
| 2 quality of life.tw. |
| 3 “Value of Life”/ |
| 4 Quality-Adjusted Life Years/ |
| 5 quality adjusted life.tw. |
| 6 (qaly* or qald* or qale* or qtime*).tw. |
| 7 disability adjusted life.tw. |
| 8 daly*.tw. |
| 9 Health Status Indicators/ |
| 10 (sf36 or sf 36 or short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).tw. |
| 11 (sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).tw. |
| 12 (sf12 or sf 12 or short form 12 or shortform 12 or sf twelve or sftwelve or shortform twelve or short form twelve).tw. |
| 13 (sf16 or sf 16 or short form 16 or shortform 16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).tw. |
| 14 (sf20 or sf 20 or short form 20 or shortform 20 or sf twenty or sftwenty or shortform twenty or short form twenty).tw. |
| 15 (euroqol or euro qol or eq5d or eq 5d).tw. |
| 16 (qol or hql or hqol or hrqol).tw. |
| 17 (hye or hyes).tw. |
| 18 health* year* equivalent*.tw. |
| 19 utilit*.tw. |
| 20 (hui or hui1 or hui2 or hui3).tw. |
| 21 disutili*.tw. |
| 22 rosser.tw. |
| 23 quality of wellbeing.tw. |
| 24 quality of well-being.tw. |
| 25 qwb.tw. |
| 26 willingness to pay.tw. |
| 27 standard gamble*.tw. |
| 28 time trade off.tw. |
| 29 time tradeoff.tw. |
| 30 tto.tw. |
| 31 or/1–30 |
Appendix E. Excluded studies
Clinical studies
| No. | Study | Reason for exclusion |
|---|---|---|
| 1 | Hinchliffe R J, Ribbons T, Ulug P, and Powell J T (2013) Transfer of patients with ruptured abdominal aortic aneurysm from general hospitals to specialist vascular centres: Results of a Delphi consensus study. Emergency Medicine Journal 30(6), 483–486 [PMC free article: PMC3664393] [PubMed: 22761515] | Wrong study design: study reports the results of a Delphi consensus. Specialists in emergency medicine, vascular and endovascular surgery were asked about patient characteristics and clinical management issues for emergency inter-hospital transfer of people with ruptured AAA. |
| 2 | Ilonzo Nicole, Egorova Natalia N, and Nowygrod Roman (2016) Interhospital transfer for intact abdominal aortic aneurysm repair. Journal of vascular surgery 63(4), 859–65.e2 [PubMed: 26781080] | Wrong study population: study assessed factors associated with inter-hospital transfer of people who had complications following surgical repair of unruptured AAAs. This is out of scope of the review protocol. |
| 3 | Mell Matthew W, Wang Nancy E, Morrison Doug E, and Hernandez-Boussard Tina (2014) Interfacility transfer and mortality for patients with ruptured abdominal aortic aneurysm. Journal of vascular surgery 60(3), 553–7 [PubMed: 24768368] | This retrospective study did not assess factors associated with suitability for transfer. Instead, investigators assessed factors associated with likelihood of transfer by comparing people with ruptured aneurysms who were transferred to other hospitals and those who were not transferred. It is unclear whether the people were transferred to specialist vascular units. Furthermore, the assessed risk factors were focussed on a USA context and were not relevant to those specified in the review protocol: for example, type of healthcare insurance, state (California vs. Florida, or New York), teaching hospital, high-tech hospital. |
| 4 | Mell Matthew W, Schneider Peter A, and Starnes Benjamin W (2015) Variability in transfer criteria for patients with ruptured abdominal aortic aneurysm in the western United States. Journal of vascular surgery 62(2), 326–30 [PubMed: 25937601] | Wrong study design: study involved the use of an online questionnaire to investigate clinician’s opinions on transfer criteria for people with ruptured AAA. |
| 5 | Thompson Andrew R, Rodway Alex, Mitchell Adam, and Hafez Hany (2006) Screening and ultrasound surveillance of large abdominal aortic aneurysms do not improve suitability for endovascular repair. Journal of vascular surgery 43(2), 265–269 [PubMed: 16476598] | Study did not assess factors associated with suitability for transfer. Instead, investigators assessed suitability for EVAR. |
Economic studies
No full text papers were retrieved. All studies were excluded at review of titles and abstracts.
Appendix F. Glossary
- Abdominal Aortic Aneurysm (AAA)
A localised bulge in the abdominal aorta (the major blood vessel that supplies blood to the lower half of the body including the abdomen, pelvis and lower limbs) caused by weakening of the aortic wall. It is defined as an aortic diameter greater than 3 cm or a diameter more than 50% larger than the normal width of a healthy aorta. The clinical relevance of AAA is that the condition may lead to a life threatening rupture of the affected artery. Abdominal aortic aneurysms are generally characterised by their shape, size and cause:
- Infrarenal AAA: an aneurysm located in the lower segment of the abdominal aorta below the kidneys.
