Summary
Clinical characteristics.
Untreated pyridox(am)ine 5'-phosphate oxidase (PNPO) deficiency, characterized by a range of seizure types, is "classic" (i.e., seizure onset in the neonatal period) in about 90% of affected individuals and "late onset" (seizure onset after the neonatal period) in about 10%. In classic PNPO deficiency, seizures (including status epilepticus) often begin on the first day of life and typically before age two weeks. In both classic and late-onset untreated PNPO deficiency, seizure semiology varies from myoclonic to clonic or tonic seizures, and seizures are typically resistant to common anti-seizure medications. Independent of age of onset, seizures respond to life-long treatment with a B6 vitamer: pyridoxal 5'-phosphate (PLP) in about 60% of affected individuals and pyridoxine (PN) in about 40%.
About 60% of individuals with PNPO deficiency have developmental impairment, affecting speech, cognition, and behavior; some individuals have neurologic impairment such as muscular hypotonia or dystonia. Severe neurodevelopmental impairment is more likely to occur in individuals with PNPO deficiency who experienced diagnostic delay and prolonged periods of uncontrolled seizures.
Diagnosis/testing.
The diagnosis of PNPO deficiency is established in a proband with suggestive findings (i.e., infantile onset of a wide range of seizure types resistant to common anti-seizure medications and a positive standardized vitamin B6 trial) and (most commonly) biallelic pathogenic variants in PNPO identified by molecular genetic testing or deficient PNPO enzyme activity.
Management.
Targeted therapy: Pharmacologic treatment: PLP, the active form of vitamin B6, is typically given orally, divided into 4-6 single daily doses. The lowest effective PLP dose should be used to avoid possible liver toxicity. PN is typically given orally, divided into 3-4 single daily doses. PN side effects can include sensory (or motor) neuropathy, usually reversible with dose reduction.
Supportive care: Supportive care often includes specialists from multiple disciplines such as neurology, developmental pediatrics, speech-language therapy, physical therapy, occupational therapy, and mental health.
Surveillance: Routine monitoring of seizure control and possible adverse effects of PLP therapy; neurologic examination for emergence of new findings and/or response to medications used in symptomatic treatment; and assessment of development/educational needs.
Agents/circumstances to avoid: Avoid anti-seizure medications (such as carbamazepine, valproate, phenytoin, and phenobarbital) that can reduce plasma PLP concentration. Attention to PLP dose requirements when hydrazines or isoniazid are given to treat other conditions.
Evaluation of relatives at risk: When prenatal testing has not been performed on a pregnancy at risk, prompt evaluation of a newborn sib is essential to determine if treatment with either PN or PLP is necessary.
Pregnancy management: Although empiric data on the utility of maternal PN supplementation during pregnancy for a fetus known to have or be at risk for PNPO deficiency are limited, consider giving 50-100 mg/day of PN to the mother during the last 20 weeks of pregnancy. PN (not PLP) supplementation is recommended for two reasons: the mother has the capacity to metabolize PN into PLP, and the risk of PLP hepatotoxicity in pregnancy is unknown.
Genetic counseling.
PNPO deficiency is inherited in an autosomal recessive manner. If both parents are known to be heterozygous for a PNPO pathogenic variant, each sib of an affected individual, irrespective of sex, has at conception a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. Once both PNPO pathogenic variants have been identified in an affected family member, carrier testing for at-risk relatives, prenatal testing for a pregnancy at increased risk, and preimplantation genetic testing for PNPO deficiency are possible.
GeneReview Scope
Table.
PNPO Deficiency: Included Phenotypes
Diagnosis
No consensus clinical diagnostic criteria for pyridox(am)ine 5'-phosphate oxidase (PNPO) deficiency have been published.
Suggestive Findings
PNPO deficiency should be suspected in individuals with the following suggestive clinical phenotypes, positive response to a standardized vitamin B6 trial, supportive laboratory findings, and family history.
Clinical Findings
Classic PNPO deficiency (defined as neonatal onset) in premature infants and neonates
- Intrauterine seizures, recognized by mothers as episodic, repetitive rhythmic movements
- Fetal distress before delivery
- Low APGAR scores
- Difficult-to-treat seizures irrespective of a history of fetal distress
- Epileptic encephalopathy or signs of encephalopathy (e.g., inconsolable crying, hyperalertness, jitteriness, irritability, dysregulation of muscle tone)
- Seizures and neurologic findings (e.g., roving eye movements, hypotonia, dystonia) and/or systemic signs (e.g., respiratory distress, anemia, failure to gain weight, abdominal distention, poor feeding)
- Cryptogenic infantile or epileptic spasms (i.e., an underlying cause is assumed, but not proven)
Late-onset PNPO deficiency (i.e., onset after age 28 days) in individuals of any age. Cryptogenic seizures refractory to common anticonvulsants
Standardized Vitamin B6 Trial
A standardized vitamin B6 trial [Wilson et al 2019] may suggest a diagnosis of PNPO deficiency (Figure 1).
- In the 40% of individuals with PNPO deficiency who are pyridoxine (PN) responsive, the majority show cessation of seizures in one to three days; in others amelioration of clinically evident seizures may take several days or may initially be evident on EEG only.
- In the 60% of individuals with PNPO deficiency who are pyridoxal 5'-phosphate (PLP) responsive, the majority show cessation of seizures in one to three days, accompanied by improvement of abnormal EEG findings.
- Note: PN- and/or PLP-responsive seizures can also be indicative of other vitamin B6-dependent or vitamin B6-responsive seizures.
- Measurement of biomarkers can help to distinguish PNPO deficiency from some of these disorders (e.g., increased plasma and urinary alpha-aminoadipic semialdehyde is indicative of pyridoxine-dependent epilepsy – ALDH7A1, and sulfocysteine is indicative of molybdenum cofactor deficiency or isolated sulfite oxidase deficiency).
- There is no biomarker for PLPHP deficiency (also referred to as PLPBP or PROSC deficiency).
- While simultaneous EEG recording is informative, it may not be practical as improvement may take hours to days.
Note: In the event of a favorable response to either PLP or PN, administration should be continued until results of biomarkers and genetic testing are available (see Establishing the Diagnosis).
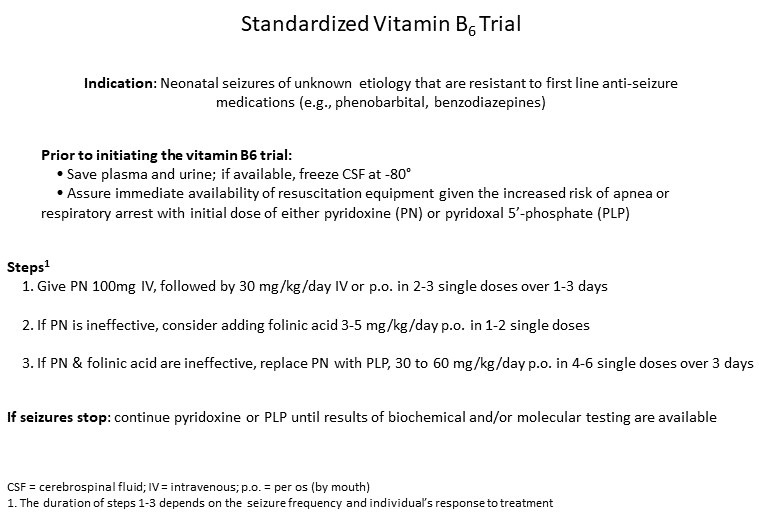
Figure 1.
Stages of a standardized vitamin B6 trial
Supportive Laboratory Findings
Cerebrospinal fluid and plasma PLP concentrations, in most instances when reported, are below the reference range prior to administration of PN or PLP. See Table 1 (pdf).
Family History
Family history is consistent with autosomal recessive inheritance (e.g., affected sibs and/or parental consanguinity). Absence of a known family history does not preclude the diagnosis.
Note: (1) Sibs with seizures, epileptic encephalopathy, and/or epilepsy attributed to birth trauma or prematurity should be reevaluated when subsequent sibs have a similar presentation. (2) Families with pathogenic variants segregating with autosomal recessive epileptic encephalopathy may have a history of infertility and miscarriage [Mills et al 2014].
