NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
PDQ Cancer Information Summaries [Internet]. Bethesda (MD): National Cancer Institute (US); 2002-.

PDQ Cancer Information Summaries [Internet].
Show detailsThis PDQ cancer information summary has current information about the treatment of hairy cell leukemia. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change. The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
General Information About Hairy Cell Leukemia
Key Points for This Section
Hairy cell leukemia is a type of cancer in which the bone marrow makes too many lymphocytes (a type of white blood cell).
Hairy cell leukemia is a cancer of the blood and bone marrow. This rare type of leukemia gets worse slowly or does not get worse at all. The disease is called hairy cell leukemia because the leukemia cells look "hairy" when viewed under a microscope.
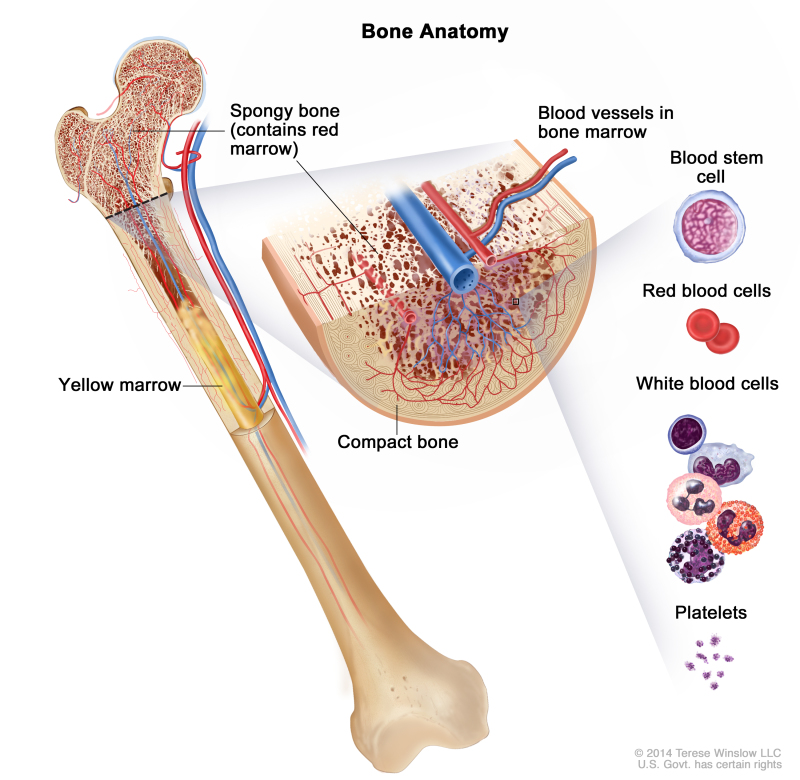
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Leukemia may affect red blood cells, white blood cells, and platelets.
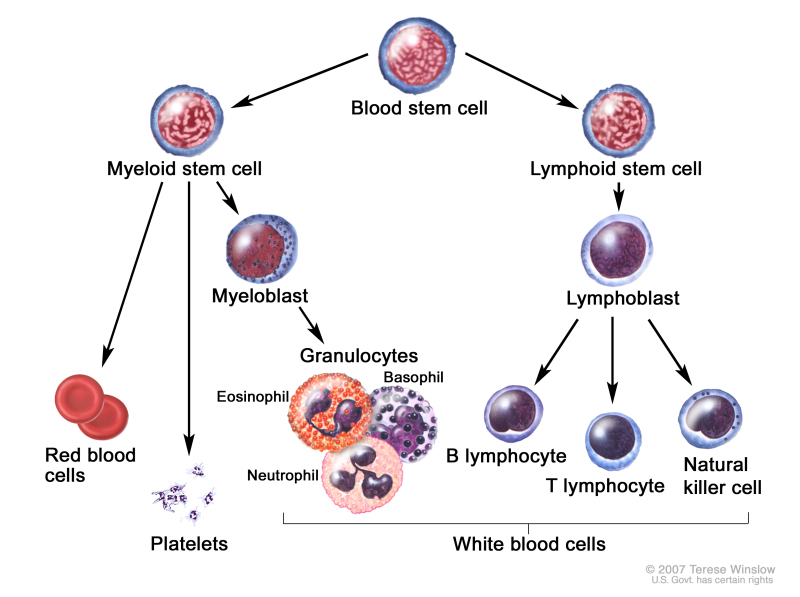
Normally, the bone marrow makes blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell.
