NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Summary of review questions covered in this report
This evidence report contains information on 2 reviews:
- D.2a.
What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
- D.2b.
What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
Service coordination: Inpatient to outpatient settings for people with complex rehabilitation needs after traumatic injury
Review question
This evidence report contains information on 2 reviews relating to service coordination when transferring from inpatient to outpatient settings:
- D.2a.
What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
- D.2b.
What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
Introduction
The transition from inpatient to outpatient services can provoke many emotions for the patient and their families, from excitement and happiness to loneliness and anxiety. Typically, the patient moves from inpatient care where there is consistent daily rehabilitation support to less intensive or fragmented outpatient community-based services, with the addition of social care if required. There are many challenges in achieving a seamless transition, such as regional variation in how services are offered (if they exist at all), waiting times for services and the handover of good quality patient information. The patient and family can often feel isolated and frustrated that they are left to fend for themselves. Therefore, it is vital to strive to deliver an equitable and seamless pathway through both health and social care across this transition point to achieve a high quality rehabilitation journey.
The objective of this review is to determine the best methods to deliver and coordinate rehabilitation services and social services for people with complex rehabilitation needs following traumatic injury, when they are transferring from inpatient to outpatient rehabilitation services.
Summary of the protocol
This review was a mixed methods review. See Table 1 and Table 2 for a summary of the Population, Intervention, Comparison and Outcome (PICO; quantitative) and Population, Phenomenon of interest and Context (PPC; qualitative) characteristics characteristics of this review in the adult and children and young people populations, respectively
For further details see the review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual. Methods specific to this review question are described in the review protocol in appendix A and in the methods chapter (Supplement 1).
This is a mixed methods review, using parallel synthesis. Quantitative and qualitative data were analysed and synthesised separately and integrated through the committee’s interpretation of results, described in the committee’s discussion of the evidence.
Declarations of interest were recorded according to NICE’s 2018 conflicts of interest policy.
Clinical evidence: Adults
The included studies are summarised in Table 3 and Table 4.
See the literature search strategy in appendix B and study selection flow chart in appendix C.
Included quantitative studies
Eleven studies (reported in 12 papers) were included in the quantitative section of this review. Nine of these studies were randomised controlled trials (RCTs; Browne 2013, Chong 2013, Hall 2005, Lin 2009, Parson 2019, Ryan 2006, Stenvall 2007, Vikane 2017 and Wiechman 2015), with the remaining 2 being non-randomised cohort studies (Flikweert 2014 and Hall 2018).
One RCT compared the effectiveness of multidisciplinary team care with usual care in general trauma patients, and was conducted in Austrialia (Browne 2013). Another RCT compared the effectiveness of multidisciplinary team care plus structured assessments with multidisciplinary team care only in hip fracture patients, and was conducted in Singapore (Chong 2015). Two RCTs were conducted in Tawainese hip fracture patients: 1 compared the effectiveness of discharge planning by a gerontological nurse with routine discharge planning (Huang 2005) and the other compared comprehensive discharge planning with routine discharge planning (Lin 2009). Another RCT compared supported discharge team care with usual care in general trauma patients, and was conducted in New Zealand (Parsons 2019), while another RCT compared an intensive multidisciplinary intervention with a less intensive intervention in hip fracture patients and was conducted in the UK (Ryan 2006). Please note that this study reported 3-month and 12-month data in 2 separate publications. An RCT compared the effectiveness of multidisciplinary outpatient treatment with usual care by general practitioners in patients with traumatic brain injury (TBI), and was conducted in Norway (Vikane 2009), while another RCT compared the effectiveness of an extended care practitioner care plus telephone calls with standard outpatient care in burn injury patients, and was conducted in the USA (Wiechman 2015).
The final RCT compared the effectiveness of a multidisciplinary post-operative rehabilitation intervention with conventional post-operative rehabilitation, and was conducted in Sweden (Stenvall 2007). This intervention spanned rehabilitation coordination both while patients were in inpatient settings and when patients were transferring between inpatient and outpatient settings. It therefore met the inclusion criteria for 2 of the coordination of rehabilitation reviews. Stenvall (2007) is therefore included in both reviews, with the outpatient outcomes reported in this review and the inpatient outcomes reported in the review focusing on coordination of inpatient rehabilitation services.
One cohort study compared the effectiveness of a multidisciplinary care pathway with standard care in hip fracture patients and was conducted in the Netherlands (Flikweert 2014), while the other cohort study compared the effectiveness of a traumatic clinical care coordination with no traumatic clinical care coordination and was conducted in the USA (Hall 2018).
Included qualitative studies
Nineteen primary studies were included in the qualitative section of this review. One of these studies was conducted in the UK (Odumuyiwa 2019), 7 were conducted in Australia (Barclay 2019, Braaf 2018, Isbel 2017, Kennedy 2012, Kornhaber 2019, O’Callaghan 2012 and Turner 2011), 4 in Canada (Glenny 2013, Jeyaraj 2013, Sims-Gould 2012 and Singh 2018) and 3 in Denmark (Christensen 2018, Graff 2018 and Lindahl 2013). One study each was carried out in Belgium (Christiaens 2015), Portugal (Sena Martins 2017) and Norway (Slomic 2017). The final study was a multinational study between France and Finland (Jourdan 2019).
One paper was a framework-based meta-synthesis of 12 primary studies, all conducted by the same research team in Canada (Stolee 2019). It is important to note that this paper included 2 of the above studies in their synthesis (Glenny 2013 and Sims-Gould 2012). In order to prevent double counting of data, findings have only been extracted from Glenny 2013 and Sims-Gould 2012 if they have not appeared in Stolee 2019.
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix K.
Summary of studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 3 (quantitative studies) and Table 4 (qualitative studies).
See the full evidence tables in appendix D. No meta-analysis was conducted (and so there are no forest plots in appendix E).
Results and quality assessment of clinical outcomes included in the evidence review
The quality of the evidence was assessed using GRADE for the quantitative evidence and CERQual for the qualitative evidence. See the evidence profiles in appendix F.
Summary of the quantitative evidence
No meta-analyses were performed as the interventions or outcomes were either not sufficiently similar to allow them to be combined or they were not reported by more than one study.
Of the pre-defined outcomes, evidence was found for:
- Patient satisfaction
- Length of hospital stay
- Return to work or education
- Overall quality of life
- Changes in activities of daily living
No evidence was found for outcomes relating to carer impact or unplanned readmission rates following discharge.
One RCT compared the effectiveness of an MDT care with usual care (Browne 2013). No statistically or clinically important difference was found in length of hospital stay between the groups. Additionally, no statistically or clinically important difference was found between groups in return to work or education, number of participants with impairment of ADL or FIM scores at 6 months post-discharge. All of these effect estimates were judged to be of very low quality.
One RCT compared the effectiveness of an MDT care plus structured assessments with MDT care only (Chong 2015). No statistically or clinically important difference in patient satisfaction at discharge was found between the groups. The evidence was judged to be of very low quality. Median length of hospital stay was reported in the study and, based on statistical analyses by the authors, was found to be statistically importantly lower in the MDT plus structured assessment than the MDT only group. However, the authors did not report whether this difference was clinically important and the evidence was judged to be of very low quality. No statistically or clinically important differences in overall quality of life (measured using SF-12 physical component score and SF-12 mental component score) or changes in ADL (measured using modified Barthel Index and Montebello Rehabiliation Factor score) were found at either 6 or 12 months. Evidence ranged from very low to low quality for these outcomes.
One cohort study compared the effectiveness of multidisciplinary care pathway with standard care (Flikweert 2014). According to the statistical analyses performed by the author, the median hospital length of stay was statistically importantly shorter in the multidisciplinary care pathway group. However, the authors did not report whether this difference was clinically important. This was judged to be of moderate quality.
One cohort study compared the effectiveness of traumatic clinical care coordination with no traumatic clinical care coordination (Hall 2018). Length of hospital stay was both clinically and statistically importantly longer in the traumatic clinical care coordination group when compared to the control group. This evidence was judged to be of low quality.
One RCT compared the effectiveness of discharge planning by a gerontological nurse with routine discharge planning (Huang 2005). The length of hospital stay was statistically and clinically importantly shorter in the discharge planning by a gerontological nurse group. Overall quality of life (measured using SF-36) and changes in ADL (measured using the Bathel Index) were statistically and clinically importantly higher (better) at discharge, at 2 weeks post-discharge and at 3 months post-discharge in the discharge planning by a gerontological nurse group when compared to the routine discharge planning group. Evidence ranged from low to moderate quality.
One RCT compared comprehensive discharge planning with routine discharge planning (Lin 2009). Outcomes were reported for patient satisfaction, length of hospital stay and changes in ADL (measured using Functional Status Subscale) up to 3 months post-discharge. No statistically or clinically important differences were reported between the groups for any of these outcomes. Evidence was judged to be very low to low quality.
One RCT compared supported discharge team with usual care (Parsons 2019). Length of hospital stay was statistically signficantly shorter in the supported discharge group compared to the usual care group. As the authors did not report standard deviations, and there are no published MIDs, clinical significance could not be determined. Evidence was of moderate quality.
One RCT compared an more intensive MDT care intervention with a less intensive MDT care intervention (Ryan 2006). Outcomes were reported for overall quality of life (measured using EQ-5D and EQ-VAS) and changes in ADL (measured using Barthel Index and Franchay Activities Index) at 3 and 12 months. No statistically or clinically important difference was found between the groups at either time point, and evidence was all judged to be very low quality.
One RCT compared the effectiveness of a multidisciplinary post-operative rehabilitation intervention with conventional post-operative rehabilitation (Stenvall 2007). No statistically or clinically important differences were found between the groups in the proportion of participants achieving independence in P-ADL at the 4 or 12 months post-operative follow-up or in each of the Katz ADL grades at discharge. Additionally, there were no statistically or clinically important differences in the proportion of participants achieving each Katz ADL score at 12 months, apart from grade G, where a statistically and clinically importantly lower number of participants achieved Grade G in the multidisciplinary post-operative rehabilitation compared to conventional post-operative rehabilitation. There was a statisticcally and clinically important increase in the proportion of participants returning to at least the same Katz ADL levels as before trauma in the multidisciplinary post-operative rehabilitation group compared to the conventional post-operative rehabilitation group at 12 months (although this was not true at 4 months follow-up). The evidence was judged to be of very low quality for all outcomes.
One RCT compared the effectiveness of multidisciplinary outpatient treatment with usual care by general practitioners (Vikane 2009). There was no statistically or clinically important differences between the groups in the proportion of participants able to return to work or changes in ADL (measured using the Glasgow Outcome Scale) at 12 months post-injury. Evidence was judged to be of very low quality.
One RCT compared the effectiveness of an extended care practitioner care plus telephone calls with standard outpatient care (Wiechman 2015). No statistically or clinically important differences were found between groups in patient satisfaction, overall quality of life (measured using the mental component of SF-12) or changes in ADL (measured using Goal Attainment Score) at either 6 or 12 months. There was a statistically, but not clinically, importantly higher (better) SF-12 physical component score in the extended care practitioner care plus telephone calls group at 6 months. However, this had disappeared at 12 months when no statistical or clinical important difference in SF-12 physical component score was reported. Evidence was very low to low quality for outcomes.
Summary of qualitative evidence
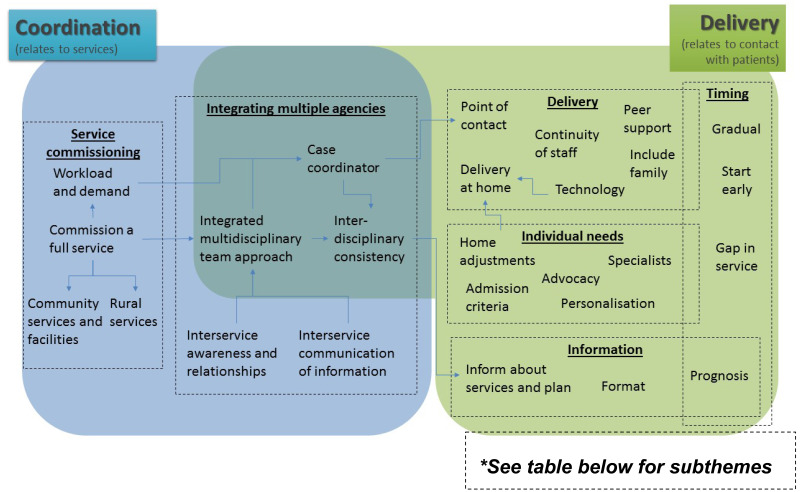
The views of adults with complex rehabilitation needs after traumatic injury, as well as staff who work in rehabilitation services and/or social services, were thematically analysed to find what they believed to be important for coordinating and delivering rehabilitation services and social services across transfer from inpatient to outpatient rehabilitation services. ‘Coordination’ was considered to relate mostly to the ways services organise within themselves, and ‘delivery’ was considered to relate mostly to how these should operate in front-line contact with service users. Six overarching themes were identified that had a total of 26 sub-themes (see appendix F).
The theme ‘service commissioning’ related to service coordination, as did the theme ‘integrating multiple services’ although some parts also crossed into delivery. The themes ‘delivery’, ‘individual needs’, and ‘information’ were all a part of how services should be delivered, and these were intersected by the theme of ‘timing’ and the need for action and consideration before, during and after discharge to the community. Although all the sub-themes are relevant to the question, some relate very practically and conceptually to others and this is indicated by blue arrows.
Summary of relevant qualitative and quantitative evidence
This is a mixed methods review, using parallel synthesis. Quantitative and qualitative data were analysed and synthesised separately and integrated through the committee’s interpretation of results, described in the committee’s discussion of the evidence.
Some of the qualitative evidence helped to explain or contextualise the quantitative findings and Table 6 shows where this was the case. Table 6 lists the sub themes from the qualitative evidence and matches it with the quantitative evidence from interventions targeting the identified area of coordination. It should be noted that not all aspects of a quantitative intervention will relate to a qualitative theme. Interventions often include features of more than 1 theme, and can therefore appear multiple times.
The contents of Table 6 are restricted to the results of the quantitative evidence and the qualitative themes this evidence speaks to. The following themes did not appear in any of the identified quantitative studies: 1.2 Community services and facilities; 1.4 Rural services; 2.2 Inter-service awareness and relationships; 3.1 Continuity of staff; 3.2 Include family; 3.5 Delivery at home; 3.6 Technology; 4.2 Prognosis; 5.2 Admission criteria; 5.3 Specialists; 6.1 Gradual; and 6.3 Gap in service. Additionally, 2 of the quantitative interventions did not include any of the qualitative themes identified in this review. Chong 2013 compared MDT care plus structured assessments and checklists with MDT care only and Ryan 2006a compared more intensive MDT care with less intensive MDT care.
For details of all study results, see the adult Summary of the quantitative evidence and Summary of qualitative evidence sections above.
Clinical evidence: Children and young people
The included studies are summarised in Table 7 and Table 8.
See the literature search strategies in appendix B and study selection flow charts in appendix C.
Included quantitative studies
One study was included in this review, a RCT conducted in Brazil which compared a family-supported rehabilitation programme to a clinician-delivered rehabilitation programme in children with TBI (Braga 2005).
Included qualitative studies
One study was included for this review, a qualitative study conducted in healthcare professionals involved in acquired brain injury (ABI) rehabilitation in Canada (Rashid 2018).
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix K.
Summary of studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 7 and Table 4.
See the full evidence tables in appendix D. No meta-analysis was conducted (and so there are no forest plots in appendix E).
Results and quality assessment of clinical outcomes included in the evidence review
The quality of the evidence was assessed using GRADE for the quantitative evidence and CERQual for the qualitative evidence. See the evidence profiles in appendix F.
Summary of the quantitative evidence
No meta-analyses were performed as the interventions or outcomes were either not sufficiently similar to allow them to be combined or they were not reported by more than one study.
Of the pre-defined outcomes, evidence was only found for changes in activity of ADL. No evidence was found for:
- Patient satisfaction
- Length of hospital stays
- Return to nursey, education, training or work
- Overall quality of life including sleep
- Carer impact
- Unplanned readmission
One RCT found that a family-supported rehabilitation programme was associated with a statistically significantly, but not clinically importantly, higher (better) motor development score (as measured by the SARAH scale of motor development) compared to a clinician-delivered rehabilitation programme in children with TBI (Braga 2005).
Summary of the qualitative evidence
The following sub-groups were specified in the protocol but no evidence was found.
- Major trauma/non-major trauma
- Children and young people who are currently receiving social care services/not receiving social care services
- Children on at risk register/not on the register
- Children from lower socioeconomic group/not from lower socioeconomic groups
Additionally, no evidence was found for the coordination of rehabilitation services and social services.
Please see Table 9 for a summary of the extracted themes.
Summary of relevant qualitative and quantitative evidence
The quantitative and qualitative results were extracted, analysed and summarised separately before being considered together in an overall synthesis of the evidence. Table 10 lists the sub-themes identified in the qualitative evidence that are also addressed by the identified quantitative evidence along with the results of the corresponding quantitative evidence. It should be noted that not all aspects of a quantitative intervention will relate to a qualitative theme. Interventions often include features of more than 1 theme, and will therefore appear multiple times.
The contents of Table 10 are restricted to the results of the quantitative evidence and the qualitative themes this evidence speaks to. The following themes did not appear in the identified quantitative study: 1.1 Setting common goals and 2.2 Importance of community support. Peer support was a theme identified in the qualitative literature, and was a component of the family-supported rehabilitation intervention. However, this feature was also offered to the clinician-delivered rehabilitation control group and did not differ between groups. Due to this, it has not been included in the above synthesis.
For details of all study results, see the children and young people Summary of the quantitative evidence and Summary of qualitative evidence sections above.
Economic evidence: Adults and children and young people
Included studies
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to these review questions.
See the literature search strategy in appendix B and study selection flow chart in appendix G.
Excluded studies
Economic studies not included in these reviews are listed, and reasons for their exclusion are provided in appendix K.
Summary of studies included in the economic evidence review
No economic evidence was identified which was applicable to this review question.
Economic model
Thes adult review question was identified as an economic priority, however, no economic modelling was undertaken because the committee could not identify a recommendation in this area that would benefit from supporting economic modelling. No economic modelling was undertaken for the children and young people review because the committee agreed that other topics were higher priorities for economic evaluation.
The committee’s discussion of the evidence
The outcomes that matter most
Quantiative evidence
When selecting the critical and important quantitative outcomes to examine for adults, the committee prioritised outcomes that can be applied to the whole heterogeneous population of people with complex rehabilitation needs after traumatic injury, complement the anticipated qualitative themes in the literature, and apply to the services and settings covered in this review question. Patient satisfaction, length of hospital stay and return to work or education were selected as critical outcomes. Patient satisfaction was chosen as it is indicative of a person’s trust and future engagement with rehabilitation and social services. Length of hospital stay was chosen due to its applicability to coordination of rehabilitation care, and preparation for discharge. The committee discussed an outcome that would encompass both rehabilitation and social services. Return to work or education requires co-ordination of multiple services (for example, healthcare professionals, social services, employment services) and was identified as a suitable outcome to measure this co-ordination. Return to nursery was added to this outcome for the children and young people review. The committee discussed that their interest in investigating co-ordination of care was ultimately to improve rehabilitation outcomes for people after traumatic injury. Therefore, although not direct indicators of care co-ordination, quality of life and changes in activities of daily living were selected as important outcomes. Sleep was added to the quality of life outcome for the children and young people review because especially in younger people it can be difficult to measure well-being, function and quality of life adequately, but if young children are not functioning well, this is often reflected in poor sleep. Traumatic injury also has a large effect on carers, who may have to take on a greater supportive or advocacy role. To encompass this population, carer impact was selected as another important outcome. Finally, unplanned readmission can occur when rehabilitation needs after discharge have not been adequately addressed. Therefore, the committee also included this as an important outcome.
Qualitative evidence
This was a mixed-methods review so the committee were unable to specify in advance the qualitative data that would be located. Instead they identified the following example main themes to guide the review and were aware that additional themes may have been identified:
- Rehabilitation prescription
- Case managers
- Rehabilitation specialist
- Multidisciplinary team approach
- Social worker
The quality of the evidence
Quantitative evidence
The overall quality of evidence was assessed using GRADE methodology.
For adults, the evidence was judged as being very low to moderate quality, with the majority being very low quality. Evidence was downgraded in 2 areas: concerns about the risk of bias in contributing studies (commonly due to lack of standardisation of intervention duration and dose for non-randomised studies, and a lack of blinding in RCTs) and imprecision in the effect estimates.
For children and young people, the evidence was judged as being very low quality. Evidence was downgraded in 2 areas: concerns about risk of bias (namely differences in intensity and duration of rehabilitation sessions for children carrying out their rehabilitation at home compared to children attending rehabilitation at the clinic) and imprecision in the effect estimate (probably due to a small number of study participants).
Qualitative evidence
The evidence was assessed using GRADE-CERQual methodology.
For adults, the evidence was found to range in quality from very low to high quality, with the majority being high quality. In some cases, the evidence was downgraded due to poor applicability (for example, where the themes were not based on any research from a UK context, and/or had only been identified in studies of populations with only one particular type of traumatic injury). Some downgrading for adequacy occurred when the richness or quantity of the data was low, or where there were few first-order quotes to back up the author’s second-order findings. Other issues resulting in downgrading were in the event of methodological problems that may have had an impact on the findings, and/or for incoherence within the findings.
For children and young people, the evidence was judged to be very low quality. Evidence was downgraded due to concerns over the applicability of the rehabilitation population as no data came from UK settings and the population which can include traumatic and non-traumatic ABI. Adequacy of data was also a concern.
Benefits and harms
High quality qualitative evidence from the theme ‘Prognosis’ in the adult review showed that people with rehabilitation needs want information about their condition, probable long-term prognosis and how this could affect their lives in future. The committee agreed with this finding, but added that this can often be difficult to correctly predict and that not everyone with traumatic injuries will want this information. Therefore, they added that prognoses should only be delivered after receiving the views and opinions of the entire MDT so that any considerations and limitations can be conveyed to patients. Additionally, healthcare staff might be delivering sensitive and distressing information which should be communicated in a private and thoughtful manner.
Moderate quality qualitative evidence from the theme ‘Inter-service communication of information’ in the adult review showed that people with rehabilitation needs and healthcare staff believe that relevant healthcare information should be communicated in a timely and simple manner. Particularly, a relevant history of the patient’s events, injuries, treatments, and results (for example, x-rays) should be passed on to services in advance. This theme included evidence from a variety of traumatic injury populations, as well as moderate quality quantitative evidence from 2 quantitative studies reporting a significantly shorter length of hospital stay during interventions that included prompt information exchange prior to discharge. The committee discussed that one way of facilitating this simple transfer was to make sure that all the relevant information was collated into a rehabilitation plan, so it is all in one place when needed. The committee agreed that data linkage is a very important factor across the rehabilitation healthcare pathway. Not only does this greatly assist co-ordination within and between rehabilitation settings, but provides reliable data for audits, service reviews and pathway improvements. The committee therefore recommended services use a unique identifier when communicating rehabilitation information between settings. Ideally, this should be their NHS number as this can be used by a wider number of services and settings within the NHS (rather than just rehabilitation). The use of a rehabilitation plan will also help to increase consistency between members of the rehabilitation MDT. Moderate quality qualitative evidence from the theme ‘Interdisciplinary consistency’ in the adult review showed that people undergoing rehabilitation are confused when they receive different information and instructions from different healthcare professionals. This in turn decreases their trust in rehabilitation services which may cause decreased engagement in their rehabilitation programme. The committee recommended that the rehabilitation plan includes input from the whole MDT in order to increase consistency. Very low quality qualitative evidence from the theme ‘Format’ in the adult review reports that people with rehabilitation needs may find information easier to understand and retain if it is presented to them in plain, accessible language. The committee agreed if information is not written in an accessible format, it can lead to confusion, and therefore specified that the rehabilitation plan should be written in clear and easy-to-understand language.
The benefits of a shared rehabilitation plan between healthcare professionals and people undergoing rehabilitation after traumatic injury was supported by high quality qualitative evidence from the theme ‘Inform about services and plans’ in the adult review. This finding showed that people with rehabilitation needs after traumatic injury appreciate being offered information about rehabilitation, believing that it smoothes transitions between healthcare settings (particularly when being discharged into the community). This information should include information on what services are available to them, how to access them, what arrangements have been made by healthcare professionals and what they may need to arrange themselves. Educating people on these matters empowers them and increases engagement in rehabilitation. Three of the included quantitative studies investigated the effectiveness of using a central healthcare professional for people to contact, and to help co-ordinate rehabilitation. The committee discussed the conflicting quantitative evidence identified in the adult population. One study investigating a discharge planning intervention versus routine care reported evidence of a clinically importantly shorter hospital length of stay (low quality evidence), as well as clinically importantly higher quality of life (moderate quality evidence) and changes in activities of daily living up to 3 months post discharge (moderate quality evidence) in the group that received the discharge planning intervention. This was contradicted by results from another study using a trauma clinical care co-ordinator, which found a clinically importantly longer length of hospital stay in the group who received input from a trauma clinical care co-ordinator. However, this intervention intentionally increased the length of stay in people receiving the intervention and the committee therefore disregarded the evidence. The remaining study compared an extended care practitioner plus telephone calls intervention to standard outpatient care. This study reported no clinically important difference between groups in patient satisfaction, overall quality of life or changes in activities of daily living. Despite the conflicting evidence, the committee agreed that their experience and expertise support the beneficial effects of informing people about their rehabilitation plans, and noted that the qualitative evidence also encompassed a variety of different trauma populations (general trauma, burns, hip fracture and brain injury), so was widely applicable. They noted that they have made several recommendations throughout the guideline regarding keeping people educated and informed of their rehabilitation options and support available. They used the above evidence to expand and strengthen recommendations on what the rehabilitation plan should include, which healthcare professionals it should be shared with, and how it should be shared with people undergoing rehabilitation.
Low quality evidence from the theme ‘Personalisation’ in the adult review showed that both healthcare staff and people with rehabilitation needs after traumatic injury feel that a rehabilitation plan should be tailored to each person (for example, their age, co-morbidities, physical function), and should be flexible around other commitments. It will also need to take into consideration particular vulnerabilities (for example, housing or risk of substance misuse). Seven of the included quantitative studies identified in the adult review stressed the importance of personalising the rehabilitation pathway for patients, rather than a standard ‘one-size-fits-all’ approach. Of the 5 that reported length of hospital stay, 3 reported a clinically significantly shorter stay in hospital for people receiving personalised rehabilitation care when compared to the standard rehabilitation care (judged to be moderate to low quality). Furthermore, 1 study investigating the effectiveness of a discharge planning intervention reported that is was associated with a clinically importantly higher quality of life (moderate quality) and changes in activities of daily living up to 3 months post discharge (moderate quality) compared to standard care. No clinically important difference was found for either patient satisfaction or return to work or education (very low quality, reported in 1 study each). The committee recommended including people in developing their rehabilitation plan, to ensure that it is personalised and focused on the most important goals to the person. The committee also applied this evidence to agree the importance of personalisation at all stages of the rehabilitation pathway, reporting that it promoted communication, as well as increasing trust and engagement with rehabilitation services. The committee used this evidence to strengthen several recommendations throughout the guideline that highlight the importance of a holistic and individualised rehabilitation programme.
High quality evidence from the theme ‘Advocacy’ in the adult review showed that adults with rehabilitative needs reported that they sometimes relied upon family members to research available rehabilitation services, support them with arranging appointments and completing administration, and starting conversations with healthcare professionals. However, advocacy services were not supported by the quantitative evidence (also in the adult population), with no difference reported for patient satisfaction, overall quality of life or changes in activities of daily living between groups receiving extra coordination of rehabilitation services when compared to those who did not. One study reported a higher length of hospital stay in people receiving advocacy as part of their intervention. However, the committee discussed that the intervention in question had specifically increased hospital stay in order to complete all aspects of the intervention, and decided to disregard this low quality evidence. The committee decided not to make recommendations in the area of advocacy, but did discuss the strength of the qualitative evidence and the positive testimonies of support received from healthcare professionals shared by the lay members. Therefore, the committee highlighted the legal entitlement of certain populations of people to professional advocacy services under the Mental Capacity Act 2005 and/or the Care Act 2014. Further information can also be found in the NICE guideline on decision making and mental capacity which can be used as a guide to ensure that people are supported to make decisions for themselves when they have the mental capacity to do so or, where they lack the mental capacity to make specific decisions, they remain at the centre of the decision-making process.
High quality qualitative evidence from the theme ‘Continuity of staff’ in the adult review showed that people with rehabilitation needs prefer to see the same healthcare professionals wherever possible. This is because patients and healthcare staff both invest time to build trust and rapport with each other, which can lead to more honest and open communication. When healthcare staff are changed, service users lose that relationship and can become discouraged with continuing rehabilitation. Additionally, there is an increased resource impact of time taken to re-share history and personal details, as well as the possibility of mistakes when information is not passed on. Both the healthcare professionals and lay members of the committee agreed with this theme. While it was acknowledged that full continuity is not always possible, the committee highlighted the importance of considering this aspect of a patient’s rehabilitation journey. The committee discussed periods of transfer when changes in rehabilitation teams are unavoidable (for example, when being discharged back into the community), and how this can be managed. In their experience, community teams meeting patients and families before the transfer of care, rather than a ‘cold’ transfer, is very important in making people feel more comfortable with the change. It allows introductions in a less formal setting, a detailed handover of care needs from the current clinical team, and time for any questions patients and family members might have. The committee were aware that time is often limited during scheduled rehabilitation appointments, and this extra meeting would decrease pressure for all parties in the subsequent appointments.
Low to moderate quality quantitative evidence in the adult review showed that interventions that focused on the early initiation of conversations about discharge led to a decreased length of hospital stay, increased overall quality of life and increased changes in activities of daily living. Moreover, these differences were sustained at 3 months after discharge. These results were supported by low quality qualitative evidence from the theme ‘Start early’ in the adult review, which shows that both healthcare staff and adults with rehabilitation needs believe that discussions about discharge planning should begin early, in order to allow for a gradual incorporation of necessary exercises and adjustments into rehabilitation plans. The committee used their experience and expertise to recommend that these discussions should be multidisciplinary, in order to capture the full range of exercises and adjustments that a person will need once discharged from inpatient services. However, the committee were also aware that not every rehabilitation setting will be adequately resourced to deliver this discharge planning. Similarly, it might not be appropriate to start discharge planning conversations early (for example, if people are still distress or confused, leading to a difficultly processing and retaining information). Therefore, the committee suggested that this format of discharge planning be considered, but not mandatory.
High quality qualitative evidence from the theme ‘Include family’ in the adult review reported that healthcare staff and adults with rehabilitation needs are aware of the significant support family members can offer, especially when discharged into the community. This was somewhat supported by quantitative evidence from the children and young people’s population, where a family supported rehabilitation programme reported significantly (but not clinically) importantly improved activities of daily living when compared to a clinician-delivered rehabilitation programme. The committee discussed that this support is often invaluable, covering potential gaps in services and coordination of care during the transition process. Therefore, they recommended that family members be actively involved in the discharge planning process as well receiving any rehabilitation education they may need. However, they also are aware of a potential safeguarding aspect of a blanket recommendation to include family members in discharge planning (for example, if there are disagreements about what rehabilitation options should be taken). They therefore highlighted that this inclusion should only be done after consent has been given by patients and if families feel comfortable with it.
High quality qualitative evidence from the theme ‘Gradual’ in the adult review reported that healthcare staff and adults with rehabilitation needs believe that rehabilitation should include a gradual and incremental return to the community. The committee discussed that this softer discharge approach can reduce the distress of the sudden loss of inpatient-support. In their experience, using local step-down wards, pre-discharge weekend home visits and supported community accommodations are all good ways of providing a continued level of support for rehabilitation patients. However, the committee agreed that this strategy is not always needed by patients, and may even at times prolong time away from home which brings its own disadvantages. Additionally, there is a corresponding increase in the level of planning healthcare professionals will need to undertake in order to organise these interventions. Therefore, the committee recommended that this approach is offered to rehabilitation patients with significant ongoing medical and therapy needs, where their experience suggests the most benefit will be had.
High quality qualitative evidence from the theme ‘Integrated multidisciplinary team approach’ in the adult review showed that healthcare professionals and people undergoing rehabilitation highlight the importance of a multidisciplinary team approach when delivering rehabilitation after traumatic injury. This is especially true when transferring from inpatient to outpatient care, to co-ordinate medical and social support needs. A multidisciplinary team was involved in 5 of the included quantitative studies identified in the adult review. Three of these studies reported length of hospital stay as an outcome measure, with 2 reporting moderate quality evidence showing a clinically importantly shorter length of stay in the groups that received multidisciplinary discharge coordination Three studies also reported changes in activities of daily living, all of which were very low quality. Of the 14 measures of activities of daily living reported, there were 2 clinically importantly better results in intervention groups that received multidisciplinary discharge coordination, with the remaining 12 reporting no clinically important difference between the groups. Very low quality evidence from 2 of these studies showed no clinically important difference between the groups in return to work or education either. The committee discussed how the quantitative results did not agree with their clinical experience. They noted that the included studies varied in the amount of post-discharge support provided by the multi-disciplinary team and the length of the interventions. Because of this and the quality of the quantitative evidence, the committee made their recommendations based on the above high quality evidence from the theme ‘Integrated multidisciplinary team approach’, supplemented by 3 additional themes identified for this review. High quality qualitative evidence from the theme ‘Interservice awareness and relationships’ in the adult review shows that healthcare staff find it helpful to work with other agencies if they have the opportunity to build a working relationship. The opportunity to meet in person may help to delivery better integrated and coordinated rehabilitation care. Moderate quality qualitative evidence from the theme ‘Interdisciplinary consistency’ (in the adult population) and very low quality evidence from the theme ‘Setting common goals’ (in the children and young people population) shows that people find it confusing when different professionals provide them with inconsistent information, advice or instructions. This in turn decreases their trust in rehabilitation services which may decrease their engagement in their rehabilitation programme. Arranging pre-discharge meetings or joint-handover sessions will allow professionals from different settings to directly communicate with each other, increase their opportunity to form working relationships and ensure that the same information is provided to all parties at the same time. Finally, low quality qualitative evidence from the theme ‘Home adjustments’ in the adult review showed that people may need home adjustments in order to increase their independence and aid rehabilitation progress. Arranging a pre-discharge planning meeting with community practitioners will not only increase communication between healthcare and social care professionals, it will also allow any home adjustments to be noted and implemented by the relevant community teams before people are discharged back home. However, the committee were also aware that not every rehabilitation setting will be able deliver this pre-discharge meeting, as finding a time for suitable for multiple agencies presents a challenge. Therefore, the committee suggested that this meeting be considered, but not mandatory.
High quality qualitative evidence from the theme ‘Point of contact’ in the adult review showed that adults appreciated a single point of contact to provide information, support and rehabilitation co-ordination as they transfer from inpatient to outpatient settings. This was supported by high quality qualitative evidence from the theme ‘Case co-ordinator’ (also in the adult review) showing that healthcare professionals and adults with rehabilitation needs appreciated being able to communicate with one source for all information regarding a person’s rehabilitation plan. Additional very low quality evidence from the theme ‘Case workers’ in the children and young people population was consisted with this finding. Three of the included quantitative studies investigated the effectiveness of using a central healthcare professional for people to contact, and to help co-ordinate rehabilitation. The committee discussed the conflicting quantitative evidence identified in the review population. One study investigating a discharge planning intervention versus routine care reported evidence of a clinically importantly shorter hospital length of stay (low quality evidence), as well as clinically importantly higher quality of life (moderate quality evidence) and changes in activities of daily living up to 3 months post discharge (moderate quality evidence). This was contradicted by results from another study using a trauma clinical care co-ordinator, which found that the length of hospital stay was clinically importantly longer in the group who received input from the trauma clinical care co-ordinator. However, this intervention intentionally increased the length of stay in people receiving the input from the trauma clinical care co-ordinator and the committee therefore disregarded the evidence. The remaining study compared an extended care practitioner plus telephone calls intervention with standard outpatient care. This study reported no clinically important difference between groups in patient satisfaction, overall quality of life or changes in activities of daily living. The committee acknowledged the conflicting quantitative evidence, but discussed the strong qualitative evidence presented in this review and in other co-ordination reviews showing that a central point of contact was very helpful in developing relationships with patients and their families. In their experience, this can cause a better rapport with and increased trust in rehabilitation services. The committee discussed concerns about patients assuming that they could contact a named healthcare professional at any time, regardless of shifts and annual leave. However, they agreed that a central point of contact will be particularly important when patients transfer from inpatient to outpatient settings, when care is being handed over to community healthcare teams. This contact can be a team or service within a hospital, which will give support to patients and flexibility in staffing. They recommended that the hospital point of contact be available to patients for a limited period of time after discharge in order to improve continuity of care during this period. The committee gave an example of 3 months which was designed to encompass the transition period while still providing a stimulus to ensure healthcare is properly transferred to the appropriate setting. The committee understood that this recommendation would not necessarily be appropriate for rehabilitation patients with long-term and/or complex conditions that require the cooperation of more than one agency. Here, a continuing relationship between professionals and service users is important to understand personal and medical history as fully as possible, in order to better help patients navigate complicated and interacting agencies. Therefore, the committee recommended that appointing a key worker should be considered for patients with complex or long term conditions and/or social care needs. This can be a healthcare or social care professional, depending on which is more appropriate for the person in question. For children and young people, the healthcare or social care professional should also have experience in education and training support, as this will form a portion of their social needs. The committee highlighted additional guidance on the role of a named worker for young people transitioning to adult services, which can be found in the NICE guideline on transferring from children’s to adults’ services for young people using health or social care services.
Moderate quality quantitative evidence from 1 large study in the adult population investigating a multi-disciplinary care pathway spanning from accident and emergency to eventual discharge from a rehabilitation unit showed a significantly shorter length of hospital stay in patients following the multi-disciplinary care pathway. Clinical importance could not be determined due to only median and IQRs being reported by the study authors, and no MIDs identified either in the literature or from the committee. This was supported by moderate quality evidence from the theme ‘Commission a full service’ in the adult review. This theme described the importance of commissioning and funding rehabilitation pathways covering the entire pathway of a service user, including how services within these pathways should communicate and coordinate. Commissioners should collaborate with other commissioning bodies to ensure that rehabilitation pathways include the full range of services people may need access to (for example, vocational and educational rehabilitation services). The committee discussed that the wider rehabilitation needs of young people who are transferring from paediatric to adult services can be overlooked by commissioners, and therefore specifically mentioned this population. The committee discussed a central aspect of this theme, which described that criteria and rehabilitation milestones should be standardised within the pathway in order to facilitate easy transfer of care. In their experience, without this standardisation and clear direction of how services and healthcare professionals should interact with each other, delays are common from a variety of sources (for example, patients might be able to be discharged from one setting but not fulfil the admission criteria for another, or reduced funding of a downstream service might lead to less capacity and therefore longer waiting lists).
High quality qualitative evidence from the theme ‘Community services and facilities’ in the adult review showed that the availability of community and social services is just as important for overall rehabilitation as rehabilitative medical services are. These services are wide ranging and can include social care, housing, home-adaption, transport services, and sports/recreational facilities. The committee discussed that information on how to access these services should be given to service users prior to discharge, so patients and their families are aware of what is available in their local area.
High quality qualitative evidence from the theme ‘Inter-service awareness and relationships’ in the adult review reported that continuity of care is increased when staff from different areas of the rehabilitation pathway are aware of the other areas (for example, rehabilitation healthcare professionals knowing about social services available in their areas), and have an opportunity to network with these difference areas. The committee discussed how providing networking opportunities will increase staff knowledge of how to access these different facilities, increase the amount of opportunities professionals have to communicate with rehabilitation peers, and strengthen communication channels between organisations.
High quality evidence from the theme ‘Rural services’ in the adult review showed that rural areas are often underserved by specialist rehabilitation services. This is supported by evidence on the availability of specialist services in other co-ordination reviews. The committee discussed that it is not simply rural areas that are underserved, and that there is a wide spectrum of access to specialist rehabilitation professionals across healthcare settings in the UK (for example, some people are unable to leave their homes). This becomes particularly important when people are returning home from a hospital in-patient setting. The committee discussed this finding along with high quality qualitative evidence from the theme ‘Specialists’ in the adult review, which showed that it is important for rehabilitation outcomes that an individual’s ongoing care team include some staff with specialist knowledge, in order to support more generalised healthcare areas. For example, GPs may not have specialist knowledge of a patient’s disabilities and/or conditions following complex trauma but they act as gatekeepers to more specialist services. Therefore, they may not be aware of the appropriate referrals to make when confronted with patients undergoing rehabilitation. The committee discussed that this could be mitigated by ensuring patients have an ongoing rehabilitation team that contains staff with specialist knowledge. The committee were aware that it would not be feasible to recommend increasing the amount of specialist healthcare professionals in this area due to the large resource implications this would have. However, they discussed the feasibility of ensuring that more generalised services received some specialist support to cover rehabilitation populations (for example, psychologist trained in trauma). The committee agreed that, as support would not be needed full time, it could be delivered remotely, which would keep potential resource implications low. However, it would greatly increase the ability of generalised healthcare services to provide rehabilitation care. Low quality evidence from the theme ‘Technology’ in the adult review showed that healthcare professionals and people undergoing rehabilitation after traumatic injury report technology is a useful tool to increase access to rehabilitation specialists. Further low quality qualitative evidence from the theme ‘Delivery at home’ was found regarding the ability of healthcare services to provide rehabilitation at home earlier in the recovery process, which decreases length of length of hospital stay. Both use of technology and options for home rehabilitation have been identified in other co-ordination reviews, and the committee discussed how technology can be used to deliver follow-up, support and rehabilitation sessions to people in the community if these services are not available in their area (for example, videoconferencing being used to deliver specialist rehabilitation sessions at community services or in a person’s home). To support this recommendation, the committee also recommended that professionals in generalised medical settings should have access to individualised peer support and networking opportunities with specialised rehabilitation settings. However, the committee were aware that not every individual has accesss to the technology (for example, the internet) or the level of technological knowledge needed to deliver technology-enabled follow-up, support and rehabilitation sessions. Therefore, they recommended that this is only 1 way that can be considered in increase flexibility and accessability.
Very low quality qualitative evidence from the themes ‘Peer support (in the adult population) and ‘Importance of community support’ (in the children and young people population) showed that healthcare professionals and people undergoing rehabilitation after traumatic injury reported the benefits of support from people with lived experience. Due to the quality of the evidence, the committee used this evidence to strengthen previous recommendations on peer support rather than create new recommednations in this area.
The committee discussed the 3 remaining themes found in the adult population, but decided not to use them to make recommendations. High quality qualitative evidence from the theme ‘Workload and demand’ showed that efficiency can be decreased when staff are overworked and waiting list times may be increased. There was very low quality quantitative evidence supporting this, with changes in activities of daily living being clinically importantly better in participants receiving a multi-disciplinary team post-operative rehabilitation intervention which included increased staffing levels of the wards allocated to this intervention. However, this was only seen in 2 measures of activities of daily living (number of participants achieving independence in activities of daily living at 12 months and number of participants achieving Katz Grade G at 12 months). The other 9 activities of daily living measures did not find a difference between the groups. With this in mind, the large number of settings any recommendations would apply to, and the large resource impact recommendations in this area would have, the committee decided not to use this evidence in any recommendations. Low quality qualitative evidence from the theme ‘Admission criteria’ showed that inflexible admission criteria (for example, income factors or postcodes) can limit the services available to some adults with rehabilitation needs. While the committee discussed the importance of every patient receiving equal treatment access, they have made several other recommendations regarding flexibility of appointments throughout the guideline. While they do not target admission criteria directly, the committee believe that these will lead to greater access for all. Low quality evidence from the theme ‘Gap in service’ showed that, when discharged back into the community, some adults with rehabilitation needs experienced long waiting times before community rehabilitation began. The committee agreed that it was difficult to make specific recommendations to reduce waiting times, but they were confident that the recommendations made from this evidence review (along with co-ordination reviews) will lead to reduced waiting time for rehabilitation services in the longer-term.
Despite the limited evidence identified for children and young people in this review, the committee decided not to make a research recommendation in this area. Within the UK there is a relatively small number of paediatric major trauma centres, making studies in this population difficult. This, combined with the large amount of evidence found for the adult population, meant that the committee decided that other areas of the guideline would benefit more from new research.
Cost effectiveness and resource use
There was no existing economic evidence for this review.
The committee explained that multidisciplinary team reviews happen anyway. If people ask for information about the likely long-term prognosis providing such information only after a multidisciplinary team review will not incur additional resources. In most cases, the long-term prognosis is discussed at multidisciplinary team meetings to plan for long term rehabilitation, i.e. it is not something new that the teams will need to discuss.
The committee discussed delays between acute and rehabilitation settings. The committee explained that trauma systems are efficient and are ready to discharge much quicker than rehabilitation services which by their very nature are of a slower stream with much longer length of stays. The committee discussed potential solutions, e.g. commissioner’s/service managers focus on discharge to the community, making the system work as efficiently as possible, including early discharge conversations and early engagement with social services/funders. The committee explained that the transfer recommendations might make the process more efficient and result in cost savings to services.
Additional professional time might be needed to cover early discharge planning, checking access to community rehabilitation services, and organising home visits. The recommendations imply more coordination between inpatient teams and other health and social care services, which will take more time. However, this additional time spent will result in patients feeling more supported, increasing their confidence in services and improving outcomes. Also, this would only be required for a small number of people with the most complex needs. The committee explained that these recommendations reinforce current practice in this subset of people with the most complex needs for most services. However, there may be resource implications for services that are providing sub-optimal care / are underperforming.
Similarly, the committee explained that if a person has significant ongoing and complex medical and therapy needs, offering a gradual and incremental return into the community, e.g., transfer to a local hospital, a stepdown bed or a pre-discharge visit to a home, is a standard practice. Also, a pre-discharge planning meeting with community practitioners involved in the person’s rehabilitation, social care and support would be a standard practice in people with the most complex needs. These recommendations are not expected to result in a resource impact. However, there may be resource implications for services that are providing sub-optimal care / are underperforming.
The committee explained that for children and young people, meetings between the school or education setting, one or more members of the multidisciplinary team, parents and the child or young person (as appropriate) should be already happening and this recommendation should not represent a change in practice or require additional resources to implement. The committee explained that in spite of the existence of major trauma networks there is still considerable variation in practice around planning, commissioning and coordination of many aspects of rehabilitation. The committee explained that organising services with whole care pathways in mind and collaboration between commissioners represent good practice principles and should be happening across services. Where this is not happening, there may be some resource implications because services will need to set up or extend existing frameworks for more integrated commissioning and collaborative rehabilitation planning. In practice, this may entail more communication, effective information sharing and more meetings between services/practitioners. However, it is also likely to create efficiencies by ensuring that services are joined up and providing integrated care, with a potential to improve access to services, reducing waiting times and improving transfer and discharge practices, and ultimately improve patient outcomes.
The recommendation about giving people and their families and carers information about community rehabilitation and social services and/or national support networks and how they can access these are only about signposting and will not incur additional resources. It might require more practitioner time. However, it is expected to be standard practice for most services.
Most professionals already have networking opportunities. However, the practice may need to change for some services where this is not the case (for example, rural areas). Overall this recommendation is not expected to result in a resource impact for services.
Staff working with complex rehabilitation needs should already have specialist skills, knowledge, expertise, and experience of their particular injuries. This recommendation is stating the principle of good practice and should not result in a resource impact.
The recommendation on making sure that community rehabilitation practitioners have access to training expertise, advice or peer support from specialist services may mean that specialist rehabilitation professionals might need to spend more time providing peer support/training to general services/non-specialists. This could be done in low-cost ways, e.g., virtual meetings, signposting to information sources. The committee noted that if non-specialist healthcare professionals are better supported, people’s needs are more likely to be met locally and there will be less pressure on specialist services. The committee also discussed some benefits of such support to practitioners, e.g., individuals not feeling isolated, sharing experiences, empowerment, which ultimately lead to better care and improved patient outcomes. Overall, the committee expect that basic specialist/support for practitioners might be a cost-saving strategy, e.g. even though clinicians may spend time on initial support, local/community/generalist practitioners will provide care with minimal input from then on. This would also benefit people (e.g. care closer to home, less disruptive) and the health service (e.g. no need to cover travel costs, less reliance on ambulance transport).
The committee discussed recommendation around technology-enabled follow-up and explained that this is already standard practice in some services. The committee also discussed that an individual might have follow-up care/rehabilitation with their initial rehabilitation specialist with, e.g., videoconferencing. The committee member with an experience of trauma discussed that the use of technology might mean that rehabilitation is more accessible, e.g. not driving to appointments. Allows individualised support with the original team. The committee noted that this might result in a higher intervention cost, i.e. support/training local therapist would take half a day to a day versus continuous support by a consultant. However, overall this could be a cost-effective approach, i.e. any cost increase in staff costs could be offset by benefits/cost-savings due to less disruption to care (continuity), no need to train/support local community therapists who may not understand the complexity of a problem, and better patient outcomes.
The committee explained that handover, i.e. between the inpatient multidisciplinary team and community practitioners at the point of discharge, does happen and should not have a resource impact on services. Where this is not happening, more professional time will be required to attend these joint handover meetings. The committee explained that handover is crucial and, if not done appropriately, may adversely affect patient outcomes. For example, a committee member with an experience of trauma referred to a situation where a community therapist advised an individual to undertake weight-bearing, which conflicted with the advice by a specialist rehabilitation therapist. Such a joint handover appointment has the potential to avoid conflicting advice and ensure an individual is receiving appropriate care in the community. This may also reduce the number of people coming back to specialist services with unmet needs, which may require intensive rehabilitation further down the line.
The single patient document, such as a rehabilitation prescription, is standard good practice; however, it is variable. The recommendations on this might have resource implications for services that are providing sub-optimal care / are underperforming.
The committee also discussed a single point of contact (e.g. a clinical nurse specialist) at discharge from the hospital to provide people and their family/carers with information, help and advice. The committee explained that anyone could do this with a clinical background and that it doesn’t have to be one particular person. However, this is currently happening inconsistently, and so this recommendation may represent a change in practice for some services. The committee discussed the benefits of having a single point of contact, including developing relationships with patients and their families, a better rapport with and increased trust in rehabilitation services, particularly when patients transfer from inpatient to outpatient settings, i.e. when care is being handed over to community healthcare teams. Having a single point of contact will provide assurance to individuals and their family/carers, may potentially ensure continuity in care and also engagement with care. The committee was of a view that benefits would offset any additional costs to services where this is not happening, and having a single point of contact for a limited time would represent value for money.
The committee explained that all other recommendations reinforce standard practice and will not require additional resources.
Recommendations supported by this evidence review
This evidence review supports recommendations 1.1.1, 1.2.1, 1.2.2, 1.4.1, 1.4.2, 1.5.7, 1.6.6, 1.7.1, 1.7.6, 1.7.9, 1.7.10, 1.8.1, 1.8.3, 1.8.9, 1.8.15, 1.8.16, 1.8.22 to 1.8.24, 1.9.1, 1.9.2, 1.10.1, 1.10.2, 1.10.6, 1.10.8 to 1.10.10, 1.10.12 and 1.10.14 in the NICE guideline.
References
Barclay 2019
Barclay, Linda, Lalor, Aislinn, Migliorini, Christine, Robins, Lauren, A comparative examination of models of service delivery intended to support community integration in the immediate period following inpatient rehabilitation for spinal cord injury, Spinal Cord, 2019 [PubMed: 31827256]Braaf 2018
Braaf, Sandra, Ameratunga, Shanthi, Nunn, Andrew, Christie, Nicola, Teague, Warwick, Judson, Rodney, Gabbe, Belinda J., Patient-identified information and communication needs in the context of major trauma, BMC health services research, 18, 163, 2018 [PMC free article: PMC5842544] [PubMed: 29514689]Browne 2013
Browne, Allyson L., Appleton, Sally, Fong, Kim, Wood, Fiona, Coll, Fiona, de Munck, Sonja, Newnham, Elizabeth, Schug, Stephan A., A pilot randomized controlled trial of an early multidisciplinary model to prevent disability following traumatic injury, Disability and Rehabilitation, 35, 1149–63, 2013 [PubMed: 23083416]Chong 2013
Chong, Tsung Wei, Chan, Gribson, Feng, Liang, Goh, Susie, Hew, Agnes, Ng, Tze Pin, Tan, Boon Yeow, Integrated care pathway for hip fractures in a subacute rehabilitation setting, Annals of the Academy of Medicine, Singapore, 42, 579–84, 2013 [PubMed: 24356654]Christensen 2018
Christensen, Jan, Langberg, Henning, Doherty, Patrick, Egerod, Ingrid, Ambivalence in rehabilitation: thematic analysis of the experiences of lower limb amputated veterans, Disability and Rehabilitation, 40, 2553–2560, 2018 [PubMed: 28631501]Christiaens 2015
Christiaens, Wendy, Van de Walle, Elke, Devresse, Sophie, Van Halewyck, Dries, Benahmed, Nadia, Paulus, Dominique, Van den Heede, Koen, The view of severely burned patients and healthcare professionals on the blind spots in the aftercare process: a qualitative study, BMC health services research, 15, 302, 2015 [PMC free article: PMC4521491] [PubMed: 26231290]Flikweert 2014
Flikweert, E. R., Izaks, G. J., Knobben, B. A., Stevens, M., Wendt, K., The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial, BMC Musculoskeletal Disorders, 15, 188, 2014 [PMC free article: PMC4053577] [PubMed: 24885674]Glenny 2013
Glenny, Christine, Stolee, Paul, Sheiban, Linda, Jaglal, Susan, Communicating during care transitions for older hip fracture patients: family caregiver and health care provider’s perspectives, International journal of integrated care, 13, e044, 2013 [PMC free article: PMC3817953] [PubMed: 24198738]Graff 2018
Graff, Heidi J., Christensen, Ulla, Poulsen, Ingrid, Egerod, Ingrid, Patient perspectives on navigating the field of traumatic brain injury rehabilitation: a qualitative thematic analysis, Disability and Rehabilitation, 40, 926–934, 2018 [PubMed: 28129694]Hall 2018
Hall, Erin C., Tyrrell, Rebecca L., Doyle, Karen E., Scalea, Thomas M., Stein, Deborah M., Trauma transitional care coordination: A mature system at work, The journal of trauma and acute care surgery, 84, 711–717, 2018 [PubMed: 29370060]Huang 2005
Huang, T. T., Liang, S. H., A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling, J Clin Nurs, 14, 1193–201, 2005 [PubMed: 16238765]Isbel 2017
Isbel, Stephen T., Jamieson, Maggie I., Views from health professionals on accessing rehabilitation for people with dementia following a hip fracture, Dementia (London, England), 16, 1020–1031, 2017 [PubMed: 26843421]Jeyaraj 2013
Jeyaraj, J. A., Clendenning, A., Bellemare-Lapierre, V., Iqbal, S., Lemoine, M. C., Edwards, D., Korner-Bitensky, N., Clinicians’ perceptions of factors contributing to complexity and intensity of care of outpatients with traumatic brain injury, Brain Injury, 27, 1338–1347, 2013 [PubMed: 23923818]Jourdan 2019
Jourdan, Claire, Bahrami, Stephane, Azouvi, Philippe, Tenovuo, Olli, Practitioners’ opinions on traumatic brain injury care pathways in Finland and France: different organizations, common issues, Brain Injury, 33, 205–211, 2019 [PubMed: 30449182]Kennedy 2012
Kennedy, Nicole, Barnes, Jessica, Rose, Anna, Veitch, Craig, Bowling, Cott Dahlberg Degeneffe Gage Higgins Keightley Majdan McCabe McColl O’Callaghan Patterson Patton Patton Schlossberg Sheppard Sinnakaruppan Smith Turner Turner Turner Turner Turner Voss, Clinicians’ expectations and early experiences of a new comprehensive rehabilitation case management model in a specialist brain injury rehabilitation unit, Brain Impairment, 13, 62–71, 2012Kornhaber 2019
Kornhaber, Rachel, Rickard, Greg, McLean, Loyola, Wiechula, Rick, Lopez, Violeta, Cleary, Michelle, Burn care and rehabilitation in Australia: health professionals’ perspectives, Disability and Rehabilitation, 41, 714–719, 2019 [PubMed: 29207887]Lin 2009
Lin, P. C., Wang, C. H., Chen, C. S., Liao, L. P., Kao, S. F., Wu, H. F., To evaluate the effectiveness of a discharge-planning programme for hip fracture patients, Journal of Clinical Nursing, 18, 1632–1639, 2009 [PubMed: 19490299]Lindahl 2013
Lindahl, Marianne, Hvalsoe, Berit, Poulsen, Jeppe Rosengaard, Langberg, Henning, Quality in rehabilitation after a working age person has sustained a fracture: partnership contributes to continuity, Work (Reading, Mass.), 44, 177–89, 2013 [PubMed: 23324675]O’Callaghan 2012
O’Callaghan, Anna, McAllister, Lindy, Wilson, Linda, Insight vs readiness: factors affecting engagement in therapy from the perspectives of adults with TBI and their significant others, Brain Injury, 26, 1599–610, 2012 [PubMed: 22738228]Odumuyiwa 2019
Odumuyiwa, Tolu, Improving access to social care services following acquired brain injury: a needs analysis, Journal of Long-Term Care, 164–175, 2019Parsons 2019
Parsons, M., Parsons, J., Pillai, A., Rouse, P., Mathieson, S., Bregmen, R., Smith, C., Kenealy, T., Post-Acute Care for Older People Following Injury: A Randomized Controlled Trial, Journal of the American Medical Directors Association, 2019 [PubMed: 31629646]Ryan 2006
Ryan, T., Enderby, P., Rigby, A. S., A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age, Clinical Rehabilitation, 20, 123–131, 2006 [PubMed: 16541932]
Ryan, T., Enderby, P., Rigby, A. S., A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age: results at 12-month followup, International journal on disability and human development, 5, 83–89, 2006 [PubMed: 16541932]Sena Martins 2017
Sena Martins, Bruno, Fontes, Fernando, Hespanha, Pedro, Barnes, Barnes Davis Fontes Fontes Goffman Guion Hahn Henriques Hughes Klein Leder Martins Martins Oliver Oliver Oliver Santos Somers Stiker Stone Turner Wall, Spinal cord injury in Portugal: Institutional and personal challenges, Journal of Disability Policy Studies, 28, 119–128, 2017Sims-Gould 2012
Sims-Gould, Joanie, Byrne, Kerry, Hicks, Elisabeth, Khan, Karim, Stolee, Paul, Examining “success” in post-hip fracture care transitions: a strengths-based approach, Journal of Interprofessional Care, 26, 205–11, 2012 [PubMed: 22251369]Singh 2018
Singh, Hardeep, Shah, Meeral, Flett, Heather M., Craven, B. Catherine, Verrier, Mary C., Musselman, Kristin E., Perspectives of individuals with sub-acute spinal cord injury after personalized adapted locomotor training, Disability and Rehabilitation, 40, 820–828, 2018 [PubMed: 28084843]Slomic 2017
Slomic, M., Soberg, H. L., Sveen, U., Christiansen, B., Transitions of patients with traumatic brain injury and multiple trauma between specialized and municipal rehabilitation services-Professionals’ perspectives, Cogent Medicine, 4, 1320849, 2017Stenvall 2007
Stenvall, Michael, Olofsson, Birgitta, Nyberg, Lars, Lundstrom, Maria, Gustafson, Yngve, Improved performance in activities of daily living and mobility after a multidisciplinary post-operative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up, Journal of rehabilitation medicine, 39, 232–8, 2007 [PubMed: 17468792]Stolee 2019
Stolee, Paul, Elliott, Jacobi, Byrne, Kerry, Sims-Gould, Joanie, Tong, Catherine, Chesworth, Bert, Egan, Mary, Ceci, Christine, Forbes, Dorothy, A Framework for Supporting Post-acute Care Transitions of Older Patients With Hip Fracture, Journal of the American Medical Directors Association, 20, 414–419.e1, 2019 [PubMed: 30852166]Turner 2011
Turner, Benjamin James, Fleming, Jennifer, Ownsworth, Tamara, Cornwell, Petrea, Perceived service and support needs during transition from hospital to home following acquired brain injury, Disability and Rehabilitation, 33, 818–29, 2011 [PubMed: 20812814]Vikane 2017
Vikane, E., Hellstrom, T., Roe, C., Bautz-Holter, E., Assmus, J., Skouen, J. S., Multidisciplinary outpatient treatment in patients with mild traumatic brain injury: A randomised controlled intervention study, Brain Injury, 31, 475–484, 2017 [PubMed: 28296510]Wiechman 2015
Wiechman, Shelley A., Carrougher, Gretchen J., Esselman, Peter C., Klein, Matthew B., Martinez, Erin M., Engrav, Loren H., Gibran, Nicole S., An expanded delivery model for outpatient burn rehabilitation, Journal of burn care & research : official publication of the American Burn Association, 36, 14–22, 2015 [PubMed: 25198101]Braga 2005
Braga, L. W., Da Paz, A. C., Ylvisaker, M., Direct clinician-delivered versus indirect family-supported rehabilitation of children with traumatic brain injury: a randomized controlled trial, Brain Injury, 19, 819–831, 2005 [PubMed: 16175842]Rashid 2018
Rashid, M., Caine, V., Newton, A. S., Goez, H. R., Healthcare professionals’ perspective on the delivery of care to children with Acquired Brain Injury (ABI) and communication with their parents, Journal of Pediatric Rehabilitation Medicine, 11, 125–131, 2018 [PubMed: 30010150]
Evidence for adults
Evidence for children and young people
Appendices
Appendix A. Review protocol
Appendix B. Literature search strategies
Literature search strategies for review question
- D.2a.