Treatment with pharmacologic doses of PLP or PN should be continued (see Management, Targeted Therapy) in individuals with a positive clinical or EEG response to the standardized vitamin B6 trial pending definitive diagnosis (see Establishing the Diagnosis).
Establishing the Diagnosis
The diagnosis of PNPO deficiency is established in a proband with suggestive findings typically by molecular genetic testing or, where available, by enzyme analysis.
Molecular Genetic Testing
The molecular diagnosis of PNPO deficiency is established in a proband with biallelic pathogenic (or likely pathogenic) variants in PNPO identified by molecular genetic testing (see Table 2).
Note: (1) Per ACMG/AMP variant interpretation guidelines, the terms "pathogenic variant" and "likely pathogenic variant" are synonymous in a clinical setting, meaning that both are considered diagnostic and can be used for clinical decision making [Richards et al 2015]. Reference to "pathogenic variants" in this GeneReview is understood to include any likely pathogenic variants. (2) Identification of biallelic PNPO variants of uncertain significance (or of one known PNPO pathogenic variant and one PNPO variant of uncertain significance) does not itself establish or rule out the diagnosis. (See Molecular Pathogenesis, PNPO-specific laboratory technical considerations for more information.)
Molecular genetic testing approaches can include a combination of gene-targeted testing (multigene panel) and comprehensive genomic testing (exome sequencing, genome sequencing).
Gene-targeted testing requires that the clinician determine which gene(s) are likely involved, whereas genomic testing does not. Individuals with the distinctive findings described in Suggestive Findings may be more likely to be diagnosed using gene-targeted testing (see Option 1), whereas those in whom the diagnosis of a seizure disorder caused by an inborn error of metabolism has not been considered are more likely to be diagnosed using genomic testing (see Option 2).
Option 1
A multigene panel (e.g., comprehensive epilepsy panel, infantile epilepsy panel, or epileptic encephalopathy panel) that includes PNPO and other genes of interest (see Differential Diagnosis) is most likely to identify the genetic cause of the condition while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests.
For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
Option 2
When the diagnosis of PNPO deficiency has not been considered because an individual has atypical clinical findings, comprehensive genomic testing (which does not require the clinician to determine which gene is likely involved) can be considered. Exome sequencing is most commonly used; genome sequencing is also possible.
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 2.
Molecular Genetic Testing Used in PNPO Deficiency
PNPO Enzyme Activity
Diagnosis of PNPO deficiency, irrespective of treatment status, can be confirmed by analysis of PNPO enzyme activity in dried blood spots [Wilson et al 2017]. (If not clinically available, see Chapter Notes, Author Notes for more information.)
Clinical Characteristics
Clinical Description
As of 2022, approximately 90 individuals have been identified with pyridox(am)ine 5'-phosphate oxidase (PNPO) deficiency based on the identification of biallelic pathogenic variants in PNPO.
The following description of the phenotypic features of PNPO deficiency is based on these reports [Levtova et al 2015, Mercimek-Mahmutoglu et al 2015, Raimondi et al 2015, Veeravigrom et al 2015, Jaeger et al 2016, di Salvo et al 2017, Fung et al 2017, Guerriero et al 2017, Olson et al 2017, Xue et al 2017, Borst & Tchapyjnikov 2018, Fathalla et al 2018, Kvarnung et al 2018, Wilson et al 2019, Mohanlal et al 2020, Alghamdi et al 2021, Jiao et al 2022]. Levtova et al [2015] includes a review of all publications up to 2015. Alghamdi et al [2021] also includes a review of all publications up to 2021; some affected individuals included in subsequent follow-up reports may have been counted more than once.
Note that the clinical presentations of PNPO deficiency, ALDH7A1 deficiency, and PLPHP deficiency (also referred to as PLPBP or PROSC deficiency) are indistinguishable (see Differential Diagnosis).
The spectrum of the PNPO deficiency phenotype ranges from classic (i.e., neonatal-onset seizures) to late-onset seizures (i.e., manifesting after the neonatal period), which can be distinguished by age of onset and seizure patterns.
Classic PNPO deficiency (89% of affected individuals) is characterized by high seizure frequency and status epilepticus. The vast majority of these infants have seizures before age two weeks, with 30% presenting on day one of life.
In about 10% of pregnancies, rhythmic fetal movements have been reported in the last trimester, suggesting intrauterine seizure onset.
In newborns, seizures caused by PNPO deficiency can be confused with seizures associated with birth asphyxia as a result of prematurity (reported in about 64% of infants) and fetal distress (reported in about 15% of infants).
Seizures are typically resistant to common anti-seizure medications. Seizure semiology varies from myoclonic to clonic or tonic seizures.
To date, epileptic spasms (ES) have been reported in seven infants with classic PNPO deficiency. In four infants ES was the presenting seizure type (within the first 24 hours of life); three infants who had onset of focal seizures before age one month subsequently developed ES and other seizure types (generalized tonic/clonic/tonic-clonic and focal seizures). EEG records on six individuals showed hypsarrhythmia in three, atypical hypsarrhythmia in two, and burst suppression in one; see Fung et al [2017] (Patient 55); Jiao et al [2022].
Affected individuals may show episodes of roving eye, head movements without ictal EEG patterns, and signs of encephalopathy such as hyperalertness and inconsolable crying [Schmitt et al 2010] (full text; see especially supporting information Video S4).
About 60% of individuals with PNPO deficiency have developmental impairment, affecting speech, cognition, and behavior; some have neurologic impairment such as muscular hypotonia or dystonia. Severe neurodevelopmental impairment is more likely to occur in individuals with PNPO deficiency who experienced diagnostic delay and prolonged periods of uncontrolled seizures.
Other organ involvement. Systemic findings may include respiratory distress, vomiting, abdominal distention, hepatomegaly, and failure to gain weight. Routine laboratory investigations may show anemia, hypoglycemia, elevated plasma lactate, metabolic acidosis, and/or coagulopathy.
The observation of older deceased sibs (with manifestations consistent with PNPO deficiency) in families of probands with PNPO deficiency suggests that the mortality rate of untreated PNPO deficiency is high.
Late-onset seizures (i.e., manifesting after the neonatal period) have been reported to date in eight individuals from seven unrelated families [Mills et al 2014, di Salvo et al 2017, Xue et al 2017, Kvarnung et al 2018].
In the report by Mills et al [2014], Patient 7 had onset of infantile spasms at age five months with hypsarrhythmia on EEG.
In the report of Xue et al [2017]:
- Patient 3 had an afebrile seizure at age five months and gradually developed therapy-resistant epilepsy and developmental delay;
- Patient 4 had episodic stiffening at age 40 days that increased to daily seizures by age ten months, controlled by a combination of valproate and topiramate.
In the report of di Salvo et al [2017]:
- Patient 1 had focal clonic status epilepticus at age 20 months;
- Patient 2 had myoclonic atonic as well as generalized tonic-clonic seizures starting at age three years and two months (diagnosed as myoclonic atonic epilepsy with developmental decline);
- Patient 3 had episodic stiffening (clustering during febrile episodes) starting at age eight months, subsequent mild cognitive impairment, and occasional seizures while on valproic acid monotherapy.
In the report of Kvarnung et al [2018], two brothers had seizure onset at age eight months; no other details were provided.
Prognosis. In the absence of specific treatment with vitamin B6, individuals with classic PNPO deficiency may experience early death. Preterm babies are at higher risk for developmental delay (84%) compared to term babies (50%). In the presence of neonatal-onset seizures, shorter treatment delay (<4 weeks) is clearly correlated with better outcomes. Seizure onset beyond the neonatal period appears to have a better prognosis. About 40% of all individuals with PNPO deficiency reported to date have a sustained favorable response to pyridoxine (PN). PN response has been observed in individuals with neonatal-onset seizures and is even more likely in individuals with late-onset seizures [Mills et al 2014, Plecko et al 2014].
Detailed EEG records available for 41 individuals with PNPO deficiency (classic and late onset) revealed the following:
- Seventeen individuals had burst suppression patterns prior to the administration of PLP or PN.
- Seventeen individuals demonstrated a pattern of multifocal or bilateral epileptic discharges.
- Three individuals had hypsarrhythmia.
- Four individuals had a normal EEG.