- Juxtarenal AAA: a type of infrarenal aneurysm that extends to, and sometimes, includes the lower margin of renal artery origins.
- Suprarenal AAA: an aneurysm involving the aorta below the diaphragm and above the renal arteries involving some or all of the visceral aortic segment and hence the origins of the renal, superior mesenteric, and celiac arteries, it may extend down to the aortic bifurcation.
- Abdominal compartment syndrome
Abdominal compartment syndrome occurs when the pressure within the abdominal cavity increases above 20 mm Hg (intra-abdominal hypertension). In the context of a ruptured AAA this is due to the mass effect of a volume of blood within or behind the abdominal cavity. The increased abdominal pressure reduces blood flow to abdominal organs and impairs pulmonary, cardiovascular, renal, and gastro-intestinal function. This can cause multiple organ dysfunction and eventually lead to death.
- Cardiopulmonary exercise testing
Cardiopulmonary Exercise Testing (CPET, sometimes also called CPX testing) is a non-invasive approach used to assess how the body performs before and during exercise. During CPET, the patient performs exercise on a stationary bicycle while breathing through a mouthpiece. Each breath is measured to assess the performance of the lungs and cardiovascular system. A heart tracing device (Electrocardiogram) will also record the hearts electrical activity before, during and after exercise.
- Device migration
Migration can occur after device implantation when there is any movement or displacement of a stent-graft from its original position relative to the aorta or renal arteries. The risk of migration increases with time and can result in the loss of device fixation. Device migration may not need further treatment but should be monitored as it can lead to complications such as aneurysm rupture or endoleak.
- Endoleak
An endoleak is the persistence of blood flow outside an endovascular stent - graft but within the aneurysm sac in which the graft is placed.
- Type I – Perigraft (at the proximal or distal seal zones): This form of endoleak is caused by blood flowing into the aneurysm because of an incomplete or ineffective seal at either end of an endograft. The blood flow creates pressure within the sac and significantly increases the risk of sac enlargement and rupture. As a result, Type I endoleaks typically require urgent attention.
- Type II – Retrograde or collateral (mesenteric, lumbar, renal accessory): These endoleaks are the most common type of endoleak. They occur when blood bleeds into the sac from small side branches of the aorta. They are generally considered benign because they are usually at low pressure and tend to resolve spontaneously over time without any need for intervention. Treatment of the endoleak is indicated if the aneurysm sac continues to expand.
- Type III – Midgraft (fabric tear, graft dislocation, graft disintegration): These endoleaks occur when blood flows into the aneurysm sac through defects in the endograft (such as graft fractures, misaligned graft joints and holes in the graft fabric). Similarly to Type I endoleak, a Type III endoleak results in systemic blood pressure within the aneurysm sac that increases the risk of rupture. Therefore, Type III endoleaks typically require urgent attention.
- Type IV– Graft porosity: These endoleaks often occur soon after AAA repair and are associated with the porosity of certain graft materials. They are caused by blood flowing through the graft fabric into the aneurysm sac. They do not usually require treatment and tend to resolve within a few days of graft placement.
- Type V – Endotension: A Type V endoleak is a phenomenon in which there is continued sac expansion without radiographic evidence of a leak site. It is a poorly understood abnormality. One theory that it is caused by pulsation of the graft wall, with transmission of the pulse wave through the aneurysm sac to the native aneurysm wall. Alternatively it may be due to intermittent leaks which are not apparent at imaging. It can be difficult to identify and treat any cause.
- Endovascular aneurysm repair
Endovascular aneurysm repair (EVAR) is a technique that involves placing a stent –graft prosthesis within an aneurysm. The stent-graft is inserted through a small incision in the femoral artery in the groin, then delivered to the site of the aneurysm using catheters and guidewires and placed in position under X-ray guidance.
- Conventional EVAR refers to placement of an endovascular stent graft in an AAA where the anatomy of the aneurysm is such that the ‘instructions for use’ of that particular device are adhered to. Instructions for use define tolerances for AAA anatomy that the device manufacturer considers appropriate for that device. Common limitations on AAA anatomy are infrarenal neck length (usually >10mm), diameter (usually ≤30mm) and neck angle relative to the main body of the AAA
- Complex EVAR refers to a number of endovascular strategies that have been developed to address the challenges of aortic proximal neck fixation associated with complicated aneurysm anatomies like those seen in juxtarenal and suprarenal AAAs. These strategies include using conventional infrarenal aortic stent grafts outside their ‘instructions for use’, using physician-modified endografts, utilisation of customised fenestrated endografts, and employing snorkel or chimney approaches with parallel covered stents.
