All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob). Requests for permission to reproduce or translate WHO publications – whether for sale or for non-commercial distribution – should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index.html).
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Pocket Book of Hospital Care for Children: Guidelines for the Management of Common Childhood Illnesses. 2nd edition. Geneva: World Health Organization; 2013.
Pocket Book of Hospital Care for Children: Guidelines for the Management of Common Childhood Illnesses. 2nd edition.
Show details7.1. Severe acute malnutrition
Severe acute malnutrition is defined in these guidelines as the presence of oedema of both feet or severe wasting (weight-for-height/length <-3SD or mid-upper arm circumference < 115 mm). No distinction is made between the clinical conditions of kwashiorkor or severe wasting because their treatment is similar.
Children who are <-3SD weight-for-age may be stunted (short stature) but not severely wasted. Stunted children who are not severely wasted do not require hospital admission unless they have a serious illness.
Diagnosis
The main diagnostic features are:
- weight-for-length/height < -3SD (wasted) or
- mid-upper arm circumference < 115 mm or
- oedema of both feet (kwashiorkor with or without severe wasting).
Children with severe acute malnutrition should first be assessed with a full clinical examination to confirm whether they have any general danger sign, medical complications and an appetite.
Children with severe acute malnutrition with loss of appetite or any medical complication have complicated severe acute malnutrition and should be admitted for inpatient care. Children who have a good appetite and no medical complications can be managed as outpatients.
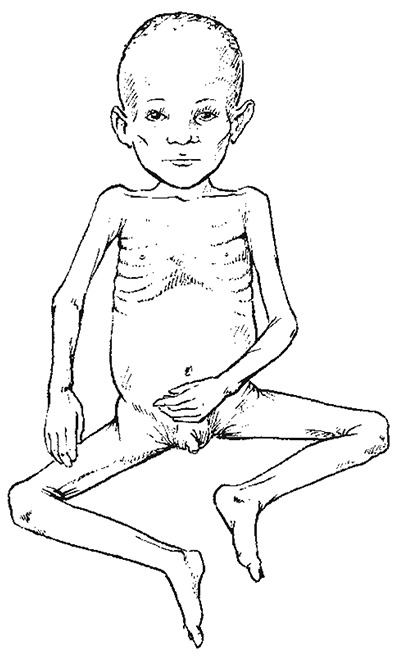
Child with marasmus
7.2. Initial assessment
Assess for general danger signs or emergency signs and take a history concerning:
- recent intake of food and fluids
- usual diet before the current illness
- breastfeeding
- duration and frequency of diarrhoea and vomiting
- type of diarrhoea (watery/bloody)
- loss of appetite
- family circumstances
- cough > 2 weeks
- contact with TB
- recent contact with measles
- known or suspected HIV infection/exposure.

Child with severe acute malnutrition oedema
On examination, look for:
- shock: lethargic or unconscious; with cold hands, slow capillary refill (> 3 s), or weak (low volume), rapid pulse and low blood pressure
- signs of dehydration
- severe palmar pallor
- bilateral pitting oedema
- eye signs of vitamin A deficiency:
- –
dry conjunctiva or cornea, Bitot spots
- –
corneal ulceration
- –
keratomalacia
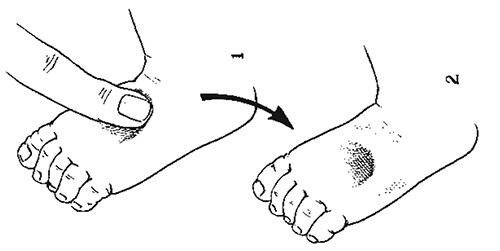
Pitting oedema on dorsum of foot
When pressure is applied for a few seconds, a pit remains after the finger is removed.
Children with vitamin A deficiency are likely to be photophobic and will keep their eyes closed. It is important to examine the eyes very gently to prevent corneal rupture.
- localizing signs of infection, including ear and throat infections, skin infection or pneumonia
- signs of HIV infection (see Chapter 8)
- fever (temperature ≥ 37.5 °C or ≥ 99.5 °F) or hypothermia (rectal temperature < 35.5 °C or < 95.9 °F)
- mouth ulcers
- skin changes of kwashiorkor:
- –
hypo- or hyperpigmentation
- –
desquamation
- –
ulceration (spreading over limbs, thighs, genitalia, groin and behind the ears)
- –
exudative lesions (resembling severe burns) often with secondary infection (including Candida).
- Conduct an appetite test:
- –
Check if the child has appetite by providing ready-to-use therapeutic food.
Laboratory investigations should be conducted for Hb or EVF, especially if there is severe palmar pallor.
7.3. Organization of care
Children who have an appetite (pass the appetite test) and are clinically well and alert should be treated as outpatients for uncomplicated severe acute malnutrition. Children who have severe oedema +++ or a poor appetite (fail the appetite test) or present with one or more general danger signs or medical conditions requiring admission should be treated as inpatients.
- ►
On admission, a child with complicated severe acute malnutrition should be separated from infectious children and kept in a warm area (25–30 °C, with no draughts) or in a special nutrition unit if available, and constantly monitored.
Facilities and sufficient staff should be available to ensure correct preparation of appropriate therapeutic foods and to feed the child regularly, day and night. Accurate weighing machines or MUAC tapes are needed, and records of the feeds given and the child's weight or anthropometric measurements should be kept so that progress can be monitored.
7.4. General management
Plan for inpatient care
For triage assessment of children with severe acute malnutrition and management of shock, see Chapter 1. When there is corneal ulceration, give vitamin A, instil chloramphenicol or tetracycline and atropine drops into the eye, cover with a saline-soaked eye pad, and bandage (see section 7.5.1). Severe anaemia, if present, will require urgent treatment (see section 7.5.2).