What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
- D.2b.
What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
A combined search was conducted for both review questions.
Qualitative literature search strategies
Please note that this search was a combined search for the adult and children and young people evidence reviews covering this question AND the following evidence review questions: D.1 (What are the best methods to coordinate rehabilitation services for people with complex rehabilitation needs after traumatic injury whilst they are an inpatient, including when transferring between inpatient settings?), D.3 (What are the barriers and facilitators to accessing rehabilitation services, including follow-up, following discharge to the community for people with complex rehabilitation needs after traumatic injury?) and D.4 (What are the support needs and preferences of people who have complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient or community rehabilitation services?).
Databases: Medline; Medline EPub Ahead of Print; and Medline In-Process & Other Non-Indexed Citations
Date of last search: 17/01/2020 (PDF, 227K)
Databases: Embase; and Embase Classic
Date of last search: 17/01/2020 (PDF, 288K)
Database: PsycInfo
Date of last search: 17/01/2020 (PDF, 224K)
Database: Social Policy and Practice
Date of last search: 17/01/2020 (PDF, 217K)
Databases: Cochrane Central Register of Controlled Trials (CCTR); and Cochrane Database of Systematic Reviews (CDSR)
Date of last search: 17/01/2020 (PDF, 252K)
Database: Social Care Online
Date of last search: 17/01/2020 (PDF, 137K)
Quantitative literature search strategies
Please note that this search was a combined search for the adult and children and young people evidence reviews covering this question AND evidence review D.1 (What are the best methods to coordinate rehabilitation services for people with complex rehabilitation needs after traumatic injury whilst they are an inpatient, including when transferring between inpatient settings?).
Databases: Medline; Medline EPub Ahead of Print; and Medline In-Process & Other Non-Indexed Citations
Date of last search: 03/03/2020 (PDF, 313K)
Databases: Embase; and Embase Classic
Date of last search: 03/03/2020 (PDF, 293K)
Databases: Cochrane Central Register of Controlled Trials (CCTR); and Cochrane Database of Systematic Reviews (CDSR)
Date of last search: 03/03/2020 (PDF, 298K)
Health economics literature search strategies
Please note that this search was a combined search for the adult and children and young people evidence reviews covering this question AND evidence review D.1 (What are the best methods to coordinate rehabilitation services for people with complex rehabilitation needs after traumatic injury whilst they are an inpatient, including when transferring between inpatient settings?).
Databases: Medline; Medline EPub Ahead of Print; and Medline In-Process & Other Non-Indexed Citations
Date of last search: 18/03/2020 (PDF, 329K)
Databases: Embase; and Embase Classic
Date of last search: 18/03/2020 (PDF, 336K)
Databases: Cochrane Central Register of Controlled Trials (CCTR)
Date of last search: 18/03/2020 (PDF, 286K)
Appendix C. Clinical evidence study selection
Study selection for (PDF, 174K)
Appendix D. Clinical evidence tables
Appendix E. Forest plots
Forest plots for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No meta-analyses were performed as the interventions or outcomes were either not sufficiently similar to allow them to be combined or they were not reported by more than one study.
Forest plots for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No meta-analyses were performed as only one study was identified.
Appendix F. GRADE and GRADE-CERQual tables
Appendix G. Economic evidence study selection
Economic evidence study selection for review question (PDF, 161K)
Appendix H. Economic evidence tables
Economic evidence tables for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic studies were identified which were applicable to this review question.
Economic evidence tables for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic studies were identified which were applicable to this review question.
Appendix I. Economic evidence profiles
Economic evidence profiles for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic evidence was identified which was applicable to this review question.
Economic evidence profiles for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic evidence was identified which was applicable to this review question.
Appendix J. Economic analysis
Economic evidence analysis for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic analysis was undertaken for this review question.
Economic evidence analysis for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No economic analysis was undertaken for this review question.
Appendix K. Excluded studies
Excluded studies for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
Quantitative clinical studies
Table 39Excluded quantitative studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Adams, Annette L., Schiff, Melissa A., Koepsell, Thomas D., Rivara, Frederick P., Leroux, Brian G., Becker, Thomas M., Hedges, Jerris R., Physician consultation, multidisciplinary care, and 1-year mortality in Medicare recipients hospitalized with hip and lower extremity injuries, Journal of the American Geriatrics Society, 58, 1835–42, 2010 [PubMed: 20929461] | Outcome not in PICO: Mortality |
| Aitken, Mary E., Korehbandi, Patricia, Parnell, Donna, Parker, James G., Stefans, Vikki, Tompkins, Esther, Schulz, Eldon G., Experiences from the development of a comprehensive family support program for pediatric trauma and rehabilitation patients, Archives of Physical Medicine and Rehabilitation, 86, 175–9, 2005 [PubMed: 15641010] | Study design not in PICO: Non-comparative study |
| Albert, Steven M., Im, Ashley, Brenner, Lynda, Smith, Michael, Waxman, Richard, Effect of a social work liaison program on family caregivers to people with brain injury, The Journal of Head Trauma Rehabilitation, 17, 175–89, 2002 [PubMed: 11909513] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=27 in intervention, n=29 in control) |
| Anderson, J., Mason, C., Reverse culture - How intensive care coordination eases military transitions for returning soldiers with traumatic brain injuries, Brain Injury, Conference, 2010 | Published as abstract only |
| Anderson, J., Mason, C., Reverse culture shock - Military transitions for returning soldiers with traumatic brain injury, Journal of Head Trauma Rehabilitation, Conference, 2008 | Published as abstract only |
| Andersson, E. E., Emanuelson, I., Björklund, R., StaËšlhammar, D., Mild traumatic brain injuries: the impact of early intervention on late sequelae. A randomized controlled trial, Brain Injury, 26, 520–521, 2012 | Published as abstract only |
| Anonymous,, Trauma center boosts patient outcomes, Hospital case management : the monthly update on hospital-based care planning and critical paths, 9, 115–6, 2001 [PubMed: 11469007] | Narrative review |
| Asplin, G., Carlsson, G., Zidén, L., Kjellby-Wendt, G., Early coordinated rehabilitation in acute phase after hip fracture - a model for increased patient participation, BMC Geriatrics, 17, 240, 2017 [PMC free article: PMC5646112] [PubMed: 29041916] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=63 in intervention, n=63 in control) |
| Atwal, Anita, Caldwell, Kay, Do multidisciplinary integrated care pathways improve interprofessional collaboration?, Scandinavian journal of caring sciences, 16, 360–7, 2002 [PubMed: 12445105] | Study design not in PICO: Qualitative study and audit performed before 2000 |
| Avlund, K., Jepsen, E., Vass, M., Lundemark, H., Effects of comprehensive follow-up home visits after hospitalization on functional ability and readmissions among old patients. A randomized controlled study, Scandinavian Journal of Occupational Therapy, 9, 17–22, 2002 | Study dates not in PICO: 1996-1997 |
| Ayvazian, J., Lucente, J., Dudley-Brown, S., Clinical management of veterans with traumatic brain injury within the context of polytrauma, Journal of Head Trauma Rehabilitation, Conference, 2012 | Published as abstract only |
| Bandyopadhyay, S., Wilkinson, I., Giokarinin-Royal, T., How incorporating ‘lean’ approach led to improved delivery of care and reduction in length of hospital stay, Age and Ageing, 48, 2019 | Published as abstract only |
| Baron, Justine S., Sullivan, Katrina J., Swaine, Jillian M., Aspinall, Arlene, Jaglal, Susan, Presseau, Justin, White, Barry, Wolfe, Dalton, Grimshaw, Jeremy M., Self-management interventions for skin care in people with a spinal cord injury: part 1-a systematic review of intervention content and effectiveness, Spinal Cord, 56, 823–836, 2018 [PMC free article: PMC6128818] [PubMed: 29802393] | Systematic review: Included studies checked for relevance. |
| Baron, Justine S., Sullivan, Katrina J., Swaine, Jillian M., Aspinall, Arlene, Jaglal, Susan, Presseau, Justin, Wolfe, Dalton, Grimshaw, Jeremy M., Self-management interventions for skin care in people with a spinal cord injury: part 2-a systematic review of use of theory and quality of intervention reporting, Spinal Cord, 56, 837–846, 2018 [PMC free article: PMC6128816] [PubMed: 29795415] | Systematic review: Included studies checked for relevance. |
| Baron, Justine, Swaine, Jillian, Presseau, J., Aspinall, Arlene, Jaglal, Susan, White, Barry, Wolfe, Dalton, Grimshaw, Jeremy, Self-management interventions to improve skin care for pressure ulcer prevention in people with spinal cord injuries: a systematic review protocol, Systematic reviews, 5, 150, 2016 [PMC free article: PMC5011862] [PubMed: 27600153] | Published protocol for a systematic review |
| Bayley, M. T., Lamontagne, M. E., Kua, A., Marshall, S., Marier-Deschenes, P., Allaire, A. S., Kagan, C., Truchon, C., Janzen, S., Teasell, R., Swaine, B., Unique features of the INESSS-Onf rehabilitation guidelines for moderate to severe traumatic brain injury: Responding to users’ needs, Journal of Head Trauma Rehabilitation, 33, 296–305, 2018 [PubMed: 30188459] | Results not in PICO: Guideline recommendations for moderate/severe TBI. No raw data presented. Systematic review performed as part of methodology but results and references not presented to check. |
| Beadle, E., Watter, K., Murray, A., Kennedy, A., The integration of telehealth into a community-based interdisciplinary brain injury service, Brain Impairment, 20, 345, 2019 | Published as abstract only |
| Berggren, M., Karlsson, Å, Lindelöf, N., Englund, U., Olofsson, B., Nordström, P., Gustafson, Y., Stenvall, M., Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: a randomized controlled trial, Clinical Rehabilitation, 33, 64–73, 2019 [PMC free article: PMC6311618] [PubMed: 30064264] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=106 in intervention, n=93 in control) |
| Bhattacharyya, R., Agrawal, Y., Elphick, H., Blundell, C., The impact of a new model of hip fracture care at a teaching hospital, Osteoporosis International, 23, S566–S567, 2012 | Published as abstract only |
| Bhattacharyya, Rahul, Agrawal, Yuvraj, Elphick, Heather, Blundell, Chris, A unique orthogeriatric model: a step forward in improving the quality of care for hip fracture patients, International journal of surgery (London, England), 11, 1083–6, 2013 [PubMed: 24120890] | Unclear comparator: Only described as “patients remain primarily under the care of the orthopaedic teams” (p. 1084) |
| Bloemen-Vrencken, J. H. A., de Witte, L. P., Engels, J. P. G. M., van den Heuvel, W. J. A., Post, M. W. M., Transmural care in the rehabilitation sector: implementation experiences with a transmural care model for people with spinal cord injury, International journal of integrated care, 5, e02, 2005 [PMC free article: PMC1395505] [PubMed: 16773154] | Study design not in PICO: No comparison group |
| Bloemen-Vrencken, J. H. A., de Witte, L. P., Post, M. W. M., Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation, Spinal cord, 43, 462–75, 2005 [PubMed: 15838530] | Systematic review: Included studies checked for relevance. |
| Bogie, Kath M., Ho, Chester H., Multidisciplinary approaches to the pressure ulcer problem, Ostomy/wound management, 53, 26–32, 2007 [PubMed: 17978412] | Narrative review |
| Bolster, M. B., Cevallos, S., Beyer, L., Kronenberg, H. M., Leder, B., A model for improved management of fragility fractures: Navigating the fracture liaison service, Arthritis and Rheumatology, 69, 2017 | Published as abstract only |
| Braga, L. W., Da Paz, A. C., Ylvisaker, M., Direct clinician-delivered versus indirect family-supported rehabilitation of children with traumatic brain injury: a randomized controlled trial, Brain Injury, 19, 819–831, 2005 [PubMed: 16175842] | Population not in PICO: ≤ 18 years old. |
| Brasure, Michelle, Lamberty, Greg J., Sayer, Nina A., Nelson, Nathaniel W., Macdonald, Roderick, Ouellette, Jeannine, Wilt, Timothy J., Participation after multidisciplinary rehabilitation for moderate to severe traumatic brain injury in adults: a systematic review, Archives of physical medicine and rehabilitation, 94, 1398–420, 2013 [PubMed: 23348125] | Systematic review: Included studies checked for relevance. |
| Buccellato, K. H., Nordstrom, M., Murphy, J. M., Burdea, G. C., Polistico, K., House, G., Kim, N., Grampurohit, N., Sorensen, J., Isaacson, B. M., et al.,, A Randomized Feasibility Trial of a Novel, Integrative, and Intensive Virtual Rehabilitation Program for Service Members Post-Acquired Brain Injury, Military Medicine, 2019 [PubMed: 31268524] | Comparison not in PICO: Immediate (weeks 0-6) versus delayed (weeks 3-9) outpatient cognitive rehabilitation program. However, immediate versus delayed does not appear to relate to the time of discharge for the patients; same study as Buccellato 2020 |
| Buccellato, Kiara H., Nordstrom, Michelle, Murphy, Justin M., Burdea, Grigore C., Polistico, Kevin, House, Gregory, Kim, Nam, Grampurohit, Namrata, Sorensen, Jeff, Isaacson, Brad M., Pasquina, Paul F., A Randomized Feasibility Trial of a Novel, Integrative, and Intensive Virtual Rehabilitation Program for Service Members Post-Acquired Brain Injury, Military Medicine, 185, e203–e211, 2020 [PubMed: 31268524] | Comparison not in PICO: Immediate (weeks 0-6) versus delayed (weeks 3-9) outpatient cognitive rehabilitation program. However, immediate versus delayed does not appear to relate to the time of discharge for the patients; same study as Buccellato 2019 |
| Burch, D., Bernert, S., Fraser, J. F., Increased physician and physical therapist communication is associated with earlier mobility and decreased length of stay in the cerebrovascular and trauma neuroscience population, NeuroRehabilitation, 43, 195–199, 2018 [PubMed: 30040766] | Study design not in PICO: Non-randomised study with mixed population and less than N=100 in each group of population |
| Burch, D., Bernert, S., Fraser, J. F., Increased physician and physical therapist communication is associated with earlier mobility and decreased length of stay in the cerebrovascular and trauma neuroscience population, Stroke, 47, 2016 [PubMed: 30040766] | Published as abstract only |
| Burgo-Black, L., Hunt, S. C., Implementing a system of integrated post deployment care for returning combat veterans, Journal of General Internal Medicine, Conference, 2012 [PMC free article: PMC3514997] [PubMed: 22648608] | Published as abstract only |
| Burns, A., Aarabi, B., Anderson, P., Arnold, P., Brodke, D., Chiba, K., Dettori, J., Furlan, J., Harrop, J., Holly, L., Howley, S., Jeji, T., Kalsi-Ryan, S., Kotter, M., Kurpad, S., Kwon, B., Marino, R., Martin, A., Massicotte, E., Merli, G., Middleton, J., Nakashima, H., Nagoshi, N., Palmieri, K., Shamji, M., Singh, A., Skelly, A., Tetreault, L., Wilson, J., Yee, A., Fehlings, M., A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the type and timing of rehabilitation, Global Spine Journal, 7, 358S–359S, 2017 [PMC free article: PMC5684839] [PubMed: 29164029] | Published as abstract only |
| Calleja, Pauline, Aitken, Leanne M., Cooke, Marie L., Information transfer for multi-trauma patients on discharge from the emergency department: mixed-method narrative review, Journal of Advanced Nursing, 67, 4–18, 2011 [PubMed: 21158900] | Semi-systematic review emphasising qualitative research/analysis methods. Additionally, it focuses on trauma care and does not mention rehabilitation. |
| Callender, Librada, Brown, Rachel, Driver, Simon, Dahdah, Marie, Collinsworth, Ashley, Shafi, Shahid, Process for developing rehabilitation practice recommendations for individuals with traumatic brain injury, BMC neurology, 17, 54, 2017 [PMC free article: PMC5359914] [PubMed: 28320346] | Technical paper about how to develop an evidence-based guideline; contains no primary or secondary data. |
| Cameron, I. D., Handoll, H. H. G., Finnegan, T. P., Langhorne, P., Multidisciplinary rehabilitation for older people with hip fractures, Cochrane Database of Systematic Reviews, CD007125, 2008 [PMC free article: PMC8586844] [PubMed: 34766330] | Earlier version of Handoll 2009 |
| Cameron, I. D., Handoll, H. H., Finnegan, T. P., Madhok, R., Langhorne, P., Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures, The Cochrane database of systematic reviews, CD000106, 2001 [PubMed: 11686951] | Earlier version of Cameron 2009 |
| Cameron, Ian D., Coordinated multidisciplinary rehabilitation after hip fracture, Disability and rehabilitation, 27, 1081–90, 2005 [PubMed: 16315427] | Narrative review |
| Cameron, Ian D., Handoll, Helen Hg, Finnegan, Terence P., Madhok, Rajan, Langhorne, Peter, WITHDRAWN: Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures, The Cochrane database of systematic reviews, CD000106, 2009 [PubMed: 10796300] | Withdrawn from the Cochrane library as it has been incorporated into another review with an expended scope (Handoll 2009) |
| Campbell, C. V., Cooper, J., Shabir, F., Wills, E., Ong, T., An enhanced therapy service for patients with fractured neck of femur - Service evaluation of a pilot project, Age and Ageing, 46, 2017 | Published as abstract only |
| Canadillas Rueda, R., Domingo Montesinos, N., Natividad Pedreno, M., Comprehensive treatment and secondary prevention of fragility fractures in the elderly in an orthogeriatric unit. Multidisciplinary management of osteoporotic patients pre and post surgery. Advantages and results, Osteoporosis International, 27, S539, 2016 | Published as abstract only |
| Careau, Emmanuelle, Dussault, Julie, Vincent, Claude, Development of interprofessional care plans for spinal cord injury clients through videoconferencing, Journal of interprofessional care, 24, 115–8, 2010 [PubMed: 19705312] | Study design not in PICO: No comparison group |
| Carney, Nancy A., Petroni, Gustavo J., Lujan, Silvia B., Ballarini, Nicolas M., Faguaga, Gabriela A., du Coudray, Hugo E. M., Huddleston, Amy E., Baggio, Gloria M., Becerra, Juan M., Busso, Leonardo O., Dikmen, Sureyya S., Falcone, Roberto, Garcia, Mirta E., Gonzalez Carrillo, Osvaldo R., Medici, Paula L., Quaglino, Marta B., Randisi, Carina A., Saenz, Silvia S., Temkin, Nancy R., Vanella, Elida E., Postdischarge Care of Pediatric Traumatic Brain Injury in Argentina: A Multicenter Randomized Controlled Trial, Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 17, 658–66, 2016 [PMC free article: PMC4938734] [PubMed: 27243414] | Intervention not in PICO: Discharge support related to medical care. Study does not report on patients receiving rehabilitation or social care |
| Carroll, V., The Adult Patient Assessment Tool and care plan, Australian nursing journal (July 1993), 14, 29–32, 2007 [PubMed: 17319187] | Outcomes and population not in PICO: Description of the development of an assessment tool by a multi-disciplinary working group |
| Castillo, Renan C., Wegener, Stephen T., Newell, Mary Zadnik, Carlini, Anthony R., Bradford, Anna N., Heins, Sara E., Wysocki, Elizabeth, Pollak, Andrew N., Teter, Harry, Mackenzie, Ellen J., Improving outcomes at Level I trauma centers: an early evaluation of the Trauma Survivors Network, The journal of trauma and acute care surgery, 74, 1534–40, 2013 [PubMed: 23694884] | Intervention and comparison not in PICO: Trauma survivor network program consisting of self-management course, peer support, information access and provider training standard care versus standard care |
| Chang, C. B., Yang, R. S., Huang, W. J., Chan, D. C., Fracture type on the outcome of patients managed within the fracture liaison and osteoporosis medication management services, Osteoporosis International, 30, S92, 2019 [PMC free article: PMC6626060] [PubMed: 31300660] | Published as abstract only |
| Chudyk, Anna M., Jutai, Jeffrey W., Petrella, Robert J., Speechley, Mark, Systematic review of hip fracture rehabilitation practices in the elderly, Archives of physical medicine and rehabilitation, 90, 246–62, 2009 [PubMed: 19236978] | Systematic review: Included studies checked for relevance. |
| Clark, J., Gill, C., Sprott, A., Joined up thinking: A model for long-term abi rehabilitation after return home, Brain Injury, 26, 432–433, 2012 | Published as abstract only |
| Closa, Conxita, Mas, Miquel A., Santaeugenia, Sebastia J., Inzitari, Marco, Ribera, Aida, Gallofre, Miquel, Hospital-at-home Integrated Care Program for Older Patients With Orthopedic Processes: An Efficient Alternative to Usual Hospital-Based Care, Journal of the American Medical Directors Association, 18, 780–784, 2017 [PubMed: 28578883] | Study design not in PICO: Non-randomised study with less than N=100 in at least 1 intervention group |
| Coetzer, Rudi, Holistic neuro-rehabilitation in the community: is identity a key issue?, Neuropsychological rehabilitation, 18, 766–83, 2008 [PubMed: 18654932] | Narrative review |
| Collins, Nina, Miller, Richard, Kapu, April, Martin, Rita, Morton, Melissa, Forrester, Mary, Atkinson, Shelley, Evans, Bethany, Wilkinson, Linda, Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction, The journal of trauma and acute care surgery, 76, 353–7, 2014 [PubMed: 24398767] | Intervention not in PICO: Acute care nurse practitioner (ACNP) who coordinated acute/ clinical care with a very brief mention of rehabilitation was “The ACNP attended the daily “discharge huddle”™ a team meeting that encompasses T2 [step-down care from ICU] and T3 [trauma nurse practitioner satellite service] NPs [nurse practitioner], case managers, social worker, liaisons to rehabilitation and nursing home facilities, and home health agency staff to facilitate communication and the discharge process." (p. 354). Only outcome reported is length of stay. |
| Cooper, M., Ganda, K., Palmer, A., Seibel, M. J., Cost effectiveness of a targeted intervention to reduce refracture rates: Analysis of a four year prospective controlled study, Journal of Bone and Mineral Research, 26, 2011 | Published as abstract only |
| Cooper, M., Palmer, A., Ganda, K., Seibel, M. J., Cost-effectiveness of a targeted intervention to reduce the rate of refracture: Results ofa 4-year prospective controlled study, Osteoporosis International, 22, S651–S652, 2011 [PubMed: 21107534] | Published as abstract only |
| Cordasco, K. M., Saifu, H., Rubenstein, L. V., Khafaf, M., Doyle, B., Hsiao, J., Orshansky, G., Ganz, D., The ED-PACT tool: Communicating veterans’ care needs after emergency department visits via electronic messages, Journal of General Internal Medicine, 32, S800, 2017 | Published as abstract only |
| Corser, William D., Postdischarge outcome rates influenced by comorbidity and interdisciplinary collaboration, Outcomes management, 8, 45–51, 2004 [PubMed: 14740584] | Study design and population not in PICO: Non-randomised study with less than N=100 in each arm (total N=189). Unclear exactly why population admitted, but n=67 were admitted from medical cardiac services. |
| Crotty, M., Rowett, D., Spurling, L., Giles, L. C., Phillips, P. A., Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial, American Journal Geriatric Pharmacotherapy, 2, 257–264, 2004 [PubMed: 15903284] | Unclear population: Older people being transferred from hospital to long term care facility with no further details. |
| Crotty, M., Whitehead, C. H., Gray, S., Finucane, P. M., Early discharge and home rehabilitation after hip fracture achieves functional improvements: A randomized controlled trial, Clinical Rehabilitation, 16, 406–413, 2002 [PubMed: 12061475] | Study dates not in PICO: 1998-1999 |
| Crouch, D., Taking spinal care into the community, Nursing times, 100, 24–25, 2004 [PubMed: 15307640] | Narrative review |
| Cuthbert, J., Anderson, J., Mason, C., Block, S., Martin, K., Dettmer, J., Weintraub, A., Harrison-Felix, C., Evaluating case management needs and impact for adults with chronic TBI, Brain Injury, 28, 706, 2014 | Published as abstract only |
| Davies Urizar, B., Malanga Ferrari, A., Garcia Fernandez, J. A., Martin De Francisco Murga, E., Alonso Bouzon, C., Rodriguez-Manas, L., Benefits of an orthogeriatric unit, European Geriatric Medicine, 2, S138, 2011 | Published as abstract only |
| De Goumoens, V., Rio, L. M., Jaques, C., Ramelet, A. S., Family-oriented interventions for adults with acquired brain injury and their families: A scoping review, JBI Database of Systematic Reviews and Implementation Reports, 16, 2330–2367, 2018 [PubMed: 30531483] | Systematic review: Included studies checked for relevance. |
| Dibardino, D., Cohen, E. R., Didwania, A., Meta-analysis: Multidisciplinary fall prevention strategies in the acute care inpatient population, Journal of Hospital Medicine, 7, 497–503, 2012 [PubMed: 22371369] | Systematic review: Included studies checked for relevance. |
| Doloresco, L., CARF: symbol of rehabilitation excellence, SCI nursing : a publication of the American Association of Spinal Cord Injury Nurses, 18, 165–172, 2001 [PubMed: 12503464] | Article not available |
| Donohue, Kathleen, Hoevenaars, Richelle, McEachern, Jocelyn, Zeman, Erica, Mehta, Saurabh, Home-Based Multidisciplinary Rehabilitation following Hip Fracture Surgery: What Is the Evidence?, Rehabilitation research and practice, 2013, 875968, 2013 [PMC free article: PMC3877638] [PubMed: 24455275] | Systematic review: Included studies checked for relevance. |
| Dorsey, Julie, Bradshaw, Michelle, Effectiveness of Occupational Therapy Interventions for Lower-Extremity Musculoskeletal Disorders: A Systematic Review, The American journal of occupational therapy : official publication of the American Occupational Therapy Association, 71, 7101180030p1–7101180030p11, 2017 [PubMed: 28027040] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Drago, K., Bernstein, J., Graven, P., Dobbertin, K., Eckstrom, E., Higher quality, lower cost with a geriatrics consult service, Journal of the American Geriatrics Society, 65, S36, 2017 [PubMed: 30094830] | Published as abstract only |
| Driessen, Julia, Bellon, Johanna E., Stevans, Joel, Forsythe, Raquel M., Reynolds, Benjamin R., James, A. Everette, 3rd, Perceived performance and impact of a non-physician-led interprofessional team in a trauma clinic setting, Journal of interprofessional care, 31, 112–114, 2017 [PubMed: 27880082] | Outcomes not in PICO: Team survey responses, consults given and new therapy referrals initiated. |
| Dunn, A. M., Boylston, M., Establishing a consultation service through multidisciplinary rounds, PM and R, 7, S151–S152, 2015 | Published as abstract only |
| Dutton, Richard P., Cooper, Carnell, Jones, Alan, Leone, Susan, Kramer, Mary E., Scalea, Thomas M., Daily multidisciplinary rounds shorten length of stay for trauma patients, The Journal of trauma, 55, 913–9, 2003 [PubMed: 14608165] | Intervention not in PICO: Daily multidisciplinary rounds focused on medical care, not coordination or delivery of rehabilitation or social care. |
| Eicher, Vicki, Murphy, Mary Pat, Murphy, Thomas F., Malec, James F., Progress assessed with the Mayo-Portland Adaptability Inventory in 604 participants in 4 types of post-inpatient rehabilitation brain injury programs, Archives of Physical Medicine and Rehabilitation, 93, 100–7, 2012 [PubMed: 22200388] | Interventions not in PICO: 4 different rehabilitation programmes with different content, not coordination or delivery of rehabilitation or social care. |
| Espinoza, L., Scudder, B., Rosario, E., Patient navigation for traumatic brain injury, Journal of Head Trauma Rehabilitation, Conference, 2013 | Published as abstract only |
| Farba, L., Cypin, I., Spesivtcev, I., The first assessment of the principles of “Co-managed care in elderly patients” in Moscow City hospital #13, Osteoporosis International, 27, S131, 2016 | Published as abstract only |
| Faux, S., Wu, J., Harris, I., Poulos, C., Klein, L., Murray, G., Wilson, S., John, E., Early rehabilitation after hospital admission for road-trauma via an in-reach mobile team; a randomised controlled trial, Archives of Physical Medicine and Rehabilitation, 97, e15–e16, 2016 | Published as abstract only |
| Featherall, J., Brigati, D. P., Faour, M., Messner, W., Higuera, C. A., Implementation of a Total Hip Arthroplasty Care Pathway at a High-Volume Health System: Effect on Length of Stay, Discharge Disposition, and 90-Day Complications, Journal of Arthroplasty, 33, 1675–1680, 2018 [PubMed: 29478678] | Intervention not in PICO: Hip arthroplasty care pathway, including pre-operative, peri-operative and post-operative interventions. Mention of clinical care coordinator in the post-operative section but not able to quantify what is due to care coordinator and what is attributable to other interventions. |
| Fernandez, M. A., Griffin, X. L., Costa, M. L., Management of hip fracture, British medical bulletin, 115, 165–72, 2015 [PubMed: 26311503] | Narrative review |
| Fernandez-Moyano, A., Fernandez-Ojeda, R., Ruiz-Romero, V., Garcia-Benitez, B., Palmero-Palmero, C., Aparicio-Santos, R., Comprehensive care program for elderly patients over 65 years with hip fracture, Revista clinica espanola, 214, 17–23, 2014 [PubMed: 23541310] | Length of stay and readmission data does not have enough details reported to compare results of pre-implementation group and post-implementation group (no mean or standard deviation for the before group and no statistical analysis presented). Barthel Index is only compared between those who survived and those who died during the study period. |
| Fiona, N., Lucinda, M., Margot, P., Gabor, M., Suzanne, M., Bernard, W., Erica, E., Sanjay, G., Implementation of re-fracture prevention of >65 year old inpatient fractured neck of femur prior to discharge, Internal Medicine Journal, 46, 10, 2016 | Published as abstract only |
| Fitzsimmons, R. D., Brain injury case management: The potential and limitations of late-stage intervention - A pilot study, Brain Injury, 17, 947–971, 2003 [PubMed: 14514447] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (total N=22) |
| Flinn, N. A., Kelley, T., Foo, S., Medical home for persons with disabilities: A target for the triple aim, Archives of Physical Medicine and Rehabilitation, 94, e55–e56, 2013 | Published as abstract only |
| Fojas Ma, C. M., Ing, S. W., Phieffer, L., Stephens, J., Southerland, L., Evolution of a fracture prevention program : A review of our experience at the Ohio state university, Endocrine Reviews, 37, 2016 | Published as abstract only |
| Forni, Silvia, Pieralli, Francesca, Sergi, Alessandro, Lorini, Chiara, Bonaccorsi, Guglielmo, Vannucci, Andrea, Mortality after hip fracture in the elderly: The role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients, Archives of Gerontology and Geriatrics, 66, 13–7, 2016 [PubMed: 27174126] | Intervention not in PICO: Multi-disciplinary team designed to acutely treat hip fracture patients in order to decrease time from admission to surgery, rather than multi-disciplinary team for rehabilitation care |
| Franz, Shiney, Muser, Jurgen, Thielhorn, Ulrike, Wallesch, Claus W., Behrens, Johann, Inter-professional communication and interaction in the neurological rehabilitation team: a literature review, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30457016] | Systematic review: Included studies checked for relevance. |
| Fukuda, Haruhisa, Shimizu, Sayuri, Ishizaki, Tatsuro, Has the Reform of the Japanese Healthcare Provision System Improved the Value in Healthcare? A Cost-Consequence Analysis of Organized Care for Hip Fracture Patients, PLoS ONE, 10, e0133694, 2015 [PMC free article: PMC4514762] [PubMed: 26208322] | Comparison not in PICO: Hip fracture care in hospitals autonomously providing integrated care across specialties versus in acute care hospitals and rehabilitative care hospitals providing organized care across separate facilities (the organisation of the care is not further described). |
| Furlan, Andrea D., Irvin, Emma, Munhall, Claire, Giraldo-Prieto, Mario, Fullerton, Laura, McMaster, Robert, Danak, Shivang, Costante, Alicia, Pitzul, Kristen, Bhide, Rohit P., Marchenko, Stanislav, Mahood, Quenby, David, Judy A., Flannery, John F., Bayley, Mark, Rehabilitation service models for people with physical and/or mental disability living in low- and middle-income countries: A systematic review, Journal of Rehabilitation Medicine, 50, 487–498, 2018 [PubMed: 29616278] | Systematic review: Included studies checked for relevance. |
| Gailey, Robert, Gaunaurd, Ignacio, Raya, Michele, Kirk-Sanchez, Neva, Prieto-Sanchez, Luz M., Roach, Kathryn, Effectiveness of an Evidence-Based Amputee Rehabilitation (EBAR) Program: A Pilot Randomized Controlled Trial, Physical therapy, 2020 [PubMed: 31951260] | Intervention not in PICO: Rehabilitation programme designed to occur after participants had completed physical therapy and prosthetic training. |
| Gjerberg, Elisabeth, Flottorp, Signe, Holte, Hilde H., 2008 [PubMed: 29320096] | Article not available |
| Grabljevec, Klemen, Singh, Rajiv, Denes, Zoltan, Angerova, Yvona, Nunes, Renato, Boldrini, Paolo, Delargy, Mark, Laxe, Sara, Kiekens, Carlotte, Varela Donoso, Enrique, Christodoulou, Nicolas, Evidence-based position paper on Physical and Rehabilitation Medicine professional practice for Adults with Acquired Brain Injury. The European PRM position (UEMS PRM Section), European journal of physical and rehabilitation medicine, 54, 971–979, 2018 [PubMed: 30160441] | Systematic review: Included studies checked for relevance. |
| Gregersen, Merete, Morch, Marianne Metz, Hougaard, Kjeld, Damsgaard, Else Marie, Geriatric intervention in elderly patients with hip fracture in an orthopedic ward, Journal of injury & violence research, 4, 45–51, 2012 [PMC free article: PMC3426900] [PubMed: 21502786] | Intervention not in PICO: Multi-disciplinary team designed to acutely treat hip fracture patients in order to decrease time from admission to surgery, rather than multi-disciplinary team for rehabilitation care |
| Grigoryan, K., Javedan, H., Rudolph, J., Ortho-geriatric models and optimal outcomes: A systematic review and meta-analysis, Journal of the American Geriatrics Society, 61, S8–S9, 2013 | Published as abstract only |
| Grigoryan, Konstantin V., Javedan, Houman, Rudolph, James L., Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis, Journal of Orthopaedic Trauma, 28, e49–55, 2014 [PMC free article: PMC3909556] [PubMed: 23912859] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Grill, E., Ewert, T., Lipp, B., Mansmann, U., Stucki, G., Effectiveness of a community-based 3-year advisory program after acquired brain injury, European Journal of Neurology, 14, 1256–65, 2007 [PubMed: 17956446] | Mixed population: Only 310/1181 were in PICO (traumatic brain injury) but results are not presented separately for target population. |
| Grobe, K. F., Lin, S. J., Ababneh, A. F., Orozco, E. M., Maxey, K., Smarda, M. J., Lopez, A. R., The feasibility and effectiveness of an internet-based exercise program in individuals with spinal cord injury, Cardiopulmonary Physical Therapy Journal, 31, e16–e17, 2020 | Published as abstract only |
| Gupta, A., The effectiveness of geriatrician-led comprehensive hip fracture collaborative care in a new acute hip unit based in a general hospital setting in the UK, The journal of the Royal College of Physicians of Edinburgh, 44, 20–6, 2014 [PubMed: 24995442] | Intervention not in PICO: Multi-disciplinary team designed to acutely care for hip fracture patients pre- and post-operatively, rather than multidisciplinary team for coordination of rehabilitation. |
| Guy, S., Kras-Dupuis, A., Wolfe, D., Hsieh, J., Walia, S., Askes, H., Spinal cord injury best practice implementation for pressure ulcer prevention: Initial implementation results, Archives of Physical Medicine and Rehabilitation, 94, e25, 2013 [PubMed: 30419231] | Published as abstract only |
| Haan, James M., Dutton, Richard P., Willis, Michelle, Leone, Susan, Kramer, Mary E., Scalea, Thomas M., Discharge rounds in the 80-hour workweek: importance of the trauma nurse practitioner, The Journal of trauma, 63, 339–43, 2007 [PubMed: 17693833] | Intervention not in PICO: Daily multidisciplinary rounds focused on medical care, not coordination or delivery of rehabilitation or social care. |
| Halbert, J., Crotty, M., Whitehead, C., Cameron, I., Kurrle, S., Graham, S., Handoll, H., Finnegan, T., Jones, T., Foley, A., Shanahan, M., Multi-disciplinary rehabilitation after hip fracture is associated with improved outcome: A systematic review, Journal of Rehabilitation Medicine, 39, 507–512, 2007 [PubMed: 17724548] | Systematic review: Included studies checked for relevance. |
| Hall, Erin C., Tyrrell, Rebecca, Scalea, Thomas M., Stein, Deborah M., Trauma Transitional Care Coordination: protecting the most vulnerable trauma patients from hospital readmission, Trauma surgery & acute care open, 3, e000149, 2018 [PMC free article: PMC5887824] [PubMed: 29766133] | No information presented for comparison group, including number of participants. |
| Hammond, Flora M., Gassaway, Julie, Abeyta, Nichola, Freeman, Erma S., Primack, Donna, Kreider, Scott E. D., Whiteneck, Gale, Outcomes of social work and case management services during inpatient spinal cord injury rehabilitation: the SCIRehab project, The journal of spinal cord medicine, 35, 611–23, 2012 [PMC free article: PMC3522900] [PubMed: 23318040] | Study design not in PICO: No intervention. |
| Handoll, H. H. G., Cameron, I. D., Mak, J. C. S., Finnegan, T. P., Multidisciplinary rehabilitation for older people with hip fractures, Cochrane Database of Systematic Reviews, CD007125, 2009 [PubMed: 19821396] | Systematic review: Included studies checked for relevance. |
| Hart, Tessa, Brockway, Jo Ann, Maiuro, Roland D., Vaccaro, Monica, Fann, Jesse R., Mellick, David, Harrison-Felix, Cindy, Barber, Jason, Temkin, Nancy, Anger Self-Management Training for Chronic Moderate to Severe Traumatic Brain Injury: Results of a Randomized Controlled Trial, The Journal of head trauma rehabilitation, 32, 319–331, 2017 [PMC free article: PMC5593756] [PubMed: 28520666] | Intervention not in PICO: Treatment protocol for anger self-management training. No mention of co-ordination or delivery of rehabilitation. |
| Hart, Tessa, Driver, Simon, Sander, Angelle, Pappadis, Monique, Dams-O’Connor, Kristen, Bocage, Claire, Hinkens, Emma, Dahdah, Marie N., Cai, Xinsheng, Traumatic brain injury education for adult patients and families: a scoping review, Brain Injury, 32, 1295–1306, 2018 [PMC free article: PMC6321983] [PubMed: 30084694] | Systematic review: Included studies checked for relevance. |
| Hartwell, J., Albanese, K., Retterer, A., Martin, S., O’Mara, M. S., A trauma patient advocate is a valuable addition to the multidisciplinary trauma team: A process improvement project, American Surgeon, 82, S183–S185, 2016 [PubMed: 27657560] | No study results presented in paper |
| He, J., Wei, Q., Effect observation of community rehabilitation model on generic set of ICF for patients with TBI, Neurorehabilitation and Neural Repair, 32, 323–324, 2018 | Published as abstract only |
| Heinemann, A. W., Corrigan, J. D., Moore, D., Case Management for Traumatic Brain Injury Survivors with Alcohol Problems, Rehabilitation Psychology, 49, 156–166, 2004 | Intervention not in PICO: Comprehensive case management for people with traumatic brain injury and postinjury substance abuse |
| Heppenstall, C. P., Hanger, H. C., Wilkinson, T. J., The canterbury community rehabilitation, enablement and support team (CREST) service: A novel service to support wellbeing and independence in the community, Age and Ageing, 48, 2019 | Published as abstract only |
| Herrera-Espiñeira, C., Rodríguez del Águila Mdel, M., Navarro Espigares, J. L., Godoy Montijano, A., García Priego, A., Rodríguez, J. G., Sánchez, I. R., Effect of a telephone care program after hospital discharge from a trauma surgery unit, Gaceta sanitaria, 25, 133–138, 2011 [PubMed: 21334787] | Article in Spanish |
| Heyman, Noemi, Etzion, Isaac, Ben Natan, Merav, A coordination project for improvement of osteoporosis medication use among patients who sustained an osteoporotic fracture: The Israeli experience, Osteoporosis and Sarcopenia, 4, 134–139, 2018 [PMC free article: PMC6372825] [PubMed: 30775556] | Outcomes not in PICO: Osteoporosis medication use |
| Ho, W. S., Chan, H. H., Ying, S. Y., Cheng, H. S., Wong, C. S., Skin care in burn patients: A team approach, Burns, 27, 489–491, 2001 [PubMed: 11451603] | Study dates not in PICO: 1992-January 2000. Results not presented separately for the 1 month that was in PICO (January 2000) |
| Holliday, Anna, Samanta, Damayanti, Budinger, Julie, Hardway, Jessica, Bethea, Audis, An Outcome Analysis of Nurse Practitioners in Acute Care Trauma Services, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 24, 365–370, 2017 [PMC free article: PMC5929127] [PubMed: 29117053] | Intervention not in PICO: Nurse practitioners facilitated transfer throughout acute trauma services (including intensive care, floor, and post-acute clinic). Apart from placing the order for a rehabilitation consultation, there is no further mention of coordination of rehabilitation services. |
| Holstege, M. S., Bakkers, E., van Balen, R., Gussekloo, J., Achterberg, W. P., Caljouw, M. A., Structured scoring of supporting nursing tasks to enhance early discharge in geriatric rehabilitation: The BACK-HOME quasi-experimental study, International journal of nursing studies, 64, 13–18, 2016 [PubMed: 27657663] | Population not in PICO: Only 31% (reference) and 34% (intervention) were admitted for traumatic injury. Results not presented separately for cause of admission. |
| Holstege, M. S., Caljouw, M. A. A., Van Balen, R., Gussekloo, J., Achterberg, W. P., Effectiveness of innovations in geriatric rehabilitation. The SINGER Study, European Geriatric Medicine, 4, S109–S110, 2013 | Published as abstract only |
| Hossain, M. S., Harvey, L. A., Rahman, M. A., Bowden, J. L., Islam, M. S., Taylor, V., Muldoon, S., Herbert, R. D., A pilot randomised trial of community-based care following discharge from hospital with a recent spinal cord injury in Bangladesh, Clinical Rehabilitation, 31, 781–789, 2017 [PubMed: 27311454] | Unclear population: Inclusion criteria states participants with both traumatic and nontraumatic spinal cord injury. No further information about what proportions were traumatic, and results not presented separately for target population. |
| Houlihan, B., Brody, M., Skeels, S., Pernigotti, D., Zazula, J., Burnett, S., Green, C., Seetharama, S., Hasiotis, S., Belliveau, T., Rosenblum, D., Jette, A., RCT of peer-led phone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management, Archives of Physical Medicine and Rehabilitation, 98, e152, 2017 [PubMed: 28284835] | Published as abstract only |
| Houlihan, Bethlyn Vergo, Brody, Miriam, Everhart-Skeels, Sarah, Pernigotti, Diana, Burnett, Sam, Zazula, Judi, Green, Christa, Hasiotis, Stathis, Belliveau, Timothy, Seetharama, Subramani, Rosenblum, David, Jette, Alan, Randomized Trial of a Peer-Led, Telephone-Based Empowerment Intervention for Persons With Chronic Spinal Cord Injury Improves Health Self-Management, Archives of Physical Medicine and Rehabilitation, 98, 1067–1076.e1, 2017 [PubMed: 28284835] | Intervention not in PICO: ‘My Care My Call’ designed for people with SCI already in the community. No mention of coordination or delivery of rehabilitation or social care during transfer. |
| Hums, Wendy, Williams, Julianne, Dedicated trauma care unit: an outcome-based model, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 12, 21–6, 2005 [PubMed: 15916314] | Narrative review |
| Jaber, Ala’a F., Hartwell, Julie, Radel, Jeff D., Interventions to Address the Needs of Adults With Postconcussion Syndrome: A Systematic Review, The American journal of occupational therapy : official publication of the American Occupational Therapy Association, 73, 7301205020p1–7301205020p12, 2019 [PubMed: 30839257] | Article not available |
| Johansen, Inger, Lindbaek, Morten, Stanghelle, Johan K., Brekke, Mette, Structured community-based inpatient rehabilitation of older patients is better than standard primary health care rehabilitation: an open comparative study, Disability and Rehabilitation, 34, 2039–46, 2012 [PubMed: 22452632] | Study design not in PICO: Non-randomised study. Although N=100 in one of the comparison groups, patients had mixed aetiologies (for example, 16/100 had stroke) |
| Johnson, M. K., Yanko, J. R., Collaborative practice: a successful model, SCI nursing : a publication of the American Association of Spinal Cord Injury Nurses, 18, 7–10, 2001 [PubMed: 12035480] | Article not available |
| Jones, Taryn M., Dean, Catherine M., Hush, Julia M., Dear, Blake F., Titov, Nickolai, A systematic review of the efficacy of self-management programs for increasing physical activity in community-dwelling adults with acquired brain injury (ABI), Systematic reviews, 4, 51, 2015 [PMC free article: PMC4422226] [PubMed: 25927591] | Systematic review: Included studies checked for relevance. |
| Jonsson, A., Gustafson, Y., Scholl, M., Hansen, F. R., Saarela, M., Nygaard, H., Laake, K., Jonsson, P. V., Valvanne, J., Dehlin, O., Geriatric rehabilitation as an integral part of geriatric medicine in the Nordic countries, Danish Medical Bulletin, 50, 439–445, 2003 [PubMed: 14694856] | Narrative review |
| Kammerlander, C., Gosch, M., Blauth, M., Lechleitner, M., Luger, T. J., Roth, T., The Tyrolean Geriatric Fracture Center: an orthogeriatric co-management model, Zeitschrift fur Gerontologie und Geriatrie, 44, 363–7, 2011 [PubMed: 22159829] | Study design not in PICO: No comparison group. |
| Kapu, A., Jones, P., Financial impact of adding acute care nurse practitioners (ACNPs) to inpatient models of care, Critical Care Medicine, 40, 27, 2012 | Published as abstract only |
| Karlsson, A., Berggren, M., Gustafson, Y., B, Olofsson, Lindelöf, N., Stenvall, M., Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial, Journal of the American Medical Directors Association, 17, 464.e9–e464.e15, 2016 [PubMed: 26975205] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard inpatient rehabilitation but the intervention group received Geriatric Interdisciplinary Home Rehabilitation after discharge which included a High-Intensity Functional Exercise programme and medical care. |
| Karlsson, A., Lindelof, N., Olofsson, B., Berggren, M., Gustafson, Y., Nordstrom, P., Stenvall, M., Effects of Geriatric Interdisciplinary Home Rehabilitation on Independence in Activities of Daily Living in Older People With Hip Fracture: A Randomized Controlled Trial, Archives of Physical Medicine and Rehabilitation, 2020 [PubMed: 31935353] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard inpatient rehabilitation but the intervention group received Geriatric Interdisciplinary Home Rehabilitation after discharge which included a High-Intensity Functional Exercise programme and medical care. |
| Kennedy, K., Establishing an orthopaedic physiotherapy practitioner role on the wards of an acute trauma hospital, Physiotherapy (United Kingdom), 97, eS1529, 2011 | Published as abstract only |
| Khan, F., Amatya, B., Hoffman, K., Systematic review of multidisciplinary rehabilitation in patients with multiple trauma, The British journal of surgery, 99 Suppl 1, 88–96, 2012 [PubMed: 22441861] | Systematic review: Included studies checked for relevance. |
| Khan, S. K., Shirley, M. D., Glennie, C., Fearon, P. V., Deehan, D. J., Achieving best practice tariff may not reflect improved survival after hip fracture treatment, Clinical Interventions in Aging, 9, 2097–2102, 2014 [PMC free article: PMC4257023] [PubMed: 25489240] | Intervention not in PICO: Best practice tariffs for achieving targets, but no information presented on how these were achieved so no information on coordination and delivery of rehabilitation or social care. |
| Khan, S. K., Weusten, A., Bonczek, S., Tate, A., Port, A., The Best Practice Tariff helps improve management of neck of femur fractures: A completed audit loop, British Journal of Hospital Medicine, 74, 644–647, 2013 [PubMed: 24220529] | Population not in PICO: Inclusion criteria includes pathological hip fractures. Results not presented separately for target population. |
| Kiel, S., Zimak, C., Chenot, J. F., Schmidt, C. O., Evaluation of an ambulatory geriatric rehabilitation program - results of a matched cohort study based on claims data, BMC geriatrics, 20, 30, 2020 [PMC free article: PMC6990495] [PubMed: 31996158] | Study design not in PICO: Case-control design |
| Kind, A., Polnaszek, B., Hovanes, M., Smith, M., Designation of a clinician for post-hospital follow-up care and 30-day rehospitalizations in patients discharged to nursing homes and rehabilitation facilities, Journal of the American Geriatrics Society, 61, S16, 2013 | Published as abstract only |
| Koo, W. W. H., Hip care clinic: Improving osteoporosis treatment after a hip fracture, Osteoporosis International, 25, 609, 2014 | Published as abstract only |
| Kooijmans, H., Post, M. W. M., Stam, H. J., van der Woude, L. H. V., Spijkerman, D. C. M., Snoek, G. J., Bongers-Janssen, H. M. H., van Koppenhagen, C. F., Twisk, J. W., Bussmann, J. B. J., Effectiveness of a Self-Management Intervention to Promote an Active Lifestyle in Persons With Long-Term Spinal Cord Injury: The HABITS Randomized Clinical Trial, Neurorehabilitation and Neural Repair, 31, 991–1004, 2017 [PubMed: 29256337] | Intervention not in PICO: Self-management intervention designed to increase physical activity in chronic SCI. No mention of coordination or delivery of rehabilitation or social care. |
| Krulova, A., Vackova, J., Svestkova, O., Community-based rehabilitation system for people with acquired brain injury in the Czech Republic (from the point of view of occupational therapist), Brain Injury, 31, 852–853, 2017 | Published as abstract only |
| Kurowski, Brad G., Taylor, H. Gerry, McNally, Kelly A., Kirkwood, Michael W., Cassedy, Amy, Horn, Paul S., Stancin, Terry, Wade, Shari L., Online Family Problem-Solving Therapy (F-PST) for Executive and Behavioral Dysfunction After Traumatic Brain Injury in Adolescents: A Randomized, Multicenter, Comparative Effectiveness Clinical Trial, The Journal of head trauma rehabilitation, 2019 [PMC free article: PMC7205575] [PubMed: 31834062] | Outcomes not in PICO: Behaviour Rating Inventory of Executive Function, Global Executive Composite, Behaviour Regulation Index, Metacognition Index and Strengths and Difficulties Questionnaire |
| Kusen, J. Q., Schafroth, B., Poblete, B., van der Vet, P. C. R., Link, B. C., Wijdicks, F. J. G., Babst, R. H., Beeres, F. J. P., The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: an observational study, Archives of Orthopaedic and Trauma Surgery, 139, 1705–1712, 2019 [PubMed: 31309288] | Intervention not in PICO: Not concerned with the coordination of rehabilitation and social care for trauma patients while they are transferring between inpatients and outpatients. inpatients. Included in the review for coordination while inpatients. |
| Lamb, Laura C., Montgomery, Stephanie C., Wong Won, Brian, Harder, Siobhan, Meter, Jeffrey, Feeney, James M., A multidisciplinary approach to improve the quality of care for patients with fragility fractures, Journal of orthopaedics, 14, 247–251, 2017 [PMC free article: PMC5362133] [PubMed: 28367005] | Intervention not in PICO: Not concerned with the coordination of rehabilitation and social care for trauma patients while they are transferring between inpatients and outpatients. inpatients. Included in the review for coordination while inpatients. |
| Lannin, Natasha, Carr, Belinda, Allaous, Jeanine, Mackenzie, Bronwyn, Falcon, Alex, Tate, Robyn, A randomized controlled trial of the effectiveness of handheld computers for improving everyday memory functioning in patients with memory impairments after acquired brain injury, Clinical Rehabilitation, 28, 470–81, 2014 [PubMed: 24452701] | Comparison not in PICO: Electronic vs non-electronic memory aid after discharge |
| Lathbury, K., The road ahead-managing a spinal cord injury, The Case manager, 11, 55–7, 2000 [PubMed: 11935641] | Narrative review |
| Latz, David, Bergermann, Anja, Jungnitsch, Jeannie, Grassmann, Jan Peter, Schiffner, Erik, Gahr, Britta, Tank, Anne, Windolf, Joachim, Ritz-Timme, Stefanie, Gras, Lilly, Jungbluth, Pascal, Characterisation of Victims Of Violence in the A & E Department and Analysis of the Acceptance of a Medico-Legal Expertise Centre After its Implementation vs. Multi-Year Consolidation, Charakterisierung unfallchirurgischer Gewaltopfer und Erfassung der Inanspruchnahme nach Implementierung und mehrjahriger Etablierung einer rechtsmedizinischen Gewaltopferambulanz., 157, 426–433, 2019 [PubMed: 30481835] | Population not in PICO: People presenting to A&E without admission |
| Lau, T. W., Leung, F., Siu, D., Wong, G., Luk, K. D. K., Geriatric hip fracture clinical pathway: The Hong Kong experience, Osteoporosis International, 21, S627–S636, 2010 [PMC free article: PMC2974932] [PubMed: 21058003] | No information presented on historical comparison group, including number of participants |
| Laver, Kate, Lannin, Natasha A., Bragge, Peter, Hunter, Peter, Holland, Anne E., Tavender, Emma, O’Connor, Denise, Khan, Fary, Teasell, Robert, Gruen, Russell, Organising health care services for people with an acquired brain injury: an overview of systematic reviews and randomised controlled trials, BMC health services research, 14, 397, 2014 [PMC free article: PMC4263199] [PubMed: 25228157] | Systematic review: Included studies checked for relevance. |
| Leal, J., Gray, A. M., Hawley, S., Prieto-Alhambra, D., Delmestri, A., Arden, N. K., Cooper, C., Javaid, M. K., Judge, A., Cost-Effectiveness of Orthogeriatric and Fracture Liaison Service Models of Care for Hip Fracture Patients: A Population-Based Study, Journal of Bone and Mineral Research, 32, 203–211, 2017 [PMC free article: PMC5321497] [PubMed: 27632945] | Outcomes not in PICO: 30 day mortality, 1 year mortality, risk of 2nd fracture and assorted intervention cost measures |
| Leclercq, M. M., For the return at home: Mobil teams brain-injury, Annals of Physical and Rehabilitation Medicine, 57, e411, 2014 | Published as abstract only |
| Lee, John C., Horst, Michael, Rogers, Amelia, Rogers, Frederick B., Wu, Daniel, Evans, Tracy, Edavettal, Mathew, Checklist-styled daily sign-out rounds improve hospital throughput in a major trauma center, The American surgeon, 80, 434–40, 2014 [PubMed: 24887721] | Intervention not in PICO: Checklist designed to coordinate medical care of trauma patients rather than coordination or delivery of rehabilitation or social care |
| Lee, S. Y., Amatya, B., Judson, R., Truesdale, M., Reinhardt, J. D., Uddin, T., Xiong, X. H., Khan, F., Clinical practice guidelines for rehabilitation in traumatic brain injury: a critical appraisal, Brain Injury, 33, 1263–1271, 2019 [PubMed: 31314607] | Review of guidelines. References checked for possible included studies - none were identified. |
| Lems, W. F., Dreinhofer, K. E., Bischoff-Ferrari, H., Blauth, M., Czerwinski, E., Da Silva, J., Herrera, A., Hoffmeyer, P., Kvien, T., Maalouf, G., Marsh, D., Puget, J., Puhl, W., Poor, G., Rasch, L., Roux, C., Schuler, S., Seriolo, B., Tarantino, U., Van Geel, T., Woolf, A., Wyers, C., Geusens, P., EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures, Annals of the Rheumatic Diseases, 76, 802–810, 2017 [PubMed: 28007756] | Systematic review: Included studies checked for relevance. |