- Goal directed therapy
Goal directed therapy refers to a method of fluid administration that relies on minimally invasive cardiac output monitoring to tailor fluid administration to a maximal cardiac output or other reliable markers of cardiac function such as stroke volume variation or pulse pressure variation.
- Post processing technique
For the purpose of this review, a post-processing technique refers to a software package that is used to augment imaging obtained from CT scans, (which are conventionally presented as axial images), to provide additional 2- or 3-dimensional imaging and data relating to an aneurysm’s, size, position and anatomy.
- Permissive hypotension
Permissive hypotension (also known as hypotensive resuscitation and restrictive volume resuscitation) is a method of fluid administration commonly used in people with haemorrhage after trauma. The basic principle of the technique is to maintain haemostasis (the stopping of blood flow) by keeping a person’s blood pressure within a lower than normal range. In theory, a lower blood pressure means that blood loss will be slower, and more easily controlled by the pressure of internal self-tamponade and clot formation.
- Remote ischemic preconditioning
Remote ischemic preconditioning is a procedure that aims to reduce damage (ischaemic injury) that may occur from a restriction in the blood supply to tissues during surgery. The technique aims to trigger the body’s natural protective functions. It is sometimes performed before surgery and involves repeated, temporary cessation of blood flow to a limb to create ischemia (lack of oxygen and glucose) in the tissue. In theory, this “conditioning” activates physiological pathways that render the heart muscle resistant to subsequent prolonged periods of ischaemia.
- Tranexamic acid
Tranexamic acid is an antifibrinolytic agent (medication that promotes blood clotting) that can be used to prevent, stop or reduce unwanted bleeding. It is often used to reduce the need for blood transfusion in adults having surgery, in trauma and in massive obstetric haemorrhage.
Final
Methods, evidence and recommendations
This evidence review was developed by the NICE Guideline Updates Team
Disclaimer: The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. All NICE guidance is subject to regular review and may be updated or withdrawn.
- The importance of timing in surgical treatment of unruptured symptomatic aneurysm of abdominal aorta.[Bratisl Lek Listy. 2012]The importance of timing in surgical treatment of unruptured symptomatic aneurysm of abdominal aorta.Pasternak J, Nikolic D, Popovic V, Vucaj-Cirilovic V. Bratisl Lek Listy. 2012; 113(11):652-6.
- Glasgow aneurysm score predicts the outcome after emergency open repair of symptomatic, unruptured abdominal aortic aneurysms.[Eur J Vasc Endovasc Surg. 2007]Glasgow aneurysm score predicts the outcome after emergency open repair of symptomatic, unruptured abdominal aortic aneurysms.Antonello M, Lepidi S, Kechagias A, Frigatti P, Tripepi A, Biancari F, Deriu GP, Grego F. Eur J Vasc Endovasc Surg. 2007 Mar; 33(3):272-6. Epub 2006 Nov 9.
- Establishing a protocol for endovascular treatment of ruptured abdominal aortic aneurysms: outcomes of a prospective analysis.[J Vasc Surg. 2006]Establishing a protocol for endovascular treatment of ruptured abdominal aortic aneurysms: outcomes of a prospective analysis.Mehta M, Taggert J, Darling RC 3rd, Chang BB, Kreienberg PB, Paty PS, Roddy SP, Sternbach Y, Ozsvath KJ, Shah DM. J Vasc Surg. 2006 Jul; 44(1):1-8; discussion 8.
- Review Signs, symptoms and risk factors predicting ruptured or symptomatic unruptured aneurysms before arrival at the hospital, and in non-specialist hospital settings: Abdominal aortic aneurysm: diagnosis and management: Evidence review N[ 2020]Review Signs, symptoms and risk factors predicting ruptured or symptomatic unruptured aneurysms before arrival at the hospital, and in non-specialist hospital settings: Abdominal aortic aneurysm: diagnosis and management: Evidence review N. 2020 Mar
- Review Outcome after emergency repair of symptomatic, unruptured abdominal aortic aneurysm: results in 42 patients and review of the literature.[Scand Cardiovasc J. 2005]Review Outcome after emergency repair of symptomatic, unruptured abdominal aortic aneurysm: results in 42 patients and review of the literature.Leo E, Biancari F, Kechagias A, Ylönen K, Rainio P, Romsi P, Juvonen T. Scand Cardiovasc J. 2005 Apr; 39(1-2):91-5.
- Signs, symptoms and risk factors indicating suitability for transfer to a region...Signs, symptoms and risk factors indicating suitability for transfer to a regional vascular service
Your browsing activity is empty.
Activity recording is turned off.
See more...