General treatment involves 10 steps in two phases: initial stabilization and rehabilitation (see Table 21).
Table 21Time frame for the management of a child with complicated severe acute malnutrition
| Stabilization | Rehabilitation | ||
|---|---|---|---|
| Days 1–2 | Days 3–7 | Weeks 2–6 | |
| 1. Hypoglycaemia |
 | ||
| 2. Hypothermia |
 | ||
| 3. Dehydration |
 | ||
| 4. Electrolytes |
 | ||
| 5. Infection |
 | ||
| 6. Micronutrients |
 |
 | |
| 7. Initiate feeding |
 | ||
| 8. Catch-up feeding |
 | ||
| 9. Sensory stimulation |
 | ||
| 10. Prepare for follow-up |
 | ||
7.4.1. Hypoglycaemia
All severely malnourished children are at risk of hypoglycaemia and, immediately on admission, should be given a feed or 10% glucose or sucrose (see below). Frequent 2 h feeding is important.
Diagnosis
If there is any suspicion of hypoglycaemia and when blood glucose can be measured quickly (e.g. with Dextrostix®), this should be done immediately. Hypoglycaemia is present when the blood glucose is < 3 mmol/litre (< 54 mg/dl). If blood glucose cannot be measured, it should be assumed that all children with severe acute malnutrition are hypoglycaemic and given treatment.
Treatment
- ►
Give 50 ml of 10% glucose or sucrose solution (one rounded teaspoon of sugar in three tablespoons of water) orally or by nasogastric tube, followed by the first feed as soon as possible.
- ►
Give the first feed of F-75 therapeutic milk, if it is quickly available, and then continue with feeds every 2 h for 24 h; then continue feeds every 2 or 3 h, day and night.
- ►
If the child is unconscious, treat with IV 10% glucose at 5 ml/kg or, if IV access cannot be quickly established, then give 10% glucose or sucrose solution by nasogastric tube. If IV glucose is not available, give one teaspoon of sugar moistened with one or two drops of water sublingually, and repeat every 20 min to prevent relapse. Children should be monitored for early swallowing, which leads to delayed absorption; in this case another dose of sugar should be given. Continue with 2 h oral or nasogastric feeds to prevent recurrence.
- ►
Start on appropriate IV or IM antibiotics.
Monitoring
If the initial blood glucose was low, repeat the measurement (using finger or heel prick blood and measure with the Dextrostix®, when available) after 30 min.
- If blood glucose falls to < 3 mmol/litre (< 54 mg/dl), repeat the 10% glucose or oral sugar solution.
- If the rectal temperature falls to < 35.5 °C, or if the level of consciousness deteriorates, repeat the Dextrostix® measurement and treat accordingly.
Prevention
- ►
Feed every 2 h, starting immediately (see initial refeeding) or, when dehydrated, rehydrate first. Continue feeding throughout the night.
- ►
Encourage mothers to watch for any deterioration, help feed and keep the child warm.
- ►
Check on abdominal distension.
7.4.2. Hypothermia
Hypothermia is very common in malnourished children and often indicates coexisting hypoglycaemia or serious infection.
Diagnosis
- If the axillary temperature is < 35 °C (< 95°F) or does not register on a normal thermometer, assume hypothermia. When a low-reading thermometer is available, take the rectal temperature (< 35.5 °C or < 95.9 °F) to confirm hypothermia.
Treatment
All children with hypothermia should be treated routinely for hypoglycaemia and infection.
- ►
Feed the child immediately and then every 2 h unless they have abdominal distension; if dehydrated, rehydrate first.
- ►
Re-warm the child: Make sure the child is clothed (especially the head); cover with a warmed blanket and place a heater (not pointing directly at the child) or lamp nearby, or put the child on the mother's bare chest or abdomen (skin-to-skin) and cover them with a warmed blanket and/or warm clothing.
- ►
Keep the child away from draughts.
- ►
Give appropriate IV or IM antibiotics.
Monitoring
- Take the child's rectal temperature every 2 h until it rises to > 36.5 °C. Take it every 30 min if a heater is being used.
- Ensure that the child is covered at all times, especially at night. Keep the head covered, preferably with a warm bonnet, to reduce heat loss.
- Check for hypoglycaemia whenever hypothermia is found.
Prevention
- ►
Feed immediately and then every 2–3 h, day and night.
- ►
Place the bed in a warm, draught-free part of the ward, and keep the child covered.
- ►
Use the Kangaroo technique for infants, cover with a blanket and let the mother sleep with child to keep the child warm.
- ►
Avoid exposing the child to cold (e.g. after bathing or during medical examinations).
- ►
Change wet nappies, clothes and bedding to keep the child and the bed dry. Dry carefully after bathing, but do not bathe if very ill.
- ►
Use a heater or incandescent lamp with caution.
- ►
Do not use a hot water bottle or fluorescent lamp.
7.4.3. Dehydration
Diagnosis
Dehydration tends to be overdiagnosed and its severity overestimated in children with severe acute malnutrition because it is difficult to determine dehydration accurately from clinical signs alone. Assume that all children with watery diarrhoea or reduced urine output have some dehydration. It is important to note that poor circulatory volume or perfusion can co-exist with oedema.
Treatment
Do not use the IV route for rehydration, except in cases of shock. Rehydrate slowly, either orally or by nasogastric tube, using oral rehydration solution for malnourished children (5–10ml/kg per h up to a maximum of 12 hours). The standard WHO ORS solution for general use has a high sodium and low potassium content, which is not suitable for severely malnourished children. Instead, give special rehydration solution for malnutrition, ReSoMal.
- ►
Give the ReSoMal rehydration fluid orally or by nasogastric tube, more slowly than you would when rehydrating a well-nourished child:
- –
Give 5 ml/kg every 30 min for the first 2 h.