| Leung, Andraay Hon-Chi, Lam, Tsz-Ping, Cheung, Wing-Hoi, Chan, Tan, Sze, Pan-Ching, Lau, Thomas, Leung, Kwok-Sui, An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study, The Journal of trauma, 71, 1390–4, 2011 [PubMed: 22002614] | Intervention not in PICO: Orthogeriatric Collaborative Programme consisting of geriatric reviews. Aim was to optimise patient condition for surgery and to address previously undiagnosed medical problems. |
| Li, L., Dai, J. X., Xu, L., Huang, Z. X., Pan, Q., Zhang, X., Jiang, M. Y., Chen, Z. H., The effect of a rehabilitation nursing intervention model on improving the comprehensive health status of patients with hand burns, Burns, 43, 877–885, 2017 [PubMed: 28062082] | Intervention not in PICO: Nursing intervention involving elements of occupational therapy and psychological treatment rather than interventions comparing the coordination and/or delivery of rehabilitation or social services |
| Lin, Francis O. Y., Luk, James K. H., Chan, T. C., Mok, Winnie W. Y., Chan, Felix H. W., Effectiveness of a discharge planning and community support programme in preventing readmission of high-risk older patients, Hong Kong medical journal = Xianggang yi xue za zhi, 21, 208–16, 2015 [PubMed: 25904292] | Population not in PICO: Home-dwelling older patients aged >60 years admitted to the general medical wards. Only 10% admitted through falls, results not presented separately for target population. |
| Lin, L., Wade, C., Comprehensive prevention and management of pressure ulcers in an acute inpatient rehabilitation facility: An evidence ebased assessment, PM and R, 8, S182–S183, 2016 [PubMed: 27672832] | Published as abstract only |
| Linden, M., Hawley, C., Blackwood, B., Evans, J., Anderson, V., O’Rourke, C., Technological aids for the rehabilitation of memory and executive functioning in children and adolescents with acquired brain injury, Cochrane Database of Systematic Reviews, 2016 [PMC free article: PMC6457968] [PubMed: 27364851] | Systematic review: Included studies checked for relevance. |
| Ling, Shi-Neng James, Kleimeyer, Christopher, Lynch, Genni, Burmeister, Elizabeth, Kennedy, Diana, Bell, Kate, Watkins, Leith, Cooke, Cameron, Can geriatric hip fractures be managed effectively within a level 1 trauma center?, Journal of Orthopaedic Trauma, 29, 160–4, 2015 [PubMed: 25699541] | Intervention not in PICO: Coordination of acute management of hip fracture, rather than rehabilitation. |
| Lisk, R., Krasuski, M., Watters, H., Parsons, C., Yeong, K., 12 months impact of an orthopaedic early supportive discharge (OSD) team in our hip fracture service, European Geriatric Medicine, 6, S150, 2015 [PMC free article: PMC6334156] [PubMed: 30958784] | Published as abstract only |
| Liu, Vincent X., Rosas, Efren, Hwang, Judith, Cain, Eric, Foss-Durant, Anne, Clopp, Molly, Huang, Mengfei, Lee, Derrick C., Mustille, Alex, Kipnis, Patricia, Parodi, Stephen, Enhanced Recovery After Surgery Program Implementation in 2 Surgical Populations in an Integrated Health Care Delivery System, JAMA Surgery, 152, e171032, 2017 [PMC free article: PMC5568841] [PubMed: 28492816] | Intervention not in PICO: Enhanced recovery after surgery programme designed to impact peri-operative management and does not include rehabilitation or social care. |
| Lloyd-James, Lucy, Facing reality: discharge challenges after neuro-rehabilitation, Paediatric nursing, 18, 28, 2006 [PubMed: 16881499] | Narrative review |
| Lohse, Grant R., Leopold, Seth S., Theiler, Susan, Sayre, Cindy, Cizik, Amy, Lee, Michael J., Systems-based safety intervention: reducing falls with injury and total falls on an orthopaedic ward, The Journal of bone and joint surgery. American volume, 94, 1217–22, 2012 [PubMed: 22760390] | Population not in PICO: Mixture of traumatic and non-traumatic with results not reported separately for target population |
| Losh, Joseph, Duncan, Thomas K., Diaz, Graal, Lee, HyeSun, Romero, Javier, Multidisciplinary Patient Management Improves Mortality in Geriatric Trauma Patients, The American surgeon, 85, 230–233, 2019 [PubMed: 30819305] | Intervention not in PICO: Multi-disciplinary medical trauma care, not rehabilitation |
| Lumba-Brown, A., Yeates, K. O., Sarmiento, K., Breiding, M. J., Haegerich, T. M., Gioia, G. A., Turner, M., Benzel, E. C., Suskauer, S. J., Giza, C. C., Joseph, M., Broomand, C., Weissman, B., Gordon, W., Wright, D. W., Moser, R. S., McAvoy, K., Ewing-Cobbs, L., Duhaime, A. C., Putukian, M., Holshouser, B., Paulk, D., Wade, S. L., Herring, S. A., Halstead, M., Keenan, H. T., Choe, M., Christian, C. W., Guskiewicz, K., Raksin, P. B., Gregory, A., Mucha, A., Taylor, H. G., Callahan, J. M., Dewitt, J., Collins, M. W., Kirkwood, M. W., Ragheb, J., Ellenbogen, R. G., Spinks, T. J., Ganiats, T. G., Sabelhaus, L. J., Altenhofen, K., Hoffman, R., Getchius, T., Gronseth, G., Donnell, Z., O’Connor, R. E., Timmons, S. D., Diagnosis and Management of Mild Traumatic Brain Injury in Children: A Systematic Review, JAMA Pediatrics, 172, 2018 [PubMed: 30193325] | Systematic review: Included studies checked for relevance.. |
| Mackey, Patricia A., Rosenthal, Laura D., Mi, Lanyu, Whitaker, Michael D., Subsequent Fracture Prevention in Patients 50 Years and Older With Fragility Fractures: A Quality Improvement Initiative, Journal for healthcare quality : official publication of the National Association for Healthcare Quality, 41, 17–22, 2019 [PubMed: 29553966] | Intervention not in PICO: Osteoporosis education, screening and treatment. |
| Malec, J. F., Eicher, V., Murphy, M. P., Murphy, T. F., Progress assessed with the mayo-portland adaptability inventory through the client outcome system for 604 participants in four types of postacute brain injury rehabilitation programs, Brain Impairment, 12, 68, 2011 | Published as abstract only |
| Malec, J., Eicher, V., Murphy, M. P., Murphy, T., Progress in four postacute brain rehabilitation program types compared through the MPAI-4 outcome info system, Archives of Physical Medicine and Rehabilitation, 92, 1698, 2011 | Published as abstract only |
| Mallick, Emad, Gulihar, Abhinav, Taylor, Grahame, Furlong, Andrew, Pandey, Radhakant, Impact of organisational changes on fracture neck of femur management, Annals of the Royal College of Surgeons of England, 93, 61–6, 2011 [PMC free article: PMC3293276] [PubMed: 20955664] | Intervention not in PICO: Project group aimed at changing surgical and medical management of hip fracture. No mention of rehabilitation. |
| Man, D. W., Soong, W. Y., Tam, S. F., Hui-Chan, C. W., Self-efficacy outcomes of people with brain injury in cognitive skill training using different types of trainer-trainee interaction, Brain Injury, 20, 959–970, 2006 [PubMed: 17062427] | Population not in PICO: Only 16/103 patients within PICO with results not reported separately for the target population. |
| Mangram, Alicia J., Shifflette, Vanessa K., Mitchell, Christopher D., Johnson, Van A., Lorenzo, Manuel, Truitt, Micheal S., Goel, Anuj, Lyons, Mark, Dunn, Ernest L., The creation of a geriatric trauma unit “G-60”, The American surgeon, 77, 1144–6, 2011 [PubMed: 21944622] | Study design not in PICO: Non-randomised study with less than N=100 in 1 arm (n=150 in intervention group, n=78 in control group) |
| Massey, T., Smith, S., Bezzina, C., Ball, A., Specialist rehabilitation in a major trauma centre: It’s not just about saving lives, Brain Injury, 28, 655, 2014 | Published as abstract only |
| Mayo-Wilson, Evan, Grant, Sean, Burton, Jennifer, Parsons, Amanda, Underhill, Kristen, Montgomery, Paul, Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis, PLoS ONE, 9, e89257, 2014 [PMC free article: PMC3951196] [PubMed: 24622676] | Systematic review: Included studies checked for relevance. |
| McMartin, K., Discharge planning in chronic conditions: An evidence-based analysis, Ontario Health Technology Assessment Series, 13, 1–72, 2013 [PMC free article: PMC3804053] [PubMed: 24167538] | Systematic review: Included studies checked for relevance. |
| Meaney, Mark, Divided loyalties in a brain injury case, The Case manager, 14, 30–72, 2003 [PubMed: 12649687] | Case report |
| Miller, Megan W., Emeny, Rebecca T., Freed, Gary L., Reduction of Hospital-acquired Pressure Injuries Using a Multidisciplinary Team Approach: A Descriptive Study, Wounds : a compendium of clinical research and practice, 31, 108–113, 2019 [PMC free article: PMC6586476] [PubMed: 30802207] | Population not in PICO: Hospital-wide implementation, with no separation of trauma and non-trauma patients |
| Mittal, Chikul, Lee, Hsien Chieh Daniel, Goh, Kiat Sern, Lau, Cheng Kiang Adrian, Tay, Leeanna, Siau, Chuin, Loh, Yik Hin, Goh, Teck Kheng Edward, Sandi, Chit Lwin, Lee, Chien Earn, ValuedCare program: a population health model for the delivery of evidence-based care across care continuum for hip fracture patients in Eastern Singapore, Journal of orthopaedic surgery and research, 13, 129, 2018 [PMC free article: PMC5977502] [PubMed: 29848378] | Intervention not in PICO: ValuedCare involved delivery of pre- and post-operative hip fracture care. No mention of delivery or coordination of rehabilitation or social care |
| Momosaki, Ryo, Kakuda, Wataru, Yamada, Naoki, Abo, Masahiro, Impact of board-certificated physiatrists on rehabilitation outcomes in elderly patients after hip fracture: An observational study using the Japan Rehabilitation Database, Geriatrics & gerontology international, 16, 963–8, 2016 [PubMed: 26311043] | Intervention not in PICO: Not concerned with the coordination of rehabilitation and social care for trauma patients while they are transferring between inpatients and outpatients. inpatients. Included in the review for coordination while inpatients. |
| Morris, D. S., Reilly, P., Rohrbach, J., Telford, G., Kim, P., Sims, C. A., The influence of unit-based nurse practitioners on hospital outcomes and readmission rates for patients with trauma, Journal of Trauma and Acute Care Surgery, 73, 474–478, 2012 [PubMed: 22846959] | Intervention not in PICO: Unit-based nurse practitioners are involved in delivering acute trauma care, not delivery and coordination of rehabilitation or social care |
| Murphy, R. P., Reddin, C., Murphy, E. P., Waters, R., Murphy, C. G., Canavan, M., Key Service Improvements After the Introduction of an Integrated Orthogeriatric Service, Geriatric Orthopaedic Surgery and Rehabilitation, 10, 2019 [PMC free article: PMC6906332] [PubMed: 31853381] | Intervention not in PICO: Integrated orthogeriatric service designed to streamline pre- and post-operative care for hip fracture. No mention of delivery or coordination of rehabilitation or social care |
| Naeem, F., Rodriguez, S., MacRae, A., Implementation of an analgesia and bowels protocol to improve patient care after hip fracture, Age and Ageing, 48, 2019 | Published as abstract only |
| Naglie, Gary, Tansey, Catherine, Kirkland, James L., Ogilvie-Harris, Darryl J., Detsky, Allan S., Etchells, Edward, Tomlinson, George, O’Rourke, Keith, Goldlist, Barry, Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial, CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 167, 25–32, 2002 [PMC free article: PMC116636] [PubMed: 12137074] | Study years not in PICO: 1993-1997 |
| Nakase-Richardson, Risa, Stevens, Lillian Flores, Tang, Xinyu, Lamberty, Greg J., Sherer, Mark, Walker, William C., Pugh, Mary Jo, Eapen, Blessen C., Finn, Jacob A., Saylors, Mimi, Dillahunt-Aspillaga, Christina, Adams, Rachel Sayko, Garofano, Jeffrey S., Comparison of the VA and NIDILRR TBI Model System Cohorts, The Journal of Head Trauma Rehabilitation, 32, 221–233, 2017 [PubMed: 28678118] | Comparison not in PICO: Comparison between population characteristics of 2 databases contributing to Traumatic Brain Injury Model System |
| Niemeijer, Gerard C., Flikweert, Elvira, Trip, Albert, Does, Ronald J. M. M., Ahaus, Kees T. B., Boot, Anja F., Wendt, Klaus W., The usefulness of lean six sigma to the development of a clinical pathway for hip fractures, Journal of Evaluation in Clinical Practice, 19, 909–14, 2013 [PubMed: 22780308] | Intervention not in PICO: Lean Six Sigma aimed at decreasing the length of stay in hospital rather than coordinating or delivering rehabilitation |
| Nizamoglu, Metin, O’Connor, Edmund Fitzgerald, Bache, Sarah, Theodorakopoulou, Evgenia, Sen, Sankhya, Sherren, Peter, Barnes, David, Dziewulski, Peter, The impact of major trauma network triage systems on patients with major burns, Burns : journal of the International Society for Burn Injuries, 42, 1662–1670, 2016 [PubMed: 27810131] | Study design not in PICO: Non-RCT with less than 100 per arm |
| Noticewala, M. S., Swart, E., Shah, R. P., Macaulay, W., Geller, J. A., First Place Award Multidisciplinary care of the hip fracture patient: A case control analysis of differing treatment protocols, Current Orthopaedic Practice, 27, 346–350, 2016 | Intervention not in PICO: Multi-disciplinary team delivering acute inpatient hip fracture care, with no mention of delivery or coordination of rehabilitation or social care |
| O’Keefe, Sophie, Stanley, Mandy, Adam, Kerry, Lannin, Natasha A., A Systematic Scoping Review of Work Interventions for Hospitalised Adults with an Acquired Neurological Impairment, Journal of Occupational Rehabilitation, 29, 569–584, 2019 [PubMed: 30515620] | Systematic review: Included studies checked for relevance. |
| Olenginski, T. P., Maloney-Saxon, G., Matzko, C. K., Mackiewicz, K., Kirchner, H. L., Bengier, A., Newman, E. D., High-risk osteoporosis clinic (HiROC): improving osteoporosis and postfracture care with an organized, programmatic approach, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 26, 801–10, 2015 [PubMed: 25398432] | Study design not in PICO: No comparison group. |
| O’Malley, Natasha T., Blauth, Michael, Suhm, Norbert, Kates, Stephen L., Hip fracture management, before and beyond surgery and medication: a synthesis of the evidence, Archives of orthopaedic and trauma surgery, 131, 1519–27, 2011 [PubMed: 21706188] | Systematic review: Included studies checked for relevance. |
| O’Mara, Michael Shaymus, Ramaniuk, Aliaksandr, Graymire, Vickie, Rozzell, Monica, Martin, Stacey, Lean methodology for performance improvement in the trauma discharge process, The journal of trauma and acute care surgery, 77, 137–142, 2014 [PubMed: 24977768] | Comparison not in PICO: Trauma vs non-trauma wards |
| O’Neil, Jennifer, van Ierssel, Jacquie, Sveistrup, Heidi, Remote supervision of rehabilitation interventions for survivors of moderate or severe traumatic brain injury: A scoping review, Journal of telemedicine and telecare, 1357633X19845466, 2019 [PubMed: 31148489] | Systematic review: Included studies checked for relevance. |
| Parsons, Matthew, Parsons, John, Pillai, Avinesh, Rouse, Paul, Mathieson, Sean, Bregmen, Rochelle, Smith, Christine, Kenealy, Tim, Post-Acute Care for Older People Following Injury: A Randomized Controlled Trial, Journal of the American Medical Directors Association, 21, 404–409.e1, 2020 [PubMed: 31629646] | Duplicate |
| Patrick, P. D., Allaire, J. H., Hostler, S. L., A pediatric brain injury program: Families are catalysts for change, SAGGI - Child Development and Disabilities, 29, 31–39, 2003 | Article not available |
| Perez Santamaria, M., Dominguez Arevalo, M. J., Manso Perez Cossio, J., Peraza Sanchez, M., Outcomes of a multidisciplinary approach for the management of hip fractures in older patients. Experience in a regional hospital, Osteoporosis International, 27, S419, 2016 | Published as abstract only |
| Pfeifer, M., Dionyssiotis, Y., Musculoskeletal Rehabilitation after Hip Fracture: A Review, Osteologie, 28, 183–191, 2019 | Systematic review: Included studies checked for relevance. |
| Pfeifer, M., Minne, H. W., Musculoskeletal rehabilitation after hip fracture: A review, Archives of Osteoporosis, 5, 49–59, 2010 | Systematic review: Included studies checked for relevance. |
| Phillips, V. L., Vesmarovich, S., Hauber, R., Wiggers, E., Egner, A., Telehealth: reaching out to newly injured spinal cord patients, Public health reports (Washington, D.C. : 1974), 116 Suppl 1, 94–102, 2001 [PMC free article: PMC1913671] [PubMed: 11889278] | Study dates not in PICO: 1998-August/September 2000. Results not presented separately for the period in PICO (January-August/September 2000) |
| Pils, K., Vavrovsky, G., Meisner, W., Schreiber, W., Bohmer, F., Improvement of rehabilitation outcomes of hip fractures: discharge assessment by patient care team, case management and wound healing]. [German, Wiener klinische wochenschrift, 112, 413–419, 2000 [PubMed: 10849953] | Article in German |
| Pioli, G., Pellicciotti, F., Davoli, M. L., Pignedoli, P., Sabetta, E., Ferrari, A., Hip fracture management and outcomes in Italy, European Geriatric Medicine, 1, 104–107, 2010 | Narrative description of hip fracture care model. No presentation of data |
| Pope, Sue, Vickerstaff, A. L., Wareham, A. P., Lessons learned from early rehabilitation of complex trauma at the Royal Centre for Defence Medicine, Journal of the Royal Army Medical Corps, 163, 124–131, 2017 [PubMed: 27412360] | Narrative description of Royal Centre for Defence Medicine rehabilitation model. No presentation of study data. |
| Powell, J., Heslin, J., Greenwood, R., Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial, Journal of neurology, neurosurgery, and psychiatry, 72, 193–202, 2002 [PMC free article: PMC1737759] [PubMed: 11796769] | Study dates not in PICO: Pre-2000 |
| Powell, Janet M., Fraser, Robert, Brockway, Jo Ann, Temkin, Nancy, Bell, Kathleen R., A Telehealth Approach to Caregiver Self-Management Following Traumatic Brain Injury: A Randomized Controlled Trial, The Journal of head trauma rehabilitation, 31, 180–90, 2016 [PubMed: 26394294] | Intervention not in PICO: Education for caregivers of people with traumatic brain injury |
| Prestmo, A., Sletvold, O., Thingstad, P., Taraldsen, K., Johnsen, L. G., Helbostad, J., Saltvedt, I., Outcomes of activities of daily living, cognition and mobility in the Trondheim Hip Fracture Trial. A randomized controlled trial, European Geriatric Medicine, 3, S56, 2012 | Published as abstract only |
| Proudfoot, Suzanne, Bennett, Brandon, Duff, Simon, Palmer, Julie, Implementation and effects of Enhanced Recovery After Surgery for hip and knee replacements and fractured neck of femur in New Zealand orthopaedic services, The New Zealand medical journal, 130, 77–90, 2017 [PubMed: 28494480] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Multi-component intervention with only 1 of 5 sections focused on discharge planning. Other areas targeted by the intervention was within the ambulance, pre-operative care, peri-operative care and post-operative care. |
| Prvu Bettger, Janet A., Stineman, Margaret G., Effectiveness of multidisciplinary rehabilitation services in postacute care: state-of-the-science. A review, Archives of physical medicine and rehabilitation, 88, 1526–34, 2007 [PMC free article: PMC4309994] [PubMed: 17964900] | Systematic review: Included studies checked for relevance. |
| Rae-Grant, Alex D., Turner, Aaron P., Sloan, Alicia, Miller, Deborah, Hunziker, James, Haselkorn, Jodie K., Self-management in neurological disorders: systematic review of the literature and potential interventions in multiple sclerosis care, Journal of rehabilitation research and development, 48, 1087–100, 2011 [PubMed: 22234713] | Systematic review: Included studies checked for relevance. |
| Rapidi, C. A., Tederko, P., Moslavac, S., Popa, D., Branco, C. A., Kiekens, C., Varela Donoso, E., Christodoulou, N., Evidence-based position paper on Physical and Rehabilitation Medicine (PRM) professional practice for persons with spinal cord injury. The European PRM position (UEMS PRM Section), European Journal of Physical and Rehabilitation Medicine, 54, 797–807, 2018 [PubMed: 29952157] | Systematic review: Included studies checked for relevance. |
| Reguant, F., Arnau, A., Lorente, J. V., Maestro, L., Bosch, J., Efficacy of a multidisciplinary approach on post-operative morbidity and mortality of elderly patients with hip fracture, Journal of Clinical Anesthesia, 53, 11–19, 2019 [PubMed: 30286380] | Intervention not in PICO: MDT intervention designed to optimise patient health before hip fracture surgery, rather than rehabilitation. |
| Reinhardt, J., Chen, S., Gosney, J., Hu, X., Li, J., Liu, S., Zhang, X., Effectiveness of a comprehensive rehabilitation services program on long-term physical functioning in injured survivors of the 2008 sichuan earthquake, PM and R, 4, S300, 2012 | Published as abstract only |
| Rezaei, Mojtaba, Sharifi, Amirsina, Vaccaro, Alexander Richard, Rahimi-Movaghar, Vafa, Home-Based Rehabilitation Programs: Promising Field to Maximize Function of Patients with Traumatic Spinal Cord Injury, Asian journal of neurosurgery, 14, 634–640, 2019 [PMC free article: PMC6703054] [PubMed: 31497079] | Systematic review: Included studies checked for relevance. |
| Robalino, S., Nyakang’o, S. B., Beyer, F., Fox, C., Allan, L. M., Effectiveness of interventions aimed at improving physical and psychological outcomes of fall-related injuries in people with dementia a systematic review, Age and Ageing, 47, 2018 [PMC free article: PMC5819703] [PubMed: 29463292] | Published as abstract only |
| Robles, L., Slogoff, M., Ladwig-Scott, E., Zank, D., Larson, M. K., Aranha, G., Shoup, M., The addition of a nurse practitioner to an inpatient surgical team results in improved use of resources, Surgery, 150, 711–717, 2011 [PubMed: 22000183] | Population not in PICO: Surgical and colorectal patients with no distinction between trauma and non-trauma surgical patients. |
| Roels, E. H., Aertgeerts, B., Ramaekers, D., Peers, K., Hospital- and community-based interventions enhancing (re)employment for people with spinal cord injury: a systematic review, Spinal cord, 54, 2–7, 2016 [PubMed: 26305872] | Systematic review: Included studies checked for relevance. |
| Rosario, Emily R., Espinoza, Laura, Kaplan, Stephanie, Khonsari, Sepehr, Thurndyke, Earl, Bustos, Melissa, Vickers, Kayla, Navarro, Brittney, Scudder, Bonnie, Patient navigation for traumatic brain injury promotes community re-integration and reduces re-hospitalizations, Brain Injury, 31, 1340–1347, 2017 [PubMed: 28650255] | Study design not in PICO: Non-RCT with less than 100 per arm. |
| Rothman, E. F., Cohort study: Violent reinjury and mortality highlights the need for a comprehensive care approach to youth presenting for assault-related injury, Evidence-Based Medicine, 20, 112, 2015 [PubMed: 25827138] | Setting not in PICO: Emergency department |
| Ruggiero, C., Zampi, E., Baroni, M., Mecocci, P., Rinonapoli, G., Caraffa, A., Conti, F., Brandi, M. L., The fracture unit to bridge the osteoporosis care gap in Italy, Osteoporosis International, 25, S365, 2014 | Published as abstract only |
| Rypkema, G., Adang, E., Dicke, H., Naber, T., De Swart, B., Disselhorst, L., Goluke-Willemse, G., Rikkert, M. O., Cost-effectiveness of an interdisciplinary intervention in geriatric inpatients to prevent malnutrition, Journal of Nutrition, Health and Aging, 8, 122–127, 2004 [PubMed: 14978608] | Unclear population: All non-terminally ill geriatric patients admitted for more than 2 days. Study does not report reason for admission. |
| Rytter, H. M., Westenbaek, K., Henriksen, H., Christiansen, P., Humle, F., Specialized interdisciplinary rehabilitation reduces persistent post-concussive symptoms: a randomized clinical trial, Brain Injury, 33, 266–281, 2019 [PubMed: 30500267] | Population not in PICO: People in the general population with post-concussive syndrome. Attended A&E but not admitted. |
| Saha, Sumit, DiRusso, Stephen M., Welle, Scott, Lieberman, Benjamin, Sender, Joel, Shabsigh, Ridwan, Baltazar, Gerard A., Integration of Geriatrician Consultation for Trauma Admissions May Benefit Patient Outcomes, Gerontology & geriatric medicine, 5, 2333721419858735, 2019 [PMC free article: PMC6589989] [PubMed: 31259206] | Intervention not in PICO: Geriatrician consultation for trauma patients upon admission to trauma centre if above 65 years old. No mention of coordination or delivery of rehabilitation. |
| Saltvedt, Ingvild, Prestmo, Anders, Einarsen, Elin, Johnsen, Lars Gunnar, Helbostad, Jorunn L., Sletvold, Olav, Development and delivery of patient treatment in the Trondheim Hip Fracture Trial. A new geriatric in-hospital pathway for elderly patients with hip fracture, BMC research notes, 5, 355, 2012 [PMC free article: PMC3463430] [PubMed: 22800378] | No study results presented in paper |
| Sander, Beate, Elliot-Gibson, Victoria, Beaton, Dorcas E., Bogoch, Earl R., Maetzel, Andreas, A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs, The Journal of bone and joint surgery. American volume, 90, 1197–205, 2008 [PubMed: 18519311] | Intervention not in PICO: Coordination of osteoporosis treatment after fragility fracture |
| Savage, R., Camejo, M., Kramer, S., Jeanne Lozada, A., McAllister, T., Mensah, N., Romanelli, L., Sanchez, L., Schneider, L., Donohue, P., Does multidisciplinary and intense rehabilitation in a post-acute brain injury school produce positive outcomes?, Journal of Head Trauma Rehabilitation, 32, E87, 2017 | Published as abstract only |
| Sayer, J., Quality improvement-fracture liaison service development, Osteoporosis International, 27, S557, 2016 | Published as abstract only |
| Schneider, Kathryn J., Leddy, John J., Guskiewicz, Kevin M., Seifert, Tad, McCrea, Michael, Silverberg, Noah D., Feddermann-Demont, Nina, Iverson, Grant L., Hayden, Alix, Makdissi, Michael, Rest and treatment/rehabilitation following sport-related concussion: a systematic review, British journal of sports medicine, 51, 930–934, 2017 [PubMed: 28341726] | Systematic review: Included studies checked for relevance. |
| Semerano, Luca, Guillot, Xavier, Rossini, Maurizio, Avice, Evelyne, Begue, Thierry, Wargon, Mathias, Boissier, Marie-Christophe, Saidenberg-Kermanac’h, Nathalie, What predicts initiation of osteoporosis treatment after fractures: education organisation or patients’ characteristics?, Clinical and Experimental Rheumatology, 29, 89–92, 2011 [PubMed: 21345297] | Intervention not in PICO: Patient osteoporosis education and organisation of osteoporosis care |
| Sen, A., Xiao, Y., Lee, S. A., Dutton, R., Scalea, T., Multidisciplinary discharge rounds may reduce ED overcrowding by facilitating hospital throughput, Academic Emergency Medicine, 17, S98–S99, 2010 | Published as abstract only |
| Serghiou, Michael A., Holmes, Christina L., McCauley, Robert L., A survey of current rehabilitation trends for burn injuries to the head and neck, The Journal of burn care & rehabilitation, 25, 514–8, 2004 [PubMed: 15534463] | Study design not in PICO: Survey of burn rehabilitation providers (N=100) |
| Shahrokhi, Akram, Azimian, Jalil, Amouzegar, Atousa, Oveisi, Sonia, Effect of Telenursing on Outcomes of Provided Care by Caregivers of Patients With Head Trauma After Discharge, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 25, 21–25, 2018 [PubMed: 29319646] | Intervention not in PICO: Weekly telephone calls to caregivers of people with head injury to discuss health status and possible issues. No mention of rehabilitation. |
| Shahrokhi, Akram, Azimian, Jalil, Amouzegar, Atousa, Oveisi, Sonia, The Effect of Telenursing on Referral Rates of Patients With Head Trauma and Their Family’s Satisfaction After Discharge, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 25, 248–253, 2018 [PubMed: 29985860] | Intervention not in PICO: Checklist teleheath intervention with no questions about rehabilitation |
| Shaw, W., Hong, Q. N., Pransky, G., Loisel, P., A literature review describing the role of return-to-work coordinators in trial programs and interventions designed to prevent workplace disability, Journal of Occupational Rehabilitation, 18, 2–15, 2008 [PubMed: 18080827] | Systematic review: Included studies checked for relevance. |
| Shepperd, S., Lannin, N. A., Clemson, L. M., McCluskey, A., Cameron, I. D., Barras, S. L., Discharge planning from hospital to home, Cochrane Database of Systematic Reviews, 2013, CD000313, 2013 [PubMed: 23440778] | Systematic review: Included studies checked for relevance. |
| Shingleton, S. K., Salinas, R. D., Aden, J. K., Berry, P. A., Palmer, C. R., Russe, C. S., Trichel, R. M., Melvin, J. J., King, B. T., Wound care team effectiveness on patient care efficiency and quality, Journal of Burn Care and Research, 37, S74, 2016 | Published as abstract only |
| Shyu, Y. I. L., Liang, J., Wu, C. C., Su, J. Y., Cheng, H. S., Chou, S. W., Chen, M. C., Yang, C. T., Interdisciplinary intervention for hip fracture in older Taiwanese: Benefits last for 1 year, Journals of Gerontology - Series A Biological Sciences and Medical Sciences, 63, 92–97, 2008 [PubMed: 18245766] | Follow-up data from Shyu 2005 study, which is excluded |
| Shyu, Y. I., Liang, J., Wu, C. C., Su, J. Y., Cheng, H. S., Chou, S. W., Yang, C. T., A pilot investigation of the short-term effects of an interdisciplinary intervention program on elderly patients with hip fracture in Taiwan, Journal of the American Geriatrics Society, 53, 811–818, 2005 [PubMed: 15877556] | Intervention/comparison not in PICO: Multidisciplinary rehabilitation program consisting of systemic interdisciplinary involvement, geriatric assessment, in-patient and in-home rehabilitation and discharge planning versus standard care that differed on most of these components, not just the coordination/delivery components |
| Siefferman, J., Ambrose, A. F., Lin, E., Improving patient handoff for acute rehabilitation admission, PM and R, 3, S320, 2011 | Published as abstract only |
| Singh, Nalin A., Quine, Susan, Clemson, Lindy M., Williams, Elodie J., Williamson, Dominique A., Stavrinos, Theodora M., Grady, Jodie N., Perry, Tania J., Lloyd, Bradley D., Smith, Emma U. R., Singh, Maria A. Fiatarone, Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial, Journal of the American Medical Directors Association, 13, 24–30, 2012 [PubMed: 21944168] | Intervention not in PICO: High intensity progressive resistance training |
| Singler, K., Biber, R., Wicklein, S., Heppner, H. J., Sieber, C. C., Bail, H. J., “N-active”: A new comanaged, orthogeriatric ward: Observations and prospects, Zeitschrift fur Gerontologie und Geriatrie, 44, 2011 [PubMed: 22159830] | Narrative description of implementation of orthogeriatric ward. Only data presented is non-comparative. |
| Spiliotopoulou, Georgia, Atwal, Anita, Is occupational therapy practice for older adults with lower limb amputations evidence-based? A systematic review, Prosthetics and orthotics international, 36, 7–14, 2012 [PubMed: 22089164] | Systematic review: Included studies checked for relevance. |
| Stubbs, Kendra E., Sikes, Lindsay, Interdisciplinary Approach to Fall Prevention in a High-Risk Inpatient Pediatric Population: Quality Improvement Project, Physical therapy, 97, 97–104, 2017 [PubMed: 27340197] | Outcome not in PICO - Fall rates |
| Talevski, Jason, Sanders, Kerrie M., Duque, Gustavo, Connaughton, Catherine, Beauchamp, Alison, Green, Darci, Millar, Lynne, Brennan-Olsen, Sharon L., Effect of Clinical Care Pathways on Quality of Life and Physical Function After Fragility Fracture: A Meta-analysis, Journal of the American Medical Directors Association, 20, 926.e1–926.e11, 2019 [PubMed: 30975586] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Tan, T., Molina, J. D., Lim, Y., Dharmawan, A., Teo, A., Soon, M., Frailty ready inpatient care-interim findings from an integrated, comprehensive geriatric programme, Journal of the American Geriatrics Society, 67, S92–S93, 2019 | Published as abstract only |
| Taraldsen, K., Sletvold, O., Thingstad, P., Saltvedt, I., Granat, M. H., Lydersen, S., Helbostad, J. L., Physical behavior and function early after hip fracture surgery in patients receiving comprehensive geriatric care or orthopedic care--a randomized controlled trial, Journals of gerontology. Series A, Biological sciences and medical sciences, 69, 338–345, 2014 [PubMed: 23902933] | Intervention not in PICO: Comprehensive geriatric care with an element of discharge planning and early mobilisation but focus appears to be on short-term post-operative outcomes with treatment of co-morbidities and acute care rather than delivery or coordination of rehabilitation or social care. |
| Torres, Audrey, Kunishige, Nalani, Morimoto, Denise, Hanzawa, Tracie, Ebesu, Mike, Fernandez, John, Nohara, Lynne, SanAgustin, Eliseo, Borg, Stephanie, Shared governance: a way to improve the care in an inpatient rehabilitation facility, Rehabilitation nursing : the official journal of the Association of Rehabilitation Nurses, 40, 69–73, 2015 [PubMed: 24729092] | Outcomes not in PICO: Mentions improved patient outcomes but no presentation of data |
| Tran, V., Lam, M. K., Amon, K. L., Brunner, M., Hines, M., Penman, M., Lowe, R., Togher, L., Interdisciplinary eHealth for the care of people living with traumatic brain injury: A systematic review, Brain Injury, 31, 1701–1710, 2017 [PubMed: 29064300] | Systematic review: Included studies checked for relevance. |
| Tricco, Andrea C., Thomas, Sonia M., Veroniki, Areti Angeliki, Hamid, Jemila S., Cogo, Elise, Strifler, Lisa, Khan, Paul A., Robson, Reid, Sibley, Kathryn M., MacDonald, Heather, Riva, John J., Thavorn, Kednapa, Wilson, Charlotte, Holroyd-Leduc, Jayna, Kerr, Gillian D., Feldman, Fabio, Majumdar, Sumit R., Jaglal, Susan B., Hui, Wing, Straus, Sharon E., Comparisons of Interventions for Preventing Falls in Older Adults: A Systematic Review and Meta-analysis, JAMA, 318, 1687–1699, 2017 [PMC free article: PMC5818787] [PubMed: 29114830] | Systematic review: Included studies checked for relevance. |
| Truchon, C., Moore, L., Belcaid, A., Clement, J., Trudelle, N., Ulysse, M. A., Grolleau, B., Clusiau, J., Levesque, D., De Guise, M., Shaping quality through vision, structure, and monitoring of performance and quality indicators: Impact story from the Quebec trauma network, International Journal of Technology Assessment in Health Care, 33, 415–419, 2017 [PubMed: 28578738] | Narrative description of Quebec Trauma Network and its set-up. No data presented apart from brief mention of mortality data. |
| Tseng, M. Y., Liang, J., Wang, J. S., Yang, C. T., Wu, C. C., Cheng, H. S., Chen, C. Y., Lin, Y. E., Wang, W. S., Shyu, Y. I. L., Effects of a diabetes-specific care model for hip fractured older patients with diabetes: A randomized controlled trial, Experimental Gerontology, 126, 110689, 2019 [PubMed: 31404623] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard rehabilitation while inpatients but the intervention group also received in-home rehabilitation for 4 months after hospital discharge and diabetes-specific education and rehabilitation for up to 12 months after hospital discharge. |
| Tung, James Y., Stead, Brent, Mann, William, Ba’Pham,, Popovic, Milos R., Assistive technologies for self-managed pressure ulcer prevention in spinal cord injury: a scoping review, Journal of Rehabilitation Research and Development, 52, 131–46, 2015 [PubMed: 26237111] | Scoping review: Included studies checked for relevance. |
| Turner, Benjamin J., Fleming, Jennifer M., Ownsworth, Tamara L., Cornwell, Petrea L., The transition from hospital to home for individuals with acquired brain injury: A literature review and research recommendations, Disability and rehabilitation, 30, 1153–1176, 2008 [PubMed: 17852241] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, L., Disler, P. B., Nair, A., Wade, D. T., Multi-disciplinary rehabilitation for acquired brain injury in adults of working age, The Cochrane database of systematic reviews, CD004170, 2005 [PubMed: 16034923] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, Lynne, Evidence for the effectiveness of multi-disciplinary rehabilitation following acquired brain injury: a synthesis of two systematic approaches, Journal of rehabilitation medicine, 40, 691–701, 2008 [PubMed: 18843419] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, Lynne, Pick, Anton, Nair, Ajoy, Disler, Peter B., Wade, Derick T., Multi-disciplinary rehabilitation for acquired brain injury in adults of working age, The Cochrane database of systematic reviews, CD004170, 2015 [PMC free article: PMC8629646] [PubMed: 26694853] | Systematic review: Included studies checked for relevance. |
| Vaughn, S. L., King, A., A survey of state programs to finance rehabilitation and community services for individuals with brain injury, The Journal of head trauma rehabilitation, 16, 20–33, 2001 [PubMed: 11277848] | Study design not in PICO: Survey of state-funded programs for persons with traumatic brain injury. |
| Vidan, Maite, Serra, Jose A., Moreno, Concepcion, Riquelme, Gerardo, Ortiz, Javier, Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial, Journal of the American Geriatrics Society, 53, 1476–82, 2005 [PubMed: 16137275] | Study dates not in PICO: 1997 |
| Vikane, E., Hellstrom, T., Roe, C., Bautz-Holter, E., Assmus, J., Skouen, J. S., Efficacy of a multidisciplinary outpatient treatment for patients with mild traumatic brain injury: A randomized controlled intervention trial, Brain Injury, 30, 617, 2016 [PubMed: 28296510] | Published as abstract only |
| Ward, D., Drahota, A., Gal, D., Severs, M., Dean, T. P., Care home versus hospital and own home environments for rehabilitation of older people, Cochrane Database of Systematic Reviews, 2008 [PMC free article: PMC6991934] [PubMed: 18843641] | Systematic review: Included studies checked for relevance. |
| Webster, J., Kim, J. H., Hawley, C., Barbir, L., Barton, S., Young, C., Development, implementation, and outcomes of a residential vocational rehabilitation program for injured Service members and Veterans, Journal of Vocational Rehabilitation, 48, 111–126, 2018 | Study design not in PICO: No comparison group |
| Wegener, Stephen T., Mackenzie, Ellen J., Ephraim, Patti, Ehde, Dawn, Williams, Rhonda, Self-management improves outcomes in persons with limb loss, Archives of Physical Medicine and Rehabilitation, 90, 373–80, 2009 [PubMed: 19254599] | Population not in PICO: Mixed population with <40% in PICO and results not reported separately for target population |
| Westgard, T., Ottenvall Hammar, I., Holmgren, E., Ehrenberg, A., Wisten, A., Ekdahl, A. W., Dahlin-Ivanoff, S., Wilhelmson, K., Comprehensive geriatric assessment pilot of a randomized control study in a Swedish acute hospital: A feasibility study, Pilot and Feasibility Studies, 4, 41, 2018 [PMC free article: PMC5789623] [PubMed: 29423259] | Unclear population: Frail adults over 75 years who required an acute hospital admission. No information presented on traumatic or non-trauma causes. |
| Wiechman, S. A., Carrougher, G. J., Esselman, P. C., Angere, D., Klein, M. B., Gibran, N. S., A randomized controlled trial to test an expanded delivery model for patients with burn injuries, Journal of burn care & research, 35, S79-, 2014 | Published as abstract only |
| Winograd, A., Squirrell, T., Winters, B., The promise of progress: Co-ordinating interdisciplinary neuro-restorative care transitions, Brain Injury, 28, 775–776, 2014 | Published as abstract only |
| Wu, Jane, Faux, Steven G., Harris, Ian, Poulos, Christopher J., Integration of trauma and rehabilitation services is the answer to more cost-effective care, ANZ journal of surgery, 86, 900–904, 2016 [PubMed: 26631277] | Comparison not in PICO: Delivery of rehabilitation in the trauma admission hospital versus rehabilitation in an external rehabilitation service. No details reported about what rehabilitation the patients received in either facility (and no data on any coordination or delivery aspects of the rehabilitation). |
| Young, T., Andreas, N., Howard-Brown, C., Enhancing early engagement for transitions to community, Brain Impairment, 20, 374–375, 2019 | Published as abstract only |
| Zatzick, D. F., Roy-Byrne, P., Russo, J. E., Rivara, F. P., Koike, A., Jurkovich, G. J., Katon, W., Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial, General Hospital Psychiatry, 23, 114–23, 2001 [PubMed: 11427243] | Intervention and comparison not in PICO: Collaborative care intervention consisting of counselling, consultation with surgical and primary care providers and attempted post-discharge coordination versus standard care that differed on all these components, not just the coordination/delivery components. Unclear if study period (years) within PICO |
| Zatzick, D., Russo, J., Thomas, P., Darnell, D., Teter, H., Ingraham, L., Whiteside, L. K., Wang, J., Guiney, R., Parker, L., Sandgren, K., Hedrick, M. K., Van Eaton, E. G., Jurkovich, G., Patient-Centered Care Transitions After Injury Hospitalization: A Comparative Effectiveness Trial, Psychiatry (New York), 81, 141–157, 2018 [PubMed: 29533154] | Population not in PICO: Patients had to be admitted to an inpatient surgical ward or emergency department for at least 24 hours i.e. not all admitted to hospital. Results are not presented separately. |
| Zhang, Ming, Effect of HBM Rehabilitation Exercises on Depression, Anxiety and Health Belief in Elderly Patients with Osteoporotic Fracture, Psychiatria Danubina, 29, 466–472, 2017 [PubMed: 29197204] | Outcomes not in PICO : Anxiety, depression, osteoporosis knowledge, and osteoporosis health belief |
| Zhang, Xia, Reinhardt, Jan D., Gosney, James E., Li, Jianan, The NHV rehabilitation services program improves long-term physical functioning in survivors of the 2008 Sichuan earthquake: a longitudinal quasi experiment, PLoS ONE, 8, e53995, 2013 [PMC free article: PMC3538750] [PubMed: 23308293] | Intervention and comparison not in PICO: NHV is a complete rehabilitation programme (consisting of NGOs, health department and volunteers) implemented after the Sichuan earthquake. Comparisons are early-NHV, late-NHV, no NHV. |
| Zhao, Y. R., Liang, X., Yang, T. Y., Liu, Y., Prospective case-control study on comprehensive treatment for elderly hip fractures, Zhongguo gu shang [China journal of orthopaedics and traumatology], 27, 570–574, 2014 [PubMed: 25338443] | Article in Chinese |
| Zidén, L., Frändin, K., Kreuter, M., Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities, Clinical Rehabilitation, 22, 1019–1033, 2008 [PubMed: 19052241] | Intervention and comparison not in PICO: Multidisciplinary geriatric rehabilitation home program focused on supported discharge, independence in daily activities, and enhancing physical activity versus standard care with no structured rehabilitation after discharge. Interventions differed on most of these components, not just the coordination/delivery components |
| Ziden, Lena, Frandin, Kerstin, Kreuter, Margareta, Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities, Clinical Rehabilitation, 22, 1019–1033, 2008 [PubMed: 19052241] | Duplicate |
Qualitative clinical studies
Table 40Excluded qualitative studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Abrahamson, Vanessa, Jensen, Jan, Springett, Kate, Sakel, Mohamed, Experiences of patients with traumatic brain injury and their carers during transition from in-patient rehabilitation to the community: a qualitative study, Disability and rehabilitation, 39, 1683–1694, 2017 [PubMed: 27557977] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences reviews. |
| Adams, Deana, Dahdah, Marie, Coping and adaptive strategies of traumatic brain injury survivors and primary caregivers, NeuroRehabilitation, 39, 223–37, 2016 [PubMed: 27372358] | Study not conducted in one of the countries included in the review protocol. |
| Adams, R. D. F., Cole, E., Brundage, S. I., Morrison, Z., Jansen, J. O., Beliefs and expectations of rural hospital practitioners towards a developing trauma system: A qualitative case study, Injury, 49, 1070–1078, 2018 [PubMed: 29602489] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Aitken, Leanne M., Chaboyer, Wendy, Jeffrey, Carol, Martin, Bronte, Whitty, Jennifer A., Schuetz, Michael, Richmond, Therese S., Indicators of injury recovery identified by patients, family members and clinicians, Injury, 47, 2655–2663, 2016 [PubMed: 27793327] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Albrecht, Jennifer S., O’Hara, Lyndsay M., Moser, Kara A., Mullins, C. Daniel, Rao, Vani, Perception of Barriers to the Diagnosis and Receipt of Treatment for Neuropsychiatric Disturbances After Traumatic Brain Injury, Archives of Physical Medicine and Rehabilitation, 98, 2548–2552, 2017 [PMC free article: PMC6935532] [PubMed: 28688786] | Study not conducted in one of the countries included in the review protocol. |
| Alston, Margaret, Jones, Jennifer, Curtin, Michael, Alston, Bartky Blais Bourdieu Bourdieu Brookshire Butler Callaway Connell Cunningham Curtin Degeneffe Fine Foucault Graham Gwyn Howes Jones Kirkness Lupton Mukherjee O’Rance Ponsford Rees Reichard Reidpath Shildrick Slewa-Younan, Women and traumatic brain injury: “It’s not visible damage”, Australian Social Work, 65, 39–53, 2012 | No qualitative data on phenomena of interest. |
| Ammons, L. L., Harraghy, R. L., Medlin, H. J., Faku, C. T., Shupp, J. W., Flanagan, K. E., Jeng, J. C., Fidler, P., Sava, J. A., Jordan, M. H., Assessing the utility of nurse-driven post-discharge telephone calls, Journal of Burn Care and Research, 32, S153, 2011 | Conference abstract |
| Andersson, Kerstin, Bellon, Michelle, Walker, Ruth, Parents’ experiences of their child’s return to school following acquired brain injury (ABI): A systematic review of qualitative studies, Brain Injury, 30, 829–38, 2016 [PubMed: 27057776] | No findings or themes related to phenomena of interest. Included studies were checked for relevance. |
| Angel, Sanne, Kirkevold, Marit, Pedersen, Birthe D., Rehabilitation after spinal cord injury and the influence of the professional’s support (or lack thereof), Journal of Clinical Nursing, 20, 1713–22, 2011 [PubMed: 21323775] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehab following discharge. |
| Arbour-Nicitopoulos, K. P., Lamontagne, M. E., Tomasone, J., Pila, E., Cumming, I., Latimer-Cheung, A. E., Routhier, F., Why do I stick to the program? a qualitative analysis of the determinants of adherence to community-based physical activity support programs by persons with SCI and contrast with general population with disabilities, Journal of Spinal Cord Medicine, 37, 626, 2014 | Conference abstract. |
| Armstrong, E., Missing voices: Aboriginal stories of stroke and traumatic brain injury, International Journal of Stroke, 12, 14, 2017 | Conference abstract. |
| Armstrong, Elizabeth, Coffin, Juli, Hersh, Deborah, Katzenellenbogen, Judith M., Thompson, Sandra C., Ciccone, Natalie, Flicker, Leon, Woods, Deborah, Hayward, Colleen, Dowell, Catelyn, McAllister, Meaghan, “You felt like a prisoner in your own self, trapped”: the experiences of Aboriginal people with acquired communication disorders, Disability and Rehabilitation, 1–14, 2019 [PubMed: 31692386] | The majority of participants had not experienced traumatic injury and the results not reported separately for the target population. |
| Armstrong, Elizabeth, Coffin, Juli, McAllister, Meaghan, Hersh, Deborah, Katzenellenbogen, Judith M., Thompson, Sandra C., Ciccone, Natalie, Flicker, Leon, Cross, Natasha, Arabi, Linda, Woods, Deborah, Hayward, Colleen, Alway, Armstrong Armstrong Baxter Blackmer Bohanna Bronfenbrenner Chase Coffin Creswell Elder Feigin Foster Gauld Gauthier Hines Jamieson Katzenellenbogen Katzenellenbogen Katzenellenbogen Keightley Kelly Kelly Lakhani Lewis Linton McDonald McKenna O’Reilly Olver Ponsford Rutland-Brown Salas Sandelowski Taylor Togher, ‘I’ve got to row the boat on my own, more or less’: Aboriginal Australian experiences of traumatic brain injury, Brain Impairment, 20, 120–136, 2019 | No qualitative data on phenomena of interest. |
| Arshad, Sira N., Gaskell, Sarah L., Baker, Charlotte, Ellis, Nicola, Potts, Jennie, Coucill, Theresa, Ryan, Lynn, Smith, Jan, Nixon, Anna, Greaves, Kate, Monk, Rebecca, Shelmerdine, Teresa, Leach, Alison, Shah, Mamta, Measuring the impact of a burns school reintegration programme on the time taken to return to school: A multi-disciplinary team intervention for children returning to school after a significant burn injury, Burns : journal of the International Society for Burn Injuries, 41, 727–34, 2015 [PubMed: 25535118] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Ayer, Lynsay, Farris, Coreen, Farmer, Carrie M., Geyer, Lily, Barnes-Proby, Dionne, Ryan, Gery W., Skrabala, Lauren, Scharf, Deborah M., Care Transitions to and from the National Intrepid Center of Excellence (NICoE) for Service Members with Traumatic Brain Injury, Rand health quarterly, 5, 12, 2015 [PMC free article: PMC5158292] [PubMed: 28083388] | Study not conducted in one of the countries included in the review protocol. |
| Badger, Karen, Royse, David, Adult burn survivors’ views of peer support: a qualitative study, Social Work in Health Care, 49, 299–313, 2010 [PubMed: 20379901] | Study not conducted in one of the countries included in the review protocol. |
| Balcazar, Fabricio E., Kelly, Erin Hayes, Keys, Christopher B., Balfanz-Vertiz, Kristin, Albrecht, Alston Balcazar Balcazar Block Boschen Burnett Cressy Devlieger Devlieger Dijkers Dijkers Engstrom Gill Groce Haskell Hayes Hernandez Hernandez Hibbard Jackson Kroll Ljungberg McDonald McKinley Ostrander Richards Rovinsky Sable Servan Sherman Veith Waters Waters Waters Whiteneck Wilson Wilson, Using peer mentoring to support the rehabilitation of individuals with violently acquired spinal cord injuries, Journal of Applied Rehabilitation Counseling, 42, 3–11, 2011 | Study not conducted in one of the countries included in the review protocol. |
| Barclay, Linda, McDonald, Rachael, Lentin, Primrose, Social and community participation following spinal cord injury: a critical review, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 38, 1–19, 2015 [PubMed: 25305008] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Barclay, Linda, McDonald, Rachael, Lentin, Primrose, Bourke-Taylor, Helen, Facilitators and barriers to social and community participation following spinal cord injury, Australian occupational therapy journal, 63, 19–28, 2016 [PubMed: 26530379] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Beaton, Angela, O’Leary, Katrina, Thorburn, Julie, Campbell, Alaina, Christey, Grant, Improving patient experience and outcomes following serious injury, The New Zealand medical journal, 132, 15–25, 2019 [PubMed: 31048821] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Beckett, K., Earthy, S., Sleney, J., Barnes, J., Kellezi, B., Barker, M., Clarkson, J., Coffey, F., Elder, G., Kendrick, D., Providing effective trauma care: The potential for service provider views to enhance the quality of care (qualitative study nested within a multicentre longitudinal quantitative study), BMJ Open, 4, e005668, 2014 [PMC free article: PMC4091464] [PubMed: 25005598] | No qualitative data on phenomena of interest. |
| Bergmark, Lisa, Westgren, Ninni, Asaba, Eric, Returning to work after spinal cord injury: exploring young adults’ early expectations and experience, Disability and Rehabilitation, 33, 2553–8, 2011 [PubMed: 21592045] | Study did not examine rehabilitation while an inpatient, when transferring to community, or seeking to access rehabilitation following discharge. |
| Bernet, Madeleine, Sommerhalder, Kathrin, Mischke, Claudia, Hahn, Sabine, Wyss, Adrian, “Theory Does Not Get You From Bed to Wheelchair”: A Qualitative Study on Patients’ Views of an Education Program in Spinal Cord Injury Rehabilitation, Rehabilitation nursing : the official journal of the Association of Rehabilitation Nurses, 44, 247–253, 2019 [PubMed: 29889696] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Bernhoff, K., Bjorck, M., Larsson, J., Jangland, E., Patient Experiences of Life Years After Severe Civilian Lower Extremity Trauma With Vascular Injury, European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery, 52, 690–695, 2016 [PubMed: 27637376] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Biester, Rosette C., Krych, Dave, Schmidt, M. J., Parrott, Devan, Katz, Douglas I., Abate, Melissa, Hirshson, Chari I., Individuals With Traumatic Brain Injury and Their Significant Others’ Perceptions of Information Given About the Nature and Possible Consequences of Brain Injury: Analysis of a National Survey, Professional case management, 21, 22–4, 2016 [PubMed: 26618266] | Study not conducted in one of the countries included in the review protocol. |
| Body, Richard, Muskett, Tom, Perkins, Mick, Parker, Mark, Your injury, my accident: talking at cross-purposes in rehabilitation after traumatic brain injury, Brain Injury, 27, 1356–63, 2013 [PubMed: 24070204] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Boschen, K., Gerber, G., Gargaro, J., Comparison of outcomes and costs of 2 publicly-funded community-based models of acquired brain injury services, Archives of Physical Medicine and Rehabilitation, 91, e59, 2010 | Conference abstract. |
| Bourge, C., Body Image (BI) of acquired spinal cord injury (SCI) persons. Which patient care in an internal unit of physical and neurological rehabilitation. Experience of the patient care in an internal and neurological unit of PMR of the University Hospital of Liege, Annals of Physical and Rehabilitation Medicine, 59 (Supplement), e128, 2016 | No qualitative data on phenomena of interest. |
| Bourke, John A., Nunnerley, Joanne L., Sullivan, Martin, Derrett, Sarah, Relationships and the transition from spinal units to community for people with a first spinal cord injury: A New Zealand qualitative study, Disability and health journal, 12, 257–262, 2019 [PubMed: 30262164] | The focus was not specific to participants who had experienced traumatic injury and the results not reported separately for the target population. |
| Braaf, Sandra C., Lennox, Alyse, Nunn, Andrew, Gabbe, Belinda J., Experiences of hospital readmission and receiving formal carer services following spinal cord injury: a qualitative study to identify needs, Disability and Rehabilitation, 40, 1893–1899, 2018 [PubMed: 28407725] | Study did not examine phenomena of interest. |
| Brauer, Jennifer, Hay, Catherine Cooper, Francisco, Gerard, A retrospective investigation of occupational therapy services received following a traumatic brain injury, Occupational Therapy in Health Care, 25, 119–30, 2011 [PubMed: 23899029] | Study not conducted in one of the countries included in the review protocol. |
| Brimicombe, L., Ling, J., De Sousa De Abreu, I., Hoffman, K., Salisbury, C., Jefferson, R., Makela, P., Early integration of a self-management support package into usual care following traumatic brain injury (TBI): A feasibility study, British Journal of Neurosurgery, 31, 501, 2017 | Conference abstract. |
| Brito, Sara, White, Jennifer, Thomacos, Nikos, Hill, Bridget, The lived experience following free functioning muscle transfer for management of pan-brachial plexus injury: reflections from a long-term follow-up study, Disability and Rehabilitation, 1–9, 2019 [PubMed: 31574227] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Brockway, J. A., St De Lore, J., Fann, J. R., Hart, T., Hurst, S., Fey-Hinckley, S., Savage, J., Warren, M., Bell, K. R., Telephone-delivered problem-solving training after mild traumatic brain injury: qualitative analysis of service members’ perceptions, Rehabilitation Psychology, 61, 221–230, 2016 [PubMed: 26797117] | Study not conducted in one of the countries included in the review protocol. |
| Brown, F., Sofronoff, K., Whittingham, K., Boyd, R., McKinlay, L., Parenting a child with a traumatic brain injury: A focus group study, Developmental Medicine and Child Neurology, 54, 24–25, 2012 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Brown, Jessica, Hux, Karen, Hey, Morgan, Murphy, Madeline, Ackerman, Aldrich Anderson Arciniegas Bach Beigel Bogdan Brandt Brown Brown Catroppa Cicerone Cicerone Creswell Creswell Cushman de Joode de Joode DePompei Donders Dowds Doyle Edwards Ewing-Cobbs Fortuny Gillette Gillette Gioia Glang Gordon Gordon Grajzel Harper Hart Hawley Helm-Estabrooks Hendricks Hux Kelley Kennedy Kennedy Kertesz Krause Leopold Lincoln Martella Martinez McAllister McCrory Merriam Moustakas Ownsworth Patel Perna Reitan Rumrill Scherer Scherer Scherer Scherer Scherer Scherer Shanahan Sherer Sherer Sohlberg Spreen Starks Tate Todis Togher Vu Wallace Ylvisaker Ylvisaker, Exploring cognitive support use and preference by college students with TBI: A mixed-methods study, NeuroRehabilitation, 41, 483–499, 2017 [PubMed: 28946573] | Study not conducted in one of the countries included in the review protocol. |