A myeloid stem cell becomes one of three types of mature blood cells:
- White blood cells that fight infection and disease.
- Platelets that form blood clots to stop bleeding.
A lymphoid stem cell becomes a lymphoblast cell and then into one of three types of lymphocytes (white blood cells):
- B lymphocytes that make antibodies to help fight infection.
- T lymphocytes that help B lymphocytes make antibodies to help fight infection.
- Natural killer cells that attack cancer cells and viruses.
Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell.
In hairy cell leukemia, too many blood stem cells become lymphocytes. These lymphocytes are abnormal and do not become healthy white blood cells. They are also called leukemia cells. The leukemia cells can build up in the blood and bone marrow so there is less room for healthy white blood cells, red blood cells, and platelets. This may cause infection, anemia, and easy bleeding. Some of the leukemia cells may collect in the spleen and cause it to swell.
This summary is about hairy cell leukemia. See the following PDQ summaries for information about other types of leukemia:
Gender and age may affect the risk of hairy cell leukemia.
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk. The cause of hairy cell leukemia is unknown. It occurs more often in older men.
Signs and symptoms of hairy cell leukemia include infections, tiredness, and pain below the ribs.
These and other signs and symptoms may be caused by hairy cell leukemia or by other conditions. Check with your doctor if you have any of the following:
- Weakness or feeling tired.
- Fever or frequent infections.
- Easy bruising or bleeding.
- Shortness of breath.
- Weight loss for no known reason.
- Pain or a feeling of fullness below the ribs.
Tests that examine the blood and bone marrow are used to detect (find) and diagnose hairy cell leukemia.
The following tests and procedures may be used:
- Physical exam and history: An exam of the body to check general signs of health, including checking for signs of disease, such as a swollen spleen, lumps, or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
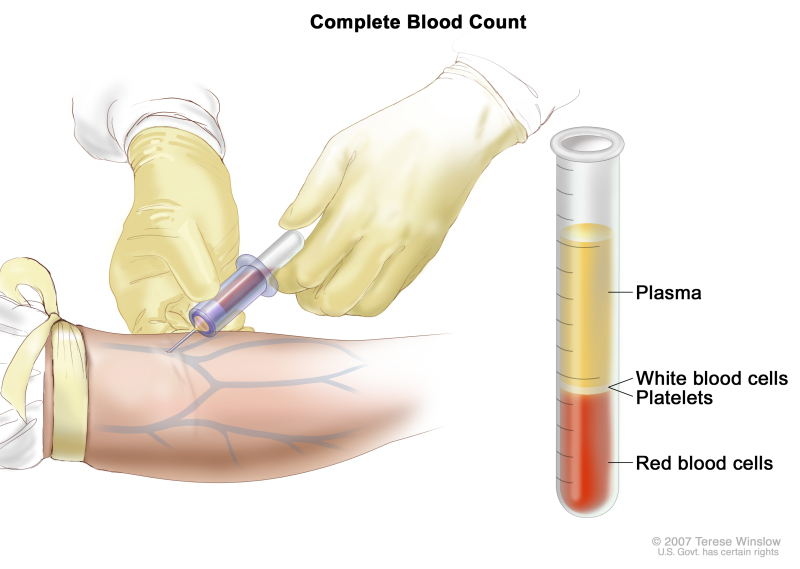
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- -
The number of red blood cells, white blood cells, and platelets.
