NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Hearing loss in adults: assessment and management. London: National Institute for Health and Care Excellence (NICE); 2018 Jun. (NICE Guideline, No. 98.)
National Institute for Health and Care Excellence
Guideline scope
Hearing loss (adult presentation): assessment and management
Topic
The Department of Health in England has asked NICE to produce a guideline on the assessment and management of hearing loss (adult presentation).
This guideline will also be used to develop the NICE quality standard for hearing loss (adult presentation).
The guideline will be developed using the methods and processes outlined in Developing NICE guidelines: the manual.
For more information about why this guideline is being developed, and how the guideline will fit into current practice, see the context section.
Who the guideline is for
- People using services, families and carers and the public
- Healthcare professionals in all settings where NHS care is commissioned or provided
- Social care professionals
- Commissioners of health and social care services.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government. Scottish Government, and Northern Ireland Executive.
Equality considerations
NICE has carried out an equality impact assessment during scoping. The assessment:
- lists equality issues identified, and how they have been addressed
- explains why any groups are excluded from the scope.
The guideline will look at inequalities relating to disability.
1. What the guideline is about
1.1. Who is the focus?
Groups that will be covered
- Adults (aged 18 years and older) with hearing loss, including those with onset before the age of 18 but presenting in adulthood.
- Special consideration will be given to:
- –
young adults (aged 18–25)
- –
people with single-sided deafness
- –
people with speech and language difficulties.
Groups that will not be covered
- Adults who presented with hearing loss before the age of 18.
1.2. Settings
Settings that will be covered
- All settings where NHS care is commissioned or provided.
1.3. Activities, services or aspects of care
We will look at evidence on the areas listed below when developing the guideline, but it may not be possible to make recommendations on all the areas.
Key areas that will be covered
- Initial assessment (first presentation) and triage.
- Further assessment.
- Management of hearing difficulties.
Areas that will not be covered
- Tinnitus (without hearing loss).
- Vertigo (without hearing loss).
- Acute temporary hearing loss caused by traumatic head injuries, for example perforated tympanic membranes or middle ear effusions.
- Management of disease processes underlying hearing loss.
- Surgical management of hearing loss.
- Screening programmes for hearing loss.
1.4. Economic aspects
We will take economic aspects into account when making recommendations. We will develop an economic plan that states for each review question (or key area in the scope) whether economic considerations are relevant, and if so whether this is an area that should be prioritised for economic modelling and analysis. We will review the economic evidence and carry out economic analyses, using an NHS and personal social services (PSS) perspective, as appropriate.
1.5. Key issues and questions
While writing this scope, we have identified the following key issues, and key questions related to them:
- Initial assessment (first presentation) and triage
- 1.1.
In whom should hearing loss be suspected? For example, people with dementia, mild cognitive impairment and learning difficulties.
- 1.2.
What are the signs and symptoms that allow early recognition of hearing loss needing urgent referral to a specialist?
- 1.3.
Which causes of hearing difficulty can be identified and treated in primary care?
- 1.4.
Who should be referred to audiovestibular medicine or ear, nose and throat (ENT) surgery for medical assessment?
- 1.5.
Which causes of hearing difficulty can be identified and treated by audiology services?
- Further assessment
- 2.1.
How should hearing and communication needs be assessed? For example, history, examination, pure tone audiometry, tympanometry, speech and hearing in noise tests, needs and goal-setting (individual management plans).
- 2.2.
Which tests and investigations should be used in secondary medical services to assess the underlying cause of hearing loss?
- 2.3.
Which tests and investigations should be used in secondary medical services to determine the cause of sudden-onset sensorineural hearing loss?
- Management of hearing difficulties
- 3.1.
How should earwax be treated?
- 3.2.
What tools (for example, patient-centred decision aids) help people with hearing difficulty choose between different management strategies, including (combinations of): hearing tactics, lip reading, hearing aids, assistive listening devices, communication training, counselling?
- 3.3.
What are the information, support and advice needs of people with hearing difficulty and their families and carers?
- 3.4.
What is the clinical and cost effectiveness of 1 hearing aid (for 1 ear) compared with 2 (for 2 ears)?
- 3.5.
What is the most clinically and cost effective treatment for idiopathic sudden-onset sensorineural hearing loss?
- 3.6.
How and when should people with hearing-related communication needs (including those with hearing aids) be monitored and followed up?
- 3.7.
What is the clinical and cost effectiveness of different types of hearing aid microphones and digital noise reduction technologies?
- 3.8.
What is the clinical and cost effectiveness of assistive listening devices (such as loops to support use of audiovisual devices)?
- 3.9.
What is the clinical and cost effectiveness of aftercare to support continuing use of devices?
The key questions may be used to develop more detailed review questions, which guide the systematic review of the literature.
1.6. Main outcomes
The main outcomes that will be considered when searching for and assessing the evidence are:
- Health-related quality of life.
- Positive predictive value of signs and symptoms.
- Diagnostic accuracy of tests.
- Adverse events.
- Use of hearing aids.
- Validated hearing-specific self-report benefit measures.