| Browne, C., Living with traumatic brain injury: Views of survivors and family members, Brain Injury, 26, 400, 2012 | Conference abstract. |
| Bruner-Canhoto, Laney, Savageau, Judith, Croucher, Deborah, Bradley, Kathryn, Lessons From a Care Management Pilot Program for People With Acquired Brain Injury, Journal for healthcare quality : official publication of the National Association for Healthcare Quality, 38, 255–263, 2016 [PubMed: 26042754] | Study not conducted in one of the countries included in the review protocol. |
| Buck, P., Kirzner, R., Sagrati, J., Laster, R., The challenge of mTBI work: An exploratory study of rehabilitation professionals, Brain Injury, 26, 583–584, 2012 | Conference abstract. |
| Buck, Page Walker, Sagrati, Jocelyn Spencer, Kirzner, Rachel Shapiro, Belson, Bloom Brenner Briggs Brody Buck Chrisman Gaboda Klein Marchione Padgett Patton Schwartz Strauss Thompson, Mild traumatic brain injury: A place for social work, Social Work in Health Care, 52, 741–751, 2013 [PubMed: 24028738] | Study not conducted in one of the countries included in the review protocol. |
| Buddai, S., Di Taranti, L. J., Adenwala, A. Y., Aepli, S., Choudhary, M., George, D. L., Koilor, C. B., Linehan, M., Peifer, H., Rub, D., Kaplan, L., Johnson, N., Lane-Fall, M. B., Characterizing intensive care unit patient and family experiences of recovery after traumatic injury, American Journal of Respiratory and Critical Care Medicine. Conference: American Thoracic Society International Conference, ATS, 195, 2017 | Conference abstract. |
| Buscemi, Valentina, Cassidy, Elizabeth, Kilbride, Cherry, Reynolds, Frances Ann, A qualitative exploration of living with chronic neuropathic pain after spinal cord injury: an Italian perspective, Disability and Rehabilitation, 40, 577–586, 2018 [PubMed: 28054832] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Bushnik, T., Smith, M., Long, C., Supporting factors for follow-up care in TBI patients post-inpatient discharge, Brain Injury, 31 (6–7), 974, 2017 | Conference abstract. |
| Byrnes, Michelle, Beilby, Janet, Ray, Patricia, McLennan, Renee, Ker, John, Schug, Stephan, Patient-focused goal planning process and outcome after spinal cord injury rehabilitation: quantitative and qualitative audit, Clinical Rehabilitation, 26, 1141–9, 2012 [PubMed: 22653375] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Cahow, C., Gassaway, J., Rider, C., Joyce, J. P., Bogenshutz, A., Edens, K., Kreider, S. E. D., Whiteneck, G., Relationship of therapeutic recreation inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: The SCIRehab project, Journal of Spinal Cord Medicine, 35, 547–564, 2012 [PMC free article: PMC3522896] [PubMed: 23318036] | Study not conducted in one of the countries included in the review protocol. |
| Calder, Allyson, Nunnerley, Jo, Mulligan, Hilda, Ahmad Ali, Nordawama, Kensington, Gemma, McVicar, Tim, van Schaik, Olivia, Experiences of persons with spinal cord injury undertaking a physical activity programme as part of the SCIPA ‘Full-On’ randomized controlled trial, Disability and Health Journal, 11, 267–273, 2018 [PubMed: 29089215] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Calleja, Pauline, Aitken, Leanne, Cooke, Marie, Staff perceptions of best practice for information transfer about multitrauma patients on discharge from the emergency department: a focus group study, Journal of Clinical Nursing, 25, 2863–73, 2016 [PubMed: 27453432] | Setting not in PICO: Emergency department. |
| Canto, Angela I., Chesire, David J., Buckley, Valerie A., Andrews, Terrie W., Roehrig, Alysia D., Arroyos-Jurado, Ball Bradley-Klug Brantlinger Braun Chesire Conoley Cook Davies Elliot Ewing-Cobbs Farmer Gioia Glang Glang Glang Gopinath Guba Guskiewicz Havey Hooper Hux Jantz Johnson Lewandowski Meehan Mellard Rosenthal Rutland-Brown Savage Sharp Shaw Shaw Shih Yeates Yeates Ylvisaker, Barriers to meeting the needs of students with traumatic brain injury, Educational Psychology in Practice, 30, 88–103, 2014 | Study not conducted in one of the countries included in the review protocol. |
| Carron, R. M. C., ‘nobody prepared me for this!’ parents’ experiences of seeking help and support with post-brain injury symptoms and changes in children and adolescents with acquired brain injury, Journal of Neurology, Neurosurgery and Psychiatry, 90, A9, 2019 | Conference abstract. |
| Caspari, Synnove, Aasgaard, Trygve, Lohne, Vibeke, Slettebo, Ashild, Naden, Dagfinn, Perspectives of health personnel on how to preserve and promote the patients’ dignity in a rehabilitation context, Journal of Clinical Nursing, 22, 2318–26, 2013 [PubMed: 23651360] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for the target population. |
| Chapple, L. A., Chapman, M., Shalit, N., Udy, A., Deane, A., Williams, L., Barriers to Nutrition Intervention for Patients With a Traumatic Brain Injury: Views and Attitudes of Medical and Nursing Practitioners in the Acute Care Setting, Journal of Parenteral and Enteral Nutrition, 42, 318–326, 2018 [PubMed: 29443400] | Study did not examine phenomena of interest. |
| Chapple, Lee-Anne, Chapman, Marianne, Shalit, Natalie, Udy, Andrew, Deane, Adam, Williams, Lauren, Barriers to Nutrition Intervention for Patients With a Traumatic Brain Injury, JPEN. Journal of parenteral and enteral nutrition, 148607116687498, 2017 [PubMed: 29443400] | Duplicate. |
| Chondronikola, M., Weller, S., Rosenberg, L., Rosenberg, M., Meyer, W. J., Herndon, D. N., Sidossis, L., Variation among clinical specialties in perceptions of pediatric burn patient needs, Journal of Burn Care and Research, 37, S244, 2016 | Conference abstract. |
| Christie, Nicola, Beckett, Kate, Earthy, Sarah, Kellezi, Blerina, Sleney, Jude, Barnes, Jo, Jones, Trevor, Kendrick, Denise, Seeking support after hospitalisation for injury: a nested qualitative study of the role of primary care, The British journal of general practice : the journal of the Royal College of General Practitioners, 66, e24–31, 2016 [PMC free article: PMC4684032] [PubMed: 26639949] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Christie, Nicola, Braaf, Sandra, Ameratunga, Shanthi, Nunn, Andrew, Jowett, Helen, Gabbe, Belinda, Barclay, Barnes Berkman Boniface Braun Cameron Carpenter Cass Charlson Christie Christie Cox Gabbe Gabbe Kellezi Larsen Levasseur Lyons Marottoli McInnes Pointer Prang Smith Syed Urry Wilson, The role of social networks in supporting the travel needs of people after serious traumatic injury: A nested qualitative study, Journal of Transport & Health, 6, 84–92, 2017 | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Cichon, S., Danford, E. K., Schladen, M. M., Bruner, D., Libin, A., Scholten, J., Integrating opportunities for family involvement into a manualized goal self-management intervention for veterans with mTBI, Archives of Physical Medicine and Rehabilitation, 96, e77, 2015 | Conference abstract. |
| Cocks, Errol, Bulsara, Caroline, O’Callaghan, Annalise, Netto, Julie, Boaden, Ross, Exploring the experiences of people with the dual diagnosis of acquired brain injury and mental illness, Brain Injury, 28, 414–21, 2014 [PubMed: 24475744] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Coffey, Nathan T., Weinstein, Ali A., Cai, Cindy, Cassese, Jimmy, Jones, Rebecca, Shaewitz, Dahlia, Garfinkel, Steven, Identifying and Understanding the Health Information Experiences and Preferences of Individuals With TBI, SCI, and Burn Injuries, Journal of patient experience, 3, 88–95, 2016 [PMC free article: PMC5513647] [PubMed: 28725843] | Study not conducted in one of the countries included in the review protocol. |
| Cogan, A., Treatment model of occupational therapy intervention for service members with chronic symptoms following MTBI, Archives of Physical Medicine and Rehabilitation, 98, e132, 2017 | Conference abstract. |
| Conneeley, A. L., Transitions and brain injury: A qualitative study exploring the journey of people with traumatic brain injury, Brain Impairment, 13, 72–84, 2012 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Conneeley, Anne Louise, Exploring vocation following brain injury: a qualitative enquiry, Social Care and Neurodisability, 4, 6–16, 2013 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Copley, Anna, McAllister, Lindy, Wilson, Linda, Attitride-Stirling, Barnes Brooks Carr-Hill Fagen Foster Frattali Grbich Harradine Harris Honey Humphreys Johnstone Kelly LeFebvre Marsh Minichiello Morse Murphy Muus Nabors Newberry O’Callaghan O’Callaghan O’Callaghan O’Callaghan O’Callaghan Patton Sample Sample Schofield Schwandt Turner-Stokes Whitehead Ylvisaker Youse, We finally learnt to demand: Consumers’ access to rehabilitation following traumatic brain injury, Brain Impairment, 14, 436–449, 2013 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Curtis, Kate, Foster, Kim, Mitchell, Rebecca, Van, Connie, How is care provided for patients with paediatric trauma and their families in Australia? A mixed-method study, Journal of Paediatrics and Child Health, 52, 832–6, 2016 [PubMed: 27203550] | Study did not examine the phenomena of interest. |
| Cuthbert, J., Anderson, J., Mason, C., Block, S., Dettmer, J., Weintraub, A., Harrison-Felix, C., Case management of individuals with chronic TBI: A research-based approach, Journal of Head Trauma Rehabilitation, 28, E49, 2013 | Conference abstract. |
| Daggett, Virginia S., Bakas, Tamilyn, Buelow, Janice, Habermann, Barbara, Murray, Laura L., Needs and concerns of male combat Veterans with mild traumatic brain injury, Journal of Rehabilitation Research and Development, 50, 327–40, 2013 [PubMed: 23881759] | Study not conducted in one of the countries included in the review protocol. |
| Dahl, O., Wickman, M., Wengstrom, Y., Adapting to life after burn injury-reflections on care, Journal of Burn Care and Research, 33, 595–605, 2012 [PubMed: 22210069] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Dalmaso, Kym, Weber, Sarah, Eley, Rob, Spencer, Lyndall, Cabilan, C. J., Nurses’ perceived benefits of trauma nursing rounds (TNR) on clinical practice in an Australian emergency department: a mixed methods study, Australasian emergency nursing journal : AENJ, 18, 42–8, 2015 [PubMed: 25601428] | Setting not in PICO: Emergency department. |
| Dams-O’Connor, K., Landau, A., De Lore, J. S., Hoffman, J., Access, barriers, and health care quality after brain injury: Insiders’ perspectives, Archives of Physical Medicine and Rehabilitation, 97, e129, 2016 | Conference abstract. |
| Dams-O’Connor, Kristen, Landau, Alexandra, Hoffman, Jeanne, St De Lore, Jef, Patient perspectives on quality and access to healthcare after brain injury, Brain Injury, 32, 431–441, 2018 [PubMed: 29388840] | Study not conducted in one of the countries included in the review protocol. |
| Darnell, Doyanne A., Parker, Lea E., Wagner, Amy W., Dunn, Christopher W., Atkins, David C., Dorsey, Shannon, Zatzick, Douglas F., Task-shifting to improve the reach of mental health interventions for trauma patients: findings from a pilot study of trauma nurse training in patient-centered activity scheduling for PTSD and depression, Cognitive behaviour therapy, 48, 482–496, 2019 [PMC free article: PMC6542717] [PubMed: 30499372] | Study not conducted in one of the countries included in the review protocol. |
| D’Cruz, K., Howie, L., Lentin, P., Client-centred practice: Perspectives of persons with a traumatic brain injury, Scandinavian Journal of Occupational Therapy, 23, 30–38, 2016 [PubMed: 26094733] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Dickson, Adele, Ward, Richard, O’Brien, Grainne, Allan, David, O’Carroll, Ronan, Difficulties adjusting to post-discharge life following a spinal cord injury: an interpretative phenomenological analysis, Psychology, health & medicine, 16, 463–74, 2011 [PubMed: 21749243] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Diener, M., Kirby, A., Canary, H., Sumison, F., Green, M., Community reintegration following pediatric acquired brain injury: Perspectives of providers and families, Journal of Head Trauma Rehabilitation, 33 (3), E97, 2018 | Conference abstract. |
| Dillahunt-Aspillaga, C., Bradley, S., Ramaiah, P., Radwan, C., Ottomanelli, L., Coalition Building: A Tool To Implement Evidenced-Based Resource Facilitation in The VHA: Pilot Results, Archives of Physical Medicine and Rehabilitation, 100, e164, 2019 | Conference abstract. |
| Dismann, Patrick D., Maignan, Maxime, Cloves, Paul D., Gutierrez Parres, Blanca, Dickerson, Sara, Eberhardt, Alice, A Review of the Burden of Trauma Pain in Emergency Settings in Europe, Pain and therapy, 7, 179–192, 2018 [PMC free article: PMC6251834] [PubMed: 29860585] | Setting not in PICO: Emergency settings. |
| Divanoglou, A., Georgiou, M., Perceived effectiveness and mechanisms of community peer-based programmes for Spinal Cord Injuries-a systematic review of qualitative findings, Spinal cord, 55, 225–234, 2017 [PubMed: 27845356] | Study did not report any findings related to the phenomena of interest. |
| Doig, E., Fleming, J., Kuipers, P., Cornwell, P., The relationship between goal attainment and the development of self-awareness in traumatic brain injury (TBI) rehabilitation: Descriptive and qualitative case analyses, Brain Impairment, 14, 159–160, 2013 | Conference abstract. |
| Doig, Emmah, Fleming, Jennifer, Cornwell, Petrea, Kuipers, Pim, Comparing the experience of outpatient therapy in home and day hospital settings after traumatic brain injury: patient, significant other and therapist perspectives, Disability and Rehabilitation, 33, 1203–14, 2011 [PubMed: 20977391] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Donnell, Zoe, Hoffman, Roseanne, Myers, Gaya, Sarmiento, Kelly, Seeking to improve care for young patients: Development of tools to support the implementation of the CDC Pediatric mTBI Guideline, Journal of Safety Research, 67, 203–209, 2018 [PMC free article: PMC6445253] [PubMed: 30553425] | Study not conducted in one of the countries included in the review protocol. |
| Donnelly, Kyla Z., Goldberg, Shari, Fournier, Debra, A qualitative study of LoveYourBrain Yoga: a group-based yoga with psychoeducation intervention to facilitate community integration for people with traumatic brain injury and their caregivers, Disability and Rehabilitation, 1–10, 2019 [PubMed: 30741032] | Study not conducted in one of the countries included in the review protocol. |
| Douglas, J., ‘Nobody wants to know you’. Understanding the experience of friendship following severe traumatic brain injury, Brain Injury, 30, 515, 2016 | Conference abstract. |
| Drew, S., Judge, A., Cooper, C., Javaid, M. K., Farmer, A., Gooberman-Hill, R., Secondary prevention of fractures after hip fracture: a qualitative study of effective service delivery, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 27, 1719–27, 2016 [PMC free article: PMC4839047] [PubMed: 26759249] | Study did not examine rehabilitation. |
| Drew, S., Judge, A., Javaid, M. K., Cooper, C., Farmer, A., Goobermen-Hill, R., Secondary prevention of fractures after hip fracture: A qualitative study of effective service delive, Osteoporosis International, 25, S308, 2014 [PMC free article: PMC4839047] [PubMed: 26759249] | Conference abstract. |
| Dwyer, Aoife, Heary, Caroline, Ward, Marcia, MacNeela, Padraig, Adding insult to brain injury: young adults’ experiences of residing in nursing homes following acquired brain injury, Disability and Rehabilitation, 41, 33–43, 2019 [PubMed: 28845724] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Dyke, J., Krupa, J., Vova, J., Medical symptoms, service gaps and barriers to care using the medical home model in adolescents with acquired brain injury, Journal of Head Trauma Rehabilitation, 27 (5), E18–E19, 2012 | Conference abstract. |
| Edworthy Ann, Donne Hannah, The availability and intelligibility of information for carers of children with a brain injury, Social Care and Neurodisability, 1, 32–40, 2010 | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Eliacin, Johanne, Fortney, Sarah, Rattray, Nicholas A., Kean, Jacob, Access to health services for moderate to severe TBI in Indiana: patient and caregiver perspectives, Brain Injury, 32, 1510–1517, 2018 [PubMed: 30036117] | Study not conducted in one of the countries included in the review protocol. |
| Fitts, M., Fleming, J., Bird, K., Condon, T., Gilroy, J., Clough, A., Maruff, P., Esterman, A., Bohanna, I., Sentinel events during hospital admission for indigenous people following traumatic brain injury, Brain Impairment, 19, 336, 2018 | Conference abstract. |
| Fitts, Michelle S., Bird, Katrina, Gilroy, John, Fleming, Jennifer, Clough, Alan R., Esterman, Adrian, Maruff, Paul, Fatima, Yaqoot, Bohanna, India, Abrahamson, Alfandre Amery Bell Blackmer Bohanna Bohanna Bohanna Braun Burnett Choi Claiborne Coronado D’Cruz Dillon Dudley Durey Durey Einsiedel Englander Feigin Foley Franks Gentilello Gilroy Gilroy Harrison Hunt Hyder Jamieson Jayaraj Juillard Katzenellenbogen Katzenellenbogen Lakhani Lee Levack Levack Liossi Marrone Martin Moreton-Robinson Nakata Nalder Nalder Nalder Niemeier Ownsworth Paradies Rutland-Brown Shahid Tuhiwai-Smith Turner Turner Willis Zeiler, A qualitative study on the transition support needs of indigenous Australians following traumatic brain injury, Brain Impairment, 20, 137–159, 2019 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Fleming, Jennifer, Sampson, Jennifer, Cornwell, Petrea, Turner, Ben, Griffin, Janell, Brain injury rehabilitation: The lived experience of inpatients and their family caregivers, Scandinavian journal of occupational therapy, 19, 184–193, 2012 [PubMed: 21936734] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Ford, James H., 2nd, Wise, Meg, Krahn, Dean, Oliver, Karen Anderson, Hall, Carmen, Sayer, Nina, Family care map: Sustaining family-centered care in Polytrauma Rehabilitation Centers, Journal of Rehabilitation Research and Development, 51, 1311–24, 2014 [PMC free article: PMC4560363] [PubMed: 25671632] | Study not conducted in one of the countries included in the review protocol. |
| Foster, Kim, Mitchell, Rebecca, Van, Connie, Young, Alexandra, McCloughen, Andrea, Curtis, Kate, Resilient, recovering, distressed: A longitudinal qualitative study of parent psychosocial trajectories following child critical injury, Injury, 50, 1605–1611, 2019 [PubMed: 31101410] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Foster, Kim, Mitchell, Rebecca, Young, Alexandra, Van, Connie, Curtis, Kate, Parent experiences and psychosocial support needs 6 months following paediatric critical injury: A qualitative study, Injury, 50, 1082–1088, 2019 [PubMed: 30655002] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences reviews. |
| Foster, Kim, Young, Alexandra, Mitchell, Rebecca, Van, Connie, Curtis, Kate, Experiences and needs of parents of critically injured children during the acute hospital phase: A qualitative investigation, Injury, 48, 114–120, 2017 [PubMed: 27692666] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Fournier, D., Goldberg, S., Figucia, C., Kennedy, P., Krauss, K., Smith, C., Springmann, J., An interdisciplinary traumatic brain injury clinic: Understanding the patient experience, Journal of Head Trauma Rehabilitation, 32, E97–E98, 2017 | Conference abstract. |
| Francis, A., Ziviani, J., Fleming, J., Rae, M., McKinlay, L., Transitioning to adulthood: Needs of young people with an acquired brain injury and those of their families, Neurorehabilitation and Neural Repair, 26, 780–781, 2012 | Conference abstract. |
| Franz, Shiney, Muser, Jurgen, Thielhorn, Ulrike, Wallesch, Claus W., Behrens, Johann, Inter-professional communication and interaction in the neurological rehabilitation team: a literature review, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30457016] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Fraser, M. A., Lind, J. D., Powell-Cope, G., Gavin-Dreschnack, D., Addressing non-direct care, psychosocial concerns of veterans with spinal cord injuries, Journal of Spinal Cord Medicine, 36, 546–547, 2013 | Conference abstract. |
| Freeman, Claire, Cassidy, Bernadette, Hay-Smith, E. Jean C., Beauregard, Beisecker Chan Craig DeSanto-Madeya Dickson Dixon Ell Esmail Esmail Fisher Fronek Gilad Kendall Kennedy Kidd Kreuter Leino-Kilpi Lemonidou New Parrott Racher Rembis Schuster Sinnott Smith Smith Steinglass Taylor Vocaturo, Couple’s experiences of relationship maintenance and intimacy in acute spinal cord injury rehabilitation: An interpretative phenomenological analysis, Sexuality and Disability, 35, 433–444, 2017 | Study did not examine phenomena of interest. |
| Fry, J. C., Price, P., Meeting the re-integration needs of individuals with spinal cord injury: Effectiveness of community-based occupational therapy, Archives of Physical Medicine and Rehabilitation, 94, e8, 2013 | Conference abstract. |
| Gabbe, Belinda J., Sleney, Jude S., Gosling, Cameron M., Wilson, Krystle, Hart, Melissa J., Sutherland, Ann M., Christie, Nicola, Patient perspectives of care in a regionalised trauma system: lessons from the Victorian State Trauma System, The Medical journal of Australia, 198, 149–52, 2013 [PubMed: 23418695] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Gagliardi, Anna R., Nathens, Avery B., Exploring the characteristics of high-performing hospitals that influence trauma triage and transfer, The journal of trauma and acute care surgery, 78, 300–5, 2015 [PubMed: 25757114] | Study did not examine rehabilitation. |
| Gagnon, I., Friedman, D., Management of mild traumatic brain injury or concussion in children: Is there a role for the physical therapist?, Physiotherapy (United Kingdom), 1), eS1487–eS1488, 2011 | Conference abstract. |
| Garrino, Lorenza, Curto, Natascia, Decorte, Rita, Felisi, Nadia, Matta, Ebe, Gregorino, Silvano, Actis, M. Vittoria, Marchisio, Cecilia, Carone, Roberto, Towards personalized care for persons with spinal cord injury: a study on patients’ perceptions, The journal of spinal cord medicine, 34, 67–75, 2011 [PMC free article: PMC3066480] [PubMed: 21528629] | Study did not examine phenomena of interest. |
| Gawel, Marcie, Emerson, Beth, Giuliano, John S., Jr., Rosenberg, Alana, Minges, Karl E., Feder, Shelli, Violano, Pina, Morrell, Patricia, Petersen, Judy, Christison-Lagay, Emily, Auerbach, Marc, A Qualitative Study of Multidisciplinary Providers’ Experiences With the Transfer Process for Injured Children and Ideas for Improvement, Pediatric Emergency Care, 34, 125–131, 2018 [PMC free article: PMC5792311] [PubMed: 29346234] | Study not conducted in one of the countries included in the review protocol. |
| Gemmel, Paul, van Steenis, Thomas, Meijboom, Bert, Bensabat, Bohmer Broekhuis Burke Chase Chase Chase Eisenhardt Fredendall Frei Gronroos Hanne Johnston Lamontagne Lamontagne Larsson Meredith Metters Metters Miles Ouwens Patricio Swanborn Vander Laane Voss Westert Yin Young Zomerdijk, Front-office/back-office configurations and operational performance in complex health services, Brain Injury, 28, 347–356, 2014 [PubMed: 24568302] | Not specific to rehabilitation, or to traumatic injury and results not presented separately for target population. |
| Gill, Carol J., Sander, Angelle M., Robins, Nina, Mazzei, Diana, Struchen, Margaret A., Allen, Aloni Aloni Anderson Anderson-Parente Bergland Brooks Ergh Garden Gillen Gosling Harrick Hibbard Hoofien Jeon Kersel Kravetz Kravetz Kreuter Kreutzer Kreutzer Kreutzer Lippert Marsh Oddy Olver Panting Patton Perlesz Peters Ponsford Porter Resnick Rosenbaum Sandel Siebert Snow Tate Tate Thomsen Vanderploeg Wallace Webster Wells Wood Wood, Exploring experiences of intimacy from the viewpoint of individuals with traumatic brain injury and their partners, The Journal of Head Trauma Rehabilitation, 26, 56–68, 2011 [PubMed: 21209563] | Study not conducted in one of the countries included in the review protocol. |
| Gill, Ian J., Wall, Gemma, Simpson Jane, Clients’ perspectives of rehabilitation in one acquired brain injury residential rehabilitation unit: a thematic analysis, Brain Injury, 26, 909–20, 2012 [PubMed: 22571407] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Glintborg, C., Hansen, T., De La Mata Benites, M., Supporting transitions in neurorehabilitation. A pathway to improved psychosocial outcomes, Brain Injury, 30, 565–566, 2016 | Conference abstract. |
| Glintborg, Chalotte, Hansen, Tia G. B., Bech, Bech Braun Brenner Creswell Ellervik Engel Ghaziani Glintborg Glintborg Glintborg Glintborg Hackett Haggerty Hald Hall Holm Jorge Jorge Keith Kennedy Miles Morton Norholm Pallant Rivera Schlossberg Teasdale Teasdale Turner, Bio-psycho-social effects of a coordinated neurorehabilitation programme: A naturalistic mixed methods study, NeuroRehabilitation, 38, 99–113, 2016 [PubMed: 26889730] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Goel, R., Fruth, S., Geigle, P., Santurri, L., Abzug, J., Telerehabilitation for Individuals With Spinal Cord Injury: Is it Feasible?, Archives of Physical Medicine and Rehabilitation, 100, e203–e204, 2019 | Conference abstract. |
| Goldsmith, Helen, McCloughen, Andrea, Curtis, Kate, Using the trauma patient experience and evaluation of hospital discharge practices to inform practice change: A mixed methods study, Journal of Clinical Nursing, 27, 1589–1598, 2018 [PubMed: 29266578] | Study did not examine rehabilitation. |
| Goldsmith, Helen, McCloughen, Andrea, Curtis, Kate, The experience and understanding of pain management in recently discharged adult trauma patients: A qualitative study, Injury, 49, 110–116, 2018 [PubMed: 28988804] | No qualitative data on phenomena of interest. |
| Goodridge, Donna, Rogers, Marla, Klassen, Laura, Jeffery, Bonnie, Knox, Katherine, Rohatinsky, Noelle, Linassi, Gary, Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas, Disability and Rehabilitation, 37, 1401–10, 2015 [PubMed: 25332089] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Gotlib Conn, Lesley, Zwaiman, Ashley, DasGupta, Tracey, Hales, Brigette, Watamaniuk, Aaron, Nathens, Avery B., Trauma patient discharge and care transition experiences: Identifying opportunities for quality improvement in trauma centres, Injury, 49, 97–103, 2018 [PubMed: 28988066] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Gourdeau, Jenna, Fingold, Alissa, Colantonio, Angela, Mansfield, Elizabeth, Stergiou-Kita, Mary, Workplace accommodations following work-related mild traumatic brain injury: what works?, Disability and Rehabilitation, 1–10, 2018 [PubMed: 30451033] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Gravell, R., Brumfit, S., Body, R., Hope and engagement following acquired brain injury: A qualitative study, Brain Injury, 31, 721–722, 2017 | Conference abstract. |
| Guilcher, S., Everall, A., Wodchis, W., Joanna, deGraaf-Dunlop, Bar-Ziv, S., Kuluski, K., Understanding Transitions of Care in Older Adults With Hip Fractures: A Multiple-Case Study in Ontario, Archives of Physical Medicine and Rehabilitation, 100, e138, 2019 | Conference abstract. |
| Gullick, Janice G., Taggart, Susan B., Johnston, Rae A., Ko, Natalie, The trauma bubble: patient and family experience of serious burn injury, Journal of burn care & research : official publication of the American Burn Association, 35, e413–27, 2014 [PubMed: 25144806] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Guptill, C. A., The lived experience of professional musicians with playing-related injuries: A phenomenological inquiry, Medical Problems of Performing Artists, 26, 84–95, 2011 [PubMed: 21695356] | No qualitative data on phenomena of interest. |
| Haarbauer-Krupa, J., Vova, J., Follow-up of preschool children with acquired brain injury, Brain Injury, 26, 424–425, 2012 | Conference abstract. |
| Haas, B. M., Price, L., Freeman, J. A., Qualitative evaluation of a community peer support service for people with spinal cord injury, Spinal Cord, 51, 295–9, 2013 [PubMed: 23184023] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Harrington, Rosamund, Foster, Michele, Fleming, Jennifer, Experiences of pathways, outcomes and choice after severe traumatic brain injury under no-fault versus fault-based motor accident insurance, Brain Injury, 29, 1561–71, 2015 [PubMed: 26382715] | No qualitative data on phenomena of interest. |
| Harris, M. B., Rafeedie, S., McArthur, D., Babikian, T., Snyder, A., Polster, D., Giza, C. C., Addition of Occupational Therapy to an Interdisciplinary Concussion Clinic Improves Identification of Functional Impairments, Journal of Head Trauma Rehabilitation, 34, 425–432, 2019 [PubMed: 31688379] | Study not conducted in one of the countries included in the review protocol. |
| Harrison, Anne L., Hunter, Elizabeth G., Thomas, Heather, Bordy, Paige, Stokes, Erin, Kitzman, Patrick, Living with traumatic brain injury in a rural setting: supports and barriers across the continuum of care, Disability and Rehabilitation, 39, 2071–2080, 2017 [PMC free article: PMC5654530] [PubMed: 27549899] | Study not conducted in one of the countries included in the review protocol. |
| Hartley, Naomi A., Spinal cord injury (SCI) rehabilitation: systematic analysis of communication from the biopsychosocial perspective, Disability and rehabilitation, 1–10, 2015 [PubMed: 25801919] | Study not conducted in one of the countries included in the review protocol. |
| Hawkins, Brent L., Crowe, Brandi M., Contextual Facilitators and Barriers of Community Reintegration Among Injured Female Military Veterans: A Qualitative Study, Archives of Physical Medicine and Rehabilitation, 99, S65–S71, 2018 [PubMed: 28866010] | Study not conducted in one of the countries included in the review protocol. |
| Haywood, C., Perceptions of recovery among adolescents and young adults with acquired spinal cord injuries, Archives of Physical Medicine and Rehabilitation, 97, e76, 2016 | Conference abstract. |
| Haywood, Carol, Pyatak, Elizabeth, Leland, Natalie, Henwood, Benjamin, Lawlor, Mary C., A Qualitative Study of Caregiving for Adolescents and Young Adults With Spinal Cord Injuries: Lessons From Lived Experiences, Topics in Spinal Cord Injury Rehabilitation, 25, 281–289, 2019 [PMC free article: PMC6907026] [PubMed: 31844380] | Study not conducted in one of the countries included in the review protocol. |
| Hellem, I., Forland, G., Eide, K., Ytrehus, S., Addressing uncertainty and stigma in social relations related to hidden dysfunctions following acquired brain injury, Scandinavian Journal of Disability Research, 20, 152–161, 2018 | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Herrera-Escobar, J. P., Columbus, A., Castillo-Angeles, M., Rios-Diaz, A. J., Weed, C. N., Kasotakis, G., Velmahos, G. C., Salim, A., Haider, A. H., Kaafara, H. M., Discontinuity of patient-provider communication throughout the phases of care: Time to be more patient-centered in trauma?, Journal of the American College of Surgeons, 225 (4 Supplement 2), e176, 2017 | Conference abstract. |
| Hill, Jennifer N., Smith, Bridget M., Weaver, Frances M., Nazi, Kim M., Thomas, Florian P., Goldstein, Barry, Hogan, Timothy P., Potential of personal health record portals in the care of individuals with spinal cord injuries and disorders: Provider perspectives, The journal of spinal cord medicine, 41, 298–308, 2018 [PMC free article: PMC6055947] [PubMed: 28325112] | Study not conducted in one of the countries included in the review protocol. |
| Hines, M., Brunner, M., Poon, S., Lam, M., Tran, V., Yu, D., Togher, L., Shaw, T., Power, E., Exploring ehealth ‘tribes and tribulations’ in interdisciplinary rehabilitation for people with a traumatic brain injury (TBI), Brain Impairment, 19, 292–293, 2018 | Conference abstract. |
| Hines, M., Brunner, M., Poon, S., Lam, M., Tran, V., Yu, D., Togher, L., Shaw, T., Power, E., Tribes and tribulations: interdisciplinary eHealth in providing services for people with a traumatic brain injury (TBI), BMC health services research, 17, 757, 2017 [PMC free article: PMC5697081] [PubMed: 29162086] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Hirsch, M. A., Grafton, L., Guerrier, T. P., Niemeier, J. P., Newman, M., Runyon, M. S., Unmet concussion care needs from the perspective of individuals with mild traumatic brain injury, Archives of Physical Medicine and Rehabilitation, 96, e33, 2015 | Conference abstract. |
| Hitzig, S., Bain, P., Haycock, S., Hebert, D. A., Evaluation of a spinal cord injury community reintegration outpatient program (CROP) service, Archives of Physical Medicine and Rehabilitation, 95, e83, 2014 [PMC free article: PMC4276116] [PubMed: 25574397] | Conference abstract. |
| Hollick, R., Reid, D., Black, A., McKee, L., What matters to patients: Working together to improve the quality of osteoporosis services, Osteoporosis International, 27, S678, 2016 | Conference abstract. |
| Holloway, Mark, Motivational interviewing and acquired brain injury, Social Care and Neurodisability, 3, 122–130, 2012 | Narrative review. |
| Hoogerdijk, Barbara, Runge, Ulla, Haugboelle, Jette, The adaptation process after traumatic brain injury an individual and ongoing occupational struggle to gain a new identity, Scandinavian Journal of Occupational Therapy, 18, 122–32, 2011 [PubMed: 20384550] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Hoonakker, Peter Leonard Titus, Wooldridge, Abigail Rayburn, Hose, Bat-Zion, Carayon, Pascale, Eithun, Ben, Brazelton, Thomas Berry, 3rd, Kohler, Jonathan Emerson, Ross, Joshua Chud, Rusy, Deborah Ann, Dean, Shannon Mason, Kelly, Michelle Merwood, Gurses, Ayse Pinar, Information flow during pediatric trauma care transitions: things falling through the cracks, Internal and emergency medicine, 14, 797–805, 2019 [PMC free article: PMC6692560] [PubMed: 31140061] | Study not conducted in one of the countries included in the review protocol. |
| Hosking, J. E., Ameratunga, S. N., Bramley, D. M., Crengle, S. M., Reducing ethnic disparities in the quality of trauma care: An important research gap, Annals of Surgery, 253, 233–237, 2011 [PubMed: 21173692] | Study did not examine rehabilitation. |
| Hull, K., Ribariach, J., Panton, V., De Jonge, J., Bulsara, C., Developing independence and empowerment through medications self management amongst persons with acquired brain injury, Neurorehabilitation and Neural Repair, 26, 775–776, 2012 | Conference abstract. |
| Hunt, Anne W., Laupacis, Dylan, Kawaguchi, Emily, Greenspoon, Dayna, Reed, Nick, Key ingredients to an active rehabilitation programme post-concussion: perspectives of youth and parents, Brain Injury, 32, 1534–1540, 2018 [PubMed: 30047796] | It was not clear that the participants had been hospitalised (study states that the intervention/ interviews were undertaken in a hospital but many of the participants were drawn from the community). |
| Hyatt, Kyong, Davis, Linda L., Barroso, Julie, Chasing the care: soldiers experience following combat-related mild traumatic brain injury, Military Medicine, 179, 849–55, 2014 [PubMed: 25102527] | Study not conducted in one of the countries included in the review protocol. |
| Irgens, Eirik Lind, Henriksen, Nils, Moe, Siri, Communicating information and professional knowledge in acquired brain injury rehabilitation trajectories - a qualitative study of physiotherapy practice, Disability and Rehabilitation, 1–8, 2018 [PubMed: 30572746] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Jacoby, Sara F., Rich, John A., Webster, Jessica L., Richmond, Therese S., ‘Sharing things with people that I don’t even know’: help-seeking for psychological symptoms in injured Black men in Philadelphia, Ethnicity & health, 1–19, 2018 [PMC free article: PMC6167172] [PubMed: 29607675] | Study not conducted in one of the countries included in the review protocol. |
| Jannings, Wendy, Pryor, Julie, The experiences and needs of persons with spinal cord injury who can walk, Disability and Rehabilitation, 34, 1820–6, 2012 [PubMed: 22423597] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Janssen, Renske M. J., Satink, Ton, Ijspeert, Jos, van Alfen, Nens, Groothuis, Jan T., Packer, Tanya L., Cup, Edith H. C., Reflections of patients and therapists on a multidisciplinary rehabilitation programme for persons with brachial plexus injuries, Disability and Rehabilitation, 41, 1427–1434, 2019 [PubMed: 29385821] | Population not in PICO: Participants had not experienced traumatic injury. |
| Jellema, Sandra, van Erp, Sabine, Nijhuis-van der Sanden, Maria W. G., van der Sande, Rob, Steultjens, Esther M. J., Activity resumption after acquired brain injury: the influence of the social network as described by social workers, Disability and Rehabilitation, 1–8, 2019 [PubMed: 31429344] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jeyathevan, Gaya, Cameron, Jill I., Craven, B. Catharine, Jaglal, Susan B., Identifying Required Skills to Enhance Family Caregiver Competency in Caring for Individuals With Spinal Cord Injury Living in the Community, Topics in Spinal Cord Injury Rehabilitation, 25, 290–302, 2019 [PMC free article: PMC6907029] [PubMed: 31844381] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jeyathevan, Gaya, Catharine Craven, B., Cameron, Jill I., Jaglal, Susan B., Facilitators and barriers to supporting individuals with spinal cord injury in the community: experiences of family caregivers and care recipients, Disability and Rehabilitation, 111, 2019 [PubMed: 30669882] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jiang, T., Webster, J. L., Robinson, A., Kassam-Adams, N., Richmond, T. S., Emotional responses to unintentional and intentional traumatic injuries among urban black men: A qualitative study, Injury, 49, 983–989, 2018 [PMC free article: PMC5932248] [PubMed: 29248186] | Study not conducted in one of the countries included in the review protocol. |
| Johnson, Rae A., Taggart, Susan B., Gullick, Janice G., Emerging from the trauma bubble: Redefining ‘normal’ after burn injury, Burns : journal of the International Society for Burn Injuries, 42, 1223–32, 2016 [PubMed: 27237124] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Jourdan, C., Azouvi, P., Pradat-Diehl, P., Ruet, A., Tenovuo, O., Traumatic Brain Injury (TBI) care pathways in Finland and in France: Organization and issues, Annals of Physical and Rehabilitation Medicine, 57, e397, 2014 | Conference abstract. |
| Jurrius, K., After care for people with acquired brain injury in the chronic phase-New equilibrium in the aftercare of people with acquired brain injury and their next of kin, Brain Injury, 30, 567, 2016 | Conference abstract. |
| Keck, Casey S., Creaghead, Nancy A., Turkstra, Lyn S., Vaughn, Lisa M., Kelchner, Lisa N., Pragmatic skills after childhood traumatic brain injury: Parents’ perspectives, Journal of communication disorders, 69, 106–118, 2017 [PubMed: 28898709] | Study not conducted in one of the countries included in the review protocol. |
| Keenan, Alanna, Joseph, Lynn, The needs of family members of severe traumatic brain injured patients during critical and acute care: a qualitative study, Canadian journal of neuroscience nursing, 32, 25–35, 2010 [PubMed: 20865832] | Mixed setting and population, results not presented separately for the target settings and population. |
| Keightley, Michelle, Kendall, Victoria, Jang, Shu-Hyun, Parker, Cindy, Agnihotri, Sabrina, Colantonio, Angela, Minore, Bruce, Katt, Mae, Cameron, Anita, White, Randy, Longboat-White, Claudine, Bellavance, Alice, From health care to home community: an Aboriginal community-based ABI transition strategy, Brain Injury, 25, 142–52, 2011 [PubMed: 21219087] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Kellezi, Blerina, Beckett, Kate, Earthy, Sarah, Barnes, Jo, Sleney, Jude, Clarkson, Julie, Regel, Stephen, Jones, Trevor, Kendrick, Denise, Understanding and meeting information needs following unintentional injury: comparing the accounts of patients, carers and service providers, Injury, 46, 564–71, 2015 [PubMed: 25533126] | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Kennedy, P., Sherlock, O., McClelland, M., Short, D., Royle, J., Wilson, C., A multi-centre study of the community needs of people with spinal cord injuries: the first 18 months, Spinal Cord, 48, 15–20, 2010 [PubMed: 19528997] | No qualitative data on phenomena of interest. |
| Kersten, Paula, Cummins, Christine, Kayes, Nicola, Babbage, Duncan, Elder, Hinemoa, Foster, Allison, Weatherall, Mark, Siegert, Richard John, Smith, Greta, McPherson, Kathryn, Making sense of recovery after traumatic brain injury through a peer mentoring intervention: a qualitative exploration, BMJ Open, 8, e020672, 2018 [PMC free article: PMC6252636] [PubMed: 30309988] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Kiekens, C., Christiaens, W., Van Den Heede, K., Organization of aftercare for patients with severe burn injuries in Belgium, Annals of Physical and Rehabilitation Medicine, 57, e212–e213, 2014 | Conference abstract. |
| Kimmel, Lara A., Holland, Anne E., Hart, Melissa J., Edwards, Elton R., Page, Richard S., Hau, Raphael, Bucknill, Andrew, Gabbe, Belinda J., Discharge from the acute hospital: trauma patients’ perceptions of care, Australian health review : a publication of the Australian Hospital Association, 40, 625–632, 2016 [PubMed: 26910554] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Kimmel, Lara A., Holland, Anne E., Lannin, Natasha, Edwards, Elton R., Page, Richard S., Bucknill, Andrew, Hau, Raphael, Gabbe, Belinda J., Clinicians’ perceptions of decision making regarding discharge from public hospitals to in-patient rehabilitation following trauma, Australian health review : a publication of the Australian Hospital Association, 41, 192–200, 2017 [PubMed: 27144728] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Kingston, Gail A., Judd, Jenni, Gray, Marion A., The experience of medical and rehabilitation intervention for traumatic hand injuries in rural and remote North Queensland: a qualitative study, Disability and Rehabilitation, 37, 423–9, 2015 [PubMed: 24856789] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Kingston, Gail A., Judd, Dr Jenni, Gray, Marion A., The experience of living with a traumatic hand injury in a rural and remote location: an interpretive phenomenological study, Rural and remote health, 14, 2764, 2014 [PubMed: 25018127] | No qualitative data on phenomena of interest. |
| Kirk, S., Fallon, D., Fraser, C., Robinson, G., Vassallo, G., Supporting parents following childhood traumatic brain injury: a qualitative study to examine information and emotional support needs across key care transitions, Child: care, health and development, 41, 303–313, 2015 [PubMed: 25039833] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Kivunja, Stephen, River, Jo, Gullick, Janice, Experiences of giving and receiving care in traumatic brain injury: An integrative review, Journal of clinical nursing, 27, 1304–1328, 2018 [PubMed: 29396883] | Systematic review, included studies checked for relevance. |
| Kjaersgaard, A., Kristensen, H. K., Brain injury and severe eating difficulties at admission-patient perspective nine to fifteen months after discharge: A pilot study, Brain Sciences, 7, 96, 2017 [PMC free article: PMC5575616] [PubMed: 28783098] | Unclear how many participants had experienced traumatic injury, the results not presented separately for target population. |
| Knox, L., Douglas, J., Bigby, C., Exploring tensions associated with supported decision making in adults with severe traumatic brain injury, Brain Injury, 26, 477, 2012 | Conference abstract. |
| Koehmstedt, Christine, Lydick, Susan E., Patel, Drasti, Cai, Xinsheng, Garfinkel, Steven, Weinstein, Ali A., Health status, difficulties, and desired health information and services for veterans with traumatic brain injuries and their caregivers: A qualitative investigation, PLoS ONE, 13, e0203804, 2018 [PMC free article: PMC6135487] [PubMed: 30208083] | Study not conducted in one of the countries included in the review protocol. |
| Koizia, L., Kings, R., Koizia, A., Peck, G., Wilson, M., Hettiaratchy, S., Fertleman, M. B., Major trauma in the elderly: Frailty decline and patient experience after injury, Trauma (United Kingdom), 21, 21–26, 2019 [PMC free article: PMC6262588] [PubMed: 30581355] | Not a qualitative study. |
| Koller, Kathryn, Woods, Lindsay, Engel, Lisa, Bottari, Carolina, Dawson, Deirdre R., Nalder, Emily, Bandura, Bottari Braun Chen Colantonio Creswell Dreer Engel Fleming Fox Gaudette Hall Hoskin Kelley Kershaw Kim Knight Kreutzer Langlois Levack Malee Marson Martin McCabe McHugh Patton Poncer Weiner, Loss of financial management independence after brain injury: Survivors’ experiences, American Journal of Occupational Therapy, 70, No-Specified, 2016 [PubMed: 27089291] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Kontos, P., Miller, K. L., Colantonio, A., Cott, C., Therapeutic landscape theory: Identifying health detracting and health enhancing aspects of neurorehabilitation, Brain Injury, 28, 535, 2014 | Conference abstract. |
| Kornhaber, R., Wilson, A., Abu-Qamar, M., McLean, L., Vandervord, J., Inpatient peer support for adult burn survivors-a valuable resource: a phenomenological analysis of the Australian experience, Burns : journal of the International Society for Burn Injuries, 41, 110–7, 2015 [PubMed: 24927991] | Study did not examine phenomena of interest. |
| Kozlowski-Moreau, O., Danze, F., Pollez, B., Brooks, N., Johnson, C., Line, M. C., Rousseaux, M., Croisiaux, C., Lanthier, A., Long-term management of severe TBI in Europe-The value of a network, Brain Injury, 30, 650, 2016 | Conference abstract. |
| Kuipers, Pim, Kendall, Melissa B., Amsters, Delena, Pershouse, Kiley, Schuurs, Sarita, Descriptions of community by people with spinal cord injuries: concepts to inform community integration and community rehabilitation, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 34, 167–74, 2011 [PubMed: 21490508] | No qualitative data on phenomena of interest. |
| Lafebvre, H., Levert, M. J., Gelinas, I., Croteau, C., Le Dorze, G., Bottari, C., McKerrall, M., Personalized accompaniment for community integration for people with a traumatic brain injury in postrehabilitation, Archives of Physical Medicine and Rehabilitation, 91, e7, 2010 | Conference abstract. |
| Lamontagne, M. E., Swaine, B. R., Lavoie, A., Careau, E., Analysis of the strengths, weaknesses, opportunities and threats of the network form of organization of traumatic brain injury service delivery systems, Brain Injury, 25, 1188–1197, 2011 [PubMed: 21939374] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Lange, R., French, L., Bailie, J., Lippa, S., Gartner, R., Driscoll, A., Wright, M., Smith, J., Dilay, A., Pizzano, B., Johnson, L., Nora, D., Mahatan, H., Sullivan, J., Thompson, D., Snelling, A., Brickell, T., Caring for U.S. military service members following mild-moderate traumatic brain injury: Examination of access to services, service needs, and barriers to care, Journal of Head Trauma Rehabilitation, 32, E71, 2017 | Conference abstract. |
| Lannin, N., Roberts, K., D’Cruz, K., Morarty, J., Unsworth, C., Who holds the ‘Power’ during goal-setting? A qualitative study exploring patient perceptions, International Journal of Stroke, 10, 68, 2015 | Conference abstract. |
| Lapierre, Alexandra, Lefebvre, Helene, Gauvin-Lepage, Jerome, Factors Affecting Interprofessional Teamwork in Emergency Department Care of Polytrauma Patients: Results of an Exploratory Study, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 26, 312–322, 2019 [PubMed: 31714492] | Setting not in PICO: Emergency department. |
| Lee, Tracy, Norton, Andrea, Hayes, Sue, Adamson, Keith, Schwellnus, Heidi, Evans, Cathy, Exploring Parents’ Perceptions and How Physiotherapy Supports Transition from Rehabilitation to School for Youth with an ABI, Physical & occupational therapy in pediatrics, 37, 444–455, 2017 [PubMed: 28121255] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Lefebvre, Helene, Levert, Marie Josee, The needs experienced by individuals and their loved ones following a traumatic brain injury, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 19, 197–207, 2012 [PubMed: 23222398] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient and accessing rehabilitation services reviews. |
| Letts, L., Martin Ginis, K. A., Faulkner, G., Colquhoun, H., Levac, D., Gorczynski, P., Preferred Methods and Messengers for Delivering Physical Activity Information to People With Spinal Cord Injury: A Focus Group Study, Rehabilitation Psychology, 56, 128–137, 2011 [PubMed: 21574732] | It was unclear if the focus was specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Lexell, E. M., Alkhed, A. K., Olsson, K., The group rehabilitation helped me adjust to a new life: Experiences shared by persons with an acquired brain injury, Brain Injury, 27, 529–537, 2013 [PubMed: 23472828] | No qualitative data on phenomena of interest. |
| Lind, J. D., Fraser, M. A., Powell-Cope, G., Gavin-Dreschnack, D., Enhancing patient dignity in va spinal cord injury units, Journal of Spinal Cord Medicine, 36, 555, 2013 | Study not conducted in one of the countries included in the review protocol. |
| Lindahl, Marianne, Teljigovic, Sanel, Heegaard Jensen, Lars, Hvalsoe, Berit, Juneja, Hemant, Barth, Clay Cooper Cott Del Bano-Aledo Donabedian Donabedian Fitinghoff Griffiths Harris Hours Hush Jensen Kidd Lempp Lindahl Martins McLean Mead Mussener Partridge Pinto Polinder Rindflesch Sanders Strauss Walton Willamson, Importance of a patient-centred approach in ensuring quality of post-fracture rehabilitation for working aged people: A qualitative study of therapists’ and patients’ perspectives, Work: Journal of Prevention, Assessment & Rehabilitation, 55, 831–839, 2016 [PubMed: 28059811] | Mixed population, cannot separate or confirm which patients were hospitalised and match the population of interest. |
| Lindberg, J., Kreuter, M., Taft, C., Person, L. O., Patient participation in care and rehabilitation from the perspective of patients with spinal cord injury, Spinal Cord, 51, 834–7, 2013 [PubMed: 23999110] | Study did not examine phenomena of interest. |
| Linnarsson, J. R., Bubini, J., Perseius, K. I., A meta-synthesis of qualitative research into needs and experiences of significant others to critically ill or injured patients, Journal of Clinical Nursing, 19, 3102–11, 2010 [PubMed: 20738453] | Systematic review, included studies outside of date limits (1997-2007). |
| Littooij, E., Leget, C. J. W., Stolwijk-Swuste, J. M., Doodeman, S., Widdershoven, G. A. M., Dekker, J., The importance of ‘global meaning’ for people rehabilitating from spinal cord injury, Spinal Cord, 54, 1047–1052, 2016 [PubMed: 27089865] | Study did not examine phenomena of interest. |
| Lundine, J. P., Utz, M., Jacob, V., Ciccia, A. H., Putting the person in person-centered care: Stakeholder experiences in pediatric traumatic brain injury, Journal of Pediatric Rehabilitation Medicine, 12, 21–35, 2019 [PubMed: 30883376] | Study not conducted in one of the countries included in the review protocol. |
| Maddick, Rosie, Norton, Ali Amir Andrews Baker Batavia Batt-Rawden Bernstein Braun Bright Bright Bruscia De Carvalho Deegan Dijkers Dorsett Dorsett Dorsett Fook Fook Galvin Golden Humphries James Larsson Lee Lefevre Lethborg Manns Montague Nielson North O’Callaghan O’Callaghan O’Neil Riessman Riessman Scheiby Slivka Stover Tamplin Whittemore Zedjlik, ‘Naming the unnameable and communicating the unknowable’: Reflections on a combined music therapy/social work program, The Arts in Psychotherapy, 38, 130–137, 2011 | Study did not examine phenomena of interest. |
| Makela, P., Jones, F., de Sousa de Abreu, M. I., Hollinshead, L., Ling, J., Supporting self-management after traumatic brain injury: Codesign and evaluation of a new intervention across a trauma pathway, Health expectations : an international journal of public participation in health care and health policy, 22, 632–642, 2019 [PMC free article: PMC6737836] [PubMed: 31033115] | Study did not examine phenomena of interest. |
| Manning, Joseph C., Hemingway, Pippa, Redsell, Sarah A., Survived so what? Identifying priorities for research with children and families post-paediatric intensive care unit, Nursing in critical care, 23, 68–74, 2018 [PubMed: 28516470] | Study did not examine rehabilitation. |
| Martin, Laurie T., Farris, Coreen, Parker, Andrew M., Epley, Caroline, The Defense and Veterans Brain Injury Center Care Coordination Program: Assessment of Program Structure, Activities, and Implementation, Rand health quarterly, 3, 4, 2013 [PMC free article: PMC5051987] [PubMed: 28083300] | Study not conducted in one of the countries included in the review protocol. |
| Martin, Suzanne, Armstrong, Elaine, Thomson, Eileen, Vargiu, Eloisa, Sola, Marc, Dauwalder, Stefan, Miralles, Felip, Daly Lynn, Jean, A qualitative study adopting a user-centered approach to design and validate a brain computer interface for cognitive rehabilitation for people with brain injury, Assistive technology : the official journal of RESNA, 30, 233–241, 2018 [PubMed: 28708963] | Study did not examine phenomena of interest. |
| Materne, M., Lundqvist, L. O., Strandberg, T., Opportunities and barriers for successful return to work after acquired brain injury: A patient perspective, Work (Reading, Mass.), 56, 125–134, 2017 [PMC free article: PMC5302032] [PubMed: 28035941] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| McBain, Sacha A., Sexton, Kevin W., Palmer, Brooke E., Landes, Sara J., Barriers to and facilitators of a screening procedure for PTSD risk in a level I trauma center, Trauma surgery & acute care open, 4, e000345, 2019 [PMC free article: PMC6699788] [PubMed: 31467988] | Study not conducted in one of the countries included in the review protocol. |
| McDermott, Garret L., McDonnell, Anne Marie, Acquired brain injury services in the Republic of Ireland: experiences and perceptions of families and professionals, Brain Injury, 28, 81–91, 2014 [PubMed: 24328803] | The focus was not specific to care of people who have experienced traumatic injury and the results not presented separately for target population. |
| McGarry, Sarah, Elliott, Catherine, McDonald, Ann, Valentine, Jane, Wood, Fiona, Girdler, Sonya, “This is not just a little accident”: a qualitative understanding of paediatric burns from the perspective of parents, Disability and Rehabilitation, 37, 41–50, 2015 [PubMed: 24576308] | Study did not examine phenomena of interest. |
| McIntyre, Michelle, Ehrlich, Carolyn, Kendall, Elizabeth, Informal care management after traumatic brain injury: perspectives on informal carer workload and capacity, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30326760] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| McKelvey, M., Bush, E., Screening and identification of individuals with brain injury (BI) seeking services through the area agency on ageing in rural Nebraska, Brain Injury, 28, 712, 2014 | Conference abstract. |
| McPherson, K., Fadyl, J., Theadom, A., Channon, A., Levack, W., Starkey, N., Wilkinson-Meyers, L., Kayes, N., Feigin, V., Barker-Collo, S., Harwood, M., Mudge, S., Christie, G., Jenkins, S., Living Life after Traumatic Brain Injury: Phase 1 of a Longitudinal Qualitative Study, Journal of Head Trauma Rehabilitation, 33, E44–E52, 2018 [PubMed: 28520671] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences reviews. |
| McPherson, K., Theadom, A., Wilkinson-Meyers, L., The experience of recovery-a qualitative study, Brain Injury, 26, 493–494, 2012 | Conference abstract. |
| McRae, Philippa, Hallab, Lisa, Simpson, Grahame, Anstey, Braun Brooks Ellingsen Frost Gilworth Gilworth Gracey Harradine Kreutzer Macaden Medin Menon Nightingale Olver Oppermann Petrella Ponsford Rubenson Sabatello Simpson Tate Teasdale van Velzen van Velzen, Navigating employment pathways and supports following brain injury in Australia: Client perspectives, Australian Journal of Rehabilitation Counselling, 22, 76–92, 2016 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Meade, M., Carr, L., Ellenbogen, P., Barrett, K., Perceptions of provider education and attitude by individuals with spinal cord injury: Implications for health care disparities, Topics in Spinal Cord Injury Rehabilitation, 17, 25–37, 2011 | Study not conducted in one of the countries included in the review protocol. |