Cranial imaging reports, available for 40% of all individuals with PNPO deficiency (including 28 MRI results, one CT, and one cranial ultrasound) revealed the following:
- Fifteen individuals had normal initial imaging studies; on follow up, three individuals had brain atrophy or delayed myelination.
- Fifteen individuals had abnormal initial MRIs ranging from increased brain edema, signal intensity of basal ganglia or white matter, delayed myelination, intraventricular hemorrhage or middle cerebral artery infarction to simplified gyral patterns with shallow sulci.
Alghamdi et al [2021] reviewed MRI data of 55 individuals with classic and late-onset PNPO deficiency, some of whom were counted twice, with follow-up reports also included. Of these, 34 had a normal brain MRI, eight had brain atrophy, three had ischemic changes or leukomalacia, and three had delayed myelination.
Genotype-Phenotype Correlations
No genotype-phenotype correlations have been reported.
Nonetheless, the following observations about PN responsiveness may be helpful in guiding clinical management. See Table 5 for details.
- Seizures in individuals homozygous for the variant c.674G>A;p.Arg225His may respond to treatment with PN [Mills et al 2014, Plecko et al 2014].
- The seizures of four of the seven individuals reported to be homozygous or compound heterozygous for the variant c.98A>T;p.Asp33Val responded to treatment with PN [Wilson et al 2019].
- The majority of individuals who are homozygous for the variant c.347G>A;p.Arg116Gln, which may be present alongside other homozygous or compound heterozygous PNPO pathogenic variants (i.e., have a total of two or three pathogenic variants), have late-onset seizures that responded to treatment with PN [Mills et al 2014, di Salvo et al 2017]. See also Molecular Pathogenesis, PNPO-specific laboratory technical considerations.
Studies suggest that affected individuals with some variants (e.g., c.685C>T;p.Arg229Trp) that affect the flavin-binding site may benefit from riboflavin therapy in addition to PN and/or PLP therapy [Musayev et al 2009].
Penetrance
Not all individuals homozygous for the variant p.Arg116Gln develop seizures [Wilson et al 2019].
Nomenclature
PN- and PLP-responsive seizures (see Differential Diagnosis) are diagnosed in children who have not had molecular confirmation of PNPO deficiency, ALDH7A1 deficiency, or PLPHP deficiency * and who have either:
- Intractable seizures for which seizure control is only partially improved with the addition of PN or PLP; or
- Seizures that do not recur after PN or PLP is withdrawn.
* Pyridoxine-dependent epilepsy caused by pathologic variants in PLPBP is also referred to as PLPHP deficiency (PLPHP is the abbreviation for the protein encoded by PLPBP, the pyridoxal phosphate homeostasis protein).
Prevalence
As of 2022, approximately 90 individuals have been identified with biallelic pathogenic variants in PNPO [Levtova et al 2015, Mercimek-Mahmutoglu et al 2015, Raimondi et al 2015, Veeravigrom et al 2015, Jaeger et al 2016, di Salvo et al 2017, Fung et al 2017, Guerriero et al 2017, Olson et al 2017, Xue et al 2017, Kvarnung et al 2018, Mohanlal et al 2020, Alghamdi et al 2021, Jiao et al 2022]. Of note, some individuals have been reported more than once.
Variants found commonly in specific populations include the following (see Table 5 for details):
- The variant c.674G>A;p.Arg225His has been reported in several individuals from the former Yugoslavia and additional individuals of southeastern European ancestry [Plecko et al 2014, Lugli et al 2019].
- Individuals from the United Arab Emirates and one individual from Qatar were homozygous for c.674G>T;p.Arg225Leu [Guerriero et al 2017].
- The c.448_451delCCTG variant may be of high prevalence in individuals from China [Xue et al 2017, Jiao et al 2022].
Genetically Related (Allelic) Disorders
No phenotypes other than those discussed in this GeneReview are known to be associated with germline pathogenic variants in PNPO.
Differential Diagnosis
PNPO deficiency must be distinguished from ALDH7A1 deficiency and PLPHP deficiency (also referred to as PLPBP deficiency), as well as other disorders associated with pyridoxine (PN)- and pyridoxal 5'-phosphate (PLP)-responsive seizures (see Table 3).
Table 3.
Selected Disorders of Interest in the Differential Diagnosis of PNPO Deficiency
Note: In the Far East, PLP has been used as an anticonvulsant when anti-seizure medications have failed, and to control seizures in children with infantile spasms and generalized and focal epilepsy in cohorts that had not undergone molecular genetic testing [Ohtahara et al 1993, Nakagawa et al 1997, Ito et al 2000, Wang et al 2005, Ohtahara et al 2011]. Specifically, PLP responsiveness was reported in 20.2% of 119 individuals with West syndrome of unknown etiology and 10.7% of individuals with West syndrome of known etiology, such as birth asphyxia or brain malformation [Ohtahara et al 2011], and PLP or PN responsiveness was reported in 11.7% of 94 children with idiopathic intractable epilepsy, including West syndrome [Wang et al 2005]. (Note: International guidelines do not generally recommend a standardized trial of PN or PLP in infants with infantile spasms; however, recently consideration of a therapeutic trial with PN or PLP has been proposed in children with West syndrome when infantile spasms are associated with other seizure types or have started before age two months [Gibaud et al 2021].)
Other Considerations in the Differential Diagnosis of PNPO Deficiency
Inborn pyridoxine dependency states. While other inborn pyridoxine dependency states have been described – for example, pyridoxine-dependent anemia and pyridoxine-dependent forms of homocystinuria (see Homocystinuria Caused by Cystathionine Beta-Synthase Deficiency), xanthurenic aciduria (OMIM 236800), and cystathioninuria (OMIM 219500) – these conditions are not genetically related to pyridoxine-dependent epilepsy and are phenotypically distinct disorders.
Nonketotic hyperglycinemia (NKH). Similar to seizures in infants with NKH, seizures in infants with PNPO deficiency commence within the first few days of life and may be associated with a burst suppression pattern alongside elevated plasma and cerebrospinal fluid glycine. However, seizures associated with NKH do not respond to vitamin B6, and it appears that the CSF glycine / plasma glycine ratio in PNPO deficiency is not as high as in NKH [Mills et al 2005].
Mitochondrial disorders. PNPO deficiency may present with lactic acidosis. Lactate acid elevation can be an important, albeit nonspecific, marker of mitochondrial disease and mislead clinicians toward other less treatable inborn errors of metabolism.
Hypoxic ischemic encephalopathy (HIE). About 15% of individuals with PNPO deficiency have fetal distress followed by poor adaptation and low APGAR scores. This presentation can mislead clinicians toward symptomatic seizures as a sign of HIE. Resistance to common anticonvulsants, a history of prematurity, and severely pathologic or persistent EEG changes should lead to reevaluation for genetic causes of neonatal seizures.
Acquired epilepsy as a result of impaired PLP availability or synthesis. Certain drugs (see Possible Drug Interactions) can bind to and inactivate PLP. Other compounds that can affect PLP synthesis include pyridoxal kinase inhibitors such as 4-O-methyl pyridoxine in Ginkgo nuts [Hasegawa et al 2006] and aminophylline [Glenn et al 1995].
Management
No clinical practice guidelines for pyridox(am)ine 5'-phosphate oxidase (PNPO) deficiency have been published; however, these are currently being formulated by an international PNPO consortium [Author, personal observation].
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with PNPO deficiency, the evaluations summarized in this section (if not performed as part of the evaluation that led to the diagnosis) are recommended.
For classic and late-onset PNPO deficiency
- Neurologic examination to evaluate eye movement and muscle tone (for hypotonia or rigidity), and to describe seizure semiology
- EEG including sleep and wake cycles (preferably with a recording time of two hours) beginning at the time of seizure onset
- Physical examination including measurement of weight, length, and head circumferenceand evaluation of liver involvement by determination of transaminases, liver function tests, and abdominal ultrasound
- Consultation with a medical geneticist, certified genetic counselor, or certified advanced genetic nurse to inform affected individuals and their families about the nature, mode of inheritance, and implications of PNPO deficiency in order to facilitate medical and personal decision making
For late-onset PNPO deficiency
- Developmental/educational assessment using age-appropriate standardized testing
- Brain MRI in individuals with abnormal development
Treatment of Manifestations
Targeted Therapy
In GeneReviews, a targeted therapy is one that addresses the specific underlying mechanism of disease causation (regardless of whether the therapy is significantly efficacious for one or more manifestation of the genetic condition); would otherwise not be considered without knowledge of the underlying genetic cause of the condition; or could lead to a cure. —ED
The two forms of vitamin B6 used in treating PNPO deficiency are pyridoxal 5'-phosphate (PLP) and pyridoxine (PN). About 60% of individuals with PNPO deficiency are resistant to PN and require treatment with PLP; about 40% respond to PN alone.