- -
The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- -
The portion of the sample made up of red blood cells.
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions.
- Peripheral blood smear: A procedure in which a sample of blood is checked for cells that look "hairy," the number and kinds of white blood cells, the number of platelets, and changes in the shape of blood cells.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
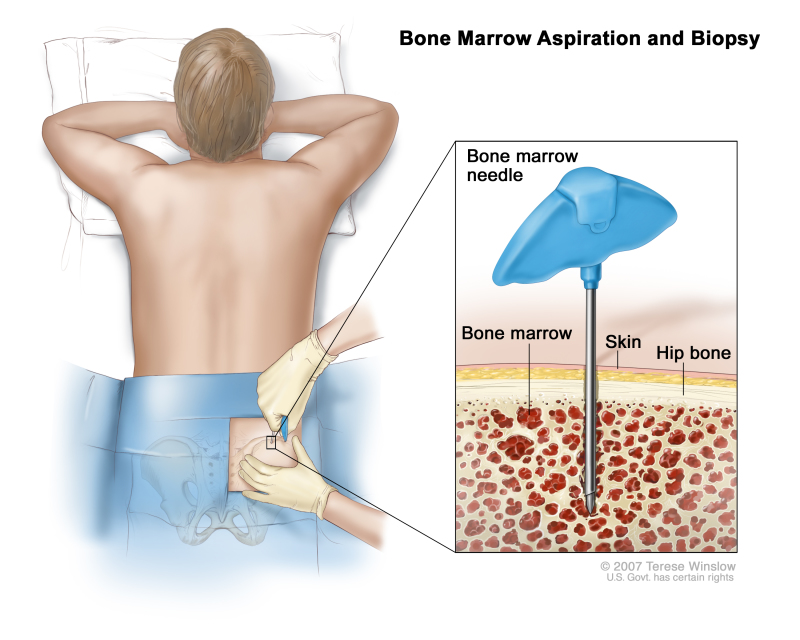
- Bone marrow aspiration and biopsy: The removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for signs of cancer.
- Immunophenotyping: A laboratory test in which the antigens or markers on the surface of a blood or bone marrow cell are checked to see what type of cell it is. This test is done to diagnose the specific type of leukemia by comparing the cancer cells to normal cells of the immune system.
- Flow cytometry: A laboratory test that measures the number of cells in a sample, the percentage of live cells in a sample, and certain characteristics of cells, such as size, shape, and the presence of tumor markers on the cell surface. The cells are stained with a light-sensitive dye, placed in a fluid, and passed in a stream before a laser or other type of light. The measurements are based on how the light-sensitive dye reacts to the light.
- Cytogenetic analysis: A laboratory test in which cells in a sample of tissue are viewed under a microscope to look for certain changes in the chromosomes.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. A CT scan of the abdomen may be done to check for swollen lymph nodes or a swollen spleen.
Certain factors affect treatment options and prognosis (chance of recovery).
The treatment options may depend on the following:
- The number of hairy (leukemia) cells and healthy blood cells in the blood and bone marrow.
- Whether the spleen is swollen.
- Whether there are signs or symptoms of leukemia, such as infection.
- Whether the leukemia has recurred (come back) after previous treatment.
The prognosis (chance of recovery) depends on the following:
- Whether the hairy cell leukemia does not grow or grows so slowly it does not need treatment.
- Whether the hairy cell leukemia responds to treatment.
Treatment often results in a long-lasting remission (a period during which some or all of the signs and symptoms of the leukemia are gone). If the leukemia returns after it has been in remission, retreatment often causes another remission.
Stages of Hairy Cell Leukemia
Key Points for This Section
There is no standard staging system for hairy cell leukemia.
Staging is the process used to find out how far the cancer has spread. Groups are used in place of stages for hairy cell leukemia. The disease is grouped as untreated, progressive, or refractory.
