Molecular Pathogenesis
The enzyme phosphorylase kinase (PhK) activates liver glycogen phosphorylase and muscle glycogen phosphorylase in response to neuronal and hormonal stimuli and thus is a key regulatory enzyme in glycogen breakdown. In liver PhK deficiency, the inability to break down glycogen results in risk for hypoglycemia and glycogen accumulation in the liver, which in turn causes hepatomegaly and liver damage.
PhK is a multi-subunit enzyme composed of four copies each of four subunits (α, β, γ, and δ). The gamma (γ) subunit contains the catalytic activity and is regulated by the alpha (α), beta (β), and delta (δ) subunits. The inhibitory effect of the alpha and beta subunits is modulated by phosphorylation (phosphorylation removes the inhibitory effect); calcium levels modulate the regulatory effect of the delta subunit (calmodulin).
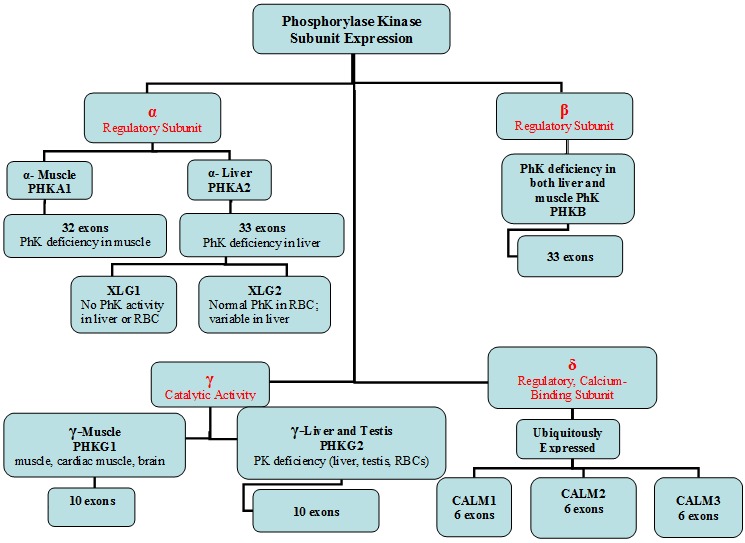
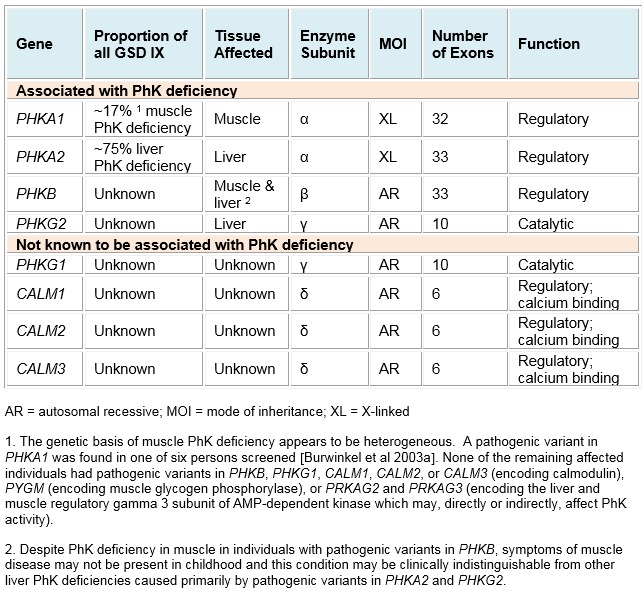
Each PhK subunit is encoded by at least one gene: PHKA1 and PHKA2 encode the muscle and liver isoforms of the α-subunit, respectively; PHKB encodes the liver and muscle β-subunits; PHKG1 and PHKG2 encode the muscle and liver isoforms of the γ-subunit, respectively; and the δ-subunit, calmodulin, is encoded by three genes: CALM1, CALM2, and CALM3. Expression of these genes is tissue dependent (). Further complexity is introduced by tissue-specific alternative splicing. The complexity of the enzyme PhK explains to some degree the clinical and biochemical heterogeneity of PhK deficiency.
Of these eight genes, four are known to contain pathogenic variants that cause PhK enzyme deficiency ().
The two X-linked genes are:
PHKA1, which causes the rare disorder X-linked muscle PhK deficiency; and
PHKA2, which causes the most common form of liver PhK deficiency, also known as X-linked liver glycogenosis (XLG).
The two autosomal genes are:
PHKB, which causes PhK deficiency in both liver and muscle but manifests primarily with liver symptoms with or without muscle involvement; and
PHKG2, which causes PhK deficiency in liver.