- –
Then give 5–10 ml/kg per h for the next 4–10 h on alternate hours, with F-75 formula. The exact amount depends on how much the child wants, the volume of stool loss and whether the child is vomiting.
- ►
If not available then give half strength standard WHO oral rehydration solution with added potassium and glucose as per the ReSoMal recipe below, unless the child has cholera or profuse watery diarrhoea.
- ►
If rehydration is still required at 10 h, give starter F-75 (see recipes) instead of ReSoMal, at the same times. Use the same volume of starter F-75 as of ReSoMal.
- ►
If in shock or severe dehydration but cannot be rehydrated orally or by nasogastric tube, give IV fluids, either Ringer's lactate solution with 5% dextrose or half-strength Darrow's solution with 5% dextrose. If neither is available, 0.45% saline with 5% dextrose should be used (see Chart 8)
Monitoring
During rehydration, respiration and pulse rate should fall and urine start to be passed. The return of tears, a moist mouth, less sunken eyes and fontanelle, and improved skin turgor are also signs that rehydration is proceeding, but many severely malnourished children will not show these changes even when fully rehydrated. Monitor weight gain.
Monitor the progress of rehydration every 30 min for 2 h, then every hour for the next 4–10 h. Be alert for signs of overhydration, which is very dangerous and may lead to heart failure. Check for:
- weight gain to ensure that it is not quick and excessive.
- increase in respiratory rate
- increase in pulse rate
- urine frequency (Has the child urinated since last checked?)
- enlarging liver size on palpation
- frequency of stools and vomit.
Recipe for ReSoMal using standard WHO ORS
| Ingredient | Amount |
|---|---|
| Water | 2 litres |
| WHO ORS | One 1-litre packeta |
| Sucrose | 50 g |
| Electrolyte/mineral solutionb | 40 ml |
- a
2.6 g sodium chloride, 2.9 g trisodium citrate dihydrate, 1.5 g potassium chloride, 13.5 g glucose
- b
See below for the recipe for the electrolyte/mineral solution. If you use a commercially prepared electrolyte and mineral powder, follow the manufacturer's instructions. If these cannot be made up, use 45 ml of potassium chloride solution (100 g potassium chloride in 1 litre of water) instead.
ReSoMal contains approximately 45 mmol sodium, 40 mmol potassium and 3 mmol magnesium per litre.
Formula for concentrated electrolyte/mineral solution
This solution is used in the preparation of starter and catch-up feeding formulas and ReSoMal. Electrolyte and mineral powders are produced by some manufacturers. If these are not available or affordable, prepare the solution (2500 ml) using the following ingredients:
| Ingredient | g | mol/20 ml |
|---|---|---|
| Potassium chloride (KCl) | 224 | 24 mmol |
| Tripotassium citrate | 81 | 2 mmol |
| Magnesium chloride (MgCl2.6H2O) | 76 | 3 mmol |
| Zinc acetate (Zn acetate.2H2O) | 8.2 | 300 μmol |
| Copper sulfate (CuSO4.5H2O) | 1.4 | 45 μmol |
| Water to make up to | 2500 ml |
If available, also add selenium (0.028 g sodium selenate, NaSeO4.10H2O) and iodine (0.012 g potassium iodide, KI) per 2500 ml.
- Dissolve the ingredients in cooled boiled water.
- Store the solution in sterilized bottles in a refrigerator to retard deterioration. Discard if it turns cloudy. Make up fresh each month.
- Add 20 ml of the concentrated electrolyte/mineral solution to each 1000 ml of milk feed. If it is not possible to prepare this electrolyte/mineral solution and pre-mixed sachets are not available, give potassium, magnesium and zinc separately. Make a 10% stock solution of potassium chloride (100 g in 1 litre of water) and a 1.5% solution of zinc acetate (15 g in 1 litre of water).
For the oral rehydration solution ReSoMal, use 45 ml of the stock potassium chloride solution instead of 40 ml electrolyte/mineral solution
For milk feeds F-75 and F-100, add 22.5 ml of the stock potassium chloride solution instead of 20 ml of the electrolyte/mineral solution to 1000 ml of feed. Give the 1.5% zinc acetate solution by mouth at 1 ml/kg per day. Give 0.3 ml/kg of 50% magnesium sulfate intramuscularly once to a maximum of 2 ml.
If you find signs of overhydration (early signs are respiratory rate increasing by 5/min and pulse rate by 25/min), stop ReSoMal immediately and reassess after 1 h.
Prevention
Measures to prevent dehydration due to continuing watery diarrhoea are similar to those for well-nourished children (see treatment plan A), except that ReSoMal fluid is used instead of standard ORS.
- ►
If the child is breastfed, continue breastfeeding.
- ►
Initiate re-feeding with starter F-75.
- ►
Give ReSoMal between feeds to replace stool losses. As a guide, give 50–100 ml after each watery stool.
7.4.4. Electrolyte imbalance
All severely malnourished children have deficiencies of potassium and magnesium, which may take about 2 weeks to correct. Oedema is partly a result of potassium deficiency and sodium retention. Do not treat oedema with a diuretic. Excess body sodium exists even though the plasma sodium may be low. Giving high sodium loads could kill the child.
Treatment
- ►
Give extra potassium (3–4 mmol/kg per day).
- ►
Give extra magnesium (0.4–0.6 mmol/kg per day).
The extra potassium and magnesium should be added to the feed during its preparation if not pre-mixed. See recipefor a combined electrolyte/mineral solution. Add 20 ml of this solution to 1 litre of feed to supply the extra potassium and magnesium required. Alternatively, use commercially available pre-mixed sachets (specially formulated for malnourished children).
- ►
When rehydrating, give low sodium rehydration fluid (ReSoMal) (see recipe).