| Medina-Mirapeix, F., Del Bano-Aledo, M. E., Oliveira-Sousa, S. L., Escolar-Reina, P., Collins, S. M., How the rehabilitation environment influences patient perception of service quality: A qualitative study, Archives of Physical Medicine and Rehabilitation, 94, 1112–1117, 2013 [PubMed: 23154133] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Mehta, Swati, Hadjistavropoulos, Heather D., Earis, Danielle, Titov, Nick, Dear, Blake F., Patient perspectives of Internet-delivered cognitive behavior therapy for psychosocial issues post spinal cord injury, Rehabilitation Psychology, 2019 [PubMed: 30958020] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services review. |
| Meixner, Cara, O’Donoghue, Cynthia R., Witt, Michelle, Accessing crisis intervention services after brain injury: a mixed methods study, Rehabilitation psychology, 58, 377–85, 2013 [PubMed: 24128269] | Study not conducted in one of the countries included in the review protocol. |
| Messinger, Seth, Bozorghadad, Sayeh, Pasquina, Paul, Social relationships in rehabilitation and their impact on positive outcomes among amputees with lower limb loss at Walter Reed National Military Medical Center, Journal of rehabilitation medicine, 50, 86–93, 2018 [PubMed: 29206273] | Study not conducted in one of the countries included in the review protocol. |
| Milte, R., Ratcliffe, J., Miller, M., Whitehead, C., Cameron, I. D., Crotty, M., What are frail older people prepared to endure to achieve improved mobility following hip fracture? A Discrete Choice Experiment, Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine, 45, 81–86, 2013 [PubMed: 23037892] | Not a qualitative study. |
| Minney, M. J., Roberts, R. M., Mathias, J. L., Raftos, J., Kochar, A., Service and support needs following pediatric brain injury: perspectives of children with mild traumatic brain injury and their parents, Brain Injury, 33, 168–182, 2019 [PubMed: 30396278] | Study did not examine rehabilitation. |
| Mitchell, Rebecca, Fajardo Pulido, Diana, Ryder, Tayhla, Norton, Grace, Brodaty, Henry, Draper, Brian, Close, Jacqueline, Rapport, Frances, Lystad, Reidar, Harris, Ian, Harvey, Lara, Sherrington, Cathie, Cameron, Ian D., Braithwaite, Jeffrey, Access to rehabilitation services for older adults living with dementia or in a residential aged care facility following a hip fracture: healthcare professionals’ views, Disability and Rehabilitation, 1–12, 2019 [PubMed: 31335212] | Study did not examine phenomena of interest. |
| Mitsch, Virginia, Curtin, Michael, Badge, Helen, The provision of brain injury rehabilitation services for people living in rural and remote New South Wales, Australia, Brain Injury, 28, 1504–13, 2014 [PubMed: 25093407] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Moore, M., Robinson, G., Mink, R., Hudson, K., Dotolo, D., Gooding, T., Ramirez, A., Zatzick, D., Vavilala, M., Acute care after pediatric traumatic brain injury: A qualitative study of the family perspective, Journal of Neurotrauma, 31, A59, 2014 | Conference abstract. |
| Moore, Megan, Robinson, Gabrielle, Mink, Richard, Hudson, Kimberly, Dotolo, Danae, Gooding, Tracy, Ramirez, Alma, Zatzick, Douglas, Giordano, Jessica, Crawley, Deborah, Vavilala, Monica S., Developing a Family-Centered Care Model for Critical Care After Pediatric Traumatic Brain Injury, Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 16, 758–65, 2015 [PMC free article: PMC4592380] [PubMed: 26135064] | Study not conducted in one of the countries included in the review protocol. |
| Morriss, Elissa, Wright, Suzanne, Smith, Sharon, Roser, Judy, Kendall, Melissa, Ackerson, Ackerson Bassett Bassett Baulderstone Baxter Bisogni Butera-Prinzi Charles Cicerone Clark Cowling Craig Degeneffe Devany-Serio Evenson Flanagan Fletcher Gan Jacob Jones Kaatz Kirshbaum Kosciulek Lancaster Leinonen Lezak Llewellyn Maitz Nicholson Olson Pessar Qu Sander Smith Stake Strauss Urbach Uysal Visser-Meily Wade, Parenting challenges and needs for fathers following acquired brain injury (ABI) in Queensland, Australia: A preliminary model, Special Issue: Family support and adjustment following acquired brain injury: An international perspective., 19, 119–134, 2013 | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Mumbower, R., Heaton, K., Dreer, L., Novack, T., Childs, G., Vance, D., Sleep experiences following traumatic brain injury: A qualitative descriptive study, Archives of Physical Medicine and Rehabilitation, 98, e155, 2017 | Conference abstract. |
| Munce, Sarah E. P., Webster, Fiona, Fehlings, Michael G., Straus, Sharon E., Jang, Eunice, Jaglal, Susan B., Meaning of self-management from the perspective of individuals with traumatic spinal cord injury, their caregivers, and acute care and rehabilitation managers: an opportunity for improved care delivery, BMC Neurology, 16, 11, 2016 [PMC free article: PMC4724136] [PubMed: 26801243] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Munce, Sarah E. P., Webster, Fiona, Fehlings, Michael G., Straus, Sharon E., Jang, Eunice, Jaglal, Susan B., Perceived facilitators and barriers to self-management in individuals with traumatic spinal cord injury: a qualitative descriptive study, BMC Neurology, 14, 48, 2014 [PMC free article: PMC4007626] [PubMed: 24624961] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Murphy, Margaret, McCloughen, Andrea, Curtis, Kate, Using theories of behaviour change to transition multidisciplinary trauma team training from the training environment to clinical practice, Implementation science : IS, 14, 43, 2019 [PMC free article: PMC6489197] [PubMed: 31036023] | Study did not examine rehabilitation. |
| Murphy, Margaret, McCloughen, Andrea, Curtis, Kate, The impact of simulated multidisciplinary Trauma Team Training on team performance: A qualitative study, Australasian emergency care, 22, 1–7, 2019 [PubMed: 30998866] | Study did not examine rehabilitation. |
| Murray, A., Watter, K., Nielsen, M., Kennedy, A., A scoping study examining vocational rehabilitation in early acquired brain injury rehabilitation, Brain Impairment, 19, 306–307, 2018 | Conference abstract. |
| Nalder, E., Fleming, J., Cornwell, P., Foster, M., Identity and the life course: Lived experiences of individuals with traumatic brain injury during the period of transition from hospital to home, Brain Impairment, 14, 159, 2013 [PubMed: 23924357] | Conference abstract. |
| Nalder, E., Fleming, J., Cornwell, P., Foster, M., Worrall, L., Ownsworth, T., Haines, T., Kendall, M., Chenoweth, L., What constitutes transition success? An investigation into factors influencing the perceptions of individuals with a TBI regarding the transition from hospital to home, Brain Injury, 24 (3), 189–190, 2010 | Conference abstract. |
| Nalder, Emily J., Zabjek, Karl, Dawson, Deirdre R., Bottari, Carolina L., Gagnon, Isabelle, McFadyen, Bradford J., Hunt, Anne W., McKenna, Suzanne, Ouellet, Marie-Christine, Giroux, Sylvain, Cullen, Nora, Niechwiej-Szwedo, Ewa, Onf-Repar Abi Team, Research Priorities for Optimizing Long-term Community Integration after Brain Injury, The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques, 45, 643–651, 2018 [PubMed: 30430969] | Data was not collected using an appropriate qualitative methodology (the authors have analysed their own field notes taken at a 2-day conference for practitioners) |
| Nalder, Emily, Fleming, Jennifer, Cornwell, Petrea, Shields, Cassandra, Foster, Michele, Reflections on life: experiences of individuals with brain injury during the transition from hospital to home, Brain Injury, 27, 1294–303, 2013 [PubMed: 23924357] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Nasrabadi, A. N., Mohammadi, N., Davatgaran, K., Yekaninejad, M., Javidan, A. N., Shabany, M., Designing a client and family empowerment model to promote constructive life recovery among persons with spinal cord injury: A qualitative study, Archives of Neuroscience, 6, e87867, 2019 | Study not conducted in one of the countries included in the review protocol. |
| Nilsson, Charlotte, Bartfai, Aniko, Lofgren, Monika, Bartfai, Ben-Yishai Brooks Carlsson Charmaz Christensen Cicerone Cicerone Cicerone Comper Creswell Cullen Dahlgren Ferguson Fleming Gard Ho Kielhofner Lincoln Miller Ohman Phipps Ponsford Prigatano Rice-Oxley Roding Roxendahl Rudolfsson Ruff Stalnacke Svendsen Tiersky Wilson, Holistic group rehabilitation-A short cut to adaptation to the new life after mild acquired brain injury, Disability and Rehabilitation: An International, Multidisciplinary Journal, 33, 969–978, 2011 [PubMed: 21067340] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Norrbrink, Cecilia, Lofgren, Monika, Needs and requests--patients and physicians voices about improving the management of spinal cord injury neuropathic pain, Disability and Rehabilitation, 38, 151–8, 2016 [PubMed: 25918963] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient and support needs and preferences reviews. |
| Nunnerley, J. L., Hay-Smith, E. J., Dean, S. G., Leaving a spinal unit and returning to the wider community: an interpretative phenomenological analysis, Disability and Rehabilitation, 35, 1164–1173, 2013 [PubMed: 23035858] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| O’Callaghan, A., McNamara, B., Cocks, E., ‘What am I supposed to do? Cartwheels down the passageway?’ Perspectives on the rehabilitation journey from people with ABI, Brain Injury, 28, 577–578, 2014 | Conference abstract. |
| O’Callaghan, Anna, McAllister, Lindy, Wilson, Linda, Blight, Brookshire Brown Cicerone Denzin Fleming Foster Gentleman Goranson Grbich Hickson Hughes Humphreys Humphreys Josselson Katz Keleher LeFebvre Mackay MacPhail Malec McNaughton Minichiello Morse Morton Muus O’Callaghan O’Callaghan O’Callaghan O’Callaghan Penchansky Rankin Sandelowski Schmidt Schwandt Seale Sherer Stringer Tuel Turner-Stokes Youse, Healthcare consumers’ need for brain-injury services: The critical importance of timing in planning future services, Brain Impairment, 13, 316–332, 2012 | Analysis methods not appropriate (data reduced into case vignettes) |
| Ogilvie, Rebekah, Foster, Kim, McCloughen, Andrea, Curtis, Kate, The injury trajectory for young people 16-24 years in the six months following injury: A mixed methods study, Injury, 47, 1966–74, 2016 [PubMed: 27282687] | Study did not examine phenomena of interest. |
| Ogilvie, Rebekah, Foster, Kim, McCloughen, Andrea, Curtis, Kate, Young peoples’ experience and self-management in the six months following major injury: A qualitative study, Injury, 46, 1841–7, 2015 [PubMed: 26036963] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Oster, Caisa, Kildal, Morten, Ekselius, Lisa, Return to work after burn injury: burn-injured individuals’ perception of barriers and facilitators, Journal of burn care & research : official publication of the American Burn Association, 31, 540–50, 2010 [PubMed: 20616648] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Oyesanya, Tolu O., Bowers, Barbara J., Royer, Heather R., Turkstra, Lyn S., Nurses’ concerns about caring for patients with acute and chronic traumatic brain injury, Journal of Clinical Nursing, 27, 1408–1419, 2018 [PMC free article: PMC5918200] [PubMed: 29399908] | Study not conducted in one of the countries included in the review protocol. |
| Palimaru, Alina, Cunningham, William E., Dillistone, Marcus, Vargas-Bustamante, Arturo, Liu, Honghu, Hays, Ron D., A comparison of perceptions of quality of life among adults with spinal cord injury in the United States versus the United Kingdom, Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation, 26, 3143–3155, 2017 [PubMed: 28712004] | Study did not examine phenomena of interest. |
| Pallesen, H., Buhl, I., Interdisciplinary facilitation of the minimal participation of patients with severe brain injury in early rehabilitation, European Journal of Physiotherapy, 19, 13–23, 2017 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Patterson, F., Fleming, J., Doig, E., Patient experiences of occupational therapy groups in traumatic brain injury rehabilitation, Brain Impairment, 19, 281, 2018 | Conference abstract. |
| Patton, Desmond, Sodhi, Aparna, Affinati, Steven, Lee, Jooyoung, Crandall, Marie, Post-Discharge Needs of Victims of Gun Violence in Chicago: A Qualitative Study, Journal of interpersonal violence, 34, 135–155, 2019 [PubMed: 27638688] | Study not conducted in one of the countries included in the review protocol. |
| Pekmezaris, Renee, Kozikowski, Andrzej, Pascarelli, Briana, Handrakis, John P., Chory, Ashley, Griffin, Doug, Bloom, Ona, Participant-reported priorities and preferences for developing a home-based physical activity telemonitoring program for persons with tetraplegia: a qualitative analysis, Spinal cord series and cases, 5, 48, 2019 [PMC free article: PMC6786286] [PubMed: 31666989] | Study not conducted in one of the countries included in the review protocol. |
| Phillips, J., Holmes, J., Auton, M., Radford, K., What are the most important outcomes of traumatic brain injury vocational rehabilitation? People with TBI, service provider and employer perspectives, Brain Injury, 30, 494–495, 2016 | Conference abstract. |
| Piccenna, Loretta, Lannin, Natasha A., Gruen, Russell, Pattuwage, Loyal, Bragge, Peter, The experience of discharge for patients with an acquired brain injury from the inpatient to the community setting: A qualitative review, Brain Injury, 30, 241–51, 2016 [PubMed: 26890803] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Plant, Sarah E., Tyson, Sarah F., Kirk, Susan, Parsons, John, What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis, Clinical rehabilitation, 30, 921–30, 2016 [PMC free article: PMC4978164] [PubMed: 27496701] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Pol, M., Peek, S., Van Nes, F., Van Hartingsveldt, M., Buurman, B., Krose, B., Everyday life after a hip fracture: What community-living older adults perceive as most beneficial for their recovery, Age and Ageing, 48, 440–447, 2019 [PMC free article: PMC6503934] [PubMed: 30806451] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences review. |
| Poncet, F., Pradat-Diehl, P., Lamontagne, M. E., Alifax, A., Barette, M., Fradelizi, P., Swaine, B., A mixed-methods approach to evaluate participants’ and service providers’ perceptions of an outpatient rehabilitation programme for persons with acquired brain injury, Brain Injury, 31, 816, 2017 [PubMed: 28716537] | Conference abstract. |
| Poncet, F., Pradat-Diehl, P., Lamontagne, M. E., Alifax, A., Fradelizi, P., Barette, M., Swaine, B., Participant and service provider perceptions of an outpatient rehabilitation program for people with acquired brain injury, Annals of Physical and Rehabilitation Medicine, 60, 334–340, 2017 [PubMed: 28716537] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Popejoy, Lori L., Dorman Marek, Karen, Scott-Cawiezell, Jill, Patterns and problems associated with transitions after hip fracture in older adults, Journal of gerontological nursing, 39, 43–52, 2013 [PubMed: 23799788] | Study not conducted in one of the countries included in the review protocol. |
| Porto, A., Anderson, L., Vogel, L., Zebracki, K., Barriers in accessing adult healthcare for transitioning youth with spinal cord injury, Developmental Medicine and Child Neurology, 60, 116, 2018 | Conference abstract. |
| Poulin, V., Lamontagne, M. E., Ouellet, M. C., Pellerin, M. A., Jean, A., Implementing best practices in cognitive rehabilitation: What are rehabilitation teams’ priorities and why?, Archives of Physical Medicine and Rehabilitation, 98, e157, 2017 | Conference abstract. |
| Prescott, Sarah, Fleming, Jennifer, Doig, Emmah, Refining a clinical practice framework to engage clients with brain injury in goal setting, Australian Occupational Therapy Journal, 66, 313–325, 2019 [PubMed: 30699467] | Study did not examine phenomena of interest. |
| Ramakrishnan, Kumaran, Johnston, Deborah, Garth, Belinda, Murphy, Gregory, Middleton, James, Cameron, Ian, Early Access to Vocational Rehabilitation for Inpatients with Spinal Cord Injury: A Qualitative Study of Patients’ Perceptions, Topics in Spinal Cord Injury Rehabilitation, 22, 183–191, 2016 [PMC free article: PMC4981013] [PubMed: 29339860] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Rashid, M., Caine, V., Newton, A. S., Goez, H. R., Healthcare professionals’ perspective on the delivery of care to children with Acquired Brain Injury (ABI) and communication with their parents, Journal of Pediatric Rehabilitation Medicine, 11, 125–131, 2018 [PubMed: 30010150] | Population is under 18s. Included in corresponding paediatric review. |
| Roberts, J. L., Pritchard, A. W., Williams, M., Totton, N., Morrison, V., D. In N.U, Williams, N. H., Mixed methods process evaluation of an enhanced community-based rehabilitation intervention for elderly patients with hip fracture, BMJ Open, 8 (8) (no pagination), 2018 [PMC free article: PMC6089270] [PubMed: 30093516] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Roberts, Jessica Louise, Din, Nafees Ud, Williams, Michelle, Hawkes, Claire A., Charles, Joanna M., Hoare, Zoe, Morrison, Val, Alexander, Swapna, Lemmey, Andrew, Sackley, Catherine, Logan, Phillipa, Wilkinson, Clare, Rycroft-Malone, Jo, Williams, Nefyn H., Development of an evidence-based complex intervention for community rehabilitation of patients with hip fracture using realist review, survey and focus groups, BMJ Open, 7, e014362, 2017 [PMC free article: PMC5652569] [PubMed: 29025824] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences review. |
| Rongen, A., Bakx, W., Nijhuis, F., Follow-up study of patients with an acquired Brain Injury after early focus on return to work during post-acute rehabilitation, Brain Injury, 24, 450–451, 2010 | Conference abstract. |
| Roscigno, Cecelia I., Parent Perceptions of How Nurse Encounters Can Provide Caring Support for the Family in Early Acute Care After Children’s Severe Traumatic Brain Injury, Journal of Neuroscience Nursing, 48, E2–E15, 2016 [PMC free article: PMC4862592] [PubMed: 26871242] | Study not conducted in one of the countries included in the review protocol. |
| Roth, Karin, Mueller, Gabi, Wyss, Adrian, Experiences of peer counselling during inpatient rehabilitation of patients with spinal cord injuries, Spinal cord series and cases, 5, 1, 2019 [PMC free article: PMC6333824] [PubMed: 30675385] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Rothlisberger, Fabian, Boes, Stefan, Rubinelli, Sara, Schmitt, Klaus, Scheel-Sailer, Anke, Challenges and potential improvements in the admission process of patients with spinal cord injury in a specialized rehabilitation clinic - an interview based qualitative study of an interdisciplinary team, BMC health services research, 17, 443, 2017 [PMC free article: PMC5485498] [PubMed: 28651583] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Ryerson Espino, S., Kelly, E., Riordan, A., Zebracki, K., Vogel, L., Personal and family experiences of caregivers of children with SCI, Developmental Medicine and Child Neurology, 58, 107–108, 2016 | Conference abstract. |
| Ryerson Espino, Susan L., Kelly, Erin H., Rivelli, Anne, Zebracki, Kathy, Vogel, Lawrence C., It is a marathon rather than a sprint: an initial exploration of unmet needs and support preferences of caregivers of children with SCI, Spinal Cord, 56, 284–294, 2018 [PubMed: 29187744] | Study not conducted in one of the countries included in the review protocol. |
| Sale, J. E. M., Bogoch, E., Hawker, G., Gignac, M., Beaton, D., Jaglal, S., Frankel, L., Patient perceptions of provider barriers to post-fracture secondary prevention, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 25, 2581–9, 2014 [PubMed: 25082555] | No qualitative data on phenomena of interest. |
| Salsbury, Stacie A., Vining, Robert D., Gosselin, Donna, Goertz, Christine M., Be good, communicate, and collaborate: a qualitative analysis of stakeholder perspectives on adding a chiropractor to the multidisciplinary rehabilitation team, Chiropractic & manual therapies, 26, 29, 2018 [PMC free article: PMC6014012] [PubMed: 29977521] | Study not conducted in one of the countries included in the review protocol. |
| Samoborec, Stella, Ayton, Darshini, Ruseckaite, Rasa, Winbolt, Gary, Evans, Sue M., System complexities affecting recovery after a minor transport-related injury: The need for a person-centred approach, Journal of Rehabilitation Medicine, 51, 120–126, 2019 [PubMed: 30426136] | Population described as people that sustained predominantly minor injuries; study does not report any results separately for target population. |
| Sandstrom, Linda, Engstrom, Asa, Nilsson, Carina, Juuso, Paivi, Experiences of suffering multiple trauma: A qualitative study, Intensive & critical care nursing, 2019 [PubMed: 31351691] | Setting not in PICO: Intensive care unit |
| Sashika, Hironobu, Takada, Kaoruko, Kikuchi, Naohisa, Rehabilitation needs and participation restriction in patients with cognitive disorder in the chronic phase of traumatic brain injury, Medicine, 96, e5968, 2017 [PMC free article: PMC5287971] [PubMed: 28121947] | Study not conducted in one of the countries included in the review protocol. |
| Schiller, Claire, Franke, Thea, Belle, Jessica, Sims-Gould, Joanie, Sale, Joanna, Ashe, Maureen C., Words of wisdom - patient perspectives to guide recovery for older adults after hip fracture: a qualitative study, Patient preference and adherence, 9, 57–64, 2015 [PMC free article: PMC4298293] [PubMed: 25609927] | Study did not examine rehabilitation. |
| Segevall, Cecilia, Soderberg, Siv, Bjorkman Randstrom, Kerstin, The Journey Toward Taking the Day for Granted Again: The Experiences of Rural Older People’s Recovery From Hip Fracture Surgery, Orthopedic nursing, 38, 359–366, 2019 [PubMed: 31764899] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Self, Megan, Driver, Simon, Stevens, Laurel, Warren, Ann Marie, Physical activity experiences of individuals living with a traumatic brain injury: a qualitative research exploration, Adapted physical activity quarterly : APAQ, 30, 20–39, 2013 [PubMed: 23283024] | Study not conducted in one of the countries included in the review protocol. |
| Sena Martins, Bruno, Fontes, Fernando, Hespanha, Pedro, Barnes, Barnes Davis Fontes Fontes Goffman Guion Hahn Henriques Hughes Klein Leder Martins Martins Oliver Oliver Oliver Santos Somers Stiker Stone Turner Wall, Spinal cord injury in Portugal: Institutional and personal challenges, Journal of Disability Policy Studies, 28, 119–128, 2017 | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Sharp, K., Richards, S., Client’s perspectives of smartphone technology in acquired brain injury rehabilitation, Brain Impairment, 14, 167, 2013 | Conference abstract. |
| Silver, Jeremy, Ljungberg, Inger, Libin, Alexander, Groah, Suzanne, Barriers for individuals with spinal cord injury returning to the community: a preliminary classification, Disability and Health Journal, 5, 190–6, 2012 [PubMed: 22726860] | Study not conducted in one of the countries included in the review protocol. |
| Silver, Samuel A., Saragosa, Marianne, Adhikari, Neill K., Bell, Chaim M., Harel, Ziv, Harvey, Andrea, Kitchlu, Abhijat, Neyra, Javier A., Wald, Ron, Jeffs, Lianne, What insights do patients and caregivers have on acute kidney injury and posthospitalisation care? A single-centre qualitative study from Toronto, Canada, BMJ Open, 8, e021418, 2018 [PMC free article: PMC6009618] [PubMed: 29909373] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Singh, Gurkaran, MacGillivray, Megan, Mills, Patricia, Adams, Jared, Sawatzky, Bonita, Mortenson, W. Ben, Patients’ Perspectives on the Usability of a Mobile App for Self-Management following Spinal Cord Injury, Journal of Medical Systems, 44, 26, 2019 [PubMed: 31828440] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in accessing rehabilitation services and support needs and preferences reviews. |
| Slomic, M., Christiansen, B., Sveen, U., Soberg, H. L., Users’ experiential knowledge as a base for evidence-based practice in inter-professional rehabilitation, Brain Injury, 30, 580–581, 2016 | Conference abstract. |
| Slomic, Mirela, Christiansen, Bjorg, Soberg, Helene L., Sveen, Unni, User involvement and experiential knowledge in interprofessional rehabilitation: a grounded theory study, BMC health services research, 16, 547, 2016 [PMC free article: PMC5051024] [PubMed: 27716269] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Smith, Bridget M., Martinez, Rachael N., Evans, Charlesnika T., Saban, Karen L., Balbale, Salva, Proescher, Eric J., Stroupe, Kevin, Hogan, Timothy P., Barriers and strategies for coordinating care among veterans with traumatic brain injury: a mixed methods study of VA polytrauma care team members, Brain Injury, 32, 755–762, 2018 [PubMed: 29537883] | Study not conducted in one of the countries included in the review protocol. |
| Smith, E. M., Boucher, N., Miller, W. C., Caregiving services in spinal cord injury: A systematic review of the literature, Spinal Cord, 54, 562–569, 2016 [PubMed: 26902459] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Smith, M., Hada, E., Long, C., Bushnik, T., Examining language preference and acculturation and implications for the continuum of care of patients with traumatic brain injury (TBI), Journal of Head Trauma Rehabilitation, 30, E107, 2015 | Conference abstract. |
| Snell, Deborah L., Martin, Rachelle, Surgenor, Lois J., Siegert, Richard J., Hay-Smith, E. Jean C., What’s wrong with me? seeking a coherent understanding of recovery after mild traumatic brain injury, Disability and Rehabilitation, 39, 1968–1975, 2017 [PubMed: 27626509] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Soong, Christine, Kurabi, Bochra, Exconde, Kathleen, Tajammal, Faiqa, Bell, Chaim M., Design of an orthopaedic-specific discharge summary, BMC Health Services Research, 16, 545, 2016 [PMC free article: PMC5050605] [PubMed: 27716194] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Sorli, H., Bach, B., Haarberg, D., Hjort-Larsen, G., Anette Hansen, S., Kristiansen, G., Hansen, H., Telerehabilitation in Norway, Brain Injury, 24, 284–285, 2010 | Conference abstract. |
| Speck, Rebecca M., Jones, Gabrielle, Barg, Frances K., McCunn, Maureen, Team composition and perceived roles of team members in the trauma bay, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 19, 133–8, 2012 [PubMed: 22955707] | Study not conducted in one of the countries included in the review protocol. |
| Starnes, C. L., Bailey, E. A., Calvert, C. T., Gusler, J., Cairns, B. A., Development of a pediatric educational tool: Helping burns heal-an adventure for kids with burns, Journal of Burn Care and Research, 37, S172, 2016 | Conference abstract. |
| Stergiou-Kita, M., Bottari, C., Dawson, D., Hebert, D., Grigorovich, A., Inter-professional approaches to vocational evaluation following traumatic brain injury, Brain Injury, 28, 774–775, 2014 | Conference abstract. |
| Stott-Eveneshen, Sarah, Sims-Gould, Joanie, McAllister, Megan M., Fleig, Lena, Hanson, Heather M., Cook, Wendy L., Ashe, Maureen C., Reflections on Hip Fracture Recovery From Older Adults Enrolled in a Clinical Trial, Gerontology & geriatric medicine, 3, 2333721417697663, 2017 [PMC free article: PMC5433673] [PubMed: 28540341] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Strandberg, T., Materne, M., Returning to working life after acquired brain injury-The rehabilitation-process, possibilities and hindrance for participation, Brain Injury, 28, 754, 2014 | Conference abstract. |
| Sullivan, Martin, Paul, Charlotte E., Herbison, G. Peter, Tamou, Peina, Derrett, Sarah, Crawford, Maureen, A longitudinal study of the life histories of people with spinal cord injury, Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention, 16, e3, 2010 [PubMed: 20876766] | A study protocol only. No data presented. |
| Sveen, Unni, Ostensjo, Sigrid, Laxe, Sara, Soberg, Helene L., Problems in functioning after a mild traumatic brain injury within the ICF framework: the patient perspective using focus groups, Disability and Rehabilitation, 35, 749–57, 2013 [PubMed: 22897238] | No qualitative data on phenomena of interest. |
| Swaine, B., Cullen, N., Bayley, M., Lavoie, A., Marshall, S., Turgeon, A., Sirois, M. J., Messier, F., Trempe, C., Who goes where and why? An environmental scan of rehab referral, admission and discharge of persons with brain injury in two canadian provinces, Brain Injury, 24, 362, 2010 | Conference abstract. |
| Takada, Kaoruko, Sashika, Hironobu, Wakabayashi, Hidetaka, Hirayasu, Yoshio, Social participation and quality-of-life of patients with traumatic brain injury living in the community: A mixed methods study, Brain Injury, 30, 1590–1598, 2016 [PubMed: 27630033] | Study not conducted in one of the countries included in the review protocol. |
| Talbot, Lise R., Levesque, Annie, Trottier, Josee, Process of implementing collaborative care and its impacts on the provision of care and rehabilitation services to patients with a moderate or severe traumatic brain injury, Journal of multidisciplinary healthcare, 7, 313–20, 2014 [PMC free article: PMC4122558] [PubMed: 25114538] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Thrussell, Helen, Coggrave, Maureen, Graham, Allison, Gall, Angela, Donald, Michelle, Kulshrestha, Richa, Geddis, Tracey, Women’s experiences of sexuality after spinal cord injury: a UK perspective, Spinal Cord, 56, 1084–1094, 2018 [PubMed: 30140048] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Todis, Bonnie, McCart, Melissa, Glang, Ann, Hospital to school transition following traumatic brain injury: A qualitative longitudinal study, NeuroRehabilitation, 42, 269–276, 2018 [PubMed: 29660964] | Study not conducted in one of the countries included in the review protocol. |
| Torjussen, I., In sickness and in health? The effect of ABI on couples’ relationships, Brain Impairment, 13, 160–161, 2012 | Conference abstract. |
| Toscan, Justine, Manderson, Brooke, Santi, Selena M., Stolee, Paul, “Just another fish in the pond”: the transitional care experience of a hip fracture patient, International journal of integrated care, 13, e023, 2013 [PMC free article: PMC3718274] [PubMed: 23882170] | Case report. |
| Turner, B., Fleming, J., Ownsworth, T., Cornwell, P., From hospital to home: A new conceptual framework for transition-based service delivery following acquired brain injury, Neurorehabilitation and Neural Repair, 26, 686, 2012 | Conference abstract. |
| Turner, Benjamin, Fleming, Jennifer, Ownsworth, Tamara, Cornwell, Petrea, Perceptions of recovery during the early transition phase from hospital to home following acquired brain injury: a journey of discovery, Neuropsychological rehabilitation, 21, 64–91, 2011 [PubMed: 21132603] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Turner, Benjamin James, Fleming, Jennifer, Ownsworth, Tamara, Cornwell, Petrea, Perceived service and support needs during transition from hospital to home following acquired brain injury, Disability and Rehabilitation, 33, 818–29, 2011 [PubMed: 20812814] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Tverdal, Cathrine Buaas, Howe, Emilie Isager, Roe, Cecilie, Helseth, Eirik, Lu, Juan, Tenovuo, Olli, Andelic, Nada, Traumatic brain injury: Patient experience and satisfaction with discharge from trauma hospital, Journal of Rehabilitation Medicine, 50, 505–513, 2018 [PubMed: 29620136] | Not a qualitative study. |
| Tyerman, Emma, Eccles, Fiona J. R., Gray, Victoria, The experiences of parenting a child with an acquired brain injury: A meta-synthesis of the qualitative literature, Brain Injury, 31, 1553–1563, 2017 [PubMed: 28750173] | Study did not examine rehabilitation. |
| Tyerman, Emma, Eccles, Fiona J. R., Gray, Victoria, Murray, Craig D., Siblings’ experiences of their relationship with a brother or sister with a pediatric acquired brain injury, Disability and Rehabilitation, 41, 2940–2948, 2019 [PubMed: 29987955] | The majority of participants’ siblings had not experienced traumatic injury and results not presented separately for target population. |
| Umeasiegbu, Veronica I., Waletich, Brittany, Whitten, Laura A., Bishop, Malachy, Abreu, Bartlett Berg Bishop Corrigan Cott Creswell Degeneffe Degeneffe deGuise Elbogen Gontkovsky Heinemann Jennekens Kreutzer Lefebvre Lehan Man Murphy O’Callaghan O’Callaghan Pickelsimer Ponsford Rotondi Sinnakaruppan Spearman Turner Vaughn, Community-based rehabilitation needs: Perceptions of individuals with brain injury and their families in the Midwestern United States, Special Issue: Family support and adjustment following acquired brain injury: An international perspective., 19, 155–163, 2013 | Study not conducted in one of the countries included in the review protocol. |
| Unger, Janelle, Singh, Hardeep, Mansfield, Avril, Hitzig, Sander L., Lenton, Erica, Musselman, Kristin E., The experiences of physical rehabilitation in individuals with spinal cord injuries: a qualitative thematic synthesis, Disability and Rehabilitation, 41, 1367–1383, 2019 [PubMed: 29334811] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Valizadeh, Sousan, Dadkhah, Behrouz, Mohammadi, Eissa, Hassankhani, Hadi, The perception of trauma patients from social support in adjustment to lower-limb amputation: a qualitative study, Indian journal of palliative care, 20, 229–38, 2014 [PMC free article: PMC4154173] [PubMed: 25191013] | Study not conducted in one of the countries included in the review protocol. |
| Van de Velde, Dominique, Bracke, Piet, Van Hove, Geert, Josephsson, Staffan, Devisch, Ignaas, Vanderstraeten, Guy, The illusion and the paradox of being autonomous, experiences from persons with spinal cord injury in their transition period from hospital to home, Disability and Rehabilitation, 34, 491–502, 2012 [PubMed: 21978173] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Van de Veldea, Dominique, Bracke, Piet, Van Hove, Geert, Josephsson, Staffan, Vanderstraeten, Guy, Perceived participation, experiences from persons with spinal cord injury in their transition period from hospital to home, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 33, 346–55, 2010 [PubMed: 20679902] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Vassallo, G., Robinson, G., Fraser, C., Fallon, D., Kirk, S., A qualitative study to investigate families’ information and support needs following severe traumatic brain injury in childhood, Developmental Medicine and Child Neurology, 1), 34, 2014 | Conference abstract. |
| Wade, S. L., Moscato, E. L., Raj, S. P., Narad, M. E., Clinician perspectives delivering telehealth interventions to children/families impacted by pediatric traumatic brain injury, Rehabilitation Psychology, 64, 298–306, 2019 [PubMed: 30816734] | Study not conducted in one of the countries included in the review protocol. |
| Waring, Justin, Marshall, Fiona, Bishop, Simon, Understanding the occupational and organizational boundaries to safe hospital discharge, Journal of health services research & policy, 20, 35–44, 2015 [PubMed: 25472988] | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Weatherhead, S., Calvert, P., Newby, G., Three models of group therapy in community brain injury rehabilitation, Brain Injury, 26, 430–431, 2012 | Conference abstract. |
| Weir, N., Prescott, S., Fleming, J., Doig, E., Exploration of structured communication during client-centred goal setting with people with acquired brain injury, Brain Impairment, 19, 347–348, 2018 | Conference abstract. |
| Wharewera-Mika, Julie, Cooper, Erana, Kool, Bridget, Pereira, Susana, Kelly, Patrick, Caregivers’ voices: The experiences of caregivers of children who sustained serious accidental and non-accidental head injury in early childhood, Clinical child psychology and psychiatry, 21, 268–86, 2016 [PubMed: 26088208] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in support needs and preferences review. |
| Wheatley, Alison, Bamford, Claire, Shaw, Caroline, Flynn, Elizabeth, Smith, Amy, Beyer, Fiona, Fox, Chris, Barber, Robert, Parry, Steve W., Howel, Denise, Homer, Tara, Robinson, Louise, Allan, Louise M., Developing an Intervention for Fall-Related Injuries in Dementia (DIFRID): an integrated, mixed-methods approach, BMC Geriatrics, 19, 57, 2019 [PMC free article: PMC6394022] [PubMed: 30819097] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Whiteneck, G., Gassaway, J., Dijkers, M., Balance of spinal cord injury rehabilitation services provided in inpatient and postdischarge settings, Archives of Physical Medicine and Rehabilitation, 91, e19, 2010 [PubMed: 21353820] | Conference abstract. |
| Whiteneck, G., Gassaway, J., Dijkers, M., Lammertse, D., Hammond, F., Heinemann, A., Backus, D., Charlifue, S., Ballard, P., Zanca, J., Inpatient and post-discharge rehabilitation services provided in the first year after spinal cord injury: Findings from the SCI rehab study, Topics in Spinal Cord Injury Rehabilitation, 16, 28–29, 2011 [PubMed: 21353820] | Conference abstract. |
| Whiteneck, Gale G., Gassaway, Julie, Dijkers, Marcel P., Lammertse, Daniel P., Hammond, Flora, Heinemann, Allen W., Backus, Deborah, Charlifue, Susan, Ballard, Pamela H., Zanca, Jeanne M., Inpatient and postdischarge rehabilitation services provided in the first year after spinal cord injury: findings from the SCIRehab Study, Archives of Physical Medicine and Rehabilitation, 92, 361–8, 2011 [PubMed: 21353820] | Study not conducted in one of the countries included in the review protocol. |
| Wilbanks, Susan R., Ivankova, Nataliya V., Exploring factors facilitating adults with spinal cord injury rejoining the workforce: a pilot study, Disability and Rehabilitation, 37, 739–49, 2015 [PubMed: 25003483] | Study not conducted in one of the countries included in the review protocol. |
| Williams, L. M., Douglas, J. M., It takes 2 to tango: The therapeutic alliance in community brain injury rehabilitation, Brain Impairment, 18, 362, 2017 | Conference abstract. |
| Wong, A., Papadimitriou, C., Whiteneck, G., Deutsch, A., Heinemann, A., Goldsmith, A., Christopher, K., Focht, C., Lenze, E., Patient engagement in spinal cord injury rehabilitation: Patient and provider perspectives, Archives of Physical Medicine and Rehabilitation, 97, e71, 2016 | Conference abstract. |
| Wright, Courtney J., Zeeman, Heidi, Biezaitis, Valda, Holistic Practice in Traumatic Brain Injury Rehabilitation: Perspectives of Health Practitioners, PLoS ONE, 11, e0156826, 2016 [PMC free article: PMC4894634] [PubMed: 27270604] | No themes examining coordination of rehabilitation and social care while transferring between inpatient and outpatient services. Included in coordination while inpatient review. |
| Yenikomshian, Haig A., Lerew, Tara L., Tam, Melvin, Mandell, Sam P., Honari, Shari E., Pham, Tam N., Evaluation of Burn Rounds Using Telemedicine: Perspectives from Patients, Families, and Burn Center Staff, Telemedicine journal and e-health : the official journal of the American Telemedicine Association, 25, 25–30, 2019 [PubMed: 29733269] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Yoshida, Karen K., Self, Hazel M., Renwick, Rebecca M., Forma, Laura L., King, Audrey J., Fell, Leslie A., A value-based practice model of rehabilitation: consumers’ recommendations in action, Disability and Rehabilitation, 37, 1825–33, 2015 [PubMed: 25427892] | No qualitative data on phenomena of interest. |
Economic studies
Table 41Excluded economic studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Bandyopadhyay, S., Wilkinson, I., Giokarinin-Royal, T., How incorporating ‘lean’ approach led to improved delivery of care and reduction in length of hospital stay, Age and Ageing, 48, 2019 | Conference abstract. |
| Bhowaneedin, A., Smith, H., Deeley, H., Reyes Payeras, C., Keating, O., Smallbone, T., Wright, I., Sharples, P. M., What evidence is available to support the development of a regional specialist neurorehabilitation outreach service, Archives of Disease in Childhood, 104, A26–A27, 2019 | Conference abstract. |
| Cheung, W. H., Shen, W. Y., Dai, D. L. K., Lee, K. B., Zhu, T. Y., Wong, R. M. Y., Leung, K. S., Evaluation of a multidisciplinary rehabilitation programme for elderly patients with hip fracture: A prospective cohort study, Journal of Rehabilitation Medicine, 50, 285–291, 2018 [PubMed: 29260234] | Intervention not in PICO: Intervention group included geriatrician care in an acute hospital and a multidisciplinary rehabilitation programme after discharge from the convalescence hospital (rehabilitation service coordination was not in an inpatient setting). |
| Closa, Conxita, Mas, Miquel A., Santaeugenia, Sebastia J., Inzitari, Marco, Ribera, Aida, Gallofre, Miquel, Hospital-at-home Integrated Care Program for Older Patients With Orthopedic Processes: An Efficient Alternative to Usual Hospital-Based Care, Journal of the American Medical Directors Association, 18, 780–784, 2017 [PubMed: 28578883] | Comparison not in PICO: Control group are in-patients and the experimental group are out-patients. |
| Collins, Nina, Miller, Richard, Kapu, April, Martin, Rita, Morton, Melissa, Forrester, Mary, Atkinson, Shelley, Evans, Bethany, Wilkinson, Linda, Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction, The journal of trauma and acute care surgery, 76, 353–7, 2014 [PubMed: 24398767] | Intervention not in PICO: Acute care nurse practitioner (ACPN) who coordinated acute/ clinical care; only mention of “rehabilitation” was “The ACNP attended the daily discharge huddle, a team meeting that encompasses T2 [step-down care from ICU] and T3 [trauma nurse practitioner satellite service] NPs [nurse practitioner], case managers, social worker, liaisons to rehabilitation and nursing home facilities, and home health agency staff to facilitate communication and the discharge process.” Only outcome reported is length of stay. |
| Cooper, M., Ganda, K., Palmer, A., Seibel, M. J., Cost effectiveness of a targeted intervention to reduce refracture rates: Analysis of a four year prospective controlled study, Journal of Bone and Mineral Research, 26, 2011 | Conference abstract. |
| Farquhar, M., Lannin, N. A., Morarty, J., Functional outcomes from a specialised acquired brain injury community rehabilitation service - Evaluating a new model of care, Brain Impairment, 18, 344, 2017 | Conference abstract. |
| Fukuda, Haruhisa, Shimizu, Sayuri, Ishizaki, Tatsuro, Has the Reform of the Japanese Healthcare Provision System Improved the Value in Healthcare? A Cost-Consequence Analysis of Organized Care for Hip Fracture Patients, PLoS ONE, 10, e0133694, 2015 [PMC free article: PMC4514762] [PubMed: 26208322] | Comparison not in PICO: Hip fracture care in hospitals autonomously providing integrated care across specialties versus in acute care hospitals and rehabilitative care hospitals providing organized care across separate facilities (the organisation of the care not further described). |
| Kapu, A., Jones, P., Financial impact of adding acute care nurse practitioners (ACNPs) to inpatient models of care, Critical Care Medicine, 40, 27, 2012 | Conference abstract. |
| Leung, C. K., Mok, H. W., Shen, W. Y., Cheung, W. H., Leung, K. S., Evaluation of cost-effectiveness of a multidisciplinary hip fracture management program in Hong Kong, Osteoporosis International, 24, S597–S598, 2013 | Conference abstract. |
| Ling, Shi-Neng James, Kleimeyer, Christopher, Lynch, Genni, Burmeister, Elizabeth, Kennedy, Diana, Bell, Kate, Watkins, Leith, Cooke, Cameron, Can geriatric hip fractures be managed effectively within a level 1 trauma center?, Journal of Orthopaedic Trauma, 29, 160–4, 2015 [PubMed: 25699541] | Intervention not in PICO: Acute hip fracture care and not coordination of rehabilitation. |
| Pogoda, Terri K., Levy, Charles E., Helmick, Katherine, Pugh, Mary Jo, Health services and rehabilitation for active duty service members and veterans with mild TBI, Brain Injury, 31, 1220–1234, 2017 [PubMed: 28981342] | Narrative overview including cost considerations; not an economic evaluation. |
| Soong, C., Cram, P., Chezar, K., Tajammal, F., Exconde, K., Matelski, J., Sinha, S.K., Abrams, H.B., Fan-Lun, C., Fabbruzzo-Cota, C. and Backstein, D., Impact of an integrated hip fracture inpatient program on length of stay and costs, Journal of orthopaedic trauma, 30, 647–652, 2016 [PubMed: 27875490] | Inpatient setting. |
Excluded studies for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
Quantitative clinical studies
Table 42Excluded quantitative studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Adams, Annette L., Schiff, Melissa A., Koepsell, Thomas D., Rivara, Frederick P., Leroux, Brian G., Becker, Thomas M., Hedges, Jerris R., Physician consultation, multidisciplinary care, and 1-year mortality in Medicare recipients hospitalized with hip and lower extremity injuries, Journal of the American Geriatrics Society, 58, 1835–42, 2010 [PubMed: 20929461] | Outcome not in PICO: Mortality |
| Aitken, Mary E., Korehbandi, Patricia, Parnell, Donna, Parker, James G., Stefans, Vikki, Tompkins, Esther, Schulz, Eldon G., Experiences from the development of a comprehensive family support program for pediatric trauma and rehabilitation patients, Archives of Physical Medicine and Rehabilitation, 86, 175–9, 2005 [PubMed: 15641010] | Study design not in PICO: Non-comparative study |
| Albert, Steven M., Im, Ashley, Brenner, Lynda, Smith, Michael, Waxman, Richard, Effect of a social work liaison program on family caregivers to people with brain injury, The Journal of Head Trauma Rehabilitation, 17, 175–89, 2002 [PubMed: 11909513] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=27 in intervention, n=29 in control) |
| Anderson, J., Mason, C., Reverse culture - How intensive care coordination eases military transitions for returning soldiers with traumatic brain injuries, Brain Injury, Conference, 2010 | Published as abstract only |
| Anderson, J., Mason, C., Reverse culture shock - Military transitions for returning soldiers with traumatic brain injury, Journal of Head Trauma Rehabilitation, Conference, 2008 | Published as abstract only |
| Anderson, Mary E., McDevitt, Kelly, Cumbler, Ethan, Bennett, Heather, Robison, Zachary, Gomez, Bryan, Stoneback, Jason W., Geriatric Hip Fracture Care: Fixing a Fragmented System, The Permanente journal, 21, 16–104, 2017 [PMC free article: PMC5424597] [PubMed: 28488991] | Population not in PICO: Patients ≥ 18 years old |
| Andersson, E. E., Emanuelson, I., Björklund, R., StaËšlhammar, D., Mild traumatic brain injuries: the impact of early intervention on late sequelae. A randomized controlled trial, Brain Injury, 26, 520–521, 2012 | Published as abstract only |
| Anonymous,, Trauma center boosts patient outcomes, Hospital case management : the monthly update on hospital-based care planning and critical paths, 9, 115–6, 2001 [PubMed: 11469007] | Narrative review |
| Asplin, G., Carlsson, G., Zidén, L., Kjellby-Wendt, G., Early coordinated rehabilitation in acute phase after hip fracture - a model for increased patient participation, BMC Geriatrics, 17, 240, 2017 [PMC free article: PMC5646112] [PubMed: 29041916] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=63 in intervention, n=63 in control) |
| Atwal, Anita, Caldwell, Kay, Do multidisciplinary integrated care pathways improve interprofessional collaboration?, Scandinavian journal of caring sciences, 16, 360–7, 2002 [PubMed: 12445105] | Study design not in PICO: Qualitative study and audit performed before 2000 |
| Avlund, K., Jepsen, E., Vass, M., Lundemark, H., Effects of comprehensive follow-up home visits after hospitalization on functional ability and readmissions among old patients. A randomized controlled study, Scandinavian Journal of Occupational Therapy, 9, 17–22, 2002 | Study dates not in PICO: 1996-1997 |
| Ayvazian, J., Lucente, J., Dudley-Brown, S., Clinical management of veterans with traumatic brain injury within the context of polytrauma, Journal of Head Trauma Rehabilitation, Conference, 2012 | Published as abstract only |
| Bandyopadhyay, S., Wilkinson, I., Giokarinin-Royal, T., How incorporating ‘lean’ approach led to improved delivery of care and reduction in length of hospital stay, Age and Ageing, 48, 2019 | Published as abstract only |
| Baron, Justine S., Sullivan, Katrina J., Swaine, Jillian M., Aspinall, Arlene, Jaglal, Susan, Presseau, Justin, White, Barry, Wolfe, Dalton, Grimshaw, Jeremy M., Self-management interventions for skin care in people with a spinal cord injury: part 1-a systematic review of intervention content and effectiveness, Spinal Cord, 56, 823–836, 2018 [PMC free article: PMC6128818] [PubMed: 29802393] | Systematic review: Included studies checked for relevance. |
| Baron, Justine S., Sullivan, Katrina J., Swaine, Jillian M., Aspinall, Arlene, Jaglal, Susan, Presseau, Justin, Wolfe, Dalton, Grimshaw, Jeremy M., Self-management interventions for skin care in people with a spinal cord injury: part 2-a systematic review of use of theory and quality of intervention reporting, Spinal Cord, 56, 837–846, 2018 [PMC free article: PMC6128816] [PubMed: 29795415] | Systematic review: Included studies checked for relevance. |
| Baron, Justine, Swaine, Jillian, Presseau, J., Aspinall, Arlene, Jaglal, Susan, White, Barry, Wolfe, Dalton, Grimshaw, Jeremy, Self-management interventions to improve skin care for pressure ulcer prevention in people with spinal cord injuries: a systematic review protocol, Systematic reviews, 5, 150, 2016 [PMC free article: PMC5011862] [PubMed: 27600153] | Published protocol for a systematic review |
| Bayley, M. T., Lamontagne, M. E., Kua, A., Marshall, S., Marier-Deschenes, P., Allaire, A. S., Kagan, C., Truchon, C., Janzen, S., Teasell, R., Swaine, B., Unique features of the INESSS-Onf rehabilitation guidelines for moderate to severe traumatic brain injury: Responding to users’ needs, Journal of Head Trauma Rehabilitation, 33, 296–305, 2018 [PubMed: 30188459] | Results not in PICO: Guideline recommendations for moderate/severe TBI. No raw data presented. Systematic review performed as part of methodology but results and references not presented to check. |
| Beadle, E., Watter, K., Murray, A., Kennedy, A., The integration of telehealth into a community-based interdisciplinary brain injury service, Brain Impairment, 20, 345, 2019 | Published as abstract only |
| Berggren, M., Karlsson, Å, Lindelöf, N., Englund, U., Olofsson, B., Nordström, P., Gustafson, Y., Stenvall, M., Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: a randomized controlled trial, Clinical Rehabilitation, 33, 64–73, 2019 [PMC free article: PMC6311618] [PubMed: 30064264] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (n=106 in intervention, n=93 in control) |
| Bhattacharyya, R., Agrawal, Y., Elphick, H., Blundell, C., The impact of a new model of hip fracture care at a teaching hospital, Osteoporosis International, 23, S566–S567, 2012 | Published as abstract only |
| Bhattacharyya, Rahul, Agrawal, Yuvraj, Elphick, Heather, Blundell, Chris, A unique orthogeriatric model: a step forward in improving the quality of care for hip fracture patients, International journal of surgery (London, England), 11, 1083–6, 2013 [PubMed: 24120890] | Unclear comparator: Only described as “patients remain primarily under the care of the orthopaedic teams” (p. 1084) |
| Bloemen-Vrencken, J. H. A., de Witte, L. P., Engels, J. P. G. M., van den Heuvel, W. J. A., Post, M. W. M., Transmural care in the rehabilitation sector: implementation experiences with a transmural care model for people with spinal cord injury, International journal of integrated care, 5, e02, 2005 [PMC free article: PMC1395505] [PubMed: 16773154] | Study design not in PICO: No comparison group |
| Bloemen-Vrencken, J. H. A., de Witte, L. P., Post, M. W. M., Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation, Spinal cord, 43, 462–75, 2005 [PubMed: 15838530] | Systematic review: Included studies checked for relevance. |
| Bogie, Kath M., Ho, Chester H., Multidisciplinary approaches to the pressure ulcer problem, Ostomy/wound management, 53, 26–32, 2007 [PubMed: 17978412] | Narrative review |
| Bolster, M. B., Cevallos, S., Beyer, L., Kronenberg, H. M., Leder, B., A model for improved management of fragility fractures: Navigating the fracture liaison service, Arthritis and Rheumatology, 69, 2017 | Published as abstract only |
| Brasure, Michelle, Lamberty, Greg J., Sayer, Nina A., Nelson, Nathaniel W., Macdonald, Roderick, Ouellette, Jeannine, Wilt, Timothy J., Participation after multidisciplinary rehabilitation for moderate to severe traumatic brain injury in adults: a systematic review, Archives of physical medicine and rehabilitation, 94, 1398–420, 2013 [PubMed: 23348125] | Systematic review: Included studies checked for relevance. |
| Browne, Allyson L., Appleton, Sally, Fong, Kim, Wood, Fiona, Coll, Fiona, de Munck, Sonja, Newnham, Elizabeth, Schug, Stephan A., A pilot randomized controlled trial of an early multidisciplinary model to prevent disability following traumatic injury, Disability and Rehabilitation, 35, 1149–63, 2013 [PubMed: 23083416] | Population not in PICO: Patients ≥ 18 years old |
| Buccellato, K. H., Nordstrom, M., Murphy, J. M., Burdea, G. C., Polistico, K., House, G., Kim, N., Grampurohit, N., Sorensen, J., Isaacson, B. M., et al.,, A Randomized Feasibility Trial of a Novel, Integrative, and Intensive Virtual Rehabilitation Program for Service Members Post-Acquired Brain Injury, Military Medicine, 2019 [PubMed: 31268524] | Comparison not in PICO: Immediate (weeks 0-6) versus delayed (weeks 3-9) outpatient cognitive rehabilitation program. However, immediate versus delayed does not appear to relate to the time of discharge for the patients; same study as Buccellato 2020 |
| Buccellato, Kiara H., Nordstrom, Michelle, Murphy, Justin M., Burdea, Grigore C., Polistico, Kevin, House, Gregory, Kim, Nam, Grampurohit, Namrata, Sorensen, Jeff, Isaacson, Brad M., Pasquina, Paul F., A Randomized Feasibility Trial of a Novel, Integrative, and Intensive Virtual Rehabilitation Program for Service Members Post-Acquired Brain Injury, Military Medicine, 185, e203–e211, 2020 [PubMed: 31268524] | Comparison not in PICO: Immediate (weeks 0-6) versus delayed (weeks 3-9) outpatient cognitive rehabilitation program. However, immediate versus delayed does not appear to relate to the time of discharge for the patients; same study as Buccellato 2019 |
| Burch, D., Bernert, S., Fraser, J. F., Increased physician and physical therapist communication is associated with earlier mobility and decreased length of stay in the cerebrovascular and trauma neuroscience population, NeuroRehabilitation, 43, 195–199, 2018 [PubMed: 30040766] | Study design not in PICO: Non-randomised study with mixed population and less than N=100 in each group of population |
| Burch, D., Bernert, S., Fraser, J. F., Increased physician and physical therapist communication is associated with earlier mobility and decreased length of stay in the cerebrovascular and trauma neuroscience population, Stroke, 47, 2016 [PubMed: 30040766] | Published as abstract only |
| Burgo-Black, L., Hunt, S. C., Implementing a system of integrated post deployment care for returning combat veterans, Journal of General Internal Medicine, Conference, 2012 [PMC free article: PMC3514997] [PubMed: 22648608] | Published as abstract only |
| Burns, A., Aarabi, B., Anderson, P., Arnold, P., Brodke, D., Chiba, K., Dettori, J., Furlan, J., Harrop, J., Holly, L., Howley, S., Jeji, T., Kalsi-Ryan, S., Kotter, M., Kurpad, S., Kwon, B., Marino, R., Martin, A., Massicotte, E., Merli, G., Middleton, J., Nakashima, H., Nagoshi, N., Palmieri, K., Shamji, M., Singh, A., Skelly, A., Tetreault, L., Wilson, J., Yee, A., Fehlings, M., A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the type and timing of rehabilitation, Global Spine Journal, 7, 358S–359S, 2017 [PMC free article: PMC5684839] [PubMed: 29164029] | Published as abstract only |
| Calleja, Pauline, Aitken, Leanne M., Cooke, Marie L., Information transfer for multi-trauma patients on discharge from the emergency department: mixed-method narrative review, Journal of Advanced Nursing, 67, 4–18, 2011 [PubMed: 21158900] | Semi-systematic review emphasising qualitative research/analysis methods. Additionally, it focuses on trauma care and does not mention rehabilitation. |