2. Links with other NICE guidance, NICE quality standards, and NICE Pathways
2.1. NICE guidance
NICE guidance about the experience of people using NHS services
NICE has produced the following guidance on the experience of people using the NHS. This guideline will not include additional recommendations on these topics unless there are specific issues related to hearing loss:
- Patient experience in adult NHS services (2012) NICE guideline CG138
- Service user experience in adult mental health (2011) NICE guideline CG136
- Medicines adherence (2009) NICE guideline CG76
NICE guidance in development that is closely related to this guideline
NICE is currently developing the following guidance that is closely related to this guideline:
- Diagnostic services NICE guideline. Publication expected November 2017.
2.2. NICE quality standards
NICE quality standards that may use this guideline as an evidence source when they are being developed
- Hearing loss NICE quality standard. Publication date to be confirmed
2.3. NICE Pathways
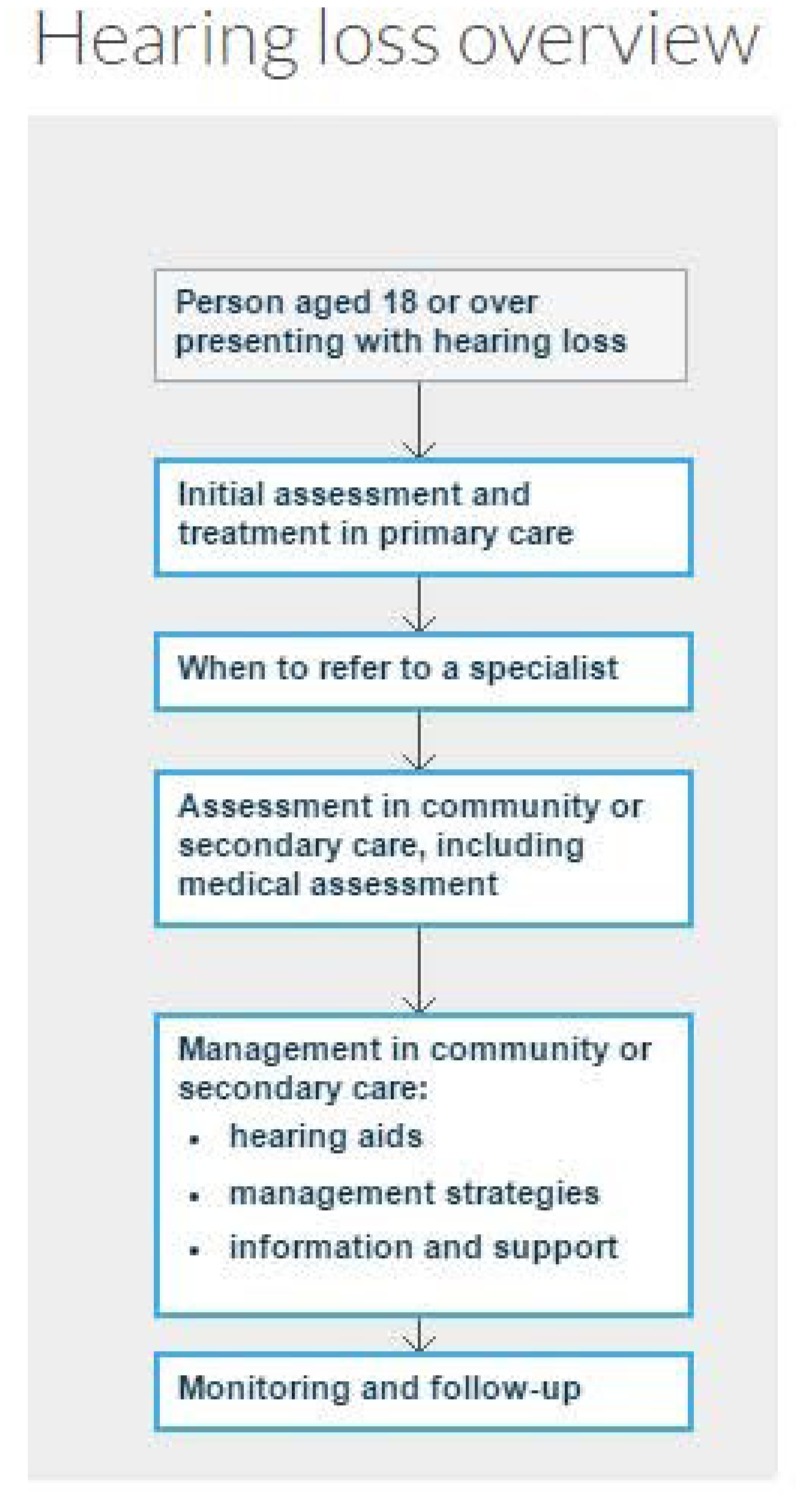
NICE Pathways bring together all NICE guidance and associated products on a topic in an interactive flow chart.