Note: Because severe apnea and respiratory insufficiency as well as prolonged somnolence can occur with the first administration of either form of vitamin B6, affected infants should be treated initially and monitored in a neonatal intensive care unit over the first three days of high-dose supplementation of either form of vitamin B6.
Individuals with PNPO deficiency will need lifelong treatment with PLP or PN.
Pyridoxal 5'-phosphate (PLP) is the active form of vitamin B6. Individuals with classic PNPO deficiency receive 30-60 mg/kg/day PLP orally, divided into four to six single doses [Mills et al 2014]. The lowest effective PLP dose should be used.
PLP is only available as a non-licensed compound outside of Asia. Because PLP is a photosensitive compound that can rapidly degrade when in solution, it should only be dissolved immediately prior to administration to avoid buildup of photochemical degradation products [Mohamed-Ahmed et al 2017].
In contrast to PN, there is no FDA statement on a safety limit for PLP.
PLP side effects include possible liver toxicity, which has been observed in a few individuals with PNPO deficiency. While Porri et al [2014] reported mild elevation of transaminases in an individual treated with 50 mg/kg/day of PLP, two individuals were reported with liver cirrhosis at age four years and eight years, respectively, following long-term use of PLP in doses ranging from 50 mg/kg/day to 100 mg/kg/day because of instability of their epilepsy [Sudarsanam et al 2014, Coman et al 2016].
One adolescent underwent liver transplantation at age 15 years because of hepatocellular carcinoma [Webster et al 2021].
Because of this reported toxicity, it may be reasonable to avoid high doses of PLP by adding anti-seizure medications (ASMs) in those patients who do not become seizure free or do not remain seizure free on PLP monotherapy, especially in the presence of elevated transaminases. Likewise, in persons who are PLP dependent who have recurrent seizures, it may be necessary to modify/adjust the dose to weight [Authors, personal experience].
Although PLP inhibits platelet function, no bleeding diathesis has been reported with its use in PNPO deficiency, except in one boy with both PNPO deficiency and mild hemophilia A (factor VIII activity of 14%) [Borst & Tchapyjnikov 2018].
Pyridoxine (PN). Individuals clinically responsive to PN should receive 30 mg/kg/day of PN (up to a total dose of 300 mg/day or, if needed, 500 mg/day) intravenously or orally in three to four single doses [Mills et al 2014, Plecko et al 2014, Ware et al 2014]. Doses rarely exceed 500 mg/day, and modification over time is rarely warranted [Authors, personal experience].
PN side effects can include sensory (or motor) neuropathy, which is usually reversible with dose reduction.
Folinic acid. In neonates who show some reduction of seizures on PN or PLP supplementation but do not become seizure free, administration of 3-5 mg/kg/day of folinic acid intravenously or orally may have additive beneficial effects because of the overlapping cofactor function of PLP and folinic acid derivatives.
Riboflavin. Individuals with PNPO variants affecting the flavin mononucleotide binding site may also benefit from supplementation with 100-200 mg/day of oral riboflavin. See Genotype-Phenotype Correlations.
Other. Absence of seizures in an individual treated with PN does not require a change to PLP. In some individuals with PNPO deficiency who respond to treatment with PN, seizure recurrence and even status epilepticus have been observed when treatment is switched from PN to PLP [Mills et al 2014, Plecko et al 2014, Ware et al 2014].
Seizures can recur during febrile episodes and/or with delayed or missed doses.
To cover their overnight sleep, some individuals need higher doses in the evening (e.g., 30%-35% of the total daily dose).
Individuals who have become seizure free on vitamin B6 therapy may be slowly tapered off conventional ASMs, as only about 15% of individuals with PNPO deficiency need ASMs in addition to vitamin B6 therapy. While carbamazepine and levetiracetam have been used successfully [B Plecko, personal experience], data are too sparse to state which ASMs would be most helpful.
Possible Drug Interactions
D-cycloserine can act as a pyridoxine antagonist and increases renal excretion of pyridoxine [Donald 2010, Kuhrau et al 2023].
PLP interacts with various small molecules:
- PLP undergoes a condensation reaction with hydrazines, leading to an increased requirement for vitamin B6 in individuals taking drugs such as hydralazine and isoniazid [Biehl & Vilter 1954, Standal et al 1974, Snider 1980, Wason et al 1981, Shigetomi & Kuchel 1993, Alvarez & Guntupalli 1995, Donald & McIlleron 2009].When an individual with PNPO deficiency needs treatment with either hydralazine (an antihypertensive medication) or isoniazid (a tuberculostatic drug), the respective dose of PLP or PN may need to be increased. When the actual dose of vitamin B6 supplementation is low, the increase in the dose could be done as a precaution; however, when the actual dose of vitamin B6 supplementation is high, increasing the dose should only be considered if seizure frequency increases.
- PLP can also react with -SH groups such as that in penicillamine [Tu et al 1964, Rumsby & Shepherd 1979, Matsui & Rozovski 1982].
PN and presumably also PLP supplementation antagonizes the therapeutic effect of L-dopa.
Supportive Care
Supportive care often includes specialists in multiple disciplines, including neurology, developmental pediatrics, speech-language therapy, physical therapy, and occupational therapy.
Developmental Delay / Intellectual Disability Management Issues
The following information represents typical management recommendations for individuals with developmental delay / intellectual disability in the United States; standard recommendations may vary from country to country.
Ages 0-3 years. Referral to an early intervention program is recommended for access to occupational, physical, speech, and feeding therapy as well as infant mental health services, special educators, and sensory impairment specialists. In the US, early intervention is a federally funded program available in all states that provides in-home services to target individual therapy needs.
Ages 3-5 years. In the US, developmental preschool through the local public school district is recommended. Before placement, an evaluation is made to determine needed services and therapies and an individualized education plan (IEP) is developed for those who qualify based on established motor, language, social, or cognitive delay. The early intervention program typically assists with this transition. Developmental preschool is center based; for children too medically unstable to attend, home-based services are provided.
All ages. Consultation with a developmental pediatrician is recommended to ensure the involvement of appropriate community, state, and educational agencies (US) and to support parents in maximizing quality of life. Some issues to consider:
- IEP services:
- An IEP provides specially designed instruction and related services to children who qualify.
- IEP services will be reviewed annually to determine whether any changes are needed.
- Special education law requires that children participating in an IEP be in the least restrictive environment feasible at school and included in general education as much as possible, when and where appropriate.
- PT, OT, and speech services will be provided in the IEP to the extent that the need affects the child's access to academic material. Beyond that, private supportive therapies based on the affected individual's needs may be considered. Specific recommendations regarding type of therapy can be made by a developmental pediatrician.
- As a child enters the teen years, a transition plan should be discussed and incorporated in the IEP. For those receiving IEP services, the public school district is required to provide services until age 21.
- A 504 plan (Section 504: a US federal statute that prohibits discrimination based on disability) can be considered for those who require accommodations or modifications such as front-of-class seating, assistive technology devices, classroom scribes, extra time between classes, modified assignments, and enlarged text.
- Developmental Disabilities Administration (DDA) enrollment is recommended. DDA is a US public agency that provides services and support to qualified individuals. Eligibility differs by state but is typically determined by diagnosis and/or associated cognitive/adaptive disabilities.
- Families with limited income and resources may also qualify for supplemental security income (SSI) for their child with a disability.
Motor Dysfunction
Gross motor dysfunction. For individuals with delays in gross motor function, physical therapy is recommended to maximize mobility and to reduce the risk for later-onset orthopedic complications (e.g., contractures, scoliosis, hip dislocation). Individuals with dystonia may need additional medication as per their treating neurologist.
Fine motor dysfunction. Occupational therapy is recommended for difficulty with fine motor skills that affect adaptive function such as feeding, grooming, dressing, and writing.
Oral motor dysfunction should be assessed at each visit and clinical feeding evaluations and/or radiographic swallowing studies should be obtained for choking/gagging during feeds, poor weight gain, frequent respiratory illnesses or feeding refusal that is not otherwise explained.
Communication issues. As expressive language difficulties are common in PNPO deficiency, consider evaluation by a speech-language therapist. The evaluation will consider cognitive abilities and sensory impairments to determine the most appropriate form of speech therapy. This may include alternative means of communication (e.g., augmentative and alternative communication [AAC]) AAC devices can range from low-tech, such as picture exchange communication, to high-tech, such as voice-generating devices. Contrary to popular belief, AAC devices do not hinder verbal development of speech, but rather support optimal speech and language development.
Social/Behavioral Concerns
Children may qualify for and benefit from interventions used in treatment of autism spectrum disorder, including applied behavior analysis (ABA). ABA therapy is targeted to the individual child's behavioral, social, and adaptive strengths and weaknesses and typically performed one on one with a board-certified behavior analyst.
Consultation with a developmental pediatrician may be helpful in guiding parents through appropriate behavior management strategies or providing prescription medications, such as medication used to treat attention-deficit/hyperactivity disorder, when necessary.
Concerns about serious aggressive or destructive behavior can be addressed by a pediatric psychiatrist.
Surveillance
Table 4.
Recommended Surveillance for Individuals with PNPO Deficiency
Agents/Circumstances to Avoid
Several anti-seizure medications (such as carbamazepine, valproate, phenytoin, and phenobarbital) can cause a low plasma concentration of PLP [Footitt et al 2011].
Evaluation of Relatives at Risk
Prenatal testing of a fetus at risk. If the PNPO pathogenic variants have been identified in an affected family member, prenatal molecular genetic testing may be performed via amniocentesis or chorionic villus sampling on future pregnancies at risk (see Pregnancy Management). This will allow precise counseling for maternal pyridoxine supplementation during pregnancy and postnatal treatment of the newborn.
When prenatal testing has not been performed on a pregnancy at risk, prompt evaluation of the newborn is essential to determine if treatment with PN or PLP is necessary. While pending results of molecular genetic testing, two options for management of an at-risk newborn are:
- Prophylactic treatment with either PN or PLP (whichever was effective in the affected sib) until molecular genetic testing clarifies whether or not the newborn is affected. A note of caution: at least one newborn at risk for ALDH7A1-related pyridoxine-dependent epilepsy developed status epilepticus after being given high-dose PN treatment before molecular genetic testing determined that the child was not affected [Hartmann et al 2011].
- Clinical and EEG monitoring with initiation of treatment with PN or PLP (whichever was effective in the affected sib) at the first sign of seizures or encephalopathy.
Symptomatic younger sib. If a younger sib (without prior molecular genetic testing) of a proband presents with encephalopathy or a non-febrile seizure, PN or PLP (depending on the drug to which the proband responded) should be administered acutely (ideally under EEG monitoring) for both diagnostic and therapeutic purposes. Note: It would be unlikely for the proband's older sibs who have not experienced seizures to have PNPO deficiency.
Pregnancy Management
As recurrence risk for couples who have had a child with PNPO deficiency is 25%, there has been discussion about the utility of empiric supplementation of PN during pregnancies in women carrying an at-risk fetus. In contrast to reports on PN supplementation in pregnancies at risk for pyridoxine-dependent epilepsy – ALDH7A1, the literature on vitamin B6 supplementation in pregnancies at risk for PNPO deficiency is limited. In one case report, the mother of a fetus with molecularly confirmed PNPO deficiency took a multivitamin containing 2.6 mg/day of PN throughout pregnancy (recommended daily allowance for PN for women during pregnancy is 1.9 mg/day), and PLP (dose not specified) for the last three days of pregnancy. At birth the infant was immediately started on PLP therapy; neurodevelopment was reported as normal at age 2.5 years [Hatch et al 2016]. In two pregnancies, mothers were treated with 10 mg/day of PN [Peter Clayton, personal communication]; no details on timing of therapy or fetal outcome are available.
Based on the Hatch et al [2016] case report and the data on prenatal vitamin B6 supplementation of women carrying a fetus with pyridoxine-dependent epilepsy – ALDH7A1, the authors suggest considering empiric supplementation with PN (50-100 mg/day) during the last 20 weeks of a pregnancy with a fetus at risk for PNPO deficiency or known to have PNPO deficiency based on prenatal testing for the family-specific PNPO pathogenic variants. PN supplementation is recommended rather than PLP, as the mother, who is heterozygous for PNPO deficiency, has a 50% capacity to form PLP out of PN, and the risk of hepatotoxicity of PLP in pregnancy is unknown.
Therapies Under Investigation
Search ClinicalTrials.gov in the US and EU Clinical Trials Register in Europe for access to information on clinical studies for a wide range of diseases and conditions. Note: There may not be clinical trials for this disorder.
Genetic Counseling
Genetic counseling is the process of providing individuals and families with information on the nature, mode(s) of inheritance, and implications of genetic disorders to help them make informed medical and personal decisions. The following section deals with genetic risk assessment and the use of family history and genetic testing to clarify genetic status for family members; it is not meant to address all personal, cultural, or ethical issues that may arise or to substitute for consultation with a genetics professional. —ED.
Mode of Inheritance
Pyridox(am)ine 5'-phosphate oxidase (PNPO) deficiency is inherited in an autosomal recessive manner.
Risk to Family Members
Parents of a proband
- The parents of an affected child are presumed to be heterozygous for a PNPO pathogenic variant.
- Molecular genetic testing is recommended for the parents of a proband to confirm that both parents are heterozygous for a PNPO pathogenic variant and to allow reliable recurrence risk assessment.
- If a pathogenic variant is detected in only one parent and parental identity testing has confirmed biological maternity and paternity, it is possible that one of the pathogenic variants identified in the proband occurred as a de novo event in the proband or as a postzygotic de novo event in a mosaic parent [Jónsson et al 2017]. If the proband appears to have homozygous pathogenic variants (i.e., the same two pathogenic variants), additional possibilities to consider include:
- A single- or multiexon deletion in the proband that was not detected by sequence analysis and that resulted in the artifactual appearance of homozygosity;
- Uniparental isodisomy for the parental chromosome with the pathogenic variant that resulted in homozygosity for the pathogenic variant in the proband.
- Heterozygotes (carriers) are asymptomatic and are not at risk of developing the disorder.
Sibs of a proband
- If both parents are known to be heterozygous for a PNPO pathogenic variant, each sib of an affected individual, irrespective of sex, has at conception a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier.
- Heterozygotes (carriers) are asymptomatic and are not at risk of developing the disorder.
Offspring of a proband
- The offspring of an individual with PNPO deficiency will be obligate heterozygotes (carriers) for a pathogenic variant in PNPO.
- If an individual with PNPO deficiency has children with an individual who is heterozygous for a PNPO pathogenic variant, offspring are at a 50% risk of being affected by PNPO deficiency. The carrier frequency of PNPO deficiency in the general population is unknown. Genetic counseling and PNPO molecular genetic testing of the unaffected reproductive partner may be warranted.
- Note: The fertility status of adults with PNPO deficiency is not known and there have been no published reports about offspring of affected individuals.
Other family members. Each sib of the proband's parents is at a 50% risk of being a carrier of a PNPO pathogenic variant.
Carrier Detection
Carrier testing for at-risk relatives requires prior identification of the PNPO pathogenic variants in the family.
Related Genetic Counseling Issues
See Management, Evaluation of Relatives at Risk for information on evaluating at-risk relatives for the purpose of early diagnosis and treatment.
Family planning
- The optimal time for determination of genetic risk and discussion of the availability of prenatal/preimplantation genetic testing is before pregnancy.
- As the recurrence risk for couples who have a child with PNPO deficiency is 25%, the parents should receive counseling regarding maternal vitamin B6 supplementation in future pregnancies (see Pregnancy Management).
- It is appropriate to offer genetic counseling (including discussion of potential risks to offspring and reproductive options) to young adults who are affected, are carriers, or are at risk of being carriers.
Prenatal Testing and Preimplantation Genetic Testing
Once the PNPO pathogenic variants have been identified in an affected family member, prenatal and preimplantation genetic testing are possible.
Differences in perspective may exist among medical professionals and within families regarding the use of prenatal testing. While most centers would consider use of prenatal testing to be a personal decision, discussion of these issues may be helpful.
Resources
GeneReviews staff has selected the following disease-specific and/or umbrella support organizations and/or registries for the benefit of individuals with this disorder and their families. GeneReviews is not responsible for the information provided by other organizations. For information on selection criteria, click here.
- American Epilepsy Society
- Epilepsy FoundationPhone: 301-459-3700Fax: 301-577-2684
- Metabolic Support UKUnited KingdomPhone: 0845 241 2173
Molecular Genetics
Information in the Molecular Genetics and OMIM tables may differ from that elsewhere in the GeneReview: tables may contain more recent information. —ED.
Table A.
PNPO Deficiency: Genes and Databases
Table B.
OMIM Entries for PNPO Deficiency (View All in OMIM)
Molecular Pathogenesis
Vitamin B6, present in the human diet in various forms, is converted to pyridoxal 5'-phosphate (PLP), which acts as a cofactor for various enzymes, including those involved in the synthesis and degradation of some neurotransmitters present in the brain. This conversion involves several enzymatic steps, one of which oxidizes pyridoxamine phosphate (PMP) and pyridoxine phosphate (PNP) to PLP, catalyzed by pyridox(am)ine 5'-phosphate oxidase (PNPO).* Pathogenic variants in PNPO cause a reduction in PNPO enzyme activity, resulting in insufficient amounts of PLP for the enzymes for which it is a necessary cofactor. Because of the vital role of PLP in neurotransmitter metabolism, PLP deficiency manifests as a vitamin B6-dependent epilepsy, usually of early onset.
* Note: The enzyme encoded by PNPO may be referred to as "pyridox(am)ine 5'-phosphate oxidase" or "pyridoxine-5'-phosphate oxidase." "Pyridox(am)ine 5'-phosphate oxidase" is preferred because it indicates that the enzyme can also use pyridoxamine 5'-phosphate as a substrate – as well as pyridoxine 5'-phosphate.
Mechanism of disease causation. Loss of function
PNPO-specific laboratory technical considerations. Clinicians and laboratories need to note that some individuals with PNPO deficiency can be homozygous for the variant p.Arg116Gln and homozygous or compound heterozygous for other PNPO pathogenic variants. Thus, these individuals may have two or three PNPO pathogenic variants. When this phenomenon was first observed, p.Arg116Gln was classified as a benign variant in the ClinVar database; however, structural assays by di Salvo et al [2017] and enzyme analysis suggest that it is pathogenic [Wilson et al 2017]. Nevertheless, not all individuals homozygous for the variant p.Arg116Gln develop seizures [Wilson et al 2019], an observation of particular importance when interpreting molecular genetic test results performed in the context of prenatal or preimplantation genetic testing.
Deep intronic variants and intragenic deletions may be missed by sequence analysis that only includes exons and exon/intron boundaries.
The effects of variants of uncertain significance can be assessed by analysis of PNPO enzyme activity in dried blood spots [Wilson et al 2017]. In one individual with only one pathogenic variant identified by Sanger sequencing of genomic DNA and sequencing of cDNA [Raimondi et al 2015], the diagnosis of PNPO deficiency was subsequently confirmed by detection of reduced PNPO enzyme activity in a dried blood spot.
Table 5.
Notable PNPO Pathogenic Variants
Chapter Notes
Author Notes
Dr Barbara Plecko (ta.zarginudem@okcelp.arabrab) and Dr Philippa Mills (ku.ca.lcu@sllim.p) are actively involved in clinical research regarding individuals with PNPO deficiency and other forms of vitamin B6-dependent epilepsy. They would be happy to communicate with individuals who have any questions regarding diagnosis or other considerations.
PNPO enzyme analysis is available in the laboratory of Dr Mills. Contact Dr Mills (ku.ca.lcu@sllim.p) to inquire about enzyme analysis testing or to review PNPO variants of uncertain significance.
Dr Plecko and Dr Mills are also interested in hearing from clinicians treating families affected by vitamin B6-dependent epilepsy in whom no causative variant has been identified through molecular genetic testing of the genes known to be involved in this group of disorders.
Acknowledgments
Dr P Mills is supported by funding from the NIHR Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
Revision History
- 23 June 2022 (bp) Review posted live
- 22 November 2021 (bp) Original submission
References
Literature Cited
- Alghamdi M, Bashiri FA, Abdelhakim M, Adly N, Jamjoom DZ, Sumaily KM, Alghanem B, Arold ST. Phenotypic and molecular spectrum of pyridoxamine-5'-phosphate oxidase deficiency: a scoping review of 87 cases of pyridoxamine-5'-phosphate oxidase deficiency. Clin Genet. 2021;99:99-110. [PMC free article: PMC7820968] [PubMed: 32888189]
- Alvarez FG, Guntupalli KK. Isoniazid overdose: four case reports and review of the literature. Intensive Care Med. 1995;21:641-4. [PubMed: 8522667]
- Biehl JP, Vilter RW. Effects of isoniazid on pyridoxine metabolism. J Am Med Assoc. 1954;156:1549-52. [PubMed: 13211282]
- Borst AJ, Tchapyjnikov D. B 6 and bleeding: a case report of a novel vitamin toxicity. Pediatrics. 2018;141:S430-3. [PMC free article: PMC5877127] [PubMed: 29610166]
- Coman D, Lewindon P, Clayton P, Riney K. PNPO deficiency and cirrhosis: expanding the clinical phenotype? JIMD Rep. 2016;25:71-5. [PMC free article: PMC5059209] [PubMed: 26108646]
- di Salvo ML, Mastrangelo M, Nogués I, Tolve M, Paiardini A, Carducci C, Mei D, Montomoli M, Tramonti A, Guerrini R, Contestabile R, Leuzzi V. Pyridoxine-5'-phosphate oxidase (PNPO) deficiency: clinical and biochemical alterations associated with the c.347g>A (P.Arg116gln) mutation. Mol Genet Metab. 2017;122:135-42. [PubMed: 28818555]
- Donald P, McIlleron H. Chapter 59: Antituberculosis drugs. In: Schaaf HS, Zumla AI, Grange JM, Raviglione MC, Yew WW, Starke JR, Pai M, Donald PR, eds. Tuberculosis: A Comprehensive Clinical Reference. Amsterdam, NL: Elsevier; 2009:608-17.
- Donald PR. Cerebrospinal fluid concentrations of antituberculosis agents in adults and children. Tuberculosis (Edinb). 2010;90:279-92. [PubMed: 20709598]
- Du X, Chen Y, Zhao Y, Luo W, Cen Z, Hao W. Dramatic response to pyridoxine in a girl with absence epilepsy with ataxia caused by a de novo CACNA1A mutation. Seizure. 2017;45:189-91. [PubMed: 28088730]
- Fathalla WM, Al Menhali N, Hosain SA, Ibrahim FH. Clinical and genetic profile of a cohort of pyridoxamine 5-phosphate oxidase deficiency – a single-center experience. Ibnosina J Med Biomed Sci. 2018;10:73-6.