- ►
Prepare food without added salt.
7.4.5. Infection
In severe acute malnutrition, the usual signs of bacterial infection, such as fever, are often absent, yet multiple infections are common. Therefore, assume that all children with severe acute malnutrition have an infection on their arrival in hospital, and treat with antibiotics immediately. Hypoglycaemia and hypothermia are often signs of severe infection.
Treatment
Give all severely malnourished children:
- ►
a broad-spectrum antibiotic
- ►
measles vaccine if the child is ≥ 6 months and not vaccinated or was vaccinated before 9 months age. Delay vaccination if the child is in shock.
Choice of broad-spectrum antibiotics
- ►
If the child has uncomplicated severe acute malnutrition, give oral amoxicillin (for dosage, see annex 2) for 5 days.
- ►
If there are complications (hypoglycaemia, hypothermia or the child looks lethargic or sickly) or any other medical complication, give parenteral antibiotics:
- –
benzylpenicillin (50 000 U/kg IM or IV every 6 h) or ampicillin (50 mg/kg IM or IV every 6 h) for 2 days, then oral amoxicillin (25–40 mg/kg every 8 h for 5 days)
plus
- –
gentamicin (7.5 mg/kg IM or IV) once a day for 7 days.
These regimens should be adapted to local resistance patterns.
Note: Metronidazole 7.5 mg/kg every 8 h for 7 days may be given in addition to broad-spectrum antibiotics; however, the efficacy of this treatment has not been established in clinical trials.
- ►
Treat other infections as appropriate:
- –
If meningitis is suspected, do a lumbar puncture for confirmation, where possible, and treat with the antibiotic regime (section 6.3.1).
- –
If you identify other specific infections (such as pneumonia, dysentery, skin or soft-tissue infections), give antibiotics as appropriate.
- –
Add antimalarial treatment if the child has a positive blood film for malaria parasites or a positive malaria rapid diagnostic test.
- –
TB is common, but anti-TB treatment should be given only if TB is diagnosed or strongly suspected (see section 7.5.5).
- –
For HIV-exposed children, see Chapter 8.
Treatment for parasitic worms
If there is evidence of worm infestation, treatment should be delayed until the rehabilitation phase. Give albendazole as a single dose or mebendazole 100 mg orally twice a day for 3 days. In countries where infestation is prevalent, also give mebendazole to children with no evidence of infestation 7 days after admission.
HIV infection
Where HIV infection is common, children with severe acute malnutrition should be tested for HIV to determine their need for antiretroviral therapy (ART). If the child is infected with HIV, start ART as soon as possible after stabilization of metabolic complications and sepsis. They should be monitored closely (inpatient and outpatient) in the first 6–8 weeks following initiation of ART to identify early metabolic complications and opportunistic infections (see Chapter 8).
Monitoring
If the child is still anorexic after 7 days of antibiotic treatment, continue for a full 10-day course. If anorexia persists, reassess the child fully.
7.4.6. Micronutrient deficiencies
All severely malnourished children have vitamin and mineral deficiencies. Although anaemia is common, do not give iron initially, but wait until the child has a good appetite and starts gaining weight (usually in the second week), because iron can make infections worse.
Multvitamins including vitamin A and folic acid, zinc and copper are already present in F-75, F-100 and ready-to-use therapeutic food packets. When premixed packets are used, there is no need for additional doses.
In addition, if there are no eye signs or history of measles, then do not give a high dose of vitamin A because the amounts already present in therapeutic foods are enough.
Treatment
- ►
Give vitamin A on day 1 and repeat on days 2 and 14 only if child has any signs of vitamin A deficiency like corneal ulceration or a history of measles (see section 7.5.1).
- –
< 6 months, 50 000 U
- –
6–12 months, 100 000 U
- –
> 12 months, 200 000 U
- ►
Start iron at 3 mg/kg per day after 2 days on F-100 catch-up formula. Do not give iron in the stabilization phase, and do not give iron if the child is receiving ready-to-use therapeutic food (RUTF).
If child is not on any of the pre-mixed therapeutic foods, give the following micronutrients daily for at least 2 weeks:
- ►
folic acid at 5 mg on day 1; then 1 mg daily
- ►
multivitamin syrup at 5 ml
- ►
zinc at 2 mg/kg per day
- ►
copper at 0.3 mg/kg per day
7.4.7. Initial re-feeding
In the initial phase, re-feeding should be gradual.
Treatment
The essential features of initial feeding are:
- frequent (every 2–3 h) oral small feeds of low osmolality and low lactose
- nasogastric feeding if the child is eating ≤ 80% of the amount offered at two consecutive feeds
- calories at 100 kcal/kg per day
- protein at 1–1.5 g/kg per day
- liquid at 130 ml/kg per day or 100 ml/kg per day if the child has severe oedema
- in addition, if the child is breastfed, encourage continued breastfeeding, but make sure the prescribed amounts of starter formula are given:
| Days | Frequency | Volume/kg feed | Volume/kg per day |
|---|---|---|---|
| 1–2 | 2h | 11 ml | 130 ml |
| 3–5 | 3h | 16 ml | 130 ml |
| ≥6 | 4h | 22 ml | 130 ml |
The suggested starter formula and feeding schedules given below are designed to meet these targets. Milk-based formulas, such as starter F-75 (with 75 kcal and 0.9 g protein/100 ml), will be satisfactory for most children (see recipes). As cereal-based F-75 partially replaces sugar with cereal flour, it has the advantage of lower osmolarity, which may benefit some children with persistent diarrhoea, but it has to be cooked.
Feed from a cup or a bowl. Use a spoon, dropper or syringe to feed very weak children.
A recommended schedule, with a gradual increase in the feed volume and a gradual decrease in feeding frequency, see Table 22. For children with a good appetite and no oedema, this schedule can be completed in 2–3 days.