When this guideline is published, the recommendations will be incorporated into a new pathway on hearing loss. Other relevant guidance will also be added to the pathway, including:
Cochlear implants for children and adults with severe to profound deafness (2009) NICE technology appraisal guidance TA166
Auditory brain stem implants (2005) NICE interventional procedure IPG108
An outline of the new pathway, based on the scope, is included below. It will be adapted and more detail added as the recommendations are written during guideline development.
3 Context
3.1. Key facts and figures
Hearing loss is a major health issue that affects over 11 million people in the UK. It is estimated that, by 2035, there will be more than 15.6 million people with hearing loss in the UK - a fifth of the population. According to the World Health Organization (WHO), by 2030 hearing loss will be in the top 10 disease burdens in the UK, above diabetes and cataracts.
It is estimated that, in 2013, the UK economy lost more than £24.8 billion in potential output because of high unemployment rates among people with hearing loss. The cost may be higher if rates of underemployment are also taken into account. These high rates of unemployment and underemployment reflect the communication and participation difficulties experienced by people with hearing loss.
Research shows that hearing loss doubles the risk of developing depression and increases the risk of anxiety and other mental health issues. Research also suggests that use of hearing aids reduces these risks. There is also evidence that people with hearing loss have a higher risk of dementia: this risk is 3 times higher in moderate hearing loss and 5 times higher in severe hearing loss.
One study found that on average there is a 10-year delay in people aged 55–74 seeking help for their hearing loss, and 45% of people who do report hearing loss to their GP are not referred to NHS hearing services.
In 2015, the Department of Health and NHS England developed the Action plan on hearing loss to produce and enforce national commissioning guidance, aiming to ensure that consistent, high-quality services are available, and to intervene if services do not improve.
3.2. Current practice
The investigation and management pathways for people with hearing loss vary, and many people face delays in treatment and inappropriate management. This is a particular issue in relation to sudden-onset sensorineural hearing loss, which needs urgent treatment.
The main referral pathway for an adult with hearing loss who meets the national ‘direct referral’ criteria set out by the British Academy of Audiology and the British Society of Hearing Aid Audiologists is direct from GP to audiology services. For those who do not meet these criteria, referral is directly to ENT or audiovestibular medicine.
Difficulties in hearing can arise from simple problems, such as occlusive earwax which can be treated in primary care, through to potentially life-threatening conditions, such as autoimmune disease which needs specialist medical care. Currently in primary care, the identification of treatable causes of hearing loss such as occlusive earwax and infections is not robust, leading to some people waiting a long time to see a specialist when they could have been treated successfully in primary care.
Assessment includes taking a history, pure tone audiometry and tympanometry. It may also include clinic-based assessment of ability to understand speech in a noisy environment, and self-report measures related to disability and participation limitations.
Audiology services are provided in a number of NHS settings. In some parts of England this is through the AQP)scheme, which means people have a choice of service providers ranging from traditional audiology services to independent high street providers.
Management pathways vary locally once hearing loss is identified. In general, if hearing aids are recommended, people are offered 1 for each ear unless there are reasons that this is inappropriate. However, in some areas people are not offered NHS hearing aids when they might conceivably benefit, while others are offered 1 hearing aid when they need 2, or given 2 when they have difficulty maintaining the use of 1. Some people are given hearing aids when strategies to improve hearing and listening would be more useful. In some cases hearing aids are tried but discontinued because the person has not had the support they need to use them.
These variations in assessment and management pathways for hearing loss can have a major impact, adversely affecting people’s prognosis, and contributing to the overall financial burden of hearing loss. Identifying the correct routes of referral and optimal management pathway for people with hearing loss is therefore very important.
3.3. Policy, legislation, regulation and commissioning
Policy
Any qualified provider (AQP) scheme Some routine and non-complex audiological care is provided by the private and independent sector in England under the ‘any qualified provider’ scheme, whereby any service can offer hearing testing and provide hearing aids if the provider meets the criteria.
Providers now include high street chains as well as local audiology departments. The guideline will be relevant to all providers of adult hearing services in England.
Legislation, regulation and guidance
Action plan on hearing loss NHS England and Department of Health, 2015
Commissioning Framework on Hearing Services, NHS England, publication expected in May 2016.
4. Further information
This is the final scope, incorporating comments from registered stakeholders during consultation.
The guideline is expected to be published in May 2018.
You can follow progress of the guideline.
Our website has information about how NICE guidelines are developed.
- Scope - Hearing loss in adultsScope - Hearing loss in adults
- Adusta subvirdis subviridis isolate BJLinnSoc_233 16S large subunit ribosomal RN...Adusta subvirdis subviridis isolate BJLinnSoc_233 16S large subunit ribosomal RNA gene, partial sequence; mitochondrial gene for mitochondrial productgi|28882717|gb|AY161612.1|Nucleotide
- Adusta onyx isolate BJLinnSoc_229 16S large subunit ribosomal RNA gene, partial ...Adusta onyx isolate BJLinnSoc_229 16S large subunit ribosomal RNA gene, partial sequence; mitochondrial gene for mitochondrial productgi|28882713|gb|AY161608.1|Nucleotide
Your browsing activity is empty.
Activity recording is turned off.
See more...