| Callender, Librada, Brown, Rachel, Driver, Simon, Dahdah, Marie, Collinsworth, Ashley, Shafi, Shahid, Process for developing rehabilitation practice recommendations for individuals with traumatic brain injury, BMC neurology, 17, 54, 2017 [PMC free article: PMC5359914] [PubMed: 28320346] | Technical paper about how to develop an evidence-based guideline; contains no primary or secondary data. |
| Cameron, I. D., Handoll, H. H. G., Finnegan, T. P., Langhorne, P., Multidisciplinary rehabilitation for older people with hip fractures, Cochrane Database of Systematic Reviews, CD007125, 2008 [PMC free article: PMC8586844] [PubMed: 34766330] | Earlier version of Handoll 2009 |
| Cameron, I. D., Handoll, H. H., Finnegan, T. P., Madhok, R., Langhorne, P., Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures, The Cochrane database of systematic reviews, CD000106, 2001 [PubMed: 11686951] | Earlier version of Cameron 2009 |
| Cameron, Ian D., Coordinated multidisciplinary rehabilitation after hip fracture, Disability and rehabilitation, 27, 1081–90, 2005 [PubMed: 16315427] | Narrative review |
| Cameron, Ian D., Handoll, Helen Hg, Finnegan, Terence P., Madhok, Rajan, Langhorne, Peter, WITHDRAWN: Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures, The Cochrane database of systematic reviews, CD000106, 2009 [PubMed: 10796300] | Withdrawn from the Cochrane library as it has been incorporated into another review with an expended scope (Handoll 2009) |
| Campbell, C. V., Cooper, J., Shabir, F., Wills, E., Ong, T., An enhanced therapy service for patients with fractured neck of femur - Service evaluation of a pilot project, Age and Ageing, 46, 2017 | Published as abstract only |
| Canadillas Rueda, R., Domingo Montesinos, N., Natividad Pedreno, M., Comprehensive treatment and secondary prevention of fragility fractures in the elderly in an orthogeriatric unit. Multidisciplinary management of osteoporotic patients pre and post surgery. Advantages and results, Osteoporosis International, 27, S539, 2016 | Published as abstract only |
| Careau, Emmanuelle, Dussault, Julie, Vincent, Claude, Development of interprofessional care plans for spinal cord injury clients through videoconferencing, Journal of interprofessional care, 24, 115–8, 2010 [PubMed: 19705312] | Study design not in PICO: No comparison group |
| Carney, Nancy A., Petroni, Gustavo J., Lujan, Silvia B., Ballarini, Nicolas M., Faguaga, Gabriela A., du Coudray, Hugo E. M., Huddleston, Amy E., Baggio, Gloria M., Becerra, Juan M., Busso, Leonardo O., Dikmen, Sureyya S., Falcone, Roberto, Garcia, Mirta E., Gonzalez Carrillo, Osvaldo R., Medici, Paula L., Quaglino, Marta B., Randisi, Carina A., Saenz, Silvia S., Temkin, Nancy R., Vanella, Elida E., Postdischarge Care of Pediatric Traumatic Brain Injury in Argentina: A Multicenter Randomized Controlled Trial, Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 17, 658–66, 2016 [PMC free article: PMC4938734] [PubMed: 27243414] | Intervention not in PICO: Discharge support related to medical care. Study does not report on patients receiving rehabilitation or social care |
| Carroll, V., The Adult Patient Assessment Tool and care plan, Australian nursing journal (July 1993), 14, 29–32, 2007 [PubMed: 17319187] | Outcomes and population not in PICO: Description of the development of an assessment tool by a multi-disciplinary working group |
| Castillo, Renan C., Wegener, Stephen T., Newell, Mary Zadnik, Carlini, Anthony R., Bradford, Anna N., Heins, Sara E., Wysocki, Elizabeth, Pollak, Andrew N., Teter, Harry, Mackenzie, Ellen J., Improving outcomes at Level I trauma centers: an early evaluation of the Trauma Survivors Network, The journal of trauma and acute care surgery, 74, 1534–40, 2013 [PubMed: 23694884] | Intervention and comparison not in PICO: Trauma survivor network program consisting of self-management course, peer support, information access and provider training standard care versus standard care |
| Chang, C. B., Yang, R. S., Huang, W. J., Chan, D. C., Fracture type on the outcome of patients managed within the fracture liaison and osteoporosis medication management services, Osteoporosis International, 30, S92, 2019 [PMC free article: PMC6626060] [PubMed: 31300660] | Published as abstract only |
| Chong, Tsung Wei, Chan, Gribson, Feng, Liang, Goh, Susie, Hew, Agnes, Ng, Tze Pin, Tan, Boon Yeow, Integrated care pathway for hip fractures in a subacute rehabilitation setting, Annals of the Academy of Medicine, Singapore, 42, 579–84, 2013 [PubMed: 24356654] | Population not in PICO: Patients ≥ 18 years old |
| Chudyk, Anna M., Jutai, Jeffrey W., Petrella, Robert J., Speechley, Mark, Systematic review of hip fracture rehabilitation practices in the elderly, Archives of physical medicine and rehabilitation, 90, 246–62, 2009 [PubMed: 19236978] | Systematic review: Included studies checked for relevance. |
| Clark, J., Gill, C., Sprott, A., Joined up thinking: A model for long-term abi rehabilitation after return home, Brain Injury, 26, 432–433, 2012 | Published as abstract only |
| Closa, Conxita, Mas, Miquel A., Santaeugenia, Sebastia J., Inzitari, Marco, Ribera, Aida, Gallofre, Miquel, Hospital-at-home Integrated Care Program for Older Patients With Orthopedic Processes: An Efficient Alternative to Usual Hospital-Based Care, Journal of the American Medical Directors Association, 18, 780–784, 2017 [PubMed: 28578883] | Study design not in PICO: Non-randomised study with less than N=100 in at least 1 intervention group |
| Coetzer, Rudi, Holistic neuro-rehabilitation in the community: is identity a key issue?, Neuropsychological rehabilitation, 18, 766–83, 2008 [PubMed: 18654932] | Narrative review |
| Collins, Nina, Miller, Richard, Kapu, April, Martin, Rita, Morton, Melissa, Forrester, Mary, Atkinson, Shelley, Evans, Bethany, Wilkinson, Linda, Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction, The journal of trauma and acute care surgery, 76, 353–7, 2014 [PubMed: 24398767] | Intervention not in PICO: Acute care nurse practitioner (ACNP) who coordinated acute/ clinical care with a very brief mention of rehabilitation was “The ACNP attended the daily “discharge huddle”™ a team meeting that encompasses T2 [step-down care from ICU] and T3 [trauma nurse practitioner satellite service] NPs [nurse practitioner], case managers, social worker, liaisons to rehabilitation and nursing home facilities, and home health agency staff to facilitate communication and the discharge process." (p. 354). Only outcome reported is length of stay. |
| Cooper, M., Ganda, K., Palmer, A., Seibel, M. J., Cost effectiveness of a targeted intervention to reduce refracture rates: Analysis of a four year prospective controlled study, Journal of Bone and Mineral Research, 26, 2011 | Published as abstract only |
| Cooper, M., Palmer, A., Ganda, K., Seibel, M. J., Cost-effectiveness of a targeted intervention to reduce the rate of refracture: Results ofa 4-year prospective controlled study, Osteoporosis International, 22, S651–S652, 2011 [PubMed: 21107534] | Published as abstract only |
| Cordasco, K. M., Saifu, H., Rubenstein, L. V., Khafaf, M., Doyle, B., Hsiao, J., Orshansky, G., Ganz, D., The ED-PACT tool: Communicating veterans’ care needs after emergency department visits via electronic messages, Journal of General Internal Medicine, 32, S800, 2017 | Published as abstract only |
| Corser, William D., Postdischarge outcome rates influenced by comorbidity and interdisciplinary collaboration, Outcomes management, 8, 45–51, 2004 [PubMed: 14740584] | Study design and population not in PICO: Non-randomised study with less than N=100 in each arm (total N=189). Unclear exactly why population admitted, but n=67 were admitted from medical cardiac services. |
| Crotty, M., Rowett, D., Spurling, L., Giles, L. C., Phillips, P. A., Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial, American Journal Geriatric Pharmacotherapy, 2, 257–264, 2004 [PubMed: 15903284] | Unclear population: Older people being transferred from hospital to long term care facility with no further details. |
| Crotty, M., Whitehead, C. H., Gray, S., Finucane, P. M., Early discharge and home rehabilitation after hip fracture achieves functional improvements: A randomized controlled trial, Clinical Rehabilitation, 16, 406–413, 2002 [PubMed: 12061475] | Study dates not in PICO: 1998-1999 |
| Crouch, D., Taking spinal care into the community, Nursing times, 100, 24–25, 2004 [PubMed: 15307640] | Narrative review |
| Cuthbert, J., Anderson, J., Mason, C., Block, S., Martin, K., Dettmer, J., Weintraub, A., Harrison-Felix, C., Evaluating case management needs and impact for adults with chronic TBI, Brain Injury, 28, 706, 2014 | Published as abstract only |
| Davies Urizar, B., Malanga Ferrari, A., Garcia Fernandez, J. A., Martin De Francisco Murga, E., Alonso Bouzon, C., Rodriguez-Manas, L., Benefits of an orthogeriatric unit, European Geriatric Medicine, 2, S138, 2011 | Published as abstract only |
| De Goumoens, V., Rio, L. M., Jaques, C., Ramelet, A. S., Family-oriented interventions for adults with acquired brain injury and their families: A scoping review, JBI Database of Systematic Reviews and Implementation Reports, 16, 2330–2367, 2018 [PubMed: 30531483] | Systematic review: Included studies checked for relevance. |
| Dibardino, D., Cohen, E. R., Didwania, A., Meta-analysis: Multidisciplinary fall prevention strategies in the acute care inpatient population, Journal of Hospital Medicine, 7, 497–503, 2012 [PubMed: 22371369] | Systematic review: Included studies checked for relevance. |
| Doloresco, L., CARF: symbol of rehabilitation excellence, SCI nursing : a publication of the American Association of Spinal Cord Injury Nurses, 18, 165–172, 2001 [PubMed: 12503464] | Article not available |
| Donohue, Kathleen, Hoevenaars, Richelle, McEachern, Jocelyn, Zeman, Erica, Mehta, Saurabh, Home-Based Multidisciplinary Rehabilitation following Hip Fracture Surgery: What Is the Evidence?, Rehabilitation research and practice, 2013, 875968, 2013 [PMC free article: PMC3877638] [PubMed: 24455275] | Systematic review: Included studies checked for relevance. |
| Dorsey, Julie, Bradshaw, Michelle, Effectiveness of Occupational Therapy Interventions for Lower-Extremity Musculoskeletal Disorders: A Systematic Review, The American journal of occupational therapy : official publication of the American Occupational Therapy Association, 71, 7101180030p1–7101180030p11, 2017 [PubMed: 28027040] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Drago, K., Bernstein, J., Graven, P., Dobbertin, K., Eckstrom, E., Higher quality, lower cost with a geriatrics consult service, Journal of the American Geriatrics Society, 65, S36, 2017 [PubMed: 30094830] | Published as abstract only |
| Driessen, Julia, Bellon, Johanna E., Stevans, Joel, Forsythe, Raquel M., Reynolds, Benjamin R., James, A. Everette, 3rd, Perceived performance and impact of a non-physician-led interprofessional team in a trauma clinic setting, Journal of interprofessional care, 31, 112–114, 2017 [PubMed: 27880082] | Outcomes not in PICO: Team survey responses, consults given and new therapy referrals initiated. |
| Dunn, A. M., Boylston, M., Establishing a consultation service through multidisciplinary rounds, PM and R, 7, S151–S152, 2015 | Published as abstract only |
| Dutton, Richard P., Cooper, Carnell, Jones, Alan, Leone, Susan, Kramer, Mary E., Scalea, Thomas M., Daily multidisciplinary rounds shorten length of stay for trauma patients, The Journal of trauma, 55, 913–9, 2003 [PubMed: 14608165] | Intervention not in PICO: Daily multidisciplinary rounds focused on medical care, not coordination or delivery of rehabilitation or social care. |
| Eicher, Vicki, Murphy, Mary Pat, Murphy, Thomas F., Malec, James F., Progress assessed with the Mayo-Portland Adaptability Inventory in 604 participants in 4 types of post-inpatient rehabilitation brain injury programs, Archives of Physical Medicine and Rehabilitation, 93, 100–7, 2012 [PubMed: 22200388] | Interventions not in PICO: 4 different rehabilitation programmes with different content, not coordination or delivery of rehabilitation or social care. |
| Espinoza, L., Scudder, B., Rosario, E., Patient navigation for traumatic brain injury, Journal of Head Trauma Rehabilitation, Conference, 2013 | Published as abstract only |
| Farba, L., Cypin, I., Spesivtcev, I., The first assessment of the principles of “Co-managed care in elderly patients” in Moscow City hospital #13, Osteoporosis International, 27, S131, 2016 | Published as abstract only |
| Faux, S., Wu, J., Harris, I., Poulos, C., Klein, L., Murray, G., Wilson, S., John, E., Early rehabilitation after hospital admission for road-trauma via an in-reach mobile team; a randomised controlled trial, Archives of Physical Medicine and Rehabilitation, 97, e15–e16, 2016 | Published as abstract only |
| Featherall, J., Brigati, D. P., Faour, M., Messner, W., Higuera, C. A., Implementation of a Total Hip Arthroplasty Care Pathway at a High-Volume Health System: Effect on Length of Stay, Discharge Disposition, and 90-Day Complications, Journal of Arthroplasty, 33, 1675–1680, 2018 [PubMed: 29478678] | Intervention not in PICO: Hip arthroplasty care pathway, including pre-operative, peri-operative and post-operative interventions. Mention of clinical care coordinator in the post-operative section but not able to quantify what is due to care coordinator and what is attributable to other interventions. |
| Fernandez, M. A., Griffin, X. L., Costa, M. L., Management of hip fracture, British medical bulletin, 115, 165–72, 2015 [PubMed: 26311503] | Narrative review |
| Fernandez-Moyano, A., Fernandez-Ojeda, R., Ruiz-Romero, V., Garcia-Benitez, B., Palmero-Palmero, C., Aparicio-Santos, R., Comprehensive care program for elderly patients over 65 years with hip fracture, Revista clinica espanola, 214, 17–23, 2014 [PubMed: 23541310] | Length of stay and readmission data does not have enough details reported to compare results of pre-implementation group and post-implementation group (no mean or standard deviation for the before group and no statistical analysis presented). Barthel Index is only compared between those who survived and those who died during the study period. |
| Fiona, N., Lucinda, M., Margot, P., Gabor, M., Suzanne, M., Bernard, W., Erica, E., Sanjay, G., Implementation of re-fracture prevention of >65 year old inpatient fractured neck of femur prior to discharge, Internal Medicine Journal, 46, 10, 2016 | Published as abstract only |
| Fitzsimmons, R. D., Brain injury case management: The potential and limitations of late-stage intervention - A pilot study, Brain Injury, 17, 947–971, 2003 [PubMed: 14514447] | Study design not in PICO: Non-randomised study with less than N=100 in each arm (total N=22) |
| Flikweert, E. R., Izaks, G. J., Knobben, B. A., Stevens, M., Wendt, K., The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial, BMC Musculoskeletal Disorders, 15, 188, 2014 [PMC free article: PMC4053577] [PubMed: 24885674] | Population not in PICO: Patients ≥ 18 years old |
| Flinn, N. A., Kelley, T., Foo, S., Medical home for persons with disabilities: A target for the triple aim, Archives of Physical Medicine and Rehabilitation, 94, e55–e56, 2013 | Published as abstract only |
| Fojas Ma, C. M., Ing, S. W., Phieffer, L., Stephens, J., Southerland, L., Evolution of a fracture prevention program : A review of our experience at the Ohio state university, Endocrine Reviews, 37, 2016 | Published as abstract only |
| Forni, Silvia, Pieralli, Francesca, Sergi, Alessandro, Lorini, Chiara, Bonaccorsi, Guglielmo, Vannucci, Andrea, Mortality after hip fracture in the elderly: The role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients, Archives of Gerontology and Geriatrics, 66, 13–7, 2016 [PubMed: 27174126] | Intervention not in PICO: Multi-disciplinary team designed to acutely treat hip fracture patients in order to decrease time from admission to surgery, rather than multi-disciplinary team for rehabilitation care |
| Franz, Shiney, Muser, Jurgen, Thielhorn, Ulrike, Wallesch, Claus W., Behrens, Johann, Inter-professional communication and interaction in the neurological rehabilitation team: a literature review, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30457016] | Systematic review: Included studies checked for relevance. |
| Fukuda, Haruhisa, Shimizu, Sayuri, Ishizaki, Tatsuro, Has the Reform of the Japanese Healthcare Provision System Improved the Value in Healthcare? A Cost-Consequence Analysis of Organized Care for Hip Fracture Patients, PLoS ONE, 10, e0133694, 2015 [PMC free article: PMC4514762] [PubMed: 26208322] | Comparison not in PICO: Hip fracture care in hospitals autonomously providing integrated care across specialties versus in acute care hospitals and rehabilitative care hospitals providing organized care across separate facilities (the organisation of the care is not further described). |
| Furlan, Andrea D., Irvin, Emma, Munhall, Claire, Giraldo-Prieto, Mario, Fullerton, Laura, McMaster, Robert, Danak, Shivang, Costante, Alicia, Pitzul, Kristen, Bhide, Rohit P., Marchenko, Stanislav, Mahood, Quenby, David, Judy A., Flannery, John F., Bayley, Mark, Rehabilitation service models for people with physical and/or mental disability living in low- and middle-income countries: A systematic review, Journal of Rehabilitation Medicine, 50, 487–498, 2018 [PubMed: 29616278] | Systematic review: Included studies checked for relevance. |
| Gailey, Robert, Gaunaurd, Ignacio, Raya, Michele, Kirk-Sanchez, Neva, Prieto-Sanchez, Luz M., Roach, Kathryn, Effectiveness of an Evidence-Based Amputee Rehabilitation (EBAR) Program: A Pilot Randomized Controlled Trial, Physical therapy, 2020 [PubMed: 31951260] | Intervention not in PICO: Rehabilitation programme designed to occur after participants had completed physical therapy and prosthetic training. |
| Gjerberg, Elisabeth, Flottorp, Signe, Holte, Hilde H., 2008 [PubMed: 29320096] | Article not available |
| Grabljevec, Klemen, Singh, Rajiv, Denes, Zoltan, Angerova, Yvona, Nunes, Renato, Boldrini, Paolo, Delargy, Mark, Laxe, Sara, Kiekens, Carlotte, Varela Donoso, Enrique, Christodoulou, Nicolas, Evidence-based position paper on Physical and Rehabilitation Medicine professional practice for Adults with Acquired Brain Injury. The European PRM position (UEMS PRM Section), European journal of physical and rehabilitation medicine, 54, 971–979, 2018 [PubMed: 30160441] | Systematic review: Included studies checked for relevance. |
| Gregersen, Merete, Morch, Marianne Metz, Hougaard, Kjeld, Damsgaard, Else Marie, Geriatric intervention in elderly patients with hip fracture in an orthopedic ward, Journal of injury & violence research, 4, 45–51, 2012 [PMC free article: PMC3426900] [PubMed: 21502786] | Intervention not in PICO: Multi-disciplinary team designed to acutely treat hip fracture patients in order to decrease time from admission to surgery, rather than multi-disciplinary team for rehabilitation care |
| Grigoryan, K., Javedan, H., Rudolph, J., Ortho-geriatric models and optimal outcomes: A systematic review and meta-analysis, Journal of the American Geriatrics Society, 61, S8–S9, 2013 | Published as abstract only |
| Grigoryan, Konstantin V., Javedan, Houman, Rudolph, James L., Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis, Journal of Orthopaedic Trauma, 28, e49–55, 2014 [PMC free article: PMC3909556] [PubMed: 23912859] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Grill, E., Ewert, T., Lipp, B., Mansmann, U., Stucki, G., Effectiveness of a community-based 3-year advisory program after acquired brain injury, European Journal of Neurology, 14, 1256–65, 2007 [PubMed: 17956446] | Mixed population: Only 310/1181 were in PICO (traumatic brain injury) but results are not presented separately for target population. |
| Grobe, K. F., Lin, S. J., Ababneh, A. F., Orozco, E. M., Maxey, K., Smarda, M. J., Lopez, A. R., The feasibility and effectiveness of an internet-based exercise program in individuals with spinal cord injury, Cardiopulmonary Physical Therapy Journal, 31, e16–e17, 2020 | Published as abstract only |
| Gupta, A., The effectiveness of geriatrician-led comprehensive hip fracture collaborative care in a new acute hip unit based in a general hospital setting in the UK, The journal of the Royal College of Physicians of Edinburgh, 44, 20–6, 2014 [PubMed: 24995442] | Intervention not in PICO: Multi-disciplinary team designed to acutely care for hip fracture patients pre- and post-operatively, rather than multi-disciplinary team for coordination of rehabilitation. |
| Guy, S., Kras-Dupuis, A., Wolfe, D., Hsieh, J., Walia, S., Askes, H., Spinal cord injury best practice implementation for pressure ulcer prevention: Initial implementation results, Archives of Physical Medicine and Rehabilitation, 94, e25, 2013 [PubMed: 30419231] | Published as abstract only |
| Haan, James M., Dutton, Richard P., Willis, Michelle, Leone, Susan, Kramer, Mary E., Scalea, Thomas M., Discharge rounds in the 80-hour workweek: importance of the trauma nurse practitioner, The Journal of trauma, 63, 339–43, 2007 [PubMed: 17693833] | Intervention not in PICO: Daily multidisciplinary rounds focused on medical care, not coordination or delivery of rehabilitation or social care. |
| Halbert, J., Crotty, M., Whitehead, C., Cameron, I., Kurrle, S., Graham, S., Handoll, H., Finnegan, T., Jones, T., Foley, A., Shanahan, M., Multi-disciplinary rehabilitation after hip fracture is associated with improved outcome: A systematic review, Journal of Rehabilitation Medicine, 39, 507–512, 2007 [PubMed: 17724548] | Systematic review: Included studies checked for relevance. |
| Hall, Erin C., Tyrrell, Rebecca L., Doyle, Karen E., Scalea, Thomas M., Stein, Deborah M., Trauma transitional care coordination: A mature system at work, The journal of trauma and acute care surgery, 84, 711–717, 2018 [PubMed: 29370060] | Population not in PICO: Patients ≥ 18 years old |
| Hall, Erin C., Tyrrell, Rebecca, Scalea, Thomas M., Stein, Deborah M., Trauma Transitional Care Coordination: protecting the most vulnerable trauma patients from hospital readmission, Trauma surgery & acute care open, 3, e000149, 2018 [PMC free article: PMC5887824] [PubMed: 29766133] | No information presented for comparison group, including number of participants. |
| Hammond, Flora M., Gassaway, Julie, Abeyta, Nichola, Freeman, Erma S., Primack, Donna, Kreider, Scott E. D., Whiteneck, Gale, Outcomes of social work and case management services during inpatient spinal cord injury rehabilitation: the SCIRehab project, The journal of spinal cord medicine, 35, 611–23, 2012 [PMC free article: PMC3522900] [PubMed: 23318040] | Study design not in PICO: No intervention. |
| Handoll, H. H. G., Cameron, I. D., Mak, J. C. S., Finnegan, T. P., Multidisciplinary rehabilitation for older people with hip fractures, Cochrane Database of Systematic Reviews, CD007125, 2009 [PubMed: 19821396] | Systematic review: Included studies checked for relevance. |
| Hart, Tessa, Brockway, Jo Ann, Maiuro, Roland D., Vaccaro, Monica, Fann, Jesse R., Mellick, David, Harrison-Felix, Cindy, Barber, Jason, Temkin, Nancy, Anger Self-Management Training for Chronic Moderate to Severe Traumatic Brain Injury: Results of a Randomized Controlled Trial, The Journal of head trauma rehabilitation, 32, 319–331, 2017 [PMC free article: PMC5593756] [PubMed: 28520666] | Intervention not in PICO: Treatment protocol for anger self-management training. No mention of co-ordination or delivery of rehabilitation. |
| Hart, Tessa, Driver, Simon, Sander, Angelle, Pappadis, Monique, Dams-O’Connor, Kristen, Bocage, Claire, Hinkens, Emma, Dahdah, Marie N., Cai, Xinsheng, Traumatic brain injury education for adult patients and families: a scoping review, Brain Injury, 32, 1295–1306, 2018 [PMC free article: PMC6321983] [PubMed: 30084694] | Systematic review: Included studies checked for relevance. |
| Hartwell, J., Albanese, K., Retterer, A., Martin, S., O’Mara, M. S., A trauma patient advocate is a valuable addition to the multidisciplinary trauma team: A process improvement project, American Surgeon, 82, S183–S185, 2016 [PubMed: 27657560] | No study results presented in paper |
| He, J., Wei, Q., Effect observation of community rehabilitation model on generic set of ICF for patients with TBI, Neurorehabilitation and Neural Repair, 32, 323–324, 2018 | Published as abstract only |
| Heinemann, A. W., Corrigan, J. D., Moore, D., Case Management for Traumatic Brain Injury Survivors with Alcohol Problems, Rehabilitation Psychology, 49, 156–166, 2004 | Intervention not in PICO: Comprehensive case management for people with traumatic brain injury and post-injury substance abuse |
| Heppenstall, C. P., Hanger, H. C., Wilkinson, T. J., The canterbury community rehabilitation, enablement and support team (CREST) service: A novel service to support wellbeing and independence in the community, Age and Ageing, 48, 2019 | Published as abstract only |
| Herrera-Espiñeira, C., Rodríguez del Águila Mdel, M., Navarro Espigares, J. L., Godoy Montijano, A., García Priego, A., Rodríguez, J. G., Sánchez, I. R., Effect of a telephone care program after hospital discharge from a trauma surgery unit, Gaceta sanitaria, 25, 133–138, 2011 [PubMed: 21334787] | Article in Spanish |
| Heyman, Noemi, Etzion, Isaac, Ben Natan, Merav, A coordination project for improvement of osteoporosis medication use among patients who sustained an osteoporotic fracture: The Israeli experience, Osteoporosis and Sarcopenia, 4, 134–139, 2018 [PMC free article: PMC6372825] [PubMed: 30775556] | Outcomes not in PICO: Osteoporosis medication use |
| Ho, W. S., Chan, H. H., Ying, S. Y., Cheng, H. S., Wong, C. S., Skin care in burn patients: A team approach, Burns, 27, 489–491, 2001 [PubMed: 11451603] | Study dates not in PICO: 1992-January 2000. Results not presented separately for the 1 month that was in PICO (January 2000) |
| Holliday, Anna, Samanta, Damayanti, Budinger, Julie, Hardway, Jessica, Bethea, Audis, An Outcome Analysis of Nurse Practitioners in Acute Care Trauma Services, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 24, 365–370, 2017 [PMC free article: PMC5929127] [PubMed: 29117053] | Intervention not in PICO: Nurse practitioners facilitated transfer throughout acute trauma services (including intensive care, floor, and post-acute clinic). Apart from placing the order for a rehabilitation consultation, there is no further mention of coordination of rehabilitation services. |
| Holstege, M. S., Bakkers, E., van Balen, R., Gussekloo, J., Achterberg, W. P., Caljouw, M. A., Structured scoring of supporting nursing tasks to enhance early discharge in geriatric rehabilitation: The BACK-HOME quasi-experimental study, International journal of nursing studies, 64, 13–18, 2016 [PubMed: 27657663] | Population not in PICO: Only 31% (reference) and 34% (intervention) were admitted for traumatic injury. Results not presented separately for cause of admission. |
| Holstege, M. S., Caljouw, M. A. A., Van Balen, R., Gussekloo, J., Achterberg, W. P., Effectiveness of innovations in geriatric rehabilitation. The SINGER Study, European Geriatric Medicine, 4, S109–S110, 2013 | Published as abstract only |
| Hossain, M. S., Harvey, L. A., Rahman, M. A., Bowden, J. L., Islam, M. S., Taylor, V., Muldoon, S., Herbert, R. D., A pilot randomised trial of community-based care following discharge from hospital with a recent spinal cord injury in Bangladesh, Clinical Rehabilitation, 31, 781–789, 2017 [PubMed: 27311454] | Unclear population: Inclusion criteria states participants with both traumatic and non-traumatic spinal cord injury. No further information about what proportions were traumatic, and results not presented separately for target population. |
| Houlihan, B., Brody, M., Skeels, S., Pernigotti, D., Zazula, J., Burnett, S., Green, C., Seetharama, S., Hasiotis, S., Belliveau, T., Rosenblum, D., Jette, A., RCT of peer-led phone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management, Archives of Physical Medicine and Rehabilitation, 98, e152, 2017 [PubMed: 28284835] | Published as abstract only |
| Houlihan, Bethlyn Vergo, Brody, Miriam, Everhart-Skeels, Sarah, Pernigotti, Diana, Burnett, Sam, Zazula, Judi, Green, Christa, Hasiotis, Stathis, Belliveau, Timothy, Seetharama, Subramani, Rosenblum, David, Jette, Alan, Randomized Trial of a Peer-Led, Telephone-Based Empowerment Intervention for Persons With Chronic Spinal Cord Injury Improves Health Self-Management, Archives of Physical Medicine and Rehabilitation, 98, 1067–1076.e1, 2017 [PubMed: 28284835] | Intervention not in PICO: ‘My Care My Call’ designed for people with SCI already in the community. No mention of coordination or delivery of rehabilitation or social care during transfer. |
| Huang, T. T., Liang, S. H., A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling, J Clin Nurs, 14, 1193–201, 2005 [PubMed: 16238765] | Population not in PICO: Patients ≥ 18 years old |
| Hums, Wendy, Williams, Julianne, Dedicated trauma care unit: an outcome-based model, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 12, 21–6, 2005 [PubMed: 15916314] | Narrative review |
| Jaber, Ala’a F., Hartwell, Julie, Radel, Jeff D., Interventions to Address the Needs of Adults With Postconcussion Syndrome: A Systematic Review, The American journal of occupational therapy : official publication of the American Occupational Therapy Association, 73, 7301205020p1–7301205020p12, 2019 [PubMed: 30839257] | Article not available |
| Johansen, Inger, Lindbaek, Morten, Stanghelle, Johan K., Brekke, Mette, Structured community-based inpatient rehabilitation of older patients is better than standard primary health care rehabilitation: an open comparative study, Disability and Rehabilitation, 34, 2039–46, 2012 [PubMed: 22452632] | Study design not in PICO: Non-randomised study. Although N=100 in one of the comparison groups, patients had mixed aetiologies (for example, 16/100 had stroke) |
| Johnson, M. K., Yanko, J. R., Collaborative practice: a successful model, SCI nursing : a publication of the American Association of Spinal Cord Injury Nurses, 18, 7–10, 2001 [PubMed: 12035480] | Article not available |
| Jones, Taryn M., Dean, Catherine M., Hush, Julia M., Dear, Blake F., Titov, Nickolai, A systematic review of the efficacy of self-management programs for increasing physical activity in community-dwelling adults with acquired brain injury (ABI), Systematic reviews, 4, 51, 2015 [PMC free article: PMC4422226] [PubMed: 25927591] | Systematic review: Included studies checked for relevance. |
| Jonsson, A., Gustafson, Y., Scholl, M., Hansen, F. R., Saarela, M., Nygaard, H., Laake, K., Jonsson, P. V., Valvanne, J., Dehlin, O., Geriatric rehabilitation as an integral part of geriatric medicine in the Nordic countries, Danish Medical Bulletin, 50, 439–445, 2003 [PubMed: 14694856] | Narrative review |
| Kammerlander, C., Gosch, M., Blauth, M., Lechleitner, M., Luger, T. J., Roth, T., The Tyrolean Geriatric Fracture Center: an orthogeriatric co-management model, Zeitschrift fur Gerontologie und Geriatrie, 44, 363–7, 2011 [PubMed: 22159829] | Study design not in PICO: No comparison group. |
| Kapu, A., Jones, P., Financial impact of adding acute care nurse practitioners (ACNPs) to inpatient models of care, Critical Care Medicine, 40, 27, 2012 | Published as abstract only |
| Karlsson, A., Berggren, M., Gustafson, Y., B, Olofsson, Lindelöf, N., Stenvall, M., Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial, Journal of the American Medical Directors Association, 17, 464.e9–e464.e15, 2016 [PubMed: 26975205] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard inpatient rehabilitation but the intervention group received Geriatric Interdisciplinary Home Rehabilitation after discharge which included a High-Intensity Functional Exercise programme and medical care. |
| Karlsson, A., Lindelof, N., Olofsson, B., Berggren, M., Gustafson, Y., Nordstrom, P., Stenvall, M., Effects of Geriatric Interdisciplinary Home Rehabilitation on Independence in Activities of Daily Living in Older People With Hip Fracture: A Randomized Controlled Trial, Archives of Physical Medicine and Rehabilitation, 2020 [PubMed: 31935353] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard inpatient rehabilitation but the intervention group received Geriatric Interdisciplinary Home Rehabilitation after discharge which included a High-Intensity Functional Exercise programme and medical care. |
| Kennedy, K., Establishing an orthopaedic physiotherapy practitioner role on the wards of an acute trauma hospital, Physiotherapy (United Kingdom), 97, eS1529, 2011 | Published as abstract only |
| Khan, F., Amatya, B., Hoffman, K., Systematic review of multidisciplinary rehabilitation in patients with multiple trauma, The British journal of surgery, 99 Suppl 1, 88–96, 2012 [PubMed: 22441861] | Systematic review: Included studies checked for relevance. |
| Khan, S. K., Shirley, M. D., Glennie, C., Fearon, P. V., Deehan, D. J., Achieving best practice tariff may not reflect improved survival after hip fracture treatment, Clinical Interventions in Aging, 9, 2097–2102, 2014 [PMC free article: PMC4257023] [PubMed: 25489240] | Intervention not in PICO: Best practice tariffs for achieving targets, but no information presented on how these were achieved so no information on coordination and delivery of rehabilitation or social care. |
| Khan, S. K., Weusten, A., Bonczek, S., Tate, A., Port, A., The Best Practice Tariff helps improve management of neck of femur fractures: A completed audit loop, British Journal of Hospital Medicine, 74, 644–647, 2013 [PubMed: 24220529] | Population not in PICO: Inclusion criteria includes pathological hip fractures. Results not presented separately for target population. |
| Kiel, S., Zimak, C., Chenot, J. F., Schmidt, C. O., Evaluation of an ambulatory geriatric rehabilitation program - results of a matched cohort study based on claims data, BMC geriatrics, 20, 30, 2020 [PMC free article: PMC6990495] [PubMed: 31996158] | Study design not in PICO: Case-control design |
| Kind, A., Polnaszek, B., Hovanes, M., Smith, M., Designation of a clinician for post-hospital follow-up care and 30-day rehospitalizations in patients discharged to nursing homes and rehabilitation facilities, Journal of the American Geriatrics Society, 61, S16, 2013 | Published as abstract only |
| Koo, W. W. H., Hip care clinic: Improving osteoporosis treatment after a hip fracture, Osteoporosis International, 25, 609, 2014 | Published as abstract only |
| Kooijmans, H., Post, M. W. M., Stam, H. J., van der Woude, L. H. V., Spijkerman, D. C. M., Snoek, G. J., Bongers-Janssen, H. M. H., van Koppenhagen, C. F., Twisk, J. W., Bussmann, J. B. J., Effectiveness of a Self-Management Intervention to Promote an Active Lifestyle in Persons With Long-Term Spinal Cord Injury: The HABITS Randomized Clinical Trial, Neurorehabilitation and Neural Repair, 31, 991–1004, 2017 [PubMed: 29256337] | Intervention not in PICO: Self-management intervention designed to increase physical activity in chronic SCI. No mention of coordination or delivery of rehabilitation or social care. |
| Krulova, A., Vackova, J., Svestkova, O., Community-based rehabilitation system for people with acquired brain injury in the Czech Republic (from the point of view of occupational therapist), Brain Injury, 31, 852–853, 2017 | Published as abstract only |
| Kurowski, Brad G., Taylor, H. Gerry, McNally, Kelly A., Kirkwood, Michael W., Cassedy, Amy, Horn, Paul S., Stancin, Terry, Wade, Shari L., Online Family Problem-Solving Therapy (F-PST) for Executive and Behavioral Dysfunction After Traumatic Brain Injury in Adolescents: A Randomized, Multicenter, Comparative Effectiveness Clinical Trial, The Journal of head trauma rehabilitation, 2019 [PMC free article: PMC7205575] [PubMed: 31834062] | Outcomes not in PICO: Behaviour Rating Inventory of Executive Function, Global Executive Composite, Behaviour Regulation Index, Metacognition Index and Strengths and Difficulties Questionnaire |
| Kusen, J. Q., Schafroth, B., Poblete, B., van der Vet, P. C. R., Link, B. C., Wijdicks, F. J. G., Babst, R. H., Beeres, F. J. P., The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: an observational study, Archives of Orthopaedic and Trauma Surgery, 139, 1705–1712, 2019 [PubMed: 31309288] | Intervention not in PICO: Not concerned with the coordination of rehabilitation services for trauma patients between inpatient and outpatient services. Included in review concerning coordination for inpatient services. |
| Lamb, Laura C., Montgomery, Stephanie C., Wong Won, Brian, Harder, Siobhan, Meter, Jeffrey, Feeney, James M., A multidisciplinary approach to improve the quality of care for patients with fragility fractures, Journal of orthopaedics, 14, 247–251, 2017 [PMC free article: PMC5362133] [PubMed: 28367005] | Intervention not in PICO: Not concerned with the coordination of rehabilitation services for trauma patients between inpatient and outpatient services. Included in review concerning coordination for inpatient services. |
| Lannin, Natasha, Carr, Belinda, Allaous, Jeanine, Mackenzie, Bronwyn, Falcon, Alex, Tate, Robyn, A randomized controlled trial of the effectiveness of handheld computers for improving everyday memory functioning in patients with memory impairments after acquired brain injury, Clinical Rehabilitation, 28, 470–81, 2014 [PubMed: 24452701] | Comparison not in PICO: Electronic vs non-electronic memory aid after discharge |
| Lathbury, K., The road ahead-managing a spinal cord injury, The Case manager, 11, 55–7, 2000 [PubMed: 11935641] | Narrative review |
| Latz, David, Bergermann, Anja, Jungnitsch, Jeannie, Grassmann, Jan Peter, Schiffner, Erik, Gahr, Britta, Tank, Anne, Windolf, Joachim, Ritz-Timme, Stefanie, Gras, Lilly, Jungbluth, Pascal, Characterisation of Victims Of Violence in the A & E Department and Analysis of the Acceptance of a Medico-Legal Expertise Centre After its Implementation vs. Multi-Year Consolidation, Charakterisierung unfallchirurgischer Gewaltopfer und Erfassung der Inanspruchnahme nach Implementierung und mehrjahriger Etablierung einer rechtsmedizinischen Gewaltopferambulanz., 157, 426–433, 2019 [PubMed: 30481835] | Population not in PICO: People presenting to A&E without admission |
| Lau, T. W., Leung, F., Siu, D., Wong, G., Luk, K. D. K., Geriatric hip fracture clinical pathway: The Hong Kong experience, Osteoporosis International, 21, S627–S636, 2010 [PMC free article: PMC2974932] [PubMed: 21058003] | No information presented on historical comparison group, including number of participants |
| Laver, Kate, Lannin, Natasha A., Bragge, Peter, Hunter, Peter, Holland, Anne E., Tavender, Emma, O’Connor, Denise, Khan, Fary, Teasell, Robert, Gruen, Russell, Organising health care services for people with an acquired brain injury: an overview of systematic reviews and randomised controlled trials, BMC health services research, 14, 397, 2014 [PMC free article: PMC4263199] [PubMed: 25228157] | Systematic review: Included studies checked for relevance. |
| Leal, J., Gray, A. M., Hawley, S., Prieto-Alhambra, D., Delmestri, A., Arden, N. K., Cooper, C., Javaid, M. K., Judge, A., Cost-Effectiveness of Orthogeriatric and Fracture Liaison Service Models of Care for Hip Fracture Patients: A Population-Based Study, Journal of Bone and Mineral Research, 32, 203–211, 2017 [PMC free article: PMC5321497] [PubMed: 27632945] | Outcomes not in PICO: 30 day mortality, 1 year mortality, risk of 2nd fracture and assorted intervention cost measures |
| Leclercq, M. M., For the return at home: Mobil teams brain-injury, Annals of Physical and Rehabilitation Medicine, 57, e411, 2014 | Published as abstract only |
| Lee, John C., Horst, Michael, Rogers, Amelia, Rogers, Frederick B., Wu, Daniel, Evans, Tracy, Edavettal, Mathew, Checklist-styled daily sign-out rounds improve hospital throughput in a major trauma center, The American surgeon, 80, 434–40, 2014 [PubMed: 24887721] | Intervention not in PICO: Checklist designed to coordinate medical care of trauma patients rather than coordination or delivery of rehabilitation or social care |
| Lee, S. Y., Amatya, B., Judson, R., Truesdale, M., Reinhardt, J. D., Uddin, T., Xiong, X. H., Khan, F., Clinical practice guidelines for rehabilitation in traumatic brain injury: a critical appraisal, Brain Injury, 33, 1263–1271, 2019 [PubMed: 31314607] | Review of guidelines. References checked for possible included studies - none were identified. |
| Lems, W. F., Dreinhofer, K. E., Bischoff-Ferrari, H., Blauth, M., Czerwinski, E., Da Silva, J., Herrera, A., Hoffmeyer, P., Kvien, T., Maalouf, G., Marsh, D., Puget, J., Puhl, W., Poor, G., Rasch, L., Roux, C., Schuler, S., Seriolo, B., Tarantino, U., Van Geel, T., Woolf, A., Wyers, C., Geusens, P., EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures, Annals of the Rheumatic Diseases, 76, 802–810, 2017 [PubMed: 28007756] | Systematic review: Included studies checked for relevance. |
| Leung, Andraay Hon-Chi, Lam, Tsz-Ping, Cheung, Wing-Hoi, Chan, Tan, Sze, Pan-Ching, Lau, Thomas, Leung, Kwok-Sui, An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study, The Journal of trauma, 71, 1390–4, 2011 [PubMed: 22002614] | Intervention not in PICO: Orthogeriatric Collaborative Programme consisting of geriatric reviews. Aim was to optimise patient condition for surgery and to address previously undiagnosed medical problems. |
| Li, L., Dai, J. X., Xu, L., Huang, Z. X., Pan, Q., Zhang, X., Jiang, M. Y., Chen, Z. H., The effect of a rehabilitation nursing intervention model on improving the comprehensive health status of patients with hand burns, Burns, 43, 877–885, 2017 [PubMed: 28062082] | Intervention not in PICO: Nursing intervention involving elements of occupational therapy and psychological treatment rather than interventions comparing the coordination and/or delivery of rehabilitation or social services |
| Lin, Francis O. Y., Luk, James K. H., Chan, T. C., Mok, Winnie W. Y., Chan, Felix H. W., Effectiveness of a discharge planning and community support programme in preventing readmission of high-risk older patients, Hong Kong medical journal = Xianggang yi xue za zhi, 21, 208–16, 2015 [PubMed: 25904292] | Population not in PICO: Home-dwelling older patients aged >60 years admitted to the general medical wards. Only 10% admitted through falls, results not presented separately for target population. |
| Lin, L., Wade, C., Comprehensive prevention and management of pressure ulcers in an acute inpatient rehabilitation facility: An evidence ebased assessment, PM and R, 8, S182–S183, 2016 [PubMed: 27672832] | Published as abstract only |
| Lin, P. C., Wang, C. H., Chen, C. S., Liao, L. P., Kao, S. F., Wu, H. F., To evaluate the effectiveness of a discharge-planning programme for hip fracture patients, Journal of Clinical Nursing, 18, 1632–1639, 2009 [PubMed: 19490299] | Population not in PICO: Patients ≥ 18 years old |
| Linden, M., Hawley, C., Blackwood, B., Evans, J., Anderson, V., O’Rourke, C., Technological aids for the rehabilitation of memory and executive functioning in children and adolescents with acquired brain injury, Cochrane Database of Systematic Reviews, 2016 [PMC free article: PMC6457968] [PubMed: 27364851] | Systematic review: Included studies checked for relevance. |
| Ling, Shi-Neng James, Kleimeyer, Christopher, Lynch, Genni, Burmeister, Elizabeth, Kennedy, Diana, Bell, Kate, Watkins, Leith, Cooke, Cameron, Can geriatric hip fractures be managed effectively within a level 1 trauma center?, Journal of Orthopaedic Trauma, 29, 160–4, 2015 [PubMed: 25699541] | Intervention not in PICO: Coordination of acute management of hip fracture, rather than rehabilitation. |
| Lisk, R., Krasuski, M., Watters, H., Parsons, C., Yeong, K., 12 months impact of an orthopaedic early supportive discharge (OSD) team in our hip fracture service, European Geriatric Medicine, 6, S150, 2015 [PMC free article: PMC6334156] [PubMed: 30958784] | Published as abstract only |
| Liu, Vincent X., Rosas, Efren, Hwang, Judith, Cain, Eric, Foss-Durant, Anne, Clopp, Molly, Huang, Mengfei, Lee, Derrick C., Mustille, Alex, Kipnis, Patricia, Parodi, Stephen, Enhanced Recovery After Surgery Program Implementation in 2 Surgical Populations in an Integrated Health Care Delivery System, JAMA Surgery, 152, e171032, 2017 [PMC free article: PMC5568841] [PubMed: 28492816] | Intervention not in PICO: Enhanced recovery after surgery programme designed to impact peri-operative management and does not include rehabilitation or social care. |
| Lloyd-James, Lucy, Facing reality: discharge challenges after neuro-rehabilitation, Paediatric nursing, 18, 28, 2006 [PubMed: 16881499] | Narrative review |
| Lohse, Grant R., Leopold, Seth S., Theiler, Susan, Sayre, Cindy, Cizik, Amy, Lee, Michael J., Systems-based safety intervention: reducing falls with injury and total falls on an orthopaedic ward, The Journal of bone and joint surgery. American volume, 94, 1217–22, 2012 [PubMed: 22760390] | Population not in PICO: Mixture of traumatic and non-traumatic with results not reported separately for target population |
| Losh, Joseph, Duncan, Thomas K., Diaz, Graal, Lee, HyeSun, Romero, Javier, Multidisciplinary Patient Management Improves Mortality in Geriatric Trauma Patients, The American surgeon, 85, 230–233, 2019 [PubMed: 30819305] | Intervention not in PICO: Multidisciplinary medical trauma care, not rehabilitation |
| Lumba-Brown, A., Yeates, K. O., Sarmiento, K., Breiding, M. J., Haegerich, T. M., Gioia, G. A., Turner, M., Benzel, E. C., Suskauer, S. J., Giza, C. C., Joseph, M., Broomand, C., Weissman, B., Gordon, W., Wright, D. W., Moser, R. S., McAvoy, K., Ewing-Cobbs, L., Duhaime, A. C., Putukian, M., Holshouser, B., Paulk, D., Wade, S. L., Herring, S. A., Halstead, M., Keenan, H. T., Choe, M., Christian, C. W., Guskiewicz, K., Raksin, P. B., Gregory, A., Mucha, A., Taylor, H. G., Callahan, J. M., Dewitt, J., Collins, M. W., Kirkwood, M. W., Ragheb, J., Ellenbogen, R. G., Spinks, T. J., Ganiats, T. G., Sabelhaus, L. J., Altenhofen, K., Hoffman, R., Getchius, T., Gronseth, G., Donnell, Z., O’Connor, R. E., Timmons, S. D., Diagnosis and Management of Mild Traumatic Brain Injury in Children: A Systematic Review, JAMA Pediatrics, 172, 2018 [PubMed: 30193325] | Systematic review: Included studies checked for relevance.. |
| Mackey, Patricia A., Rosenthal, Laura D., Mi, Lanyu, Whitaker, Michael D., Subsequent Fracture Prevention in Patients 50 Years and Older With Fragility Fractures: A Quality Improvement Initiative, Journal for healthcare quality : official publication of the National Association for Healthcare Quality, 41, 17–22, 2019 [PubMed: 29553966] | Intervention not in PICO: Osteoporosis education, screening and treatment. |
| Malec, J. F., Eicher, V., Murphy, M. P., Murphy, T. F., Progress assessed with the mayo-portland adaptability inventory through the client outcome system for 604 participants in four types of postacute brain injury rehabilitation programs, Brain Impairment, 12, 68, 2011 | Published as abstract only |
| Malec, J., Eicher, V., Murphy, M. P., Murphy, T., Progress in four postacute brain rehabilitation program types compared through the MPAI-4 outcome info system, Archives of Physical Medicine and Rehabilitation, 92, 1698, 2011 | Published as abstract only |
| Mallick, Emad, Gulihar, Abhinav, Taylor, Grahame, Furlong, Andrew, Pandey, Radhakant, Impact of organisational changes on fracture neck of femur management, Annals of the Royal College of Surgeons of England, 93, 61–6, 2011 [PMC free article: PMC3293276] [PubMed: 20955664] | Intervention not in PICO: Project group aimed at changing surgical and medical management of hip fracture. No mention of rehabilitation. |
| Man, D. W., Soong, W. Y., Tam, S. F., Hui-Chan, C. W., Self-efficacy outcomes of people with brain injury in cognitive skill training using different types of trainer-trainee interaction, Brain Injury, 20, 959–970, 2006 [PubMed: 17062427] | Population not in PICO: Only 16/103 patients within PICO with results not reported separately for the target population. |
| Mangram, Alicia J., Shifflette, Vanessa K., Mitchell, Christopher D., Johnson, Van A., Lorenzo, Manuel, Truitt, Micheal S., Goel, Anuj, Lyons, Mark, Dunn, Ernest L., The creation of a geriatric trauma unit “G-60”, The American surgeon, 77, 1144–6, 2011 [PubMed: 21944622] | Study design not in PICO: Non-randomised study with less than N=100 in 1 arm (n=150 in intervention group, n=78 in control group) |
| Massey, T., Smith, S., Bezzina, C., Ball, A., Specialist rehabilitation in a major trauma centre: It’s not just about saving lives, Brain Injury, 28, 655, 2014 | Published as abstract only |
| Mayo-Wilson, Evan, Grant, Sean, Burton, Jennifer, Parsons, Amanda, Underhill, Kristen, Montgomery, Paul, Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis, PLoS ONE, 9, e89257, 2014 [PMC free article: PMC3951196] [PubMed: 24622676] | Systematic review: Included studies checked for relevance. |
| McMartin, K., Discharge planning in chronic conditions: An evidence-based analysis, Ontario Health Technology Assessment Series, 13, 1–72, 2013 [PMC free article: PMC3804053] [PubMed: 24167538] | Systematic review: Included studies checked for relevance. |
| Meaney, Mark, Divided loyalties in a brain injury case, The Case manager, 14, 30–72, 2003 [PubMed: 12649687] | Case report |
| Miller, Megan W., Emeny, Rebecca T., Freed, Gary L., Reduction of Hospital-acquired Pressure Injuries Using a Multidisciplinary Team Approach: A Descriptive Study, Wounds : a compendium of clinical research and practice, 31, 108–113, 2019 [PMC free article: PMC6586476] [PubMed: 30802207] | Population not in PICO: Hospital-wide implementation, with no separation of trauma and non-trauma patients |
| Mittal, Chikul, Lee, Hsien Chieh Daniel, Goh, Kiat Sern, Lau, Cheng Kiang Adrian, Tay, Leeanna, Siau, Chuin, Loh, Yik Hin, Goh, Teck Kheng Edward, Sandi, Chit Lwin, Lee, Chien Earn, ValuedCare program: a population health model for the delivery of evidence-based care across care continuum for hip fracture patients in Eastern Singapore, Journal of orthopaedic surgery and research, 13, 129, 2018 [PMC free article: PMC5977502] [PubMed: 29848378] | Intervention not in PICO: ValuedCare involved delivery of pre- and post-operative hip fracture care. No mention of delivery or coordination of rehabilitation or social care |
| Momosaki, Ryo, Kakuda, Wataru, Yamada, Naoki, Abo, Masahiro, Impact of board-certificated physiatrists on rehabilitation outcomes in elderly patients after hip fracture: An observational study using the Japan Rehabilitation Database, Geriatrics & gerontology international, 16, 963–8, 2016 [PubMed: 26311043] | Intervention not in PICO: Not concerned with the coordination of rehabilitation services for trauma patients between inpatient and outpatient services. Included in review concerning coordination for inpatient services. |
| Morris, D. S., Reilly, P., Rohrbach, J., Telford, G., Kim, P., Sims, C. A., The influence of unit-based nurse practitioners on hospital outcomes and readmission rates for patients with trauma, Journal of Trauma and Acute Care Surgery, 73, 474–478, 2012 [PubMed: 22846959] | Intervention not in PICO: Unit-based nurse practitioners are involved in delivering acute trauma care, not delivery and coordination of rehabilitation or social care |
| Murphy, R. P., Reddin, C., Murphy, E. P., Waters, R., Murphy, C. G., Canavan, M., Key Service Improvements After the Introduction of an Integrated Orthogeriatric Service, Geriatric Orthopaedic Surgery and Rehabilitation, 10, 2019 [PMC free article: PMC6906332] [PubMed: 31853381] | Intervention not in PICO: Integrated orthogeriatric service designed to streamline pre- and post-operative care for hip fracture. No mention of delivery or coordination of rehabilitation or social care |
| Naeem, F., Rodriguez, S., MacRae, A., Implementation of an analgesia and bowels protocol to improve patient care after hip fracture, Age and Ageing, 48, 2019 | Published as abstract only |
| Naglie, Gary, Tansey, Catherine, Kirkland, James L., Ogilvie-Harris, Darryl J., Detsky, Allan S., Etchells, Edward, Tomlinson, George, O’Rourke, Keith, Goldlist, Barry, Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial, CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 167, 25–32, 2002 [PMC free article: PMC116636] [PubMed: 12137074] | Study years not in PICO: 1993-1997 |
| Nakase-Richardson, Risa, Stevens, Lillian Flores, Tang, Xinyu, Lamberty, Greg J., Sherer, Mark, Walker, William C., Pugh, Mary Jo, Eapen, Blessen C., Finn, Jacob A., Saylors, Mimi, Dillahunt-Aspillaga, Christina, Adams, Rachel Sayko, Garofano, Jeffrey S., Comparison of the VA and NIDILRR TBI Model System Cohorts, The Journal of Head Trauma Rehabilitation, 32, 221–233, 2017 [PubMed: 28678118] | Comparison not in PICO: Comparison between population characteristics of 2 databases contributing to Traumatic Brain Injury Model System |
| Niemeijer, Gerard C., Flikweert, Elvira, Trip, Albert, Does, Ronald J. M. M., Ahaus, Kees T. B., Boot, Anja F., Wendt, Klaus W., The usefulness of lean six sigma to the development of a clinical pathway for hip fractures, Journal of Evaluation in Clinical Practice, 19, 909–14, 2013 [PubMed: 22780308] | Intervention not in PICO: Lean Six Sigma aimed at decreasing the length of stay in hospital rather than coordinating or delivering rehabilitation |
| Nizamoglu, Metin, O’Connor, Edmund Fitzgerald, Bache, Sarah, Theodorakopoulou, Evgenia, Sen, Sankhya, Sherren, Peter, Barnes, David, Dziewulski, Peter, The impact of major trauma network triage systems on patients with major burns, Burns : journal of the International Society for Burn Injuries, 42, 1662–1670, 2016 [PubMed: 27810131] | Study design not in PICO: Non-RCT with less than 100 per arm |
| Noticewala, M. S., Swart, E., Shah, R. P., Macaulay, W., Geller, J. A., First Place Award Multidisciplinary care of the hip fracture patient: A case control analysis of differing treatment protocols, Current Orthopaedic Practice, 27, 346–350, 2016 | Intervention not in PICO: Multi-disciplinary team delivering acute inpatient hip fracture care, with no mention of delivery or coordination of rehabilitation or social care |
| O’Keefe, Sophie, Stanley, Mandy, Adam, Kerry, Lannin, Natasha A., A Systematic Scoping Review of Work Interventions for Hospitalised Adults with an Acquired Neurological Impairment, Journal of Occupational Rehabilitation, 29, 569–584, 2019 [PubMed: 30515620] | Systematic review: Included studies checked for relevance. |
| Olenginski, T. P., Maloney-Saxon, G., Matzko, C. K., Mackiewicz, K., Kirchner, H. L., Bengier, A., Newman, E. D., High-risk osteoporosis clinic (HiROC): improving osteoporosis and postfracture care with an organized, programmatic approach, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 26, 801–10, 2015 [PubMed: 25398432] | Study design not in PICO: No comparison group. |
| O’Malley, Natasha T., Blauth, Michael, Suhm, Norbert, Kates, Stephen L., Hip fracture management, before and beyond surgery and medication: a synthesis of the evidence, Archives of orthopaedic and trauma surgery, 131, 1519–27, 2011 [PubMed: 21706188] | Systematic review: Included studies checked for relevance. |
| O’Mara, Michael Shaymus, Ramaniuk, Aliaksandr, Graymire, Vickie, Rozzell, Monica, Martin, Stacey, Lean methodology for performance improvement in the trauma discharge process, The journal of trauma and acute care surgery, 77, 137–142, 2014 [PubMed: 24977768] | Comparison not in PICO: Trauma vs non-trauma wards |
| O’Neil, Jennifer, van Ierssel, Jacquie, Sveistrup, Heidi, Remote supervision of rehabilitation interventions for survivors of moderate or severe traumatic brain injury: A scoping review, Journal of telemedicine and telecare, 1357633X19845466, 2019 [PubMed: 31148489] | Systematic review: Included studies checked for relevance. |
| Parsons, M., Parsons, J., Pillai, A., Rouse, P., Mathieson, S., Bregmen, R., Smith, C., Kenealy, T., Post-Acute Care for Older People Following Injury: A Randomized Controlled Trial, Journal of the American Medical Directors Association, 2019 [PubMed: 31629646] | Population not in PICO: Patients ≥ 18 years old |
| Parsons, Matthew, Parsons, John, Pillai, Avinesh, Rouse, Paul, Mathieson, Sean, Bregmen, Rochelle, Smith, Christine, Kenealy, Tim, Post-Acute Care for Older People Following Injury: A Randomized Controlled Trial, Journal of the American Medical Directors Association, 21, 404–409.e1, 2020 [PubMed: 31629646] | Duplicate |