Muscle PhK activity is normal in individuals with pathogenic variants in either PHKA2 or PHKG2 and can be deficient in those with pathogenic variants in PHKB.
PHKA1
Gene structure. Alternatively spliced transcript variants encoding different isoforms have been identified in this gene. The longest transcript (NM_002637.3) consists of 32 exons and is transcribed into a 6-kb cDNA. PHKA1 spans approximately 133 kb of genomic DNA. A pseudogene, PHKA1P1, has been found on chromosome 1p22.2. For a detailed summary of gene and protein information, see Table A, Gene.
Pathogenic variants. To date, seven pathogenic variants have been reported in PHKA1, each of which was found in only one or two individuals. Pathogenic variants include missense (3), frameshift (2), nonsense(1), and splice site changes (1) [Wehner et al 1994, Bruno et al 1998, Burwinkel et al 2003a, Wuyts et al 2005, Ørngreen et al 2008, Echaniz-Laguna et al 2010].
A frameshift variant in mouse ortholog Phka1 causes PhK deficiency in the I-strain mouse [Schneider et al 1993].
Normal gene product.
PHKA1 encodes the muscle isoform of the alpha subunit of PhK, a 1,223-amino-acid protein (NP_002628.2).
Two alternatively spliced transcript variants encoding different isoforms have been identified [Harmann et al 1991]; alpha-FM is the predominant form in fast-twitch skeletal muscle and is also expressed in brain, while alpha-prime is the predominant form in slow-twitch skeletal muscle. Alpha-prime has an internal deletion of 59 amino acids (amino acids 654-712) when compared to alpha-FM.
The degree of phosphorylation of the alpha subunit regulates the activity of PhK; the greater the phosphorylation, the less the inhibitory effect.
Abnormal gene product. Muscle PhK deficiency due to pathogenic variants in PHKA1 appears to cause myopathy through a defect in glycogen availability during submaximal exercise (oxidative metabolism; e.g., cycle test) presumably because PhK is required to activate glycogen phosphorylase under these conditions. Interestingly, anaerobic glycogenolysis is normal, suggesting that other regulatory factors are involved in phosphorylase activation in this situation [Ørngreen et al 2008].
Complete lack of PHKA1 protein is predicted to affect formation or stability of PhK holoenzyme. Production of an altered PHKA1 protein, resulting from missense variants, may affect its ability to interact with other subunits or to activate PhK activity.
PHKA2
Gene structure. The gene contains 33 exons [Hendrickx et al 1999] and spans 91.3 kb of DNA. Alternatively spliced transcript variants have been reported, but the full-length nature of these variants has not been determined. For a detailed summary of gene and protein information, see Table A, Gene.
Pathogenic variants. More than 100 different pathogenic variants have been reported in PHKA2. Most of them are missense or nonsense variants or small deletions causing frameshifts. Only seven gross deletions/duplications have been reported. The pathogenic variants are distributed throughout the gene.
Table 4.
PHKA2 Pathogenic Variants Discussed in This GeneReview
View in own window
Variants listed in the table have been provided by the authors. GeneReviews staff have not independently verified the classification of variants.
GeneReviews follows the standard naming conventions of the Human Genome Variation Society (varnomen.hgvs.org). See Quick Reference for an explanation of nomenclature.
Normal gene product.
PHKA2 encodes the liver alpha subunit of PhK. A 5,325-bp mRNA is translated into a 1,235-amino-acid protein with high expression in liver and brain, but not in muscle [Hendrickx et al 1993]. PHKA2 is highly homologous to PHKA1 and PHKB.
Abnormal gene product. Two biochemical subtypes of X-linked glycogenosis (XLG) are caused by pathogenic variants in PHKA2 [Hendrickx et al 1994, Burwinkel et al 1996, Hendrickx et al 1996, Burwinkel et al 1998a, Hendrickx et al 1999]:
XLG1, the more common form, in which in vitro PhK activity is deficient in peripheral blood cells and liver
XLG2, in which in vitro PhK activity in peripheral blood cells is normal or even elevated and activity in liver is variable
While not yet fully understood, there are various theories as to how different pathogenic variants in PHKA2 could result in these different biochemical subtypes.
Regarding correlation between genotype and biochemical phenotype, Hendrickx et al [1999] suggested the following:
PHKA2 variants resulting in reduced amounts of alpha subunit protein (e.g., nonsense and frameshift variants or missense variants that destabilize the protein) cause detectable PhK deficiency in vitro (XLG1 biochemical subtype).
PHKA2 variants that disrupt activation of PhK enzyme activity (e.g., missense variants or small in-frame insertions or deletions affecting regulatory sites of the enzyme) can result in the normal PhK activity that is observed in vitro in some affected persons (XLG2 biochemical subtype).