- Footitt EJ, Heales SJ, Mills PB, Allen GF, Oppenheim M, Clayton PT. Pyridoxal 5'-phosphate in cerebrospinal fluid; factors affecting concentration. J Inherit Metab Dis. 2011;34:529-38. [PubMed: 21305354]
- Fung CW, Kwong AK, Wong VC. Gene panel analysis for nonsyndromic cryptogenic neonatal/infantile epileptic encephalopathy. Epilepsia Open. 2017;2:236-43. [PMC free article: PMC5719849] [PubMed: 29588952]
- Gibaud M, Barth M, Lefranc J, Mention K, Villeneuve N, Schiff M, Maurey H, Barthez MA, Caubel I, Chouchane M, Doummar D, Kossorotoff M, Lamblin MD, Roubertie A, Nabbout R, Van Bogaert P. West syndrome is an exceptional presentation of pyridoxine- and pyridoxal phosphate-dependent epilepsy: data from a French cohort and review of the literature. Front Pediatr. 2021;9:621200. [PMC free article: PMC7973036] [PubMed: 33748042]
- Glenn GM, Krober MS, Kelly P, McCarty J, Weir M. Pyridoxine as therapy in theophylline-induced seizures. Vet Hum Toxicol. 1995;37:342-5. [PubMed: 8540225]
- Guerriero RM, Patel AA, Walsh B, Baumer FM, Shah AS, Peters JM, Rodan LH, Agrawal PB, Pearl PL, Takeoka M. Systemic manifestations in pyridox(am)ine 5'-phosphate oxidase deficiency. Pediatr Neurol. 2017;76:47-53. [PMC free article: PMC6008785] [PubMed: 28985901]
- Hartmann H, Fingerhut M, Jakobs C, Plecko B. Status epilepticus in a neonate treated with pyridoxine because of a familial recurrence risk for antiquitin deficiency: pyridoxine toxicity? Dev Med Child Neurol. 2011;53:1150-3. [PubMed: 21707605]
- Hasegawa S, Oda Y, Ichiyama T, Hori Y, Furukawa S. Ginkgo nut intoxication in a 2-year-old male. Pediatr Neurol. 2006;35:275-6. [PubMed: 16996402]
- Hatch J, Coman D, Clayton P, Mills P, Calvert S, Webster RI, Riney K. Normal neurodevelopmental outcomes in PNPO deficiency: a case series and literature review. JIMD Rep. 2016;26:91-7. [PMC free article: PMC4864713] [PubMed: 26303608]
- Ito M, Seki T, Takuma Y. Current therapy for West syndrome in Japan. J Child Neurol. 2000;15:424-8. [PubMed: 10868790]
- Jaeger B, Abeling NG, Salomons GS, Struys EA, Simas-Mendes M, Geukers VG, Poll-The BT. Pyridoxine responsive epilepsy caused by novel homozygous PNPO mutation. Mol Genet Metab Rep. 2016;6:60-63. [PMC free article: PMC4789384] [PubMed: 27014579]
- Jiao X, Gong P, Niu Y, Zhang Y, Yang Z. A rare presentation characterized by epileptic spasms in ALDH7A1, pyridox(am)ine-5'-phosphate oxidase, and PLPBP deficiency. Front Genet. 2022;13:804461. [PMC free article: PMC9039010] [PubMed: 35495162]
- Jiao X, Xue J, Gong P, Wu Y, Zhang Y, Jiang Y, Yang Z. Clinical and genetic features in pyridoxine-dependent epilepsy: a Chinese cohort study. Dev Med Child Neurol. 2020;62:315-21. [PubMed: 31737911]
- Jónsson H, Sulem P, Kehr B, Kristmundsdottir S, Zink F, Hjartarson E, Hardarson MT, Hjorleifsson KE, Eggertsson HP, Gudjonsson SA, Ward LD, Arnadottir GA, Helgason EA, Helgason H, Gylfason A, Jonasdottir A, Jonasdottir A, Rafnar T, Frigge M, Stacey SN, Th Magnusson O, Thorsteinsdottir U, Masson G, Kong A, Halldorsson BV, Helgason A, Gudbjartsson DF, Stefansson K. Parental influence on human germline de novo mutations in 1,548 trios from Iceland. Nature. 2017;549:519-22. [PubMed: 28959963]
- Klotz KA, Lemke JR, Korinthenberg R, Jacobs J. Vitamin B6-responsive epilepsy due to a novel KCNQ2 mutation. Neuropediatrics. 2017;48:199-204. [PubMed: 28420012]
- Kuhrau S, Boykin T, Rech MA. D-cycloserine-induced seizure activity in the emergency department: a case report. J Pharm Pract. 2023;36:716-18. [PubMed: 35109718]
- Kvarnung M, Taylan F, Nilsson D, Anderlid BM, Malmgren H, Lagerstedt-Robinson K, Holmberg E, Burstedt M, Nordenskjöld M, Nordgren A, Lundberg ES. Genomic screening in rare disorders: New mutations and phenotypes, highlighting ALG14 as a novel cause of severe intellectual disability. Clin Genet. 2018;94:528-37. [PubMed: 30221345]
- Levtova A, Camuzeaux S, Laberge AM, Allard P, Brunel-Guitton C, Diadori P, Rossignol E, Hyland K, Clayton PT, Mills PB, Mitchell GA. Normal cerebrospinal fluid pyridoxal 5'-phosphate level in a PNPO-deficient patient with neonatal-onset epileptic encephalopathy. JIMD Rep. 2015;22:67-75. [PMC free article: PMC4486275] [PubMed: 25762494]
- Lugli L, Bariola MC, Ori L, Lucaccioni L, Berardi A, Ferrari F. Further delineation of pyridoxine-responsive pyridoxine phosphate oxidase deficiency epilepsy: report of a new case and review of the literature with genotype-phenotype correlation. J Child Neurol. 2019;34:937-43. [PubMed: 31397616]
- Matsui MS, Rozovski SJ. Drug-nutrient interaction. Clin Ther. 1982;4:423-40. [PubMed: 7046936]
- Mefford HC, Cook J, Gospe Jr SM. Epilepsy due to 20q13.33 subtelomere deletion masquerading as pyridoxine-dependent epilepsy. Am J Med Genet A. 2012;158A:3190-5. [PubMed: 23166088]
- Mercimek-Mahmutoglu S, Sidky S, Hyland K, Patel J, Donner EJ, Logan W, Mendoza-Londono R, Moharir M, Raiman J, Schulze A,2, Siriwardena K, Yoon G, Kyriakopoulou L. Prevalence of inherited neurotransmitter disorders in patients with movement disorders and epilepsy: a retrospective cohort study. Orphanet J Rare Dis. 2015;10:12. [PMC free article: PMC4342151] [PubMed: 25758715]
- Mills PB, Camuzeaux SSM, Footitt EJ, Mills KA, Gissen P, Fisher L, Das KB, Varadkar SM, Zuberi S, McWilliam R, Stödberg T, Plecko B, Baumgartner MR, Maier O, Calvert S, Riney K, Wolf N, Livingston JH, Bala P, Morel CF, Feillet F, Raimondy F, Del Giudice E, Chong WK, Pitt M, Clayton PT. Epilepsy due to PNPO mutations: genotype, environment and treatment affect presentation and outcome. Brain. 2014;137:1350-60. [PMC free article: PMC3999720] [PubMed: 24645144]
- Mills PB, Surtees RAH, Champion MP, Beesley CE, Dalton N, Scambler PJ, Heales SJR, Briddon A, Scheimberg I, Hoffmann GF, Zschocke J, Clayton P. Neonatal epileptic encephalopathy caused by mutations in the PNPO gene encoding pyridox(am)ine 5'-phosphate oxidase. Hum Mol Genet. 2005;14:1077-86. [PubMed: 15772097]
- Mohamed-Ahmed AH, Wilson MP, Albuera M, Chen T, Mills PB, Footitt EJ, Clayton PT, Tuleu C. Quality and stability of extemporaneous pyridoxal phosphate preparations used in the treatment of paediatric epilepsy. J Pharm Pharmacol. 2017;69:480-8. [PubMed: 28220480]
- Mohanlal S, Bindu PS, Sureshbabu S, Kumar S. Variable treatment response in a patient with pyridoxal N phosphate oxidase (PNPO) deficiency - understanding the paradox. Epilepsy Behav Rep. 2020;14:100357. [PMC free article: PMC7210397] [PubMed: 32395712]
- Musayev FN, Di Salvo ML, Saavedra MA, Contestabile R, Ghatge MS, Haynes A, Schirch V, Safo MK. Molecular basis of reduced pyridoxine 5'-phosphate oxidase catalytic activity in neonatal epileptic encephalopathy disorder. J Biol Chem. 2009;284:30949-56. [PMC free article: PMC2781495] [PubMed: 19759001]
- Nakagawa E, Tanaka T, Ohno M, Yamano T, Shimada M. Efficacy of pyridoxal phosphate in treating an adult with intractable status epilepticus. Neurology. 1997;48:1468-9. [PubMed: 9153499]
- Ohtahara S, Ohtsuka Y, Yamatogi Y, Oka E, Yoshinaga H, Sato M. Prenatal etiologies of West syndrome. Epilepsia. 1993;34:716-22. [PubMed: 8330583]
- Ohtahara S, Yamatogi Y, Ohtsuka Y. Vitamin B(6) treatment of intractable seizures. Brain Dev. 2011;33:783-9. [PubMed: 21345627]
- Olson HE, Kelly McK, LaCoursiere CM, Pinsky R, Tambunan D, Shain C, Ramgopal S, Takeoka M, Libenson MH, Julich K, Loddenkemper T, Marsh ED, Segal D, Koh S, Salman MS, Paciorkowski AP, Yang E, Bergin AM, Sheidley BR, Poduri A. Genetics and genotype-phenotype correlations in early onset epileptic encephalopathy with burst suppression. Ann Neurol. 2017;81:419-29. [PMC free article: PMC5366084] [PubMed: 28133863]
- Plecko B, Paul K, Mills P, Clayton P, Paschke E, Maier O, Hasselmann O, Schmiedel G, Kanz S, Connolly M, Wolf N, Struys E, Stockler S, Abela L, Hofer D. Pyridoxine responsiveness in novel mutations of the PNPO gene. Neurology. 2014;82:1425-33. [PMC free article: PMC4001193] [PubMed: 24658933]
- Porri S, Fluss J, Plecko B, Paschkle E, Korff CM, Kern I. Positive outcome following early diagnosis and treatment of pyridox(am)ine 5'-phosphate oxidase deficiency: a case report. Neuropediatrics. 2014;45:64-8. [PubMed: 24297574]
- Raimondi F, Mills Ph, Clayton PT, Del Giudice E. A preterm neonate with seizures unresponsive to conventional treatment. BMJ Case Rep. 2015;2015:bcr2015209743. [PMC free article: PMC4434345] [PubMed: 25979913]
- Reid ES, Williams H, Le Quesne Stabej P, James C, Ocaka L, Bacchelli C, Footitt EJ, Boyd S, Cleary MA, Mills PB, Clayton PT. Seizures due to a KCNQ2 mutation: treatment with vitamin B6. JIMD Rep. 2016;27:79-84. [PMC free article: PMC5580730] [PubMed: 26446091]
- Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405-24. [PMC free article: PMC4544753] [PubMed: 25741868]
- Rumsby PC, Shepherd DM. Effect of penicillamine, hydrallazine and phenelzine on the function of pyridoxal-5'-phosphate [proceedings]. Br J Pharmacol. 1979;67:453P-4P. [PMC free article: PMC2043982] [PubMed: 497570]
- Schmitt B, Baumgartner M, Mills PB, Clayton PT, Jakobs C, Keller E, Wohlrab G. Seizures and paroxysmal events: symptoms pointing to the diagnosis of pyridoxine-dependent epilepsy and pyridoxine phosphate oxidase deficiency. Dev Med Child Neurol. 2010;52:e133-42. [PubMed: 20370816]
- Shigetomi S, Kuchel O. Defective 3,4-dihydroxyphenylalanine decarboxylation to dopamine in hydralazine-treated hypertensive patients may be pyridoxine remediable. Am J Hypertens. 1993;6:33-40. [PubMed: 8427659]
- Snider DE Jr. Pyridoxine supplementation during isoniazid therapy. Tubercle. 1980;61:191-6. [PubMed: 6269259]
- Standal BR, Kao-Chen SM, Yang GY, Char DF. Early changes in pyridoxine status of patients receiving isoniazid therapy. Am J Clin Nutr 1974;27:479-84. [PubMed: 4274683]
- Stenson PD, Mort M, Ball EV, Chapman M, Evans K, Azevedo L, Hayden M, Heywood S, Millar DS, Phillips AD, Cooper DN. The Human Gene Mutation Database (HGMD®): optimizing its use in a clinical diagnostic or research setting. Hum Genet. 2020;139:1197-207. [PMC free article: PMC7497289] [PubMed: 32596782]
- Struys EA, Nota B, Bakkali A, Al Shahwan S, Salomons GS, Tabarki B. Pyridoxine-dependent epilepsy with elevated urinary α-amino adipic semialdehyde in molybdenum cofactor deficiency. Pediatrics. 2012;130:e1716-9. [PubMed: 23147983]
- Sudarsanam A, Singh H, Wilcken B, Stormon M, Arbuckle S, Schmitt B, Clayton P, Earl J, Webster R. Cirrhosis associated with pyridoxal 5'-phosphate treatment of pyridox(am)ine 5´-phosphate oxidase deficiency. JIMD Rep. 2014;17:67-70. [PMC free article: PMC4241198] [PubMed: 25256445]
- Tu JB, Blackwell RQ, Cooper WC, Chen YH. Studies of pyridoxal-penicillamine antagonism in the human. Biochem Pharmacol. 1964;13:1527-35. [PubMed: 14239629]
- Veeravigrom M, Damrongphol P, Ittiwut R, Ittiwut C, Suphapeetiporn K, Shotelersuk V. Pyridoxal 5ꞌ-phosphate-responsive epilepsy with novel mutations in the PNPO gene: a case report. Genet Mol Res. 2015;14:14130-5. [PubMed: 26535729]
- Wang H-S, Kuo M-F, Chou M-L, Hung P-C, Lin K-L, Hsieh M-Y, Chang M-Y. Pyridoxal phosphate is better than pyridoxine for controlling idiopathic intractable epilepsy. Arch Dis Child. 2005;90:512-15. [PMC free article: PMC1720393] [PubMed: 15851435]
- Wason S, Lacouture PG, Lovejoy FH Jr. Single high-dose pyridoxine treatment for isoniazid overdose. JAMA. 1981;246:1102-4. [PubMed: 7265398]
- Ware TL, Earl J, Salomons GS, Struys EA, Peters HL, Howell KB, Pitt JJ, Freeman JL. Typical and atypical phenotypes of PNPO deficiency with elevated CSF and plasma pyridoxamine on treatment. Dev Med Child Neurol. 2014;56:498-502. [PubMed: 24266778]
- Webster R, Sankaran BP, Stormon M, Thomas G, Shun A, Mills P, Clayton P, Bandokar S, Bhattacharya K. Liver transplantation in PNPO deficiency: management challenges and biological lessons. J Inherited Metab Dis. 2021;44.
- Wilson MP, Footitt EJ, Papandreou A, Uudelepp ML, Pressler R, Stevenson DC, Gabriel C, McSweeney M, Baggot M, Burke D, Stödberg T, Riney K, Schiff M, Heales SJR, Mills KA, Gissen P, Clayton PT, Mills PB. An LC-MS/MS-based method for the quantification of pyridox(am)ine 5'-phosphate oxidase activity in dried blood spots from patients with epilepsy. Anal Chem. 2017;89:8892-900. [PMC free article: PMC5588098] [PubMed: 28782931]
- Wilson MP, Plecko B, Mills PB, Clayton PT. Disorders affecting vitamin B6 metabolism. J Inherit Metab Dis. 2019;42:629-46. [PubMed: 30671974]
- Xue J, Chang X, Zhang Y, Yang Z. Novel phenotypes of pyridox(am)ine-5'-phosphate oxidase deficiency and high prevalence of c.445_del448del mutation in Chinese patients. Metab Brain Dis. 2017;32:1081-7. [PubMed: 28349276]
Publication Details
Author Information and Affiliations
Service for Child Neurology and Inherited Metabolic Disorders
Division of General Pediatrics
Department of Pediatrics and Adolescent Medicine
Medical University of Graz
Graz, Austria
University College London
Great Ormond Street Institute of Child Health
London, United Kingdom
Publication History
Initial Posting: June 23, 2022.
Copyright
GeneReviews® chapters are owned by the University of Washington. Permission is hereby granted to reproduce, distribute, and translate copies of content materials for noncommercial research purposes only, provided that (i) credit for source (http://www.genereviews.org/) and copyright (© 1993-2024 University of Washington) are included with each copy; (ii) a link to the original material is provided whenever the material is published elsewhere on the Web; and (iii) reproducers, distributors, and/or translators comply with the GeneReviews® Copyright Notice and Usage Disclaimer. No further modifications are allowed. For clarity, excerpts of GeneReviews chapters for use in lab reports and clinic notes are a permitted use.
For more information, see the GeneReviews® Copyright Notice and Usage Disclaimer.
For questions regarding permissions or whether a specified use is allowed, contact: ude.wu@tssamda.
Publisher
University of Washington, Seattle, Seattle (WA)
NLM Citation
Plecko B, Mills P. PNPO Deficiency. 2022 Jun 23. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024.