Table 22Volumes of F-75 per feed for malnourished children (approximately 130 ml/kg per day)
| Child's weight (kg) | 2-hourly (ml/feed) | 3-hourly (ml/feed) | 4-hourly (ml/feed) |
|---|---|---|---|
| 2.0 | 20 | 30 | 45 |
| 2.2 | 25 | 35 | 50 |
| 2.4 | 25 | 40 | 55 |
| 2.6 | 30 | 45 | 55 |
| 2.8 | 30 | 45 | 60 |
| 3.0 | 35 | 50 | 65 |
| 3.2 | 35 | 55 | 70 |
| 3.4 | 35 | 55 | 75 |
| 3.6 | 40 | 60 | 80 |
| 3.8 | 40 | 60 | 85 |
| 4.0 | 45 | 65 | 90 |
| 4.2 | 45 | 70 | 90 |
| 4.4 | 50 | 70 | 95 |
| 4.6 | 50 | 75 | 100 |
| 4.8 | 55 | 80 | 105 |
| 5.0 | 55 | 80 | 110 |
| 5.2 | 55 | 85 | 115 |
| 5.4 | 60 | 90 | 120 |
| 5.6 | 60 | 90 | 125 |
| 5.8 | 65 | 95 | 130 |
| 6.0 | 65 | 100 | 130 |
| 6.2 | 70 | 100 | 135 |
| 6.4 | 70 | 105 | 140 |
| 6.6 | 75 | 110 | 145 |
| 6.8 | 75 | 110 | 150 |
| 7.0 | 75 | 115 | 155 |
| 7.2 | 80 | 120 | 160 |
| 7.4 | 80 | 120 | 160 |
| 7.6 | 85 | 125 | 165 |
| 7.8 | 85 | 130 | 170 |
| 8.0 | 90 | 130 | 175 |
| 8.2 | 90 | 135 | 180 |
| 8.4 | 90 | 140 | 185 |
| 8.6 | 95 | 140 | 190 |
| 8.8 | 95 | 145 | 195 |
| 9.0 | 100 | 145 | 200 |
| 9.2 | 100 | 150 | 200 |
| 9.4 | 105 | 155 | 205 |
| 9.6 | 105 | 155 | 210 |
| 9.8 | 110 | 160 | 215 |
| 10.0 | 110 | 160 | 220 |
Note: If staff resources are limited, give priority to 2-hourly feeds for only the most seriously ill children, and aim for at least 3-hourly feeds initially. Ask mothers and other carers to help with feeding. Show them what to do, and supervise them. Night feeds are essential, and staff rosters may have to be adjusted. If, despite all efforts, not all the night feeds can be given, the feeds should be spaced equally through the night to avoid long periods without a feed (with the risk of increased hypoglycaemia and mortality).
If the child's intake (after allowing for any vomiting) does not reach 80 kcal/kg per day, despite frequent feeds, coaxing and re-offering, give the remaining feed by nasogastric tube. Do not exceed 100 kcal/kg per day in this initial phase.
In very hot climates, children might need extra water, as these foods may not contain enough water if the children are sweating.
Monitoring
Monitor and record:
- amounts of feed offered and left over
- vomiting
- stool frequency and consistency
- daily body weight
7.4.8. Catch-up growth feeding
Children in the catch-up phase should in most cases be managed as outpatients. Signs that a child has reached rehabilitation phase for catch-up growth are:
- return of appetite
- no episodes of hypoglycaemia (metabolically stable)
- reduced or disappearance of all oedema
Recipes for re-feeding formulas F-75 and F-100
| F-75a (starter: cereal-based) | F-100b (catch-up) | |
|---|---|---|
| Dried skimmed milk (g) | 25 | 80 |
| Sugar (g) | 70 | 50 |
| Cereal flour (g) | 35 | — |
| Vegetable oil (g) | 27 | 60 |
| Electrolyte/mineral solution (ml) | 20 | 20 |
| Water: make up to (ml) | 1000 | 1000 |
| Content per 100 ml | ||
| Energy (kcal) | 75 | 100 |
| Protein (g) | 1.1 | 2.9 |
| Lactose (g) | 1.3 | 4.2 |
| Potassium (mmol) | 4.2 | 6.3 |
| Sodium (mmol) | 0.6 | 1.9 |
| Magnesium (mmol) | 0.46 | 0.73 |
| Zinc (mg) | 2.0 | 2.3 |
| Copper (mg) | 0.25 | 0.25 |
| % energy from protein | 6 | 12 |
| % energy from fat | 32 | 53 |
| Osmolality (mOsm/litre) | 334 | 419 |
- a
Cook for 4 min and add mineral/vitamin mix after cooking. This may be helpful for children with dysentery or persistent diarrhoea.
- b
A comparable catch-up formula can be made from 110 g whole dried milk, 50 g sugar, 30 g oil, 20 ml electrolyte/mineral solution and water to make 1000 ml. If using fresh cow's milk, take 880 ml milk, 75 g sugar, 20 ml oil, 20 ml electrolyte/mineral solution and water to make 1000 ml.
Alternative for F-75 if milk is unavailable
Use precooked corn–soya or wheat–soya blend
- Corn–soya or wheat–soya blend, 50 g
- Sugar, 85 g
- Oil, 25 g
- Electrolyte/mineral mix, 20 ml
- Make up to 1000 ml with boiled water
Alternative for F-100 if milk is unavailable
Use precooked corn-soya or wheat-soya blend
- Corn–soya or wheat–soya blend, 150 g
- Sugar, 25 g
- Oil, 40 g
- Electrolyte/mineral mix, 20 ml
- Make up to 1000 ml with boiled water.