These subtle changes may allow normal amounts of PhK to be made but affect enzyme function [Maire et al 1991, Hendrickx et al 1994, Burwinkel et al 1996, Hendrickx et al 1996, Burwinkel et al 1997b, Burwinkel et al 1998a, Hendrickx et al 1998].
Carrière et al [2008] showed that PHKA2 missense variants and small in-frame deletions/insertions are concentrated into two domains of the protein, the N-terminal glucoamylase domain (principally leading to XLG2) and the C-terminal calcineurin B-like domain (domain D; principally leading to XLG1).
Further studies are needed to determine the molecular basis of the XLG1 and XLG2 biochemical subtypes. Of note, the same PHKA2 variant (p.Arg295His) has been associated with normal and deficient PhK activity in vitro, suggesting that other factors, such as handling of the specimen and laboratory methodologies, can also affect the biochemical phenotype [Hendrickx et al 1999].
PHKB
Gene structure. Alternatively spliced transcript variants encoding different isoforms have been identified in this gene. The longer transcript variant, NM_000293.2, is composed of 33 exons spanning 239 kb of genomic DNA. Exons 26 and 27 are two homologous, mutually exclusively spliced exons that encode muscle and non-muscle PHKB, respectively; exon 2 is a facultatively used cassette exon encoding an alternative N-terminus [Wüllrich-Schmoll & Kilimann 1996]. For a detailed summary of gene and protein information, see Table A, Gene.
Two processed pseudogenes have been identified: PHKBP1 on chromosome 20p12.3-20p12.2 and PHKBP2 on chromosome 14q13.3 [Wüllrich-Schmoll & Kilimann 1996].
Pathogenic variants. More than 20 variants suspected or known to be pathogenic have been reported in PHKB. These include nonsense, missense, splice site, frameshift, and gross deletion changes [Burwinkel et al 1997b, van den Berg et al 1997, Burwinkel et al 2003a, Beauchamp et al 2007]. Two of the missense changes, p.Met185Ile and p.Gln657Lys, were identified in heterozygotes in whom no other pathogenic variant was identified, and thus their significance is unknown [Burwinkel et al 1997a, Burwinkel et al 2003a, Beauchamp et al 2007].
Table 5.
PHKB Pathogenic Variants Discussed in This GeneReview
View in own window
| DNA Nucleotide Change | Predicted Protein Change | Reference Sequences |
|---|
| c.555G>T | p.Met185Ile |
NM_000293.2
|
| c.1969C>A | p.Gln657Lys |
Variants listed in the table have been provided by the authors. GeneReviews staff have not independently verified the classification of variants the classification of variants.
GeneReviews follows the standard naming conventions of the Human Genome Variation Society (varnomen.hgvs.org). See Quick Reference for an explanation of nomenclature.
Normal gene product.
PHKB encodes the beta subunit of liver or muscle PhK. The degree of phosphorylation of the beta subunit determines the activity of the enzyme PhK.
Abnormal gene product. It is not known exactly how PHKB pathogenic variants result in PhK deficiency. Lack of PHKB protein would affect formation of the normal PhK holoenzyme, and an abnormal PHKB protein would presumably affect its interaction with other PhK subunits and its regulatory function. Biochemical evidence suggests that an alpha-gamma-delta complex may form in the absence of the beta subunit, explaining the residual enzyme activity seen in some individuals and the mild clinical features [Burwinkel et al 1997a, Brushia & Walsh 1999].
PHKG2
Gene structure. Alternatively spliced transcript variants encoding different isoforms have been identified in this gene. The PHKG2 longer transcript isoform NM_000294.2 comprises ten exons spanning 9 kb of genomic DNA. A complex microsatellite repeat has been identified at the beginning of intron 2 [Burwinkel et al 1998b]. For a detailed summary of gene and protein information, see Table A, Gene.
Pathogenic variants. More than 30 pathogenic variants have been reported in PHKG2 including missense, nonsense, splice site, and frameshift changes [Maichele et al 1996, van Beurden et al 1997, Burwinkel et al 1998b, Burwinkel et al 2000, Burwinkel et al 2003b, Beauchamp et al 2007].
Normal gene product.
PHKG2 encodes the catalytic gamma subunit of liver PhK, a 406-amino-acid protein, NP_000285.1. Alternative splicing creates a variant of 374 amino acids with a different C-terminus.
Abnormal gene product. Pathogenic variants in PHKG2 are expected to affect the catalytic ability of the gamma subunit either by resulting in production of no protein or affecting the stability or confirmation of the protein.