Untreated hairy cell leukemia
The hairy cell leukemia is newly diagnosed and has not been treated except to relieve signs or symptoms such as weight loss and infections. In untreated hairy cell leukemia, some or all of the following conditions occur:
- The spleen may be larger than normal.
Progressive hairy cell leukemia
In progressive hairy cell leukemia, the leukemia has been treated with either chemotherapy or splenectomy (removal of the spleen) and one or both of the following conditions occur:
Relapsed or Refractory Hairy Cell Leukemia
Relapsed hairy cell leukemia has come back after treatment. Refractory hairy cell leukemia has not responded to treatment.
Treatment Option Overview
Key Points for This Section
There are different types of treatment for patients with hairy cell leukemia.
Different types of treatment are available for patients with hairy cell leukemia. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Five types of standard treatment are used:
Watchful waiting
Watchful waiting is closely monitoring a patient's condition, without giving any treatment until signs or symptoms appear or change.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated. Cladribine and pentostatin are anticancer drugs commonly used to treat hairy cell leukemia. These drugs may increase the risk of other types of cancer, especially Hodgkin lymphoma and non-Hodgkin lymphoma. Long-term follow up for second cancers is very important.
Biologic therapy
Biologic therapy is a cancer treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy. Interferon alfa is a biologic agent commonly used to treat hairy cell leukemia.
See Drugs Approved for Hairy Cell Leukemia for more information.
Surgery
Splenectomy is a surgical procedure to remove the spleen.
Targeted therapy
Targeted therapy is a treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Monoclonal antibody therapy is a type of targeted therapy used to treat hairy cell leukemia.
Monoclonal antibody therapy uses antibodies made in the laboratory from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells.
A monoclonal antibody called rituximab may be used for certain patients with hairy cell leukemia.
Other types of targeted therapies are being studied.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment Options for Hairy Cell Leukemia
Untreated Hairy Cell Leukemia
If the patient's blood cell counts are not too low and there are no signs or symptoms, treatment may not be needed and the patient is carefully watched for changes in his or her condition. If blood cell counts become too low or if signs or symptoms appear, initial treatment may include the following:
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Progressive Hairy Cell Leukemia
Treatment for progressive hairy cell leukemia may include the following:
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Relapsed or Refractory Hairy Cell Leukemia
Treatment of relapsed or refractory hairy cell leukemia may include the following:
- A clinical trial of a new biologic therapy.
- A clinical trial of a new targeted therapy.
- A clinical trial of chemotherapy and targeted therapy with a monoclonal antibody (rituximab).
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Hairy Cell Leukemia
For more information from the National Cancer Institute about hairy cell leukemia, see the following:
For general cancer information and other resources from the National Cancer Institute, see the following:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of hairy cell leukemia. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials are listed in PDQ and can be found online at NCI's website. Many cancer doctors who take part in clinical trials are also listed in PDQ. For more information, call the Cancer Information Service 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Hairy Cell Leukemia Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/leukemia/patient/hairy-cell-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389248]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 2,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
- Hairy Cell Leukemia Treatment (PDQ®) - PDQ Cancer Information SummariesHairy Cell Leukemia Treatment (PDQ®) - PDQ Cancer Information Summaries
- Childhood Ovarian Cancer Treatment (PDQ®) - PDQ Cancer Information SummariesChildhood Ovarian Cancer Treatment (PDQ®) - PDQ Cancer Information Summaries
- AI1 intron-encoded reverse transcriptase aI1 [Saccharomyces cerevisiae S288C]AI1 intron-encoded reverse transcriptase aI1 [Saccharomyces cerevisiae S288C]Gene ID:854593Gene
- Timm23 translocase of inner mitochondrial membrane 23 [Mus musculus]Timm23 translocase of inner mitochondrial membrane 23 [Mus musculus]Gene ID:53600Gene
Your browsing activity is empty.
Activity recording is turned off.
See more...