Treatment
Make a gradual transition from starter F-75 to catch-up formula F-100 or ready-to-use therapeutic food over 2–3 days, as tolerated.
- ►
Replace starter F-75 with an equal amount of catch-up F-100 for 2 days. Give a milk-based formula, such as catch-up F-100 containing 100 kcal/100 ml and 2.9 g of protein per 100 ml (see recipes) or ready-to-use therapeutic food (see below).
- ►
On the third day if on F-100, increase each successive feed by 10 ml until some feed remains uneaten. The point at which some feed remains unconsumed is likely to be when intake reaches about 200 ml/kg per day.
After a gradual transition, give:
- –
frequent feeds, unlimited amounts
- –
150–220 kcal/kg per day
- –
4–6 g of protein/kg per day.
If on ready-to-use therapeutic food:
- –
Start with small but regular meals of RUTF and encourage the child to eat often (first 8 meals per day, and later 5–6 meals per day). If the child cannot eat the whole amount of RUTF per meal in the transition phase, top up with F-75 to complete the feed, until is able to eat a full RUTF meal.
- –
If the child cannot take at least half of recommended amount of RUTF in 12 h, stop RUTF and give F-75. Try introducing RUTF again in 1–2 days until the child is able to take adequate amounts.
- –
If still breastfeeding, offer breast milk first before every RUTF feed.
After the transition phase, refer the child for rehabilitation in outpatient care or to a community feeding programme.
Wash hands before giving feeds.
- –
Sit with the child on the lap and gently offer the feeds.
- –
Encourage the child to eat the RUTF without forced feeding.
- –
Offer plenty of clean water in a cup, when the child is eating RUTF.
Recommended amounts per day of ready-to-use therapeutic food containing 500 kcal
| Transition Phase 150 kcal/kg/day | Rehabilitation Phase 200 kcal/kg/day | |
|---|---|---|
| Child's weight (kg) | Packets per day (92 g Packets Containing 500 kcal) | Packets per day (92 g Packets Containing 500 kcal) |
| 4.0–4.9 | 1.5 | 2.0 |
| 5.0–6.9 | 2.1 | 2.5 |
| 7.0–8.4 | 2.5 | 3.0 |
| 8.5–9.4 | 2.8 | 3.5 |
| 9.5–10.4 | 3.1 | 4.0 |
| 10.5–11.9 | 3.6 | 4.5 |
| ≥ 12.0 | 4.0 | 5.0 |
Monitoring
Avoid causing heart failure. Monitor for early signs of congestive heart failure (rapid pulse, fast breathing, basal lung crepitations, enlarging liver, gallop heart rhythm, raised jugular venous pressure). If both pulse and breathing rates increase (breathing by 5 breaths/min and pulse by 25 beats/min), and the increase is sustained for two successive 4-hourly readings, then:
- Reduce the volume fed to 100 ml/kg per day for 24 h.
- Then, gradually increase as follows:
- –
115 ml/kg per day for next 24 h
- –
130 ml/kg per day for the following 48 h
- Thereafter, increase each feed by 10 ml as described earlier.
Assess progress. After the transition, monitor progress by the rate of weight gain:
- Weigh the child every morning before feeding, and plot the weight.
- Calculate and record the weight gain every 3 days as g/kg per day (see box below).
Calculating weight gain
This example is for weight gain over 3 days.
- Current weight of the child in grams = 6300 g
- Weight 3 days ago in grams = 6000 g
- Step 1.
Calculate weight gain in grams: 6300–6000 = 300 g
- Step 2.
Calculate average daily weight gain: 300 g ÷ 3 days = 100 g/day
- Step 3.
Divide by child's average weight in kg: 100 g/day ÷ 6.15 kg = 16.3 g/kg per day
If the weight gain is:
- poor (< 5 g/kg per day), the child requires a full re-assessment
- moderate (5–10 g/kg per day), check whether the intake targets are being met or if infection has been overlooked
- good (> 10 g/kg per day).
7.4.9. Sensory stimulation
Provide:
- tender loving care
- a cheerful, stimulating environment
- structured play therapy for 15–30 min/day
- physical activity as soon as the child is well enough
- support for as much maternal involvement as possible (e.g. comforting, feeding, bathing, playing).
Provide suitable toys and play activities for the child.
7.4.10. Severe acute malnutrition in infants aged < 6 months
Severe acute malnutrition is less common in infants < 6 months than in older children. An organic cause for the malnutrition or failure to thrive should be considered, and, when appropriate, treated. Infants less than 6 months of age with severe acute malnutrition with any of the following complicating factors should be admitted for inpatient care:
- general danger signs or serious clinical condition as outlined for infants 6 months or older.
- recent weight loss or failure to gain weight.
- ineffective breastfeeding (attachment, positioning or suckling) directly observed for 15–20 min, ideally in a supervised separated area.
- any pitting bilateral oedema of the feet.
- any medical problem needing more detailed assessment
- any social issue requiring detailed assessment or intensive support (e.g. disability or depression of caretaker or other adverse social circumstances).
Treatment
- ►
Admit infants with any of the above complicating factors.
- ►
Give parenteral antibiotics to treat possible sepsis, and appropriate treatment for other medical complications.
- ►
Re-establish effective exclusive breastfeeding by the mother or other caregiver. If not possible, give replacement commercial infant formula with advice on safe preparation and use.
- ►
For infants with severe acute malnutrition and oedema, give infant formula or F-75 or diluted F-100 (add water to formula in recipes up to 1.5 litres instead of 1 litre) to supplement breastfeeding.
- ►
For infants with severe acute malnutrition with no oedema, give expressed breast milk; and when not possible, commercial infant formula or F-75 or diluted F-100, in this order of preference.
During nutritional rehabilitation, the basic principles for older children apply; however, young infants are less able to excrete salt and urea in their urine, especially in hot climates. Therefore, the preferred diets in the stabilization phase are (in order of preference):
- breast milk (if available in sufficient quantity)
- commercial infant formula
Assessment of the physical and mental health of mothers or caretakers should be promoted and relevant treatment or support provided.
Discharge
Infants less than 6 months of age admitted to inpatient care can be transferred to outpatient care if:
- all clinical conditions or medical complications including oedema are resolved or the child is clinically well and alert,
- the child is breastfeeding effectively or feeding well,
- weight gain is satisfactory e.g. above the median of the WHO growth velocity standards or more than 5gm/kg per day for at least 3 successive days.
Before discharge, the infant's vaccination status and other routine interventions should be checked and provided as appropriate. Mothers or caregivers should then be linked with any necessary community follow-up and support. A child should only be discharged from all nutritional care only when he or she:
- is breastfeeding effectively or feeding well with replacement feeds, and
- has an adequate weight gain, and
- has a weight-for-length equal or higher than -2 z scores.
7.5. Treatment of associated conditions
7.5.1. Eye problems
If the child has any eye signs of vitamin A deficiency:
- ►
Give vitamin A orally on days 1, 2 and 14 (age < 6 months, 50 000 IU; age 6–12 months, 100 000 IU; older children, 200 000 IU). If the first dose was given in the referring centre, treat on days 1 and 14 only.
If the eyes show signs of corneal clouding or ulceration, give the following additional care to prevent corneal rupture and extrusion of the lens:
- ►
Instil chloramphenicol or tetracycline eye drops four times a day, as required, for 7–10 days.
- ►
Instil atropine eye drops, one drop three times a day, for 3–5 days.
- ►
Cover with saline-soaked eye pads.
- ►
Bandage the eye(s).
7.5.2. Severe anaemia
Blood transfusion should be given in the first 24 h only if:
- Hb is < 4 g/dl
- Hb is 4–6 g/dl and the child has respiratory distress.
In severe acute malnutrition, the transfusion must be slower and of smaller volume than for a well-nourished child. Give:
- ►
whole blood, 10 ml/kg, slowly over 3 h
- ►
furosemide, 1 mg/kg IV at the start of the transfusion.
If the child has signs of heart failure, give 10 ml/kg of packed cells, because whole blood is likely to worsen this condition. Children with severe acute malnutrition with oedema may have redistribution of fluid leading to apparent low Hb, which does not require transfusion.
Monitoring
Monitor the pulse and breathing rates, listen to the lung fields, examine the abdomen for liver size and check the jugular venous pressure every 15 min during the transfusion.
- –
If either breathing or heart rate increases (breathing by 5 breaths/min or pulse by 25 beats/min), transfuse more slowly.
- –
If there are basal lung crepitations or an enlarging liver, stop the transfusion and give furosemide at 1 mg/kg IV.
Note: Do not repeat transfusion even if the Hb is still low or within 4 days of the last transfusion.
7.5.3. Skin lesions in kwashiorkor
Zinc deficiency is usual in children with kwashiorkor, and their skin quickly improves with zinc supplementation. In addition:
- ►
Bathe or soak the affected areas for 10 min/day in 0.01% potassium permanganate solution.
- ►
Apply barrier cream (zinc and castor oil ointment, petroleum jelly or tulle gras) to the raw areas, and gentian violet or nystatin cream to skin sores.
- ►
Avoid using nappies so that the perineum can stay dry.
7.5.4. Continuing diarrhoea
Treatment
Giardiasis
Where possible, examine the stools by microscopy.
- ►
If cysts or trophozoites of Giardia lamblia are found, give metronidazole (7.5 mg/kg every 8 h for 7 days). Treat with metronidazole if stool microscopy cannot be undertaken or if there is only clinical suspicion of giardiasis.
Lactose intolerance
Diarrhoea is only rarely due to lactose intolerance. Intolerance should be diagnosed only if copious watery diarrhoea occurs promptly after milk-based feeds are begun and if the diarrhoea clearly improves when milk intake is reduced or stopped. Starter F-75 is a low-lactose feed. In exceptional cases:
- ►
replace milk feeds with yoghurt or a lactose-free infant formula
- ►
reintroduce milk feeds gradually in the rehabilitation phase.
Osmotic diarrhoea
Osmotic diarrhoea may be suspected if the diarrhoea worsens substantially with hyperosmolar F-75 and ceases when the sugar content and osmolarity are reduced. In these cases:
- ►
Use cereal-based starter F-75 (see recipes) or, if necessary, a commercially available isotonic starter F-75.
- ►
Introduce catch-up F-100 or ready-to-use therapeutic food gradually.
7.5.5. Tuberculosis
If TB is strongly suspected:
- Perform a Mantoux test (Note: false-negative results are frequent).
- Take a chest X-ray, if possible.
If these are positive or TB is strongly suspected, treat according to national TB guidelines (see section 4.7.2).
7.6. Discharge and follow-up
7.6.1. Transfer to outpatient care
Children admitted to hospital with complicated severe acute malnutrition can be transferred to outpatient care during the rehabilitation phase. Social factors, such as loss of earnings for the mother and care for other children, should also be taken into account, as should the fact that those without complications can be managed as outpatients or in the community. Carefully assess the child and the available community support. The child will require continuing care as an outpatient to complete rehabilitation and prevent relapse.
The decision to transfer children to outpatient care should not be based on achievement of specific anthropometric or weight-for-height/length outcomes. Children should be discharged from hospital to outpatient or a nutritional programme when:
- they have completed parenteral antibiotic treatment, and are clinically well and alert
- medical complications are resolved
- their appetite has fully recovered and they are eating well
- oedema has reduced or resolved.