| Patrick, P. D., Allaire, J. H., Hostler, S. L., A pediatric brain injury program: Families are catalysts for change, SAGGI - Child Development and Disabilities, 29, 31–39, 2003 | Article not available |
| Perez Santamaria, M., Dominguez Arevalo, M. J., Manso Perez Cossio, J., Peraza Sanchez, M., Outcomes of a multidisciplinary approach for the management of hip fractures in older patients. Experience in a regional hospital, Osteoporosis International, 27, S419, 2016 | Published as abstract only |
| Pfeifer, M., Dionyssiotis, Y., Musculoskeletal Rehabilitation after Hip Fracture: A Review, Osteologie, 28, 183–191, 2019 | Systematic review: Included studies checked for relevance. |
| Pfeifer, M., Minne, H. W., Musculoskeletal rehabilitation after hip fracture: A review, Archives of Osteoporosis, 5, 49–59, 2010 | Systematic review: Included studies checked for relevance. |
| Phillips, V. L., Vesmarovich, S., Hauber, R., Wiggers, E., Egner, A., Telehealth: reaching out to newly injured spinal cord patients, Public health reports (Washington, D.C. : 1974), 116 Suppl 1, 94–102, 2001 [PMC free article: PMC1913671] [PubMed: 11889278] | Study dates not in PICO: 1998-August/September 2000. Results not presented separately for the period in PICO (January-August/September 2000) |
| Pils, K., Vavrovsky, G., Meisner, W., Schreiber, W., Bohmer, F., Improvement of rehabilitation outcomes of hip fractures: discharge assessment by patient care team, case management and wound healing]. [German, Wiener klinische wochenschrift, 112, 413–419, 2000 [PubMed: 10849953] | Article in German |
| Pioli, G., Pellicciotti, F., Davoli, M. L., Pignedoli, P., Sabetta, E., Ferrari, A., Hip fracture management and outcomes in Italy, European Geriatric Medicine, 1, 104–107, 2010 | Narrative description of hip fracture care model. No presentation of data |
| Pope, Sue, Vickerstaff, A. L., Wareham, A. P., Lessons learned from early rehabilitation of complex trauma at the Royal Centre for Defence Medicine, Journal of the Royal Army Medical Corps, 163, 124–131, 2017 [PubMed: 27412360] | Narrative description of Royal Centre for Defence Medicine rehabilitation model. No presentation of study data. |
| Powell, J., Heslin, J., Greenwood, R., Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial, Journal of neurology, neurosurgery, and psychiatry, 72, 193–202, 2002 [PMC free article: PMC1737759] [PubMed: 11796769] | Study dates not in PICO: Pre-2000 |
| Powell, Janet M., Fraser, Robert, Brockway, Jo Ann, Temkin, Nancy, Bell, Kathleen R., A Telehealth Approach to Caregiver Self-Management Following Traumatic Brain Injury: A Randomized Controlled Trial, The Journal of head trauma rehabilitation, 31, 180–90, 2016 [PubMed: 26394294] | Intervention not in PICO: Education for caregivers of people with traumatic brain injury |
| Prestmo, A., Sletvold, O., Thingstad, P., Taraldsen, K., Johnsen, L. G., Helbostad, J., Saltvedt, I., Outcomes of activities of daily living, cognition and mobility in the Trondheim Hip Fracture Trial. A randomized controlled trial, European Geriatric Medicine, 3, S56, 2012 | Published as abstract only |
| Proudfoot, Suzanne, Bennett, Brandon, Duff, Simon, Palmer, Julie, Implementation and effects of Enhanced Recovery After Surgery for hip and knee replacements and fractured neck of femur in New Zealand orthopaedic services, The New Zealand medical journal, 130, 77–90, 2017 [PubMed: 28494480] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Multi-component intervention with only 1 of 5 sections focused on discharge planning. Other areas targeted by the intervention was within the ambulance, pre-operative care, peri-operative care and post-operative care. |
| Prvu Bettger, Janet A., Stineman, Margaret G., Effectiveness of multidisciplinary rehabilitation services in postacute care: state-of-the-science. A review, Archives of physical medicine and rehabilitation, 88, 1526–34, 2007 [PMC free article: PMC4309994] [PubMed: 17964900] | Systematic review: Included studies checked for relevance. |
| Rae-Grant, Alex D., Turner, Aaron P., Sloan, Alicia, Miller, Deborah, Hunziker, James, Haselkorn, Jodie K., Self-management in neurological disorders: systematic review of the literature and potential interventions in multiple sclerosis care, Journal of rehabilitation research and development, 48, 1087–100, 2011 [PubMed: 22234713] | Systematic review: Included studies checked for relevance. |
| Rapidi, C. A., Tederko, P., Moslavac, S., Popa, D., Branco, C. A., Kiekens, C., Varela Donoso, E., Christodoulou, N., Evidence-based position paper on Physical and Rehabilitation Medicine (PRM) professional practice for persons with spinal cord injury. The European PRM position (UEMS PRM Section), European Journal of Physical and Rehabilitation Medicine, 54, 797–807, 2018 [PubMed: 29952157] | Systematic review: Included studies checked for relevance. |
| Reguant, F., Arnau, A., Lorente, J. V., Maestro, L., Bosch, J., Efficacy of a multidisciplinary approach on post-operative morbidity and mortality of elderly patients with hip fracture, Journal of Clinical Anesthesia, 53, 11–19, 2019 [PubMed: 30286380] | Intervention not in PICO: MDT intervention designed to optimise patient health before hip fracture surgery, rather than rehabilitation. |
| Reinhardt, J., Chen, S., Gosney, J., Hu, X., Li, J., Liu, S., Zhang, X., Effectiveness of a comprehensive rehabilitation services program on long-term physical functioning in injured survivors of the 2008 sichuan earthquake, PM and R, 4, S300, 2012 | Published as abstract only |
| Rezaei, Mojtaba, Sharifi, Amirsina, Vaccaro, Alexander Richard, Rahimi-Movaghar, Vafa, Home-Based Rehabilitation Programs: Promising Field to Maximize Function of Patients with Traumatic Spinal Cord Injury, Asian journal of neurosurgery, 14, 634–640, 2019 [PMC free article: PMC6703054] [PubMed: 31497079] | Systematic review: Included studies checked for relevance. |
| Robalino, S., Nyakang’o, S. B., Beyer, F., Fox, C., Allan, L. M., Effectiveness of interventions aimed at improving physical and psychological outcomes of fall-related injuries in people with dementia a systematic review, Age and Ageing, 47, 2018 [PMC free article: PMC5819703] [PubMed: 29463292] | Published as abstract only |
| Robles, L., Slogoff, M., Ladwig-Scott, E., Zank, D., Larson, M. K., Aranha, G., Shoup, M., The addition of a nurse practitioner to an inpatient surgical team results in improved use of resources, Surgery, 150, 711–717, 2011 [PubMed: 22000183] | Population not in PICO: Surgical and colorectal patients with no distinction between trauma and non-trauma surgical patients. |
| Roels, E. H., Aertgeerts, B., Ramaekers, D., Peers, K., Hospital- and community-based interventions enhancing (re)employment for people with spinal cord injury: a systematic review, Spinal cord, 54, 2–7, 2016 [PubMed: 26305872] | Systematic review: Included studies checked for relevance. |
| Rosario, Emily R., Espinoza, Laura, Kaplan, Stephanie, Khonsari, Sepehr, Thurndyke, Earl, Bustos, Melissa, Vickers, Kayla, Navarro, Brittney, Scudder, Bonnie, Patient navigation for traumatic brain injury promotes community re-integration and reduces re-hospitalizations, Brain Injury, 31, 1340–1347, 2017 [PubMed: 28650255] | Study design not in PICO: Non-RCT with less than 100 per arm. |
| Rothman, E. F., Cohort study: Violent reinjury and mortality highlights the need for a comprehensive care approach to youth presenting for assault-related injury, Evidence-Based Medicine, 20, 112, 2015 [PubMed: 25827138] | Setting not in PICO: Emergency department |
| Ruggiero, C., Zampi, E., Baroni, M., Mecocci, P., Rinonapoli, G., Caraffa, A., Conti, F., Brandi, M. L., The fracture unit to bridge the osteoporosis care gap in Italy, Osteoporosis International, 25, S365, 2014 | Published as abstract only |
| Ryan, T., Enderby, P., Rigby, A. S., A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age, Clinical Rehabilitation, 20, 123–131, 2006 [PubMed: 16541932] | Population not in PICO: Patients ≥ 18 years old |
| Ryan, T., Enderby, P., Rigby, A. S., A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age: results at 12-month followup, International journal on disability and human development, 5, 83–89, 2006 [PubMed: 16541932] | Population not in PICO: Patients ≥ 18 years old |
| Rypkema, G., Adang, E., Dicke, H., Naber, T., De Swart, B., Disselhorst, L., Goluke-Willemse, G., Rikkert, M. O., Cost-effectiveness of an interdisciplinary intervention in geriatric inpatients to prevent malnutrition, Journal of Nutrition, Health and Aging, 8, 122–127, 2004 [PubMed: 14978608] | Unclear population: All non-terminally ill geriatric patients admitted for more than 2 days. Study does not report reason for admission. |
| Rytter, H. M., Westenbaek, K., Henriksen, H., Christiansen, P., Humle, F., Specialized interdisciplinary rehabilitation reduces persistent post-concussive symptoms: a randomized clinical trial, Brain Injury, 33, 266–281, 2019 [PubMed: 30500267] | Population not in PICO: People in the general population with post-concussive syndrome. Attended A&E but not admitted. |
| Saha, Sumit, DiRusso, Stephen M., Welle, Scott, Lieberman, Benjamin, Sender, Joel, Shabsigh, Ridwan, Baltazar, Gerard A., Integration of Geriatrician Consultation for Trauma Admissions May Benefit Patient Outcomes, Gerontology & geriatric medicine, 5, 2333721419858735, 2019 [PMC free article: PMC6589989] [PubMed: 31259206] | Intervention not in PICO: Geriatrician consultation for trauma patients upon admission to trauma centre if above 65 years old. No mention of coordination or delivery of rehabilitation. |
| Saltvedt, Ingvild, Prestmo, Anders, Einarsen, Elin, Johnsen, Lars Gunnar, Helbostad, Jorunn L., Sletvold, Olav, Development and delivery of patient treatment in the Trondheim Hip Fracture Trial. A new geriatric in-hospital pathway for elderly patients with hip fracture, BMC research notes, 5, 355, 2012 [PMC free article: PMC3463430] [PubMed: 22800378] | No study results presented in paper |
| Sander, Beate, Elliot-Gibson, Victoria, Beaton, Dorcas E., Bogoch, Earl R., Maetzel, Andreas, A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs, The Journal of bone and joint surgery. American volume, 90, 1197–205, 2008 [PubMed: 18519311] | Intervention not in PICO: Coordination of osteoporosis treatment after fragility fracture |
| Savage, R., Camejo, M., Kramer, S., Jeanne Lozada, A., McAllister, T., Mensah, N., Romanelli, L., Sanchez, L., Schneider, L., Donohue, P., Does multidisciplinary and intense rehabilitation in a post-acute brain injury school produce positive outcomes?, Journal of Head Trauma Rehabilitation, 32, E87, 2017 | Published as abstract only |
| Sayer, J., Quality improvement-fracture liaison service development, Osteoporosis International, 27, S557, 2016 | Published as abstract only |
| Schneider, Kathryn J., Leddy, John J., Guskiewicz, Kevin M., Seifert, Tad, McCrea, Michael, Silverberg, Noah D., Feddermann-Demont, Nina, Iverson, Grant L., Hayden, Alix, Makdissi, Michael, Rest and treatment/rehabilitation following sport-related concussion: a systematic review, British journal of sports medicine, 51, 930–934, 2017 [PubMed: 28341726] | Systematic review: Included studies checked for relevance. |
| Semerano, Luca, Guillot, Xavier, Rossini, Maurizio, Avice, Evelyne, Begue, Thierry, Wargon, Mathias, Boissier, Marie-Christophe, Saidenberg-Kermanac’h, Nathalie, What predicts initiation of osteoporosis treatment after fractures: education organisation or patients’ characteristics?, Clinical and Experimental Rheumatology, 29, 89–92, 2011 [PubMed: 21345297] | Intervention not in PICO: Patient osteoporosis education and organisation of osteoporosis care |
| Sen, A., Xiao, Y., Lee, S. A., Dutton, R., Scalea, T., Multidisciplinary discharge rounds may reduce ED overcrowding by facilitating hospital throughput, Academic Emergency Medicine, 17, S98–S99, 2010 | Published as abstract only |
| Serghiou, Michael A., Holmes, Christina L., McCauley, Robert L., A survey of current rehabilitation trends for burn injuries to the head and neck, The Journal of burn care & rehabilitation, 25, 514–8, 2004 [PubMed: 15534463] | Study design not in PICO: Survey of burn rehabilitation providers (N=100) |
| Shahrokhi, Akram, Azimian, Jalil, Amouzegar, Atousa, Oveisi, Sonia, Effect of Telenursing on Outcomes of Provided Care by Caregivers of Patients With Head Trauma After Discharge, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 25, 21–25, 2018 [PubMed: 29319646] | Intervention not in PICO: Weekly telephone calls to caregivers of people with head injury to discuss health status and possible issues. No mention of rehabilitation. |
| Shahrokhi, Akram, Azimian, Jalil, Amouzegar, Atousa, Oveisi, Sonia, The Effect of Telenursing on Referral Rates of Patients With Head Trauma and Their Family’s Satisfaction After Discharge, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 25, 248–253, 2018 [PubMed: 29985860] | Intervention not in PICO: Checklist teleheath intervention with no questions about rehabilitation |
| Shaw, W., Hong, Q. N., Pransky, G., Loisel, P., A literature review describing the role of return-to-work coordinators in trial programs and interventions designed to prevent workplace disability, Journal of Occupational Rehabilitation, 18, 2–15, 2008 [PubMed: 18080827] | Systematic review: Included studies checked for relevance. |
| Shepperd, S., Lannin, N. A., Clemson, L. M., McCluskey, A., Cameron, I. D., Barras, S. L., Discharge planning from hospital to home, Cochrane Database of Systematic Reviews, 2013, CD000313, 2013 [PubMed: 23440778] | Systematic review: Included studies checked for relevance. |
| Shingleton, S. K., Salinas, R. D., Aden, J. K., Berry, P. A., Palmer, C. R., Russe, C. S., Trichel, R. M., Melvin, J. J., King, B. T., Wound care team effectiveness on patient care efficiency and quality, Journal of Burn Care and Research, 37, S74, 2016 | Published as abstract only |
| Shyu, Y. I. L., Liang, J., Wu, C. C., Su, J. Y., Cheng, H. S., Chou, S. W., Chen, M. C., Yang, C. T., Interdisciplinary intervention for hip fracture in older Taiwanese: Benefits last for 1 year, Journals of Gerontology - Series A Biological Sciences and Medical Sciences, 63, 92–97, 2008 [PubMed: 18245766] | Follow-up data from Shyu 2005 study, which is excluded |
| Shyu, Y. I., Liang, J., Wu, C. C., Su, J. Y., Cheng, H. S., Chou, S. W., Yang, C. T., A pilot investigation of the short-term effects of an interdisciplinary intervention program on elderly patients with hip fracture in Taiwan, Journal of the American Geriatrics Society, 53, 811–818, 2005 [PubMed: 15877556] | Intervention/comparison not in PICO: Multidisciplinary rehabilitation program consisting of systemic interdisciplinary involvement, geriatric assessment, in-patient and in-home rehabilitation and discharge planning versus standard care that differed on most of these components, not just the coordination/delivery components |
| Siefferman, J., Ambrose, A. F., Lin, E., Improving patient handoff for acute rehabilitation admission, PM and R, 3, S320, 2011 | Published as abstract only |
| Singh, Nalin A., Quine, Susan, Clemson, Lindy M., Williams, Elodie J., Williamson, Dominique A., Stavrinos, Theodora M., Grady, Jodie N., Perry, Tania J., Lloyd, Bradley D., Smith, Emma U. R., Singh, Maria A. Fiatarone, Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial, Journal of the American Medical Directors Association, 13, 24–30, 2012 [PubMed: 21944168] | Intervention not in PICO: High intensity progressive resistance training |
| Singler, K., Biber, R., Wicklein, S., Heppner, H. J., Sieber, C. C., Bail, H. J., “N-active”: A new comanaged, orthogeriatric ward: Observations and prospects, Zeitschrift fur Gerontologie und Geriatrie, 44, 2011 [PubMed: 22159830] | Narrative description of implementation of orthogeriatric ward. Only data presented is non-comparative. |
| Soong, Christine, Cram, Peter, Chezar, Ksenia, Tajammal, Faiqa, Exconde, Kathleen, Matelski, John, Sinha, Samir K., Abrams, Howard B., Fan-Lun, Christopher, Fabbruzzo-Cota, Christina, Backstein, David, Bell, Chaim M., Impact of an Integrated Hip Fracture Inpatient Program on Length of Stay and Costs, Journal of Orthopaedic Trauma, 30, 647–652, 2016 [PubMed: 27875490] | Population not in PICO: Patients ≥ 18 years old |
| Spiliotopoulou, Georgia, Atwal, Anita, Is occupational therapy practice for older adults with lower limb amputations evidence-based? A systematic review, Prosthetics and orthotics international, 36, 7–14, 2012 [PubMed: 22089164] | Systematic review: Included studies checked for relevance. |
| Stenvall, Michael, Olofsson, Birgitta, Nyberg, Lars, Lundstrom, Maria, Gustafson, Yngve, Improved performance in activities of daily living and mobility after a multidisciplinary post-operative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up, Journal of rehabilitation medicine, 39, 232–8, 2007 [PubMed: 17468792] | Population not in PICO: Patients ≥ 18 years old |
| Stubbs, Kendra E., Sikes, Lindsay, Interdisciplinary Approach to Fall Prevention in a High-Risk Inpatient Pediatric Population: Quality Improvement Project, Physical therapy, 97, 97–104, 2017 [PubMed: 27340197] | Outcome not in PICO - Fall rates |
| Talevski, Jason, Sanders, Kerrie M., Duque, Gustavo, Connaughton, Catherine, Beauchamp, Alison, Green, Darci, Millar, Lynne, Brennan-Olsen, Sharon L., Effect of Clinical Care Pathways on Quality of Life and Physical Function After Fragility Fracture: A Meta-analysis, Journal of the American Medical Directors Association, 20, 926.e1–926.e11, 2019 [PubMed: 30975586] | Systematic review. Included studies checked for relevance. Stenvall 2007 was identified as a relevant study and has been included. |
| Tan, T., Molina, J. D., Lim, Y., Dharmawan, A., Teo, A., Soon, M., Frailty ready inpatient care-interim findings from an integrated, comprehensive geriatric programme, Journal of the American Geriatrics Society, 67, S92–S93, 2019 | Published as abstract only |
| Taraldsen, K., Sletvold, O., Thingstad, P., Saltvedt, I., Granat, M. H., Lydersen, S., Helbostad, J. L., Physical behavior and function early after hip fracture surgery in patients receiving comprehensive geriatric care or orthopedic care-a randomized controlled trial, Journals of gerontology. Series A, Biological sciences and medical sciences, 69, 338–345, 2014 [PubMed: 23902933] | Intervention not in PICO: Comprehensive geriatric care with an element of discharge planning and early mobilisation but focus appears to be on short-term post-operative outcomes with treatment of co-morbidities and acute care rather than delivery or coordination of rehabilitation or social care. |
| Torres, Audrey, Kunishige, Nalani, Morimoto, Denise, Hanzawa, Tracie, Ebesu, Mike, Fernandez, John, Nohara, Lynne, SanAgustin, Eliseo, Borg, Stephanie, Shared governance: a way to improve the care in an inpatient rehabilitation facility, Rehabilitation nursing : the official journal of the Association of Rehabilitation Nurses, 40, 69–73, 2015 [PubMed: 24729092] | Outcomes not in PICO: Mentions improved patient outcomes but no presentation of data |
| Tran, V., Lam, M. K., Amon, K. L., Brunner, M., Hines, M., Penman, M., Lowe, R., Togher, L., Interdisciplinary eHealth for the care of people living with traumatic brain injury: A systematic review, Brain Injury, 31, 1701–1710, 2017 [PubMed: 29064300] | Systematic review: Included studies checked for relevance. |
| Tricco, Andrea C., Thomas, Sonia M., Veroniki, Areti Angeliki, Hamid, Jemila S., Cogo, Elise, Strifler, Lisa, Khan, Paul A., Robson, Reid, Sibley, Kathryn M., MacDonald, Heather, Riva, John J., Thavorn, Kednapa, Wilson, Charlotte, Holroyd-Leduc, Jayna, Kerr, Gillian D., Feldman, Fabio, Majumdar, Sumit R., Jaglal, Susan B., Hui, Wing, Straus, Sharon E., Comparisons of Interventions for Preventing Falls in Older Adults: A Systematic Review and Meta-analysis, JAMA, 318, 1687–1699, 2017 [PMC free article: PMC5818787] [PubMed: 29114830] | Systematic review: Included studies checked for relevance. |
| Truchon, C., Moore, L., Belcaid, A., Clement, J., Trudelle, N., Ulysse, M. A., Grolleau, B., Clusiau, J., Levesque, D., De Guise, M., Shaping quality through vision, structure, and monitoring of performance and quality indicators: Impact story from the Quebec trauma network, International Journal of Technology Assessment in Health Care, 33, 415–419, 2017 [PubMed: 28578738] | Narrative description of Quebec Trauma Network and its set-up. No data presented apart from brief mention of mortality data. |
| Tseng, M. Y., Liang, J., Wang, J. S., Yang, C. T., Wu, C. C., Cheng, H. S., Chen, C. Y., Lin, Y. E., Wang, W. S., Shyu, Y. I. L., Effects of a diabetes-specific care model for hip fractured older patients with diabetes: A randomized controlled trial, Experimental Gerontology, 126, 110689, 2019 [PubMed: 31404623] | Comparison not in PICO: Groups received different treatment rather than same rehabilitation delivered or coordinated in different ways. Both groups received standard rehabilitation while inpatients but the intervention group also received in-home rehabilitation for 4 months after hospital discharge and diabetes-specific education and rehabilitation for up to 12 months after hospital discharge. |
| Tung, James Y., Stead, Brent, Mann, William, Ba’Pham,, Popovic, Milos R., Assistive technologies for self-managed pressure ulcer prevention in spinal cord injury: a scoping review, Journal of Rehabilitation Research and Development, 52, 131–46, 2015 [PubMed: 26237111] | Scoping review: Included studies checked for relevance. |
| Turner, Benjamin J., Fleming, Jennifer M., Ownsworth, Tamara L., Cornwell, Petrea L., The transition from hospital to home for individuals with acquired brain injury: A literature review and research recommendations, Disability and rehabilitation, 30, 1153–1176, 2008 [PubMed: 17852241] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, L., Disler, P. B., Nair, A., Wade, D. T., Multi-disciplinary rehabilitation for acquired brain injury in adults of working age, The Cochrane database of systematic reviews, CD004170, 2005 [PubMed: 16034923] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, Lynne, Evidence for the effectiveness of multi-disciplinary rehabilitation following acquired brain injury: a synthesis of two systematic approaches, Journal of rehabilitation medicine, 40, 691–701, 2008 [PubMed: 18843419] | Systematic review: Included studies checked for relevance. |
| Turner-Stokes, Lynne, Pick, Anton, Nair, Ajoy, Disler, Peter B., Wade, Derick T., Multi-disciplinary rehabilitation for acquired brain injury in adults of working age, The Cochrane database of systematic reviews, CD004170, 2015 [PMC free article: PMC8629646] [PubMed: 26694853] | Systematic review: Included studies checked for relevance. |
| Vaughn, S. L., King, A., A survey of state programs to finance rehabilitation and community services for individuals with brain injury, The Journal of head trauma rehabilitation, 16, 20–33, 2001 [PubMed: 11277848] | Study design not in PICO: Survey of state-funded programs for persons with traumatic brain injury. |
| Vidan, Maite, Serra, Jose A., Moreno, Concepcion, Riquelme, Gerardo, Ortiz, Javier, Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial, Journal of the American Geriatrics Society, 53, 1476–82, 2005 [PubMed: 16137275] | Study dates not in PICO: 1997 |
| Vikane, E., Hellstrom, T., Roe, C., Bautz-Holter, E., Assmus, J., Skouen, J. S., Efficacy of a multidisciplinary outpatient treatment for patients with mild traumatic brain injury: A randomized controlled intervention trial, Brain Injury, 30, 617, 2016 [PubMed: 28296510] | Published as abstract only |
| Vikane, E., Hellstrom, T., Roe, C., Bautz-Holter, E., Assmus, J., Skouen, J. S., Multidisciplinary outpatient treatment in patients with mild traumatic brain injury: A randomised controlled intervention study, Brain Injury, 31, 475–484, 2017 [PubMed: 28296510] | Population not in PICO: Patients ≥ 18 years old |
| Ward, D., Drahota, A., Gal, D., Severs, M., Dean, T. P., Care home versus hospital and own home environments for rehabilitation of older people, Cochrane Database of Systematic Reviews, 2008 [PMC free article: PMC6991934] [PubMed: 18843641] | Systematic review: Included studies checked for relevance. |
| Webster, J., Kim, J. H., Hawley, C., Barbir, L., Barton, S., Young, C., Development, implementation, and outcomes of a residential vocational rehabilitation program for injured Service members and Veterans, Journal of Vocational Rehabilitation, 48, 111–126, 2018 | Study design not in PICO: No comparison group |
| Wegener, Stephen T., Mackenzie, Ellen J., Ephraim, Patti, Ehde, Dawn, Williams, Rhonda, Self-management improves outcomes in persons with limb loss, Archives of Physical Medicine and Rehabilitation, 90, 373–80, 2009 [PubMed: 19254599] | Population not in PICO: Mixed population with <40% in PICO and results not reported separately for target population |
| Wiechman, Shelley A., Carrougher, Gretchen J., Esselman, Peter C., Klein, Matthew B., Martinez, Erin M., Engrav, Loren H., Gibran, Nicole S., An expanded delivery model for outpatient burn rehabilitation, Journal of burn care & research : official publication of the American Burn Association, 36, 14–22, 2015 [PubMed: 25198101] | Population not in PICO: Patients ≥ 18 years old |
| Westgard, T., Ottenvall Hammar, I., Holmgren, E., Ehrenberg, A., Wisten, A., Ekdahl, A. W., Dahlin-Ivanoff, S., Wilhelmson, K., Comprehensive geriatric assessment pilot of a randomized control study in a Swedish acute hospital: A feasibility study, Pilot and Feasibility Studies, 4, 41, 2018 [PMC free article: PMC5789623] [PubMed: 29423259] | Unclear population: Frail adults over 75 years who required an acute hospital admission. No information presented on traumatic or non-trauma causes. |
| Wiechman, S. A., Carrougher, G. J., Esselman, P. C., Angere, D., Klein, M. B., Gibran, N. S., A randomized controlled trial to test an expanded delivery model for patients with burn injuries, Journal of burn care & research, 35, S79-, 2014 | Published as abstract only |
| Winograd, A., Squirrell, T., Winters, B., The promise of progress: Co-ordinating interdisciplinary neuro-restorative care transitions, Brain Injury, 28, 775–776, 2014 | Published as abstract only |
| Wu, Jane, Faux, Steven G., Harris, Ian, Poulos, Christopher J., Integration of trauma and rehabilitation services is the answer to more cost-effective care, ANZ journal of surgery, 86, 900–904, 2016 [PubMed: 26631277] | Comparison not in PICO: Delivery of rehabilitation in the trauma admission hospital versus rehabilitation in an external rehabilitation service. No details reported about what rehabilitation the patients received in either facility (and no data on any coordination or delivery aspects of the rehabilitation). |
| Young, T., Andreas, N., Howard-Brown, C., Enhancing early engagement for transitions to community, Brain Impairment, 20, 374–375, 2019 | Published as abstract only |
| Zatzick, D. F., Roy-Byrne, P., Russo, J. E., Rivara, F. P., Koike, A., Jurkovich, G. J., Katon, W., Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial, General Hospital Psychiatry, 23, 114–23, 2001 [PubMed: 11427243] | Intervention and comparison not in PICO: Collaborative care intervention consisting of counselling, consultation with surgical and primary care providers and attempted post-discharge coordination versus standard care that differed on all these components, not just the coordination/delivery components. Unclear if study period (years) within PICO |
| Zatzick, D., Russo, J., Thomas, P., Darnell, D., Teter, H., Ingraham, L., Whiteside, L. K., Wang, J., Guiney, R., Parker, L., Sandgren, K., Hedrick, M. K., Van Eaton, E. G., Jurkovich, G., Patient-Centered Care Transitions After Injury Hospitalization: A Comparative Effectiveness Trial, Psychiatry (New York), 81, 141–157, 2018 [PubMed: 29533154] | Population not in PICO: Patients had to be admitted to an inpatient surgical ward or emergency department for at least 24 hours i.e. not all admitted to hospital. Results are not presented separately. |
| Zhang, Ming, Effect of HBM Rehabilitation Exercises on Depression, Anxiety and Health Belief in Elderly Patients with Osteoporotic Fracture, Psychiatria Danubina, 29, 466–472, 2017 [PubMed: 29197204] | Outcomes not in PICO : Anxiety, depression, osteoporosis knowledge, and osteoporosis health belief |
| Zhang, Xia, Reinhardt, Jan D., Gosney, James E., Li, Jianan, The NHV rehabilitation services program improves long-term physical functioning in survivors of the 2008 Sichuan earthquake: a longitudinal quasi experiment, PLoS ONE, 8, e53995, 2013 [PMC free article: PMC3538750] [PubMed: 23308293] | Intervention and comparison not in PICO: NHV is a complete rehabilitation programme (consisting of NGOs, health department and volunteers) implemented after the Sichuan earthquake. Comparisons are early-NHV, late-NHV, no NHV. |
| Zhao, Y. R., Liang, X., Yang, T. Y., Liu, Y., Prospective case-control study on comprehensive treatment for elderly hip fractures, Zhongguo gu shang [China journal of orthopaedics and traumatology], 27, 570–574, 2014 [PubMed: 25338443] | Article in Chinese |
| Zidén, L., Frändin, K., Kreuter, M., Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities, Clinical Rehabilitation, 22, 1019–1033, 2008 [PubMed: 19052241] | Intervention and comparison not in PICO: Multidisciplinary geriatric rehabilitation home program focused on supported discharge, independence in daily activities, and enhancing physical activity versus standard care with no structured rehabilitation after discharge. Interventions differed on most of these components, not just the coordination/delivery components |
| Ziden, Lena, Frandin, Kerstin, Kreuter, Margareta, Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities, Clinical Rehabilitation, 22, 1019–1033, 2008 [PubMed: 19052241] | Duplicate |
Qualitative clinical studies
Table 43Excluded qualitative studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Abrahamson, Vanessa, Jensen, Jan, Springett, Kate, Sakel, Mohamed, Experiences of patients with traumatic brain injury and their carers during transition from in-patient rehabilitation to the community: a qualitative study, Disability and rehabilitation, 39, 1683–1694, 2017 [PubMed: 27557977] | No qualitative data on phenomena of interest. |
| Adams, Deana, Dahdah, Marie, Coping and adaptive strategies of traumatic brain injury survivors and primary caregivers, NeuroRehabilitation, 39, 223–37, 2016 [PubMed: 27372358] | Study not conducted in one of the countries included in the review protocol. |
| Adams, R. D. F., Cole, E., Brundage, S. I., Morrison, Z., Jansen, J. O., Beliefs and expectations of rural hospital practitioners towards a developing trauma system: A qualitative case study, Injury, 49, 1070–1078, 2018 [PubMed: 29602489] | No qualitative data on phenomena of interest. |
| Aitken, Leanne M., Chaboyer, Wendy, Jeffrey, Carol, Martin, Bronte, Whitty, Jennifer A., Schuetz, Michael, Richmond, Therese S., Indicators of injury recovery identified by patients, family members and clinicians, Injury, 47, 2655–2663, 2016 [PubMed: 27793327] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Albrecht, Jennifer S., O’Hara, Lyndsay M., Moser, Kara A., Mullins, C. Daniel, Rao, Vani, Perception of Barriers to the Diagnosis and Receipt of Treatment for Neuropsychiatric Disturbances After Traumatic Brain Injury, Archives of Physical Medicine and Rehabilitation, 98, 2548–2552, 2017 [PMC free article: PMC6935532] [PubMed: 28688786] | Study not conducted in one of the countries included in the review protocol. |
| Alston, Margaret, Jones, Jennifer, Curtin, Michael, Alston, Bartky Blais Bourdieu Bourdieu Brookshire Butler Callaway Connell Cunningham Curtin Degeneffe Fine Foucault Graham Gwyn Howes Jones Kirkness Lupton Mukherjee O’Rance Ponsford Rees Reichard Reidpath Shildrick Slewa-Younan, Women and traumatic brain injury: “It’s not visible damage”, Australian Social Work, 65, 39–53, 2012 | No qualitative data on phenomena of interest. |
| Ammons, L. L., Harraghy, R. L., Medlin, H. J., Faku, C. T., Shupp, J. W., Flanagan, K. E., Jeng, J. C., Fidler, P., Sava, J. A., Jordan, M. H., Assessing the utility of nurse-driven post-discharge telephone calls, Journal of Burn Care and Research, 32, S153, 2011 | Conference abstract |
| Andersson, Kerstin, Bellon, Michelle, Walker, Ruth, Parents’ experiences of their child’s return to school following acquired brain injury (ABI): A systematic review of qualitative studies, Brain Injury, 30, 829–38, 2016 [PubMed: 27057776] | No findings or themes related to phenomena of interest. Included studies were checked for relevance. |
| Angel, Sanne, Kirkevold, Marit, Pedersen, Birthe D., Rehabilitation after spinal cord injury and the influence of the professional’s support (or lack thereof), Journal of Clinical Nursing, 20, 1713–22, 2011 [PubMed: 21323775] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehab following discharge. |
| Arbour-Nicitopoulos, K. P., Lamontagne, M. E., Tomasone, J., Pila, E., Cumming, I., Latimer-Cheung, A. E., Routhier, F., Why do I stick to the program? a qualitative analysis of the determinants of adherence to community-based physical activity support programs by persons with SCI and contrast with general population with disabilities, Journal of Spinal Cord Medicine, 37, 626, 2014 | Conference abstract. |
| Armstrong, E., Missing voices: Aboriginal stories of stroke and traumatic brain injury, International Journal of Stroke, 12, 14, 2017 | Conference abstract. |
| Armstrong, Elizabeth, Coffin, Juli, Hersh, Deborah, Katzenellenbogen, Judith M., Thompson, Sandra C., Ciccone, Natalie, Flicker, Leon, Woods, Deborah, Hayward, Colleen, Dowell, Catelyn, McAllister, Meaghan, “You felt like a prisoner in your own self, trapped”: the experiences of Aboriginal people with acquired communication disorders, Disability and Rehabilitation, 1–14, 2019 [PubMed: 31692386] | The majority of participants had not experienced traumatic injury and the results not reported separately for the target population. |
| Armstrong, Elizabeth, Coffin, Juli, McAllister, Meaghan, Hersh, Deborah, Katzenellenbogen, Judith M., Thompson, Sandra C., Ciccone, Natalie, Flicker, Leon, Cross, Natasha, Arabi, Linda, Woods, Deborah, Hayward, Colleen, Alway, Armstrong Armstrong Baxter Blackmer Bohanna Bronfenbrenner Chase Coffin Creswell Elder Feigin Foster Gauld Gauthier Hines Jamieson Katzenellenbogen Katzenellenbogen Katzenellenbogen Keightley Kelly Kelly Lakhani Lewis Linton McDonald McKenna O’Reilly Olver Ponsford Rutland-Brown Salas Sandelowski Taylor Togher, ‘I’ve got to row the boat on my own, more or less’: Aboriginal Australian experiences of traumatic brain injury, Brain Impairment, 20, 120–136, 2019 | No qualitative data on phenomena of interest. |
| Arshad, Sira N., Gaskell, Sarah L., Baker, Charlotte, Ellis, Nicola, Potts, Jennie, Coucill, Theresa, Ryan, Lynn, Smith, Jan, Nixon, Anna, Greaves, Kate, Monk, Rebecca, Shelmerdine, Teresa, Leach, Alison, Shah, Mamta, Measuring the impact of a burns school reintegration programme on the time taken to return to school: A multi-disciplinary team intervention for children returning to school after a significant burn injury, Burns : journal of the International Society for Burn Injuries, 41, 727–34, 2015 [PubMed: 25535118] | No qualitative data on phenomena of interest. |
| Ayer, Lynsay, Farris, Coreen, Farmer, Carrie M., Geyer, Lily, Barnes-Proby, Dionne, Ryan, Gery W., Skrabala, Lauren, Scharf, Deborah M., Care Transitions to and from the National Intrepid Center of Excellence (NICoE) for Service Members with Traumatic Brain Injury, Rand health quarterly, 5, 12, 2015 [PMC free article: PMC5158292] [PubMed: 28083388] | Study not conducted in one of the countries included in the review protocol. |
| Badger, Karen, Royse, David, Adult burn survivors’ views of peer support: a qualitative study, Social Work in Health Care, 49, 299–313, 2010 [PubMed: 20379901] | Study not conducted in one of the countries included in the review protocol. |
| Balcazar, Fabricio E., Kelly, Erin Hayes, Keys, Christopher B., Balfanz-Vertiz, Kristin, Albrecht, Alston Balcazar Balcazar Block Boschen Burnett Cressy Devlieger Devlieger Dijkers Dijkers Engstrom Gill Groce Haskell Hayes Hernandez Hernandez Hibbard Jackson Kroll Ljungberg McDonald McKinley Ostrander Richards Rovinsky Sable Servan Sherman Veith Waters Waters Waters Whiteneck Wilson Wilson, Using peer mentoring to support the rehabilitation of individuals with violently acquired spinal cord injuries, Journal of Applied Rehabilitation Counseling, 42, 3–11, 2011 | Study not conducted in one of the countries included in the review protocol. |
| Barclay, Linda, Lalor, Aislinn, Migliorini, Christine, Robins, Lauren, A comparative examination of models of service delivery intended to support community integration in the immediate period following inpatient rehabilitation for spinal cord injury, Spinal Cord, 2019 [PubMed: 31827256] | Population not in PICO: People >18 years old. |
| Barclay, Linda, McDonald, Rachael, Lentin, Primrose, Social and community participation following spinal cord injury: a critical review, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 38, 1–19, 2015 [PubMed: 25305008] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Barclay, Linda, McDonald, Rachael, Lentin, Primrose, Bourke-Taylor, Helen, Facilitators and barriers to social and community participation following spinal cord injury, Australian occupational therapy journal, 63, 19–28, 2016 [PubMed: 26530379] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Beaton, Angela, O’Leary, Katrina, Thorburn, Julie, Campbell, Alaina, Christey, Grant, Improving patient experience and outcomes following serious injury, The New Zealand medical journal, 132, 15–25, 2019 [PubMed: 31048821] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Beckett, K., Earthy, S., Sleney, J., Barnes, J., Kellezi, B., Barker, M., Clarkson, J., Coffey, F., Elder, G., Kendrick, D., Providing effective trauma care: The potential for service provider views to enhance the quality of care (qualitative study nested within a multicentre longitudinal quantitative study), BMJ Open, 4, e005668, 2014 [PMC free article: PMC4091464] [PubMed: 25005598] | No qualitative data on phenomena of interest. |
| Bergmark, Lisa, Westgren, Ninni, Asaba, Eric, Returning to work after spinal cord injury: exploring young adults’ early expectations and experience, Disability and Rehabilitation, 33, 2553–8, 2011 [PubMed: 21592045] | Study did not examine rehabilitation while an inpatient, when transferring to community, or seeking to access rehabilitation following discharge. |
| Bernet, Madeleine, Sommerhalder, Kathrin, Mischke, Claudia, Hahn, Sabine, Wyss, Adrian, “Theory Does Not Get You From Bed to Wheelchair”: A Qualitative Study on Patients’ Views of an Education Program in Spinal Cord Injury Rehabilitation, Rehabilitation nursing : the official journal of the Association of Rehabilitation Nurses, 44, 247–253, 2019 [PubMed: 29889696] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Bernhoff, K., Bjorck, M., Larsson, J., Jangland, E., Patient Experiences of Life Years After Severe Civilian Lower Extremity Trauma With Vascular Injury, European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery, 52, 690–695, 2016 [PubMed: 27637376] | No qualitative data on phenomena of interest. |
| Biester, Rosette C., Krych, Dave, Schmidt, M. J., Parrott, Devan, Katz, Douglas I., Abate, Melissa, Hirshson, Chari I., Individuals With Traumatic Brain Injury and Their Significant Others’ Perceptions of Information Given About the Nature and Possible Consequences of Brain Injury: Analysis of a National Survey, Professional case management, 21, 22–4, 2016 [PubMed: 26618266] | Study not conducted in one of the countries included in the review protocol. |
| Body, Richard, Muskett, Tom, Perkins, Mick, Parker, Mark, Your injury, my accident: talking at cross-purposes in rehabilitation after traumatic brain injury, Brain Injury, 27, 1356–63, 2013 [PubMed: 24070204] | No qualitative data on phenomena of interest. |
| Boschen, K., Gerber, G., Gargaro, J., Comparison of outcomes and costs of 2 publicly-funded community-based models of acquired brain injury services, Archives of Physical Medicine and Rehabilitation, 91, e59, 2010 | Conference abstract. |
| Bourge, C., Body Image (BI) of acquired spinal cord injury (SCI) persons. Which patient care in an internal unit of physical and neurological rehabilitation. Experience of the patient care in an internal and neurological unit of PMR of the University Hospital of Liege, Annals of Physical and Rehabilitation Medicine, 59 (Supplement), e128, 2016 | No qualitative data on phenomena of interest. |
| Bourke, John A., Nunnerley, Joanne L., Sullivan, Martin, Derrett, Sarah, Relationships and the transition from spinal units to community for people with a first spinal cord injury: A New Zealand qualitative study, Disability and health journal, 12, 257–262, 2019 [PubMed: 30262164] | The focus was not specific to participants who had experienced traumatic injury and the results not reported separately for the target population. |
| Braaf, Sandra, Ameratunga, Shanthi, Nunn, Andrew, Christie, Nicola, Teague, Warwick, Judson, Rodney, Gabbe, Belinda J., Patient-identified information and communication needs in the context of major trauma, BMC health services research, 18, 163, 2018 [PMC free article: PMC5842544] [PubMed: 29514689] | Population not in PICO: People >18 years old. |
| Braaf, Sandra C., Lennox, Alyse, Nunn, Andrew, Gabbe, Belinda J., Experiences of hospital readmission and receiving formal carer services following spinal cord injury: a qualitative study to identify needs, Disability and Rehabilitation, 40, 1893–1899, 2018 [PubMed: 28407725] | Study did not examine phenomena of interest. |
| Brauer, Jennifer, Hay, Catherine Cooper, Francisco, Gerard, A retrospective investigation of occupational therapy services received following a traumatic brain injury, Occupational Therapy in Health Care, 25, 119–30, 2011 [PubMed: 23899029] | Study not conducted in one of the countries included in the review protocol. |
| Brimicombe, L., Ling, J., De Sousa De Abreu, I., Hoffman, K., Salisbury, C., Jefferson, R., Makela, P., Early integration of a self-management support package into usual care following traumatic brain injury (TBI): A feasibility study, British Journal of Neurosurgery, 31, 501, 2017 | Conference abstract. |
| Brito, Sara, White, Jennifer, Thomacos, Nikos, Hill, Bridget, The lived experience following free functioning muscle transfer for management of pan-brachial plexus injury: reflections from a long-term follow-up study, Disability and Rehabilitation, 1–9, 2019 [PubMed: 31574227] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Brockway, J. A., St De Lore, J., Fann, J. R., Hart, T., Hurst, S., Fey-Hinckley, S., Savage, J., Warren, M., Bell, K. R., Telephone-delivered problem-solving training after mild traumatic brain injury: qualitative analysis of service members’ perceptions, Rehabilitation Psychology, 61, 221–230, 2016 [PubMed: 26797117] | Study not conducted in one of the countries included in the review protocol. |
| Brown, F., Sofronoff, K., Whittingham, K., Boyd, R., McKinlay, L., Parenting a child with a traumatic brain injury: A focus group study, Developmental Medicine and Child Neurology, 54, 24–25, 2012 | No qualitative data on phenomena of interest. |
| Brown, Jessica, Hux, Karen, Hey, Morgan, Murphy, Madeline, Ackerman, Aldrich Anderson Arciniegas Bach Beigel Bogdan Brandt Brown Brown Catroppa Cicerone Cicerone Creswell Creswell Cushman de Joode de Joode DePompei Donders Dowds Doyle Edwards Ewing-Cobbs Fortuny Gillette Gillette Gioia Glang Gordon Gordon Grajzel Harper Hart Hawley Helm-Estabrooks Hendricks Hux Kelley Kennedy Kennedy Kertesz Krause Leopold Lincoln Martella Martinez McAllister McCrory Merriam Moustakas Ownsworth Patel Perna Reitan Rumrill Scherer Scherer Scherer Scherer Scherer Scherer Shanahan Sherer Sherer Sohlberg Spreen Starks Tate Todis Togher Vu Wallace Ylvisaker Ylvisaker, Exploring cognitive support use and preference by college students with TBI: A mixed-methods study, NeuroRehabilitation, 41, 483–499, 2017 [PubMed: 28946573] | Study not conducted in one of the countries included in the review protocol. |
| Browne, C., Living with traumatic brain injury: Views of survivors and family members, Brain Injury, 26, 400, 2012 | Conference abstract. |
| Bruner-Canhoto, Laney, Savageau, Judith, Croucher, Deborah, Bradley, Kathryn, Lessons From a Care Management Pilot Program for People With Acquired Brain Injury, Journal for healthcare quality : official publication of the National Association for Healthcare Quality, 38, 255–263, 2016 [PubMed: 26042754] | Study not conducted in one of the countries included in the review protocol. |
| Buck, P., Kirzner, R., Sagrati, J., Laster, R., The challenge of mTBI work: An exploratory study of rehabilitation professionals, Brain Injury, 26, 583–584, 2012 | Conference abstract. |
| Buck, Page Walker, Sagrati, Jocelyn Spencer, Kirzner, Rachel Shapiro, Belson, Bloom Brenner Briggs Brody Buck Chrisman Gaboda Klein Marchione Padgett Patton Schwartz Strauss Thompson, Mild traumatic brain injury: A place for social work, Social Work in Health Care, 52, 741–751, 2013 [PubMed: 24028738] | Study not conducted in one of the countries included in the review protocol. |
| Buddai, S., Di Taranti, L. J., Adenwala, A. Y., Aepli, S., Choudhary, M., George, D. L., Koilor, C. B., Linehan, M., Peifer, H., Rub, D., Kaplan, L., Johnson, N., Lane-Fall, M. B., Characterizing intensive care unit patient and family experiences of recovery after traumatic injury, American Journal of Respiratory and Critical Care Medicine. Conference: American Thoracic Society International Conference, ATS, 195, 2017 | Conference abstract. |
| Buscemi, Valentina, Cassidy, Elizabeth, Kilbride, Cherry, Reynolds, Frances Ann, A qualitative exploration of living with chronic neuropathic pain after spinal cord injury: an Italian perspective, Disability and Rehabilitation, 40, 577–586, 2018 [PubMed: 28054832] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Bushnik, T., Smith, M., Long, C., Supporting factors for follow-up care in TBI patients post-inpatient discharge, Brain Injury, 31 (6–7), 974, 2017 | Conference abstract. |
| Byrnes, Michelle, Beilby, Janet, Ray, Patricia, McLennan, Renee, Ker, John, Schug, Stephan, Patient-focused goal planning process and outcome after spinal cord injury rehabilitation: quantitative and qualitative audit, Clinical Rehabilitation, 26, 1141–9, 2012 [PubMed: 22653375] | No qualitative data on phenomena of interest. |
| Cahow, C., Gassaway, J., Rider, C., Joyce, J. P., Bogenshutz, A., Edens, K., Kreider, S. E. D., Whiteneck, G., Relationship of therapeutic recreation inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: The SCIRehab project, Journal of Spinal Cord Medicine, 35, 547–564, 2012 [PMC free article: PMC3522896] [PubMed: 23318036] | Study not conducted in one of the countries included in the review protocol. |
| Calder, Allyson, Nunnerley, Jo, Mulligan, Hilda, Ahmad Ali, Nordawama, Kensington, Gemma, McVicar, Tim, van Schaik, Olivia, Experiences of persons with spinal cord injury undertaking a physical activity programme as part of the SCIPA ‘Full-On’ randomized controlled trial, Disability and Health Journal, 11, 267–273, 2018 [PubMed: 29089215] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Calleja, Pauline, Aitken, Leanne, Cooke, Marie, Staff perceptions of best practice for information transfer about multitrauma patients on discharge from the emergency department: a focus group study, Journal of Clinical Nursing, 25, 2863–73, 2016 [PubMed: 27453432] | Setting not in PICO: Emergency department. |
| Canto, Angela I., Chesire, David J., Buckley, Valerie A., Andrews, Terrie W., Roehrig, Alysia D., Arroyos-Jurado, Ball Bradley-Klug Brantlinger Braun Chesire Conoley Cook Davies Elliot Ewing-Cobbs Farmer Gioia Glang Glang Glang Gopinath Guba Guskiewicz Havey Hooper Hux Jantz Johnson Lewandowski Meehan Mellard Rosenthal Rutland-Brown Savage Sharp Shaw Shaw Shih Yeates Yeates Ylvisaker, Barriers to meeting the needs of students with traumatic brain injury, Educational Psychology in Practice, 30, 88–103, 2014 | Study not conducted in one of the countries included in the review protocol. |
| Carron, R. M. C., ‘nobody prepared me for this!’ parents’ experiences of seeking help and support with post-brain injury symptoms and changes in children and adolescents with acquired brain injury, Journal of Neurology, Neurosurgery and Psychiatry, 90, A9, 2019 | Conference abstract. |
| Caspari, Synnove, Aasgaard, Trygve, Lohne, Vibeke, Slettebo, Ashild, Naden, Dagfinn, Perspectives of health personnel on how to preserve and promote the patients’ dignity in a rehabilitation context, Journal of Clinical Nursing, 22, 2318–26, 2013 [PubMed: 23651360] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for the target population. |
| Chapple, L. A., Chapman, M., Shalit, N., Udy, A., Deane, A., Williams, L., Barriers to Nutrition Intervention for Patients With a Traumatic Brain Injury: Views and Attitudes of Medical and Nursing Practitioners in the Acute Care Setting, Journal of Parenteral and Enteral Nutrition, 42, 318–326, 2018 [PubMed: 29443400] | Study did not examine phenomena of interest. |
| Chapple, Lee-Anne, Chapman, Marianne, Shalit, Natalie, Udy, Andrew, Deane, Adam, Williams, Lauren, Barriers to Nutrition Intervention for Patients With a Traumatic Brain Injury, JPEN. Journal of parenteral and enteral nutrition, 148607116687498, 2017 [PubMed: 29443400] | Duplicate. |
| Chondronikola, M., Weller, S., Rosenberg, L., Rosenberg, M., Meyer, W. J., Herndon, D. N., Sidossis, L., Variation among clinical specialties in perceptions of pediatric burn patient needs, Journal of Burn Care and Research, 37, S244, 2016 | Conference abstract. |
| Christensen, Jan, Langberg, Henning, Doherty, Patrick, Egerod, Ingrid, Ambivalence in rehabilitation: thematic analysis of the experiences of lower limb amputated veterans, Disability and Rehabilitation, 40, 2553–2560, 2018 [PubMed: 28631501] | Population not in PICO: People >18 years old. |
| Christie, Nicola, Beckett, Kate, Earthy, Sarah, Kellezi, Blerina, Sleney, Jude, Barnes, Jo, Jones, Trevor, Kendrick, Denise, Seeking support after hospitalisation for injury: a nested qualitative study of the role of primary care, The British journal of general practice : the journal of the Royal College of General Practitioners, 66, e24–31, 2016 [PMC free article: PMC4684032] [PubMed: 26639949] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Christiaens, Wendy, Van de Walle, Elke, Devresse, Sophie, Van Halewyck, Dries, Benahmed, Nadia, Paulus, Dominique, Van den Heede, Koen, The view of severely burned patients and healthcare professionals on the blind spots in the aftercare process: a qualitative study, BMC health services research, 15, 302, 2015 [PMC free article: PMC4521491] [PubMed: 26231290] | Population not in PICO: People >18 years old. |
| Christie, Nicola, Braaf, Sandra, Ameratunga, Shanthi, Nunn, Andrew, Jowett, Helen, Gabbe, Belinda, Barclay, Barnes Berkman Boniface Braun Cameron Carpenter Cass Charlson Christie Christie Cox Gabbe Gabbe Kellezi Larsen Levasseur Lyons Marottoli McInnes Pointer Prang Smith Syed Urry Wilson, The role of social networks in supporting the travel needs of people after serious traumatic injury: A nested qualitative study, Journal of Transport & Health, 6, 84–92, 2017 | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Cichon, S., Danford, E. K., Schladen, M. M., Bruner, D., Libin, A., Scholten, J., Integrating opportunities for family involvement into a manualized goal self-management intervention for veterans with mTBI, Archives of Physical Medicine and Rehabilitation, 96, e77, 2015 | Conference abstract. |
| Cocks, Errol, Bulsara, Caroline, O’Callaghan, Annalise, Netto, Julie, Boaden, Ross, Exploring the experiences of people with the dual diagnosis of acquired brain injury and mental illness, Brain Injury, 28, 414–21, 2014 [PubMed: 24475744] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Coffey, Nathan T., Weinstein, Ali A., Cai, Cindy, Cassese, Jimmy, Jones, Rebecca, Shaewitz, Dahlia, Garfinkel, Steven, Identifying and Understanding the Health Information Experiences and Preferences of Individuals With TBI, SCI, and Burn Injuries, Journal of patient experience, 3, 88–95, 2016 [PMC free article: PMC5513647] [PubMed: 28725843] | Study not conducted in one of the countries included in the review protocol. |
| Cogan, A., Treatment model of occupational therapy intervention for service members with chronic symptoms following MTBI, Archives of Physical Medicine and Rehabilitation, 98, e132, 2017 | Conference abstract. |
| Conneeley, A. L., Transitions and brain injury: A qualitative study exploring the journey of people with traumatic brain injury, Brain Impairment, 13, 72–84, 2012 | No qualitative data on phenomena of interest. |
| Conneeley, Anne Louise, Exploring vocation following brain injury: a qualitative enquiry, Social Care and Neurodisability, 4, 6–16, 2013 | No qualitative data on phenomena of interest. |
| Copley, Anna, McAllister, Lindy, Wilson, Linda, Attitride-Stirling, Barnes Brooks Carr-Hill Fagen Foster Frattali Grbich Harradine Harris Honey Humphreys Johnstone Kelly LeFebvre Marsh Minichiello Morse Murphy Muus Nabors Newberry O’Callaghan O’Callaghan O’Callaghan O’Callaghan O’Callaghan Patton Sample Sample Schofield Schwandt Turner-Stokes Whitehead Ylvisaker Youse, We finally learnt to demand: Consumers’ access to rehabilitation following traumatic brain injury, Brain Impairment, 14, 436–449, 2013 | No qualitative data on phenomena of interest. |
| Curtis, Kate, Foster, Kim, Mitchell, Rebecca, Van, Connie, How is care provided for patients with paediatric trauma and their families in Australia? A mixed-method study, Journal of Paediatrics and Child Health, 52, 832–6, 2016 [PubMed: 27203550] | Study did not examine the phenomena of interest. |
| Cuthbert, J., Anderson, J., Mason, C., Block, S., Dettmer, J., Weintraub, A., Harrison-Felix, C., Case management of individuals with chronic TBI: A research-based approach, Journal of Head Trauma Rehabilitation, 28, E49, 2013 | Conference abstract. |
| Daggett, Virginia S., Bakas, Tamilyn, Buelow, Janice, Habermann, Barbara, Murray, Laura L., Needs and concerns of male combat Veterans with mild traumatic brain injury, Journal of Rehabilitation Research and Development, 50, 327–40, 2013 [PubMed: 23881759] | Study not conducted in one of the countries included in the review protocol. |
| Dahl, O., Wickman, M., Wengstrom, Y., Adapting to life after burn injury-reflections on care, Journal of Burn Care and Research, 33, 595–605, 2012 [PubMed: 22210069] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Dalmaso, Kym, Weber, Sarah, Eley, Rob, Spencer, Lyndall, Cabilan, C. J., Nurses’ perceived benefits of trauma nursing rounds (TNR) on clinical practice in an Australian emergency department: a mixed methods study, Australasian emergency nursing journal : AENJ, 18, 42–8, 2015 [PubMed: 25601428] | Setting not in PICO: Emergency department. |
| Dams-O’Connor, K., Landau, A., De Lore, J. S., Hoffman, J., Access, barriers, and health care quality after brain injury: Insiders’ perspectives, Archives of Physical Medicine and Rehabilitation, 97, e129, 2016 | Conference abstract. |
| Dams-O’Connor, Kristen, Landau, Alexandra, Hoffman, Jeanne, St De Lore, Jef, Patient perspectives on quality and access to healthcare after brain injury, Brain Injury, 32, 431–441, 2018 [PubMed: 29388840] | Study not conducted in one of the countries included in the review protocol. |
| Darnell, Doyanne A., Parker, Lea E., Wagner, Amy W., Dunn, Christopher W., Atkins, David C., Dorsey, Shannon, Zatzick, Douglas F., Task-shifting to improve the reach of mental health interventions for trauma patients: findings from a pilot study of trauma nurse training in patient-centered activity scheduling for PTSD and depression, Cognitive behaviour therapy, 48, 482–496, 2019 [PMC free article: PMC6542717] [PubMed: 30499372] | Study not conducted in one of the countries included in the review protocol. |
| D’Cruz, K., Howie, L., Lentin, P., Client-centred practice: Perspectives of persons with a traumatic brain injury, Scandinavian Journal of Occupational Therapy, 23, 30–38, 2016 [PubMed: 26094733] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Dickson, Adele, Ward, Richard, O’Brien, Grainne, Allan, David, O’Carroll, Ronan, Difficulties adjusting to post-discharge life following a spinal cord injury: an interpretative phenomenological analysis, Psychology, health & medicine, 16, 463–74, 2011 [PubMed: 21749243] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Diener, M., Kirby, A., Canary, H., Sumison, F., Green, M., Community reintegration following pediatric acquired brain injury: Perspectives of providers and families, Journal of Head Trauma Rehabilitation, 33 (3), E97, 2018 | Conference abstract. |
| Dillahunt-Aspillaga, C., Bradley, S., Ramaiah, P., Radwan, C., Ottomanelli, L., Coalition Building: A Tool To Implement Evidenced-Based Resource Facilitation in The VHA: Pilot Results, Archives of Physical Medicine and Rehabilitation, 100, e164, 2019 | Conference abstract. |
| Dismann, Patrick D., Maignan, Maxime, Cloves, Paul D., Gutierrez Parres, Blanca, Dickerson, Sara, Eberhardt, Alice, A Review of the Burden of Trauma Pain in Emergency Settings in Europe, Pain and therapy, 7, 179–192, 2018 [PMC free article: PMC6251834] [PubMed: 29860585] | Setting not in PICO: Emergency settings. |
| Divanoglou, A., Georgiou, M., Perceived effectiveness and mechanisms of community peer-based programmes for Spinal Cord Injuries-a systematic review of qualitative findings, Spinal cord, 55, 225–234, 2017 [PubMed: 27845356] | Study did not report any findings related to the phenomena of interest. |
| Doig, E., Fleming, J., Kuipers, P., Cornwell, P., The relationship between goal attainment and the development of self-awareness in traumatic brain injury (TBI) rehabilitation: Descriptive and qualitative case analyses, Brain Impairment, 14, 159–160, 2013 | Conference abstract. |
| Doig, Emmah, Fleming, Jennifer, Cornwell, Petrea, Kuipers, Pim, Comparing the experience of outpatient therapy in home and day hospital settings after traumatic brain injury: patient, significant other and therapist perspectives, Disability and Rehabilitation, 33, 1203–14, 2011 [PubMed: 20977391] | No qualitative data on phenomena of interest. |
| Donnell, Zoe, Hoffman, Roseanne, Myers, Gaya, Sarmiento, Kelly, Seeking to improve care for young patients: Development of tools to support the implementation of the CDC Pediatric mTBI Guideline, Journal of Safety Research, 67, 203–209, 2018 [PMC free article: PMC6445253] [PubMed: 30553425] | Study not conducted in one of the countries included in the review protocol. |
| Donnelly, Kyla Z., Goldberg, Shari, Fournier, Debra, A qualitative study of LoveYourBrain Yoga: a group-based yoga with psychoeducation intervention to facilitate community integration for people with traumatic brain injury and their caregivers, Disability and Rehabilitation, 1–10, 2019 [PubMed: 30741032] | Study not conducted in one of the countries included in the review protocol. |
| Douglas, J., ‘Nobody wants to know you’. Understanding the experience of friendship following severe traumatic brain injury, Brain Injury, 30, 515, 2016 | Conference abstract. |
| Drew, S., Judge, A., Cooper, C., Javaid, M. K., Farmer, A., Gooberman-Hill, R., Secondary prevention of fractures after hip fracture: a qualitative study of effective service delivery, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 27, 1719–27, 2016 [PMC free article: PMC4839047] [PubMed: 26759249] | Study did not examine rehabilitation. |
| Drew, S., Judge, A., Javaid, M. K., Cooper, C., Farmer, A., Goobermen-Hill, R., Secondary prevention of fractures after hip fracture: A qualitative study of effective service delive, Osteoporosis International, 25, S308, 2014 [PMC free article: PMC4839047] [PubMed: 26759249] | Conference abstract. |
| Dwyer, Aoife, Heary, Caroline, Ward, Marcia, MacNeela, Padraig, Adding insult to brain injury: young adults’ experiences of residing in nursing homes following acquired brain injury, Disability and Rehabilitation, 41, 33–43, 2019 [PubMed: 28845724] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Dyke, J., Krupa, J., Vova, J., Medical symptoms, service gaps and barriers to care using the medical home model in adolescents with acquired brain injury, Journal of Head Trauma Rehabilitation, 27 (5), E18–E19, 2012 | Conference abstract. |
| Edworthy Ann, Donne Hannah, The availability and intelligibility of information for carers of children with a brain injury, Social Care and Neurodisability, 1, 32–40, 2010 | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Eliacin, Johanne, Fortney, Sarah, Rattray, Nicholas A., Kean, Jacob, Access to health services for moderate to severe TBI in Indiana: patient and caregiver perspectives, Brain Injury, 32, 1510–1517, 2018 [PubMed: 30036117] | Study not conducted in one of the countries included in the review protocol. |
| Fitts, M., Fleming, J., Bird, K., Condon, T., Gilroy, J., Clough, A., Maruff, P., Esterman, A., Bohanna, I., Sentinel events during hospital admission for indigenous people following traumatic brain injury, Brain Impairment, 19, 336, 2018 | Conference abstract. |
| Fitts, Michelle S., Bird, Katrina, Gilroy, John, Fleming, Jennifer, Clough, Alan R., Esterman, Adrian, Maruff, Paul, Fatima, Yaqoot, Bohanna, India, Abrahamson, Alfandre Amery Bell Blackmer Bohanna Bohanna Bohanna Braun Burnett Choi Claiborne Coronado D’Cruz Dillon Dudley Durey Durey Einsiedel Englander Feigin Foley Franks Gentilello Gilroy Gilroy Harrison Hunt Hyder Jamieson Jayaraj Juillard Katzenellenbogen Katzenellenbogen Lakhani Lee Levack Levack Liossi Marrone Martin Moreton-Robinson Nakata Nalder Nalder Nalder Niemeier Ownsworth Paradies Rutland-Brown Shahid Tuhiwai-Smith Turner Turner Willis Zeiler, A qualitative study on the transition support needs of indigenous Australians following traumatic brain injury, Brain Impairment, 20, 137–159, 2019 | No qualitative data on phenomena of interest. |
| Fleming, Jennifer, Sampson, Jennifer, Cornwell, Petrea, Turner, Ben, Griffin, Janell, Brain injury rehabilitation: The lived experience of inpatients and their family caregivers, Scandinavian journal of occupational therapy, 19, 184–193, 2012 [PubMed: 21936734] | No qualitative data on phenomena of interest. |
| Ford, James H., 2nd, Wise, Meg, Krahn, Dean, Oliver, Karen Anderson, Hall, Carmen, Sayer, Nina, Family care map: Sustaining family-centered care in Polytrauma Rehabilitation Centers, Journal of Rehabilitation Research and Development, 51, 1311–24, 2014 [PMC free article: PMC4560363] [PubMed: 25671632] | Study not conducted in one of the countries included in the review protocol. |
| Foster, Kim, Mitchell, Rebecca, Van, Connie, Young, Alexandra, McCloughen, Andrea, Curtis, Kate, Resilient, recovering, distressed: A longitudinal qualitative study of parent psychosocial trajectories following child critical injury, Injury, 50, 1605–1611, 2019 [PubMed: 31101410] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Foster, Kim, Mitchell, Rebecca, Young, Alexandra, Van, Connie, Curtis, Kate, Parent experiences and psychosocial support needs 6 months following paediatric critical injury: A qualitative study, Injury, 50, 1082–1088, 2019 [PubMed: 30655002] | No qualitative data on phenomena of interest. |
| Foster, Kim, Young, Alexandra, Mitchell, Rebecca, Van, Connie, Curtis, Kate, Experiences and needs of parents of critically injured children during the acute hospital phase: A qualitative investigation, Injury, 48, 114–120, 2017 [PubMed: 27692666] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Fournier, D., Goldberg, S., Figucia, C., Kennedy, P., Krauss, K., Smith, C., Springmann, J., An interdisciplinary traumatic brain injury clinic: Understanding the patient experience, Journal of Head Trauma Rehabilitation, 32, E97–E98, 2017 | Conference abstract. |
| Francis, A., Ziviani, J., Fleming, J., Rae, M., McKinlay, L., Transitioning to adulthood: Needs of young people with an acquired brain injury and those of their families, Neurorehabilitation and Neural Repair, 26, 780–781, 2012 | Conference abstract. |
| Franz, Shiney, Muser, Jurgen, Thielhorn, Ulrike, Wallesch, Claus W., Behrens, Johann, Inter-professional communication and interaction in the neurological rehabilitation team: a literature review, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30457016] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Fraser, M. A., Lind, J. D., Powell-Cope, G., Gavin-Dreschnack, D., Addressing non-direct care, psychosocial concerns of veterans with spinal cord injuries, Journal of Spinal Cord Medicine, 36, 546–547, 2013 | Conference abstract. |
| Freeman, Claire, Cassidy, Bernadette, Hay-Smith, E. Jean C., Beauregard, Beisecker Chan Craig DeSanto-Madeya Dickson Dixon Ell Esmail Esmail Fisher Fronek Gilad Kendall Kennedy Kidd Kreuter Leino-Kilpi Lemonidou New Parrott Racher Rembis Schuster Sinnott Smith Smith Steinglass Taylor Vocaturo, Couple’s experiences of relationship maintenance and intimacy in acute spinal cord injury rehabilitation: An interpretative phenomenological analysis, Sexuality and Disability, 35, 433–444, 2017 | Study did not examine phenomena of interest. |
| Fry, J. C., Price, P., Meeting the re-integration needs of individuals with spinal cord injury: Effectiveness of community-based occupational therapy, Archives of Physical Medicine and Rehabilitation, 94, e8, 2013 | Conference abstract. |
| Gabbe, Belinda J., Sleney, Jude S., Gosling, Cameron M., Wilson, Krystle, Hart, Melissa J., Sutherland, Ann M., Christie, Nicola, Patient perspectives of care in a regionalised trauma system: lessons from the Victorian State Trauma System, The Medical journal of Australia, 198, 149–52, 2013 [PubMed: 23418695] | No qualitative data on phenomena of interest. |
| Gagliardi, Anna R., Nathens, Avery B., Exploring the characteristics of high-performing hospitals that influence trauma triage and transfer, The journal of trauma and acute care surgery, 78, 300–5, 2015 [PubMed: 25757114] | Study did not examine rehabilitation. |
| Gagnon, I., Friedman, D., Management of mild traumatic brain injury or concussion in children: Is there a role for the physical therapist?, Physiotherapy (United Kingdom), 1), eS1487–eS1488, 2011 | Conference abstract. |
| Garrino, Lorenza, Curto, Natascia, Decorte, Rita, Felisi, Nadia, Matta, Ebe, Gregorino, Silvano, Actis, M. Vittoria, Marchisio, Cecilia, Carone, Roberto, Towards personalized care for persons with spinal cord injury: a study on patients’ perceptions, The journal of spinal cord medicine, 34, 67–75, 2011 [PMC free article: PMC3066480] [PubMed: 21528629] | Study did not examine phenomena of interest. |
| Gawel, Marcie, Emerson, Beth, Giuliano, John S., Jr., Rosenberg, Alana, Minges, Karl E., Feder, Shelli, Violano, Pina, Morrell, Patricia, Petersen, Judy, Christison-Lagay, Emily, Auerbach, Marc, A Qualitative Study of Multidisciplinary Providers’ Experiences With the Transfer Process for Injured Children and Ideas for Improvement, Pediatric Emergency Care, 34, 125–131, 2018 [PMC free article: PMC5792311] [PubMed: 29346234] | Study not conducted in one of the countries included in the review protocol. |
| Gemmel, Paul, van Steenis, Thomas, Meijboom, Bert, Bensabat, Bohmer Broekhuis Burke Chase Chase Chase Eisenhardt Fredendall Frei Gronroos Hanne Johnston Lamontagne Lamontagne Larsson Meredith Metters Metters Miles Ouwens Patricio Swanborn Vander Laane Voss Westert Yin Young Zomerdijk, Front-office/back-office configurations and operational performance in complex health services, Brain Injury, 28, 347–356, 2014 [PubMed: 24568302] | Not specific to rehabilitation, or to traumatic injury and results not presented separately for target population. |
| Gill, Carol J., Sander, Angelle M., Robins, Nina, Mazzei, Diana, Struchen, Margaret A., Allen, Aloni Aloni Anderson Anderson-Parente Bergland Brooks Ergh Garden Gillen Gosling Harrick Hibbard Hoofien Jeon Kersel Kravetz Kravetz Kreuter Kreutzer Kreutzer Kreutzer Lippert Marsh Oddy Olver Panting Patton Perlesz Peters Ponsford Porter Resnick Rosenbaum Sandel Siebert Snow Tate Tate Thomsen Vanderploeg Wallace Webster Wells Wood Wood, Exploring experiences of intimacy from the viewpoint of individuals with traumatic brain injury and their partners, The Journal of Head Trauma Rehabilitation, 26, 56–68, 2011 [PubMed: 21209563] | Study not conducted in one of the countries included in the review protocol. |
| Gill, Ian J., Wall, Gemma, Simpson, Jane, Clients’ perspectives of rehabilitation in one acquired brain injury residential rehabilitation unit: a thematic analysis, Brain Injury, 26, 909–20, 2012 [PubMed: 22571407] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Glenny, Christine, Stolee, Paul, Sheiban, Linda, Jaglal, Susan, Communicating during care transitions for older hip fracture patients: family caregiver and health care provider’s perspectives, International journal of integrated care, 13, e044, 2013 [PMC free article: PMC3817953] [PubMed: 24198738] | Population not in PICO: People >18 years old. |
| Glintborg, C., Hansen, T., De La Mata Benites, M., Supporting transitions in neurorehabilitation. A pathway to improved psychosocial outcomes, Brain Injury, 30, 565–566, 2016 | Conference abstract. |
| Glintborg, Chalotte, Hansen, Tia G. B., Bech, Bech Braun Brenner Creswell Ellervik Engel Ghaziani Glintborg Glintborg Glintborg Glintborg Hackett Haggerty Hald Hall Holm Jorge Jorge Keith Kennedy Miles Morton Norholm Pallant Rivera Schlossberg Teasdale Teasdale Turner, Bio-psycho-social effects of a coordinated neurorehabilitation programme: A naturalistic mixed methods study, NeuroRehabilitation, 38, 99–113, 2016 [PubMed: 26889730] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Goel, R., Fruth, S., Geigle, P., Santurri, L., Abzug, J., Telerehabilitation for Individuals With Spinal Cord Injury: Is it Feasible?, Archives of Physical Medicine and Rehabilitation, 100, e203–e204, 2019 | Conference abstract. |
| Goldsmith, Helen, McCloughen, Andrea, Curtis, Kate, Using the trauma patient experience and evaluation of hospital discharge practices to inform practice change: A mixed methods study, Journal of Clinical Nursing, 27, 1589–1598, 2018 [PubMed: 29266578] | Study did not examine rehabilitation. |
| Goldsmith, Helen, McCloughen, Andrea, Curtis, Kate, The experience and understanding of pain management in recently discharged adult trauma patients: A qualitative study, Injury, 49, 110–116, 2018 [PubMed: 28988804] | No qualitative data on phenomena of interest. |
| Goodridge, Donna, Rogers, Marla, Klassen, Laura, Jeffery, Bonnie, Knox, Katherine, Rohatinsky, Noelle, Linassi, Gary, Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas, Disability and Rehabilitation, 37, 1401–10, 2015 [PubMed: 25332089] | No qualitative data on phenomena of interest. |
| Gotlib Conn, Lesley, Zwaiman, Ashley, DasGupta, Tracey, Hales, Brigette, Watamaniuk, Aaron, Nathens, Avery B., Trauma patient discharge and care transition experiences: Identifying opportunities for quality improvement in trauma centres, Injury, 49, 97–103, 2018 [PubMed: 28988066] | No qualitative data on phenomena of interest. |
| Gourdeau, Jenna, Fingold, Alissa, Colantonio, Angela, Mansfield, Elizabeth, Stergiou-Kita, Mary, Workplace accommodations following work-related mild traumatic brain injury: what works?, Disability and Rehabilitation, 1–10, 2018 [PubMed: 30451033] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Graff, Heidi J., Christensen, Ulla, Poulsen, Ingrid, Egerod, Ingrid, Patient perspectives on navigating the field of traumatic brain injury rehabilitation: a qualitative thematic analysis, Disability and Rehabilitation, 40, 926–934, 2018 [PubMed: 28129694] | Population not in PICO: People >18 years old. |
| Gravell, R., Brumfit, S., Body, R., Hope and engagement following acquired brain injury: A qualitative study, Brain Injury, 31, 721–722, 2017 | Conference abstract. |
| Guilcher, S., Everall, A., Wodchis, W., Joanna, deGraaf-Dunlop, Bar-Ziv, S., Kuluski, K., Understanding Transitions of Care in Older Adults With Hip Fractures: A Multiple-Case Study in Ontario, Archives of Physical Medicine and Rehabilitation, 100, e138, 2019 | Conference abstract. |
| Gullick, Janice G., Taggart, Susan B., Johnston, Rae A., Ko, Natalie, The trauma bubble: patient and family experience of serious burn injury, Journal of burn care & research : official publication of the American Burn Association, 35, e413–27, 2014 [PubMed: 25144806] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Guptill, C. A., The lived experience of professional musicians with playing-related injuries: A phenomenological inquiry, Medical Problems of Performing Artists, 26, 84–95, 2011 [PubMed: 21695356] | No qualitative data on phenomena of interest. |
| Haarbauer-Krupa, J., Vova, J., Follow-up of preschool children with acquired brain injury, Brain Injury, 26, 424–425, 2012 | Conference abstract. |
| Haas, B. M., Price, L., Freeman, J. A., Qualitative evaluation of a community peer support service for people with spinal cord injury, Spinal Cord, 51, 295–9, 2013 [PubMed: 23184023] | The majority of participants had not experienced traumatic injury and results not presented separately for target population. |
| Harrington, Rosamund, Foster, Michele, Fleming, Jennifer, Experiences of pathways, outcomes and choice after severe traumatic brain injury under no-fault versus fault-based motor accident insurance, Brain Injury, 29, 1561–71, 2015 [PubMed: 26382715] | No qualitative data on phenomena of interest. |
| Harris, M. B., Rafeedie, S., McArthur, D., Babikian, T., Snyder, A., Polster, D., Giza, C. C., Addition of Occupational Therapy to an Interdisciplinary Concussion Clinic Improves Identification of Functional Impairments, Journal of Head Trauma Rehabilitation, 34, 425–432, 2019 [PubMed: 31688379] | Study not conducted in one of the countries included in the review protocol. |
| Harrison, Anne L., Hunter, Elizabeth G., Thomas, Heather, Bordy, Paige, Stokes, Erin, Kitzman, Patrick, Living with traumatic brain injury in a rural setting: supports and barriers across the continuum of care, Disability and Rehabilitation, 39, 2071–2080, 2017 [PMC free article: PMC5654530] [PubMed: 27549899] | Study not conducted in one of the countries included in the review protocol. |
| Hartley, Naomi A., Spinal cord injury (SCI) rehabilitation: systematic analysis of communication from the biopsychosocial perspective, Disability and rehabilitation, 1–10, 2015 [PubMed: 25801919] | Study not conducted in one of the countries included in the review protocol. |
| Hawkins, Brent L., Crowe, Brandi M., Contextual Facilitators and Barriers of Community Reintegration Among Injured Female Military Veterans: A Qualitative Study, Archives of Physical Medicine and Rehabilitation, 99, S65–S71, 2018 [PubMed: 28866010] | Study not conducted in one of the countries included in the review protocol. |
| Haywood, C., Perceptions of recovery among adolescents and young adults with acquired spinal cord injuries, Archives of Physical Medicine and Rehabilitation, 97, e76, 2016 | Conference abstract. |
| Haywood, Carol, Pyatak, Elizabeth, Leland, Natalie, Henwood, Benjamin, Lawlor, Mary C., A Qualitative Study of Caregiving for Adolescents and Young Adults With Spinal Cord Injuries: Lessons From Lived Experiences, Topics in Spinal Cord Injury Rehabilitation, 25, 281–289, 2019 [PMC free article: PMC6907026] [PubMed: 31844380] | Study not conducted in one of the countries included in the review protocol. |
| Hellem, I., Forland, G., Eide, K., Ytrehus, S., Addressing uncertainty and stigma in social relations related to hidden dysfunctions following acquired brain injury, Scandinavian Journal of Disability Research, 20, 152–161, 2018 | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Herrera-Escobar, J. P., Columbus, A., Castillo-Angeles, M., Rios-Diaz, A. J., Weed, C. N., Kasotakis, G., Velmahos, G. C., Salim, A., Haider, A. H., Kaafara, H. M., Discontinuity of patient-provider communication throughout the phases of care: Time to be more patient-centered in trauma?, Journal of the American College of Surgeons, 225 (4 Supplement 2), e176, 2017 | Conference abstract. |
| Hill, Jennifer N., Smith, Bridget M., Weaver, Frances M., Nazi, Kim M., Thomas, Florian P., Goldstein, Barry, Hogan, Timothy P., Potential of personal health record portals in the care of individuals with spinal cord injuries and disorders: Provider perspectives, The journal of spinal cord medicine, 41, 298–308, 2018 [PMC free article: PMC6055947] [PubMed: 28325112] | Study not conducted in one of the countries included in the review protocol. |
| Hines, M., Brunner, M., Poon, S., Lam, M., Tran, V., Yu, D., Togher, L., Shaw, T., Power, E., Exploring ehealth ‘tribes and tribulations’ in interdisciplinary rehabilitation for people with a traumatic brain injury (TBI), Brain Impairment, 19, 292–293, 2018 | Conference abstract. |
| Hines, M., Brunner, M., Poon, S., Lam, M., Tran, V., Yu, D., Togher, L., Shaw, T., Power, E., Tribes and tribulations: interdisciplinary eHealth in providing services for people with a traumatic brain injury (TBI), BMC health services research, 17, 757, 2017 [PMC free article: PMC5697081] [PubMed: 29162086] | No qualitative data on phenomena of interest. |
| Hirsch, M. A., Grafton, L., Guerrier, T. P., Niemeier, J. P., Newman, M., Runyon, M. S., Unmet concussion care needs from the perspective of individuals with mild traumatic brain injury, Archives of Physical Medicine and Rehabilitation, 96, e33, 2015 | Conference abstract. |
| Hitzig, S., Bain, P., Haycock, S., Hebert, D. A., Evaluation of a spinal cord injury community reintegration outpatient program (CROP) service, Archives of Physical Medicine and Rehabilitation, 95, e83, 2014 [PMC free article: PMC4276116] [PubMed: 25574397] | Conference abstract. |
| Hollick, R., Reid, D., Black, A., McKee, L., What matters to patients: Working together to improve the quality of osteoporosis services, Osteoporosis International, 27, S678, 2016 | Conference abstract. |
| Holloway, Mark, Motivational interviewing and acquired brain injury, Social Care and Neurodisability, 3, 122–130, 2012 | Narrative review. |
| Hoogerdijk, Barbara, Runge, Ulla, Haugboelle, Jette, The adaptation process after traumatic brain injury an individual and ongoing occupational struggle to gain a new identity, Scandinavian Journal of Occupational Therapy, 18, 122–32, 2011 [PubMed: 20384550] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Hoonakker, Peter Leonard Titus, Wooldridge, Abigail Rayburn, Hose, Bat-Zion, Carayon, Pascale, Eithun, Ben, Brazelton, Thomas Berry, 3rd, Kohler, Jonathan Emerson, Ross, Joshua Chud, Rusy, Deborah Ann, Dean, Shannon Mason, Kelly, Michelle Merwood, Gurses, Ayse Pinar, Information flow during pediatric trauma care transitions: things falling through the cracks, Internal and emergency medicine, 14, 797–805, 2019 [PMC free article: PMC6692560] [PubMed: 31140061] | Study not conducted in one of the countries included in the review protocol. |
| Hosking, J. E., Ameratunga, S. N., Bramley, D. M., Crengle, S. M., Reducing ethnic disparities in the quality of trauma care: An important research gap, Annals of Surgery, 253, 233–237, 2011 [PubMed: 21173692] | Study did not examine rehabilitation. |
| Hull, K., Ribariach, J., Panton, V., De Jonge, J., Bulsara, C., Developing independence and empowerment through medications self management amongst persons with acquired brain injury, Neurorehabilitation and Neural Repair, 26, 775–776, 2012 | Conference abstract. |
| Hunt, Anne W., Laupacis, Dylan, Kawaguchi, Emily, Greenspoon, Dayna, Reed, Nick, Key ingredients to an active rehabilitation programme post-concussion: perspectives of youth and parents, Brain Injury, 32, 1534–1540, 2018 [PubMed: 30047796] | It was not clear that the participants had been hospitalised (study states that the intervention/ interviews were undertaken in a hospital but many of the participants were drawn from the community). |
| Hyatt, Kyong, Davis, Linda L., Barroso, Julie, Chasing the care: soldiers experience following combat-related mild traumatic brain injury, Military Medicine, 179, 849–55, 2014 [PubMed: 25102527] | Study not conducted in one of the countries included in the review protocol. |
| Irgens, Eirik Lind, Henriksen, Nils, Moe, Siri, Communicating information and professional knowledge in acquired brain injury rehabilitation trajectories - a qualitative study of physiotherapy practice, Disability and Rehabilitation, 1–8, 2018 [PubMed: 30572746] | The focus was not specific to participants who had experienced traumatic injury and results not presented separately for target population. |
| Isbel, Stephen T., Jamieson, Maggie I., Views from health professionals on accessing rehabilitation for people with dementia following a hip fracture, Dementia (London, England), 16, 1020–1031, 2017 [PubMed: 26843421] | Population not in PICO: People >18 years old. |
| Jacoby, Sara F., Rich, John A., Webster, Jessica L., Richmond, Therese S., ‘Sharing things with people that I don’t even know’: help-seeking for psychological symptoms in injured Black men in Philadelphia, Ethnicity & health, 1–19, 2018 [PMC free article: PMC6167172] [PubMed: 29607675] | Study not conducted in one of the countries included in the review protocol. |
| Jannings, Wendy, Pryor, Julie, The experiences and needs of persons with spinal cord injury who can walk, Disability and Rehabilitation, 34, 1820–6, 2012 [PubMed: 22423597] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Janssen, Renske M. J., Satink, Ton, Ijspeert, Jos, van Alfen, Nens, Groothuis, Jan T., Packer, Tanya L., Cup, Edith H. C., Reflections of patients and therapists on a multidisciplinary rehabilitation programme for persons with brachial plexus injuries, Disability and Rehabilitation, 41, 1427–1434, 2019 [PubMed: 29385821] | Population not in PICO: Participants had not experienced traumatic injury. |
| Jellema, Sandra, van Erp, Sabine, Nijhuis-van der Sanden, Maria W. G., van der Sande, Rob, Steultjens, Esther M. J., Activity resumption after acquired brain injury: the influence of the social network as described by social workers, Disability and Rehabilitation, 1–8, 2019 [PubMed: 31429344] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jeyathevan, Gaya, Cameron, Jill I., Craven, B. Catharine, Jaglal, Susan B., Identifying Required Skills to Enhance Family Caregiver Competency in Caring for Individuals With Spinal Cord Injury Living in the Community, Topics in Spinal Cord Injury Rehabilitation, 25, 290–302, 2019 [PMC free article: PMC6907029] [PubMed: 31844381] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jeyaraj, J. A., Clendenning, A., Bellemare-Lapierre, V., Iqbal, S., Lemoine, M. C., Edwards, D., Korner-Bitensky, N., Clinicians’ perceptions of factors contributing to complexity and intensity of care of outpatients with traumatic brain injury, Brain Injury, 27, 1338–1347, 2013 [PubMed: 23923818] | Population not in PICO: People >18 years old. |
| Jeyathevan, Gaya, Catharine Craven, B., Cameron, Jill I., Jaglal, Susan B., Facilitators and barriers to supporting individuals with spinal cord injury in the community: experiences of family caregivers and care recipients, Disability and Rehabilitation, 1–11, 2019 [PubMed: 30669882] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Jiang, T., Webster, J. L., Robinson, A., Kassam-Adams, N., Richmond, T. S., Emotional responses to unintentional and intentional traumatic injuries among urban black men: A qualitative study, Injury, 49, 983–989, 2018 [PMC free article: PMC5932248] [PubMed: 29248186] | Study not conducted in one of the countries included in the review protocol. |
| Johnson, Rae A., Taggart, Susan B., Gullick, Janice G., Emerging from the trauma bubble: Redefining ‘normal’ after burn injury, Burns : journal of the International Society for Burn Injuries, 42, 1223–32, 2016 [PubMed: 27237124] | No qualitative data on phenomena of interest. |
| Jourdan, C., Azouvi, P., Pradat-Diehl, P., Ruet, A., Tenovuo, O., Traumatic Brain Injury (TBI) care pathways in Finland and in France: Organization and issues, Annals of Physical and Rehabilitation Medicine, 57, e397, 2014 | Conference abstract. |
| Jourdan, Claire, Bahrami, Stephane, Azouvi, Philippe, Tenovuo, Olli, Practitioners’ opinions on traumatic brain injury care pathways in Finland and France: different organizations, common issues, Brain Injury, 33, 205–211, 2019 [PubMed: 30449182] | Population not in PICO: People >18 years old. |
| Jurrius, K., After care for people with acquired brain injury in the chronic phase-New equilibrium in the aftercare of people with acquired brain injury and their next of kin, Brain Injury, 30, 567, 2016 | Conference abstract. |
| Keck, Casey S., Creaghead, Nancy A., Turkstra, Lyn S., Vaughn, Lisa M., Kelchner, Lisa N., Pragmatic skills after childhood traumatic brain injury: Parents’ perspectives, Journal of communication disorders, 69, 106–118, 2017 [PubMed: 28898709] | Study not conducted in one of the countries included in the review protocol. |
| Keenan, Alanna, Joseph, Lynn, The needs of family members of severe traumatic brain injured patients during critical and acute care: a qualitative study, Canadian journal of neuroscience nursing, 32, 25–35, 2010 [PubMed: 20865832] | Mixed setting and population, results not presented separately for the target settings and population. |
| Keightley, Michelle, Kendall, Victoria, Jang, Shu-Hyun, Parker, Cindy, Agnihotri, Sabrina, Colantonio, Angela, Minore, Bruce, Katt, Mae, Cameron, Anita, White, Randy, Longboat-White, Claudine, Bellavance, Alice, From health care to home community: an Aboriginal community-based ABI transition strategy, Brain Injury, 25, 142–52, 2011 [PubMed: 21219087] | No qualitative data on phenomena of interest. |
| Kellezi, Blerina, Beckett, Kate, Earthy, Sarah, Barnes, Jo, Sleney, Jude, Clarkson, Julie, Regel, Stephen, Jones, Trevor, Kendrick, Denise, Understanding and meeting information needs following unintentional injury: comparing the accounts of patients, carers and service providers, Injury, 46, 564–71, 2015 [PubMed: 25533126] | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Kennedy, Nicole, Barnes, Jessica, Rose, Anna, Veitch, Craig, Bowling, Cott Dahlberg Degeneffe Gage Higgins Keightley Majdan McCabe McColl O’Callaghan Patterson Patton Patton Schlossberg Sheppard Sinnakaruppan Smith Turner Turner Turner Turner Turner Voss, Clinicians’ expectations and early experiences of a new comprehensive rehabilitation case management model in a specialist brain injury rehabilitation unit, Brain Impairment, 13, 62–71, 2012 | Population not in PICO: People >18 years old. |
| Kennedy, P., Sherlock, O., McClelland, M., Short, D., Royle, J., Wilson, C., A multi-centre study of the community needs of people with spinal cord injuries: the first 18 months, Spinal Cord, 48, 15–20, 2010 [PubMed: 19528997] | No qualitative data on phenomena of interest. |
| Kersten, Paula, Cummins, Christine, Kayes, Nicola, Babbage, Duncan, Elder, Hinemoa, Foster, Allison, Weatherall, Mark, Siegert, Richard John, Smith, Greta, McPherson, Kathryn, Making sense of recovery after traumatic brain injury through a peer mentoring intervention: a qualitative exploration, BMJ Open, 8, e020672, 2018 [PMC free article: PMC6252636] [PubMed: 30309988] | No qualitative data on phenomena of interest. |
| Kiekens, C., Christiaens, W., Van Den Heede, K., Organization of aftercare for patients with severe burn injuries in Belgium, Annals of Physical and Rehabilitation Medicine, 57, e212–e213, 2014 | Conference abstract. |
| Kimmel, Lara A., Holland, Anne E., Hart, Melissa J., Edwards, Elton R., Page, Richard S., Hau, Raphael, Bucknill, Andrew, Gabbe, Belinda J., Discharge from the acute hospital: trauma patients’ perceptions of care, Australian health review : a publication of the Australian Hospital Association, 40, 625–632, 2016 [PubMed: 26910554] | No qualitative data on phenomena of interest. |
| Kimmel, Lara A., Holland, Anne E., Lannin, Natasha, Edwards, Elton R., Page, Richard S., Bucknill, Andrew, Hau, Raphael, Gabbe, Belinda J., Clinicians’ perceptions of decision making regarding discharge from public hospitals to in-patient rehabilitation following trauma, Australian health review : a publication of the Australian Hospital Association, 41, 192–200, 2017 [PubMed: 27144728] | No qualitative data on phenomena of interest. |
| Kingston, Gail A., Judd, Jenni, Gray, Marion A., The experience of medical and rehabilitation intervention for traumatic hand injuries in rural and remote North Queensland: a qualitative study, Disability and Rehabilitation, 37, 423–9, 2015 [PubMed: 24856789] | No qualitative data on phenomena of interest. |
| Kingston, Gail A., Judd, Dr Jenni, Gray, Marion A., The experience of living with a traumatic hand injury in a rural and remote location: an interpretive phenomenological study, Rural and remote health, 14, 2764, 2014 [PubMed: 25018127] | No qualitative data on phenomena of interest. |
| Kirk, S., Fallon, D., Fraser, C., Robinson, G., Vassallo, G., Supporting parents following childhood traumatic brain injury: a qualitative study to examine information and emotional support needs across key care transitions, Child: care, health and development, 41, 303–313, 2015 [PubMed: 25039833] | No qualitative data on phenomena of interest. |
| Kivunja, Stephen, River, Jo, Gullick, Janice, Experiences of giving and receiving care in traumatic brain injury: An integrative review, Journal of clinical nursing, 27, 1304–1328, 2018 [PubMed: 29396883] | Systematic review, included studies checked for relevance. |
| Kjaersgaard, A., Kristensen, H. K., Brain injury and severe eating difficulties at admission-patient perspective nine to fifteen months after discharge: A pilot study, Brain Sciences, 7, 96, 2017 [PMC free article: PMC5575616] [PubMed: 28783098] | Unclear how many participants had experienced traumatic injury, the results not presented separately for target population. |
| Knox, L., Douglas, J., Bigby, C., Exploring tensions associated with supported decision making in adults with severe traumatic brain injury, Brain Injury, 26, 477, 2012 | Conference abstract. |
| Koehmstedt, Christine, Lydick, Susan E., Patel, Drasti, Cai, Xinsheng, Garfinkel, Steven, Weinstein, Ali A., Health status, difficulties, and desired health information and services for veterans with traumatic brain injuries and their caregivers: A qualitative investigation, PLoS ONE, 13, e0203804, 2018 [PMC free article: PMC6135487] [PubMed: 30208083] | Study not conducted in one of the countries included in the review protocol. |
| Koizia, L., Kings, R., Koizia, A., Peck, G., Wilson, M., Hettiaratchy, S., Fertleman, M. B., Major trauma in the elderly: Frailty decline and patient experience after injury, Trauma (United Kingdom), 21, 21–26, 2019 [PMC free article: PMC6262588] [PubMed: 30581355] | Not a qualitative study. |
| Koller, Kathryn, Woods, Lindsay, Engel, Lisa, Bottari, Carolina, Dawson, Deirdre R., Nalder, Emily, Bandura, Bottari Braun Chen Colantonio Creswell Dreer Engel Fleming Fox Gaudette Hall Hoskin Kelley Kershaw Kim Knight Kreutzer Langlois Levack Malee Marson Martin McCabe McHugh Patton Poncer Weiner, Loss of financial management independence after brain injury: Survivors’ experiences, American Journal of Occupational Therapy, 70, No-Specified, 2016 [PubMed: 27089291] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Kontos, P., Miller, K. L., Colantonio, A., Cott, C., Therapeutic landscape theory: Identifying health detracting and health enhancing aspects of neurorehabilitation, Brain Injury, 28, 535, 2014 | Conference abstract. |
| Kornhaber, R., Wilson, A., Abu-Qamar, M., McLean, L., Vandervord, J., Inpatient peer support for adult burn survivors-a valuable resource: a phenomenological analysis of the Australian experience, Burns : journal of the International Society for Burn Injuries, 41, 110–7, 2015 [PubMed: 24927991] | Study did not examine phenomena of interest. |
| Kornhaber, Rachel, Rickard, Greg, McLean, Loyola, Wiechula, Rick, Lopez, Violeta, Cleary, Michelle, Burn care and rehabilitation in Australia: health professionals’ perspectives, Disability and Rehabilitation, 41, 714–719, 2019 [PubMed: 29207887] | Population not in PICO: People >18 years old. |
| Kozlowski-Moreau, O., Danze, F., Pollez, B., Brooks, N., Johnson, C., Line, M. C., Rousseaux, M., Croisiaux, C., Lanthier, A., Long-term management of severe TBI in Europe-The value of a network, Brain Injury, 30, 650, 2016 | Conference abstract. |
| Kuipers, Pim, Kendall, Melissa B., Amsters, Delena, Pershouse, Kiley, Schuurs, Sarita, Descriptions of community by people with spinal cord injuries: concepts to inform community integration and community rehabilitation, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 34, 167–74, 2011 [PubMed: 21490508] | No qualitative data on phenomena of interest. |
| Lafebvre, H., Levert, M. J., Gelinas, I., Croteau, C., Le Dorze, G., Bottari, C., McKerrall, M., Personalized accompaniment for community integration for people with a traumatic brain injury in postrehabilitation, Archives of Physical Medicine and Rehabilitation, 91, e7, 2010 | Conference abstract. |
| Lamontagne, M. E., Swaine, B. R., Lavoie, A., Careau, E., Analysis of the strengths, weaknesses, opportunities and threats of the network form of organization of traumatic brain injury service delivery systems, Brain Injury, 25, 1188–1197, 2011 [PubMed: 21939374] | No qualitative data on phenomena of interest. |
| Lange, R., French, L., Bailie, J., Lippa, S., Gartner, R., Driscoll, A., Wright, M., Smith, J., Dilay, A., Pizzano, B., Johnson, L., Nora, D., Mahatan, H., Sullivan, J., Thompson, D., Snelling, A., Brickell, T., Caring for U.S. military service members following mild-moderate traumatic brain injury: Examination of access to services, service needs, and barriers to care, Journal of Head Trauma Rehabilitation, 32, E71, 2017 | Conference abstract. |
| Lannin, N., Roberts, K., D’Cruz, K., Morarty, J., Unsworth, C., Who holds the ‘Power’ during goal-setting? A qualitative study exploring patient perceptions, International Journal of Stroke, 10, 68, 2015 | Conference abstract. |
| Lapierre, Alexandra, Lefebvre, Helene, Gauvin-Lepage, Jerome, Factors Affecting Interprofessional Teamwork in Emergency Department Care of Polytrauma Patients: Results of an Exploratory Study, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 26, 312–322, 2019 [PubMed: 31714492] | Setting not in PICO: Emergency department. |
| Lee, Tracy, Norton, Andrea, Hayes, Sue, Adamson, Keith, Schwellnus, Heidi, Evans, Cathy, Exploring Parents’ Perceptions and How Physiotherapy Supports Transition from Rehabilitation to School for Youth with an ABI, Physical & occupational therapy in pediatrics, 37, 444–455, 2017 [PubMed: 28121255] | No qualitative data on phenomena of interest. |
| Lefebvre, Helene, Levert, Marie Josee, The needs experienced by individuals and their loved ones following a traumatic brain injury, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 19, 197–207, 2012 [PubMed: 23222398] | No qualitative data on phenomena of interest. |
| Letts, L., Martin Ginis, K. A., Faulkner, G., Colquhoun, H., Levac, D., Gorczynski, P., Preferred Methods and Messengers for Delivering Physical Activity Information to People With Spinal Cord Injury: A Focus Group Study, Rehabilitation Psychology, 56, 128–137, 2011 [PubMed: 21574732] | It was unclear if the focus was specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Lexell, E. M., Alkhed, A. K., Olsson, K., The group rehabilitation helped me adjust to a new life: Experiences shared by persons with an acquired brain injury, Brain Injury, 27, 529–537, 2013 [PubMed: 23472828] | No qualitative data on phenomena of interest. |
| Lind, J. D., Fraser, M. A., Powell-Cope, G., Gavin-Dreschnack, D., Enhancing patient dignity in va spinal cord injury units, Journal of Spinal Cord Medicine, 36, 555, 2013 | Study not conducted in one of the countries included in the review protocol. |
| Lindahl, Marianne, Hvalsoe, Berit, Poulsen, Jeppe Rosengaard, Langberg, Henning, Quality in rehabilitation after a working age person has sustained a fracture: partnership contributes to continuity, Work (Reading, Mass.), 44, 177–89, 2013 [PubMed: 23324675] | Population not in PICO: People >18 years old. |
| Lindahl, Marianne, Teljigovic, Sanel, Heegaard Jensen, Lars, Hvalsoe, Berit, Juneja, Hemant, Barth, Clay Cooper Cott Del Bano-Aledo Donabedian Donabedian Fitinghoff Griffiths Harris Hours Hush Jensen Kidd Lempp Lindahl Martins McLean Mead Mussener Partridge Pinto Polinder Rindflesch Sanders Strauss Walton Willamson, Importance of a patient-centred approach in ensuring quality of post-fracture rehabilitation for working aged people: A qualitative study of therapists’ and patients’ perspectives, Work: Journal of Prevention, Assessment & Rehabilitation, 55, 831–839, 2016 [PubMed: 28059811] | Mixed population, cannot separate or confirm which patients were hospitalised and match the population of interest. |
| Lindberg, J., Kreuter, M., Taft, C., Person, L. O., Patient participation in care and rehabilitation from the perspective of patients with spinal cord injury, Spinal Cord, 51, 834–7, 2013 [PubMed: 23999110] | Study did not examine phenomena of interest. |
| Linnarsson, J. R., Bubini, J., Perseius, K. I., A meta-synthesis of qualitative research into needs and experiences of significant others to critically ill or injured patients, Journal of Clinical Nursing, 19, 3102–11, 2010 [PubMed: 20738453] | Systematic review, included studies outside of date limits (1997-2007). |
| Littooij, E., Leget, C. J. W., Stolwijk-Swuste, J. M., Doodeman, S., Widdershoven, G. A. M., Dekker, J., The importance of ‘global meaning’ for people rehabilitating from spinal cord injury, Spinal Cord, 54, 1047–1052, 2016 [PubMed: 27089865] | Study did not examine phenomena of interest. |
| Lundine, J. P., Utz, M., Jacob, V., Ciccia, A. H., Putting the person in person-centered care: Stakeholder experiences in pediatric traumatic brain injury, Journal of Pediatric Rehabilitation Medicine, 12, 21–35, 2019 [PubMed: 30883376] | Study not conducted in one of the countries included in the review protocol. |
| Maddick, Rosie, Norton, Ali Amir Andrews Baker Batavia Batt-Rawden Bernstein Braun Bright Bright Bruscia De Carvalho Deegan Dijkers Dorsett Dorsett Dorsett Fook Fook Galvin Golden Humphries James Larsson Lee Lefevre Lethborg Manns Montague Nielson North O’Callaghan O’Callaghan O’Neil Riessman Riessman Scheiby Slivka Stover Tamplin Whittemore Zedjlik, ‘Naming the unnameable and communicating the unknowable’: Reflections on a combined music therapy/social work program, The Arts in Psychotherapy, 38, 130–137, 2011 | Study did not examine phenomena of interest. |
| Makela, P., Jones, F., de Sousa de Abreu, M. I., Hollinshead, L., Ling, J., Supporting self-management after traumatic brain injury: Codesign and evaluation of a new intervention across a trauma pathway, Health expectations : an international journal of public participation in health care and health policy, 22, 632–642, 2019 [PMC free article: PMC6737836] [PubMed: 31033115] | Study did not examine phenomena of interest. |
| Manning, Joseph C., Hemingway, Pippa, Redsell, Sarah A., Survived so what? Identifying priorities for research with children and families post-paediatric intensive care unit, Nursing in critical care, 23, 68–74, 2018 [PubMed: 28516470] | Study did not examine rehabilitation. |
| Martin, Laurie T., Farris, Coreen, Parker, Andrew M., Epley, Caroline, The Defense and Veterans Brain Injury Center Care Coordination Program: Assessment of Program Structure, Activities, and Implementation, Rand health quarterly, 3, 4, 2013 [PMC free article: PMC5051987] [PubMed: 28083300] | Study not conducted in one of the countries included in the review protocol. |
| Martin, Suzanne, Armstrong, Elaine, Thomson, Eileen, Vargiu, Eloisa, Sola, Marc, Dauwalder, Stefan, Miralles, Felip, Daly Lynn, Jean, A qualitative study adopting a user-centered approach to design and validate a brain computer interface for cognitive rehabilitation for people with brain injury, Assistive technology : the official journal of RESNA, 30, 233–241, 2018 [PubMed: 28708963] | Study did not examine phenomena of interest. |
| Materne, M., Lundqvist, L. O., Strandberg, T., Opportunities and barriers for successful return to work after acquired brain injury: A patient perspective, Work (Reading, Mass.), 56, 125–134, 2017 [PMC free article: PMC5302032] [PubMed: 28035941] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| McBain, Sacha A., Sexton, Kevin W., Palmer, Brooke E., Landes, Sara J., Barriers to and facilitators of a screening procedure for PTSD risk in a level I trauma center, Trauma surgery & acute care open, 4, e000345, 2019 [PMC free article: PMC6699788] [PubMed: 31467988] | Study not conducted in one of the countries included in the review protocol. |
| McDermott, Garret L., McDonnell, Anne Marie, Acquired brain injury services in the Republic of Ireland: experiences and perceptions of families and professionals, Brain Injury, 28, 81–91, 2014 [PubMed: 24328803] | The focus was not specific to care of people who have experienced traumatic injury and the results not presented separately for target population. |
| McGarry, Sarah, Elliott, Catherine, McDonald, Ann, Valentine, Jane, Wood, Fiona, Girdler, Sonya, “This is not just a little accident”: a qualitative understanding of paediatric burns from the perspective of parents, Disability and Rehabilitation, 37, 41–50, 2015 [PubMed: 24576308] | Study did not examine phenomena of interest. |
| McIntyre, Michelle, Ehrlich, Carolyn, Kendall, Elizabeth, Informal care management after traumatic brain injury: perspectives on informal carer workload and capacity, Disability and Rehabilitation, 1–9, 2018 [PubMed: 30326760] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| McKelvey, M., Bush, E., Screening and identification of individuals with brain injury (BI) seeking services through the area agency on ageing in rural Nebraska, Brain Injury, 28, 712, 2014 | Conference abstract. |
| McPherson, K., Fadyl, J., Theadom, A., Channon, A., Levack, W., Starkey, N., Wilkinson-Meyers, L., Kayes, N., Feigin, V., Barker-Collo, S., Harwood, M., Mudge, S., Christie, G., Jenkins, S., Living Life after Traumatic Brain Injury: Phase 1 of a Longitudinal Qualitative Study, Journal of Head Trauma Rehabilitation, 33, E44–E52, 2018 [PubMed: 28520671] | No qualitative data on phenomena of interest. |
| McPherson, K., Theadom, A., Wilkinson-Meyers, L., The experience of recovery-a qualitative study, Brain Injury, 26, 493–494, 2012 | Conference abstract. |
| McRae, Philippa, Hallab, Lisa, Simpson, Grahame, Anstey, Braun Brooks Ellingsen Frost Gilworth Gilworth Gracey Harradine Kreutzer Macaden Medin Menon Nightingale Olver Oppermann Petrella Ponsford Rubenson Sabatello Simpson Tate Teasdale van Velzen van Velzen, Navigating employment pathways and supports following brain injury in Australia: Client perspectives, Australian Journal of Rehabilitation Counselling, 22, 76–92, 2016 | No qualitative data on phenomena of interest. |
| Meade, M., Carr, L., Ellenbogen, P., Barrett, K., Perceptions of provider education and attitude by individuals with spinal cord injury: Implications for health care disparities, Topics in Spinal Cord Injury Rehabilitation, 17, 25–37, 2011 | Study not conducted in one of the countries included in the review protocol. |
| Medina-Mirapeix, F., Del Bano-Aledo, M. E., Oliveira-Sousa, S. L., Escolar-Reina, P., Collins, S. M., How the rehabilitation environment influences patient perception of service quality: A qualitative study, Archives of Physical Medicine and Rehabilitation, 94, 1112–1117, 2013 [PubMed: 23154133] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Mehta, Swati, Hadjistavropoulos, Heather D., Earis, Danielle, Titov, Nick, Dear, Blake F., Patient perspectives of Internet-delivered cognitive behavior therapy for psychosocial issues post spinal cord injury, Rehabilitation Psychology, 2019 [PubMed: 30958020] | No qualitative data on phenomena of interest. |
| Meixner, Cara, O’Donoghue, Cynthia R., Witt, Michelle, Accessing crisis intervention services after brain injury: a mixed methods study, Rehabilitation psychology, 58, 377–85, 2013 [PubMed: 24128269] | Study not conducted in one of the countries included in the review protocol. |
| Messinger, Seth, Bozorghadad, Sayeh, Pasquina, Paul, Social relationships in rehabilitation and their impact on positive outcomes among amputees with lower limb loss at Walter Reed National Military Medical Center, Journal of rehabilitation medicine, 50, 86–93, 2018 [PubMed: 29206273] | Study not conducted in one of the countries included in the review protocol. |
| Milte, R., Ratcliffe, J., Miller, M., Whitehead, C., Cameron, I. D., Crotty, M., What are frail older people prepared to endure to achieve improved mobility following hip fracture? A Discrete Choice Experiment, Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine, 45, 81–86, 2013 [PubMed: 23037892] | Not a qualitative study. |
| Minney, M. J., Roberts, R. M., Mathias, J. L., Raftos, J., Kochar, A., Service and support needs following pediatric brain injury: perspectives of children with mild traumatic brain injury and their parents, Brain Injury, 33, 168–182, 2019 [PubMed: 30396278] | Study did not examine rehabilitation. |
| Mitchell, Rebecca, Fajardo Pulido, Diana, Ryder, Tayhla, Norton, Grace, Brodaty, Henry, Draper, Brian, Close, Jacqueline, Rapport, Frances, Lystad, Reidar, Harris, Ian, Harvey, Lara, Sherrington, Cathie, Cameron, Ian D., Braithwaite, Jeffrey, Access to rehabilitation services for older adults living with dementia or in a residential aged care facility following a hip fracture: healthcare professionals’ views, Disability and Rehabilitation, 1–12, 2019 [PubMed: 31335212] | Study did not examine phenomena of interest. |
| Mitsch, Virginia, Curtin, Michael, Badge, Helen, The provision of brain injury rehabilitation services for people living in rural and remote New South Wales, Australia, Brain Injury, 28, 1504–13, 2014 [PubMed: 25093407] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Moore, M., Robinson, G., Mink, R., Hudson, K., Dotolo, D., Gooding, T., Ramirez, A., Zatzick, D., Vavilala, M., Acute care after pediatric traumatic brain injury: A qualitative study of the family perspective, Journal of Neurotrauma, 31, A59, 2014 | Conference abstract. |
| Moore, Megan, Robinson, Gabrielle, Mink, Richard, Hudson, Kimberly, Dotolo, Danae, Gooding, Tracy, Ramirez, Alma, Zatzick, Douglas, Giordano, Jessica, Crawley, Deborah, Vavilala, Monica S., Developing a Family-Centered Care Model for Critical Care After Pediatric Traumatic Brain Injury, Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 16, 758–65, 2015 [PMC free article: PMC4592380] [PubMed: 26135064] | Study not conducted in one of the countries included in the review protocol. |
| Morriss, Elissa, Wright, Suzanne, Smith, Sharon, Roser, Judy, Kendall, Melissa, Ackerson, Ackerson Bassett Bassett Baulderstone Baxter Bisogni Butera-Prinzi Charles Cicerone Clark Cowling Craig Degeneffe Devany-Serio Evenson Flanagan Fletcher Gan Jacob Jones Kaatz Kirshbaum Kosciulek Lancaster Leinonen Lezak Llewellyn Maitz Nicholson Olson Pessar Qu Sander Smith Stake Strauss Urbach Uysal Visser-Meily Wade, Parenting challenges and needs for fathers following acquired brain injury (ABI) in Queensland, Australia: A preliminary model, Special Issue: Family support and adjustment following acquired brain injury: An international perspective., 19, 119–134, 2013 | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Mumbower, R., Heaton, K., Dreer, L., Novack, T., Childs, G., Vance, D., Sleep experiences following traumatic brain injury: A qualitative descriptive study, Archives of Physical Medicine and Rehabilitation, 98, e155, 2017 | Conference abstract. |
| Munce, Sarah E. P., Webster, Fiona, Fehlings, Michael G., Straus, Sharon E., Jang, Eunice, Jaglal, Susan B., Meaning of self-management from the perspective of individuals with traumatic spinal cord injury, their caregivers, and acute care and rehabilitation managers: an opportunity for improved care delivery, BMC Neurology, 16, 11, 2016 [PMC free article: PMC4724136] [PubMed: 26801243] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Munce, Sarah E. P., Webster, Fiona, Fehlings, Michael G., Straus, Sharon E., Jang, Eunice, Jaglal, Susan B., Perceived facilitators and barriers to self-management in individuals with traumatic spinal cord injury: a qualitative descriptive study, BMC Neurology, 14, 48, 2014 [PMC free article: PMC4007626] [PubMed: 24624961] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Murphy, Margaret, McCloughen, Andrea, Curtis, Kate, Using theories of behaviour change to transition multidisciplinary trauma team training from the training environment to clinical practice, Implementation science : IS, 14, 43, 2019 [PMC free article: PMC6489197] [PubMed: 31036023] | Study did not examine rehabilitation. |
| Murphy, Margaret, McCloughen, Andrea, Curtis, Kate, The impact of simulated multidisciplinary Trauma Team Training on team performance: A qualitative study, Australasian emergency care, 22, 1–7, 2019 [PubMed: 30998866] | Study did not examine rehabilitation. |
| Murray, A., Watter, K., Nielsen, M., Kennedy, A., A scoping study examining vocational rehabilitation in early acquired brain injury rehabilitation, Brain Impairment, 19, 306–307, 2018 | Conference abstract. |
| Nalder, E., Fleming, J., Cornwell, P., Foster, M., Identity and the life course: Lived experiences of individuals with traumatic brain injury during the period of transition from hospital to home, Brain Impairment, 14, 159, 2013 [PubMed: 23924357] | Conference abstract. |
| Nalder, E., Fleming, J., Cornwell, P., Foster, M., Worrall, L., Ownsworth, T., Haines, T., Kendall, M., Chenoweth, L., What constitutes transition success? An investigation into factors influencing the perceptions of individuals with a TBI regarding the transition from hospital to home, Brain Injury, 24 (3), 189–190, 2010 | Conference abstract. |
| Nalder, Emily J., Zabjek, Karl, Dawson, Deirdre R., Bottari, Carolina L., Gagnon, Isabelle, McFadyen, Bradford J., Hunt, Anne W., McKenna, Suzanne, Ouellet, Marie-Christine, Giroux, Sylvain, Cullen, Nora, Niechwiej-Szwedo, Ewa, Onf-Repar Abi Team, Research Priorities for Optimizing Long-term Community Integration after Brain Injury, The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques, 45, 643–651, 2018 [PubMed: 30430969] | Data was not collected using an appropriate qualitative methodology (the authors have analysed their own field notes taken at a 2-day conference for practitioners) |
| Nalder, Emily, Fleming, Jennifer, Cornwell, Petrea, Shields, Cassandra, Foster, Michele, Reflections on life: experiences of individuals with brain injury during the transition from hospital to home, Brain Injury, 27, 1294–303, 2013 [PubMed: 23924357] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Nasrabadi, A. N., Mohammadi, N., Davatgaran, K., Yekaninejad, M., Javidan, A. N., Shabany, M., Designing a client and family empowerment model to promote constructive life recovery among persons with spinal cord injury: A qualitative study, Archives of Neuroscience, 6, e87867, 2019 | Study not conducted in one of the countries included in the review protocol. |
| Nilsson, Charlotte, Bartfai, Aniko, Lofgren, Monika, Bartfai, Ben-Yishai Brooks Carlsson Charmaz Christensen Cicerone Cicerone Cicerone Comper Creswell Cullen Dahlgren Ferguson Fleming Gard Ho Kielhofner Lincoln Miller Ohman Phipps Ponsford Prigatano Rice-Oxley Roding Roxendahl Rudolfsson Ruff Stalnacke Svendsen Tiersky Wilson, Holistic group rehabilitation-A short cut to adaptation to the new life after mild acquired brain injury, Disability and Rehabilitation: An International, Multidisciplinary Journal, 33, 969–978, 2011 [PubMed: 21067340] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Norrbrink, Cecