| DESIGNS & POPULATIONS | Study Design | Phase III, multi-centre, multi-national, open-label, extension | Phase IIIb, international multi-centre, open-label, uncontrolled study |
|---|
| Locations | 10 sites in the US, France, Netherlands | US, Belgium, France, Italy, Netherlands, UK |
|---|
| Number of Participants (N) | 60 | 41 |
|---|
| Inclusion Criteria | Pts previously participating in RP103-03 and willing to continue with treatment
OR
Pts with:
confirmed diagnosis of nephropathic cystinosis; stable on a Cystagon dose at least 21 days prior to screening; no significant changes in liver function tests and renal function 6 mos before screening; eGFR > 30 mL/min/1.73m2; female pts of childbearing potential who agree to use contraception.
|
Confirmed diagnosis of nephropathic cystinosis On a stable dose of Cystagon at least 21 days prior to screening WBC cystine level > 1 nmol half cystine/mg protein over at least 2 measurements in the 2 yrs prior to screening eGFR > 20 mL/min/1.73m2 and no significant change in renal function within 6 mos before screening
|
|---|
| Exclusion Criteria | Pts enrolled in RP103-03 who did not complete last scheduled study visit or did not wish to continue treatment with RP103
OR, for pts who did not complete RP103-03:
Pts less than 1 year old. Pts with known history currently of the following conditions or other health issues that, in the opinion of the investigator, make it unsafe for participation:
inflammatory bowel disease (if currently active) or prior resection of small intestine; heart disease (i.e., myocardial infarction, heart failure, unstable arrhythmias, or poorly controlled hypertension) 90 days prior to screening; active bleeding disorder 90 days prior to screening; malignant disease within last 2 yrs.
Pts with hemoglobin level < 10 g/dL at screening or a level that, in the opinion of the investigator, makes it unsafe for participation. Pts with known hypersensitivity to cysteamine or penicillamine. Female pts who are nursing, planning a pregnancy, known or suspected to be pregnant, or have a positive serum pregnancy test. Pts who, in the opinion of the investigator, are unable or unwilling to comply with the protocol.
| Pts < 12 yrs of age.
Pts with current history of any of the following conditions:
inflammatory bowel disease, or prior resection of the small intestine; heart disease (i.e., myocardial infarction, heart failure, unstable arrhythmias, or poorly controlled hypertension) within 90 days prior to screening; active bleeding disorder within 90 days prior to screening; history of malignant disease within 2 yrs prior to screening.
|
|---|
| Objective | To evaluate long-term efficacy, safety, and PK of delayed-release cysteamine bitartrate (after 9-wk initial study, RP103-03) | Primary: Compare initial Cystagon phase and subsequent RP103 phase in pts to evaluate control of WBC cystine levels over 24 hours.
Secondary: Assess long-term safety and tolerability of RP103 in pts with cystinosis. |
|---|
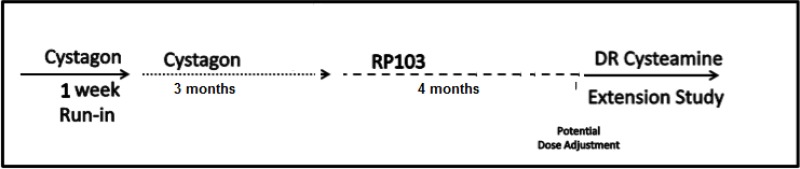
| EXPOSURE | Intervention | Long-term treatment of RP103 q.12.h. starting at a total daily dose of 70% of participants’ total daily Cystagon dose, with opportunity for quarterly dose adjustments. | RP103 q.12.h. from mos 3.5, 4, 5, 6, and 7, starting at a total daily dose of 70% of participants’ total daily
Cystagon dose with no dose adjustments Long-term treatment: RP103 q.12.h. with opportunity for quarterly dose adjustments |
|---|
| Phase | III | IIIb |
|---|
| Extension Period | 9 wks + 1 dose up to a minimum of 6 mos (median exposure 3.0 yrs, range of 35 to 1,677 days) | Mos 8 to 48, or study termination |
|---|
| Follow-up | 6 mos after study completion | 7 ± 2 days after last study dose or decision to terminate |
|---|
| OUTCOMES | Main End Point(s) | Mean WBC cystine content
Dose of RP103 | WBC cystine over time
Dosing and exposure of RP103 |
|---|
| Other End Points | Kidney function, somatic growth, BMI, patient QoL (as assessed by PedsQL 4.0)
Harms | Adverse events |
|---|
| NOTES | Publications | Clinical study report (RP103-04)35 | Preliminary report57 |
|---|