It is important to prepare the parents for outpatient treatment or in a community nutrition programme where such services are available. Ask the caregiver to bring the child back for weekly therapeutic food, and make sure the child receives vaccinations and routine vitamin A supplements, as appropriate.
The mother or carer should:
- be available for child care
- have received specific counselling on appropriate child feeding practices (types, amount, frequency)
- have the resources to feed the child. If this is not the case, give advice on available support.
7.6.2. Discharge from nutritional treatment
Children with severe acute malnutrition should be discharged from the nutritional treatment programme only when their:
- weight-for-height/length is at least ≥ -2 z score and they have had no oedema for at least 2 weeks, or
- mid-upper-arm circumference is ≥ 125 mm and they have had no oedema for at least 2 weeks.
The decision should be based on the same anthropometric indicator that was used on admission. Thus, if mid-upper arm circumference was used, then it should be used to assess and confirm nutritional recovery, and similarly for weight for length/height. Children admitted with only bilateral pitting oedema, should be discharged on the basis of either mid-upper arm circumference or weight-for-height/length depending on the indicator used routinely in the national nutrition programme. Percentage weight gain should not be used as a discharge criterion.
The child should be fed at least five times a day with foods that contain approximately 100 kcal and 2–3 g protein per 100 g of food. It is essential to give frequent meals with a high energy and protein content. The mother should be counselled on appropriate feeding to:
- ►
give appropriate meals (and the correct quantity of food) at least five times daily.
- ►
give high-energy snacks between meals (e.g. milk, banana, bread, biscuits).
- ►
assist and encourage the child to complete each meal.
- ►
give food separately to the child so that the child's intake can be checked.
- ►
breastfeed as often as the child wants.
7.6.3. Follow-up
When a child is discharged to outpatient, make a plan for following up of the child until full recovery, and contact the outpatient department, nutrition rehabilitation centre, local health clinic or health worker who will take responsibility for continuing supervision of the child. In general, the child should be weighed weekly after discharge.
If he or she fails to gain weight over a 2-week period or loses weight between two measurements or develops loss of appetite or oedema, the child should be referred back to hospital for further assessment. Once discharged from the nutritional treatment, he or she should be periodically monitored to avoid relapse.
7.7. Monitoring the quality of care
7.7.1. Mortality audit
A register of admissions, discharges and deaths should be kept. This should contain information about the children (such as weight, age and sex), day of admission, date of discharge or date and time of death.
To identify factors that can be changed to improve care, determine whether most of the deaths occurred:
- within 24 h: consider untreated or delayed treatment of hypoglycaemia, hypothermia, septicaemia or severe anaemia, incorrect rehydration fluid or volume of fluid or overuse of IV fluids.
- within 72 h: check whether the volume of feed given during re-feeding was too high or the formulation was wrong. Were potassium and antibiotics given?
- over 72 h: consider nosocomial infection, re-feeding syndrome, heart failure and HIV infection.
- at night: consider hypothermia due to insufficient covering of the child or no night feeds.
- when beginning F-100 or RUTF: consider too rapid a transition from starter to catch-up feeds.
7.7.2. Weight gain during rehabilitation
Standardize weighing on the hospital ward. Calibrate the scales every day. Weigh children at the same time each day (e.g. morning) after removing clothes (but avoid hypothermia).
Weight gain is defined as:
- –
poor: < 5 g/kg per day
- –
moderate: 5–10 g/kg per day
- –
good: > 10 g/kg per day.
If the weight gain is < 5 g/kg per day, determine whether this occurred:
- –
in all children being treated (if so, a major review of case management is required)
- –
in specific cases (reassess these children as if they were new admissions).
General aspects to be checked if weight gain is poor are described below.
Inadequate feeding
Check:
- that night feeds are given
- that target energy and protein intakes are achieved. Is the actual intake (i.e. what was offered minus what was left over) correctly recorded? Is the quantity of feed recalculated as the child gains weight? Is the child vomiting or ruminating?
- feeding technique: Is the child given frequent feeds in unlimited amounts?
- quality of care: Are staff motivated, gentle, loving and patient?
- all aspects of feed preparation: scales, measurement of ingredients, mixing, taste, hygienic storage, adequate stirring if separating out
- whether the complementary foods given to the child are energy-dense enough
- adequacy of multivitamin composition and shelf-life
- preparation of mineral mix and whether correctly prescribed and administered. If you are in a goitrous region, check whether potassium iodide is added to the electrolyte/mineral mix (12 mg/2500 ml), or give all children Lugol iodine (5–10 drops a day).
- if complementary foods are given, check that they contain electrolyte/mineral solution.
Untreated infection
If feeding is adequate and there is no malabsorption, suspect a hidden infection if there is recurrence of oedema, hypoglycaemia or hypothermia. The following are easily overlooked: urinary tract infections, otitis media, TB and giardiasis. In such cases:
- re-examine carefully
- repeat urine microscopy for white blood cells
- examine the stools
- if possible, take a chest X-ray.
Consider treatment in the absence of a confirmatory diagnosis.
HIV/AIDS
Children with HIV and AIDS can recover from malnutrition, but it may take longer, and treatment failures are commoner. Initial nutritional treatment of severe acute malnutrition in children with HIV/AIDS should be the same as for HIV-negative children.
For other HIV-related conditions, see Chapter 8.
Psychological problems
Check for abnormal behaviour, such as stereotyped movements (rocking), rumination (i.e. self-stimulation through regurgitation) and attention-seeking. Treat by giving the child special love and attention. For children who ruminate, firmness with affection can assist. Encourage the mother to spend time playing with her child.
- Severe acute malnutrition - Pocket Book of Hospital Care for ChildrenSevere acute malnutrition - Pocket Book of Hospital Care for Children
Your browsing activity is empty.
Activity recording is turned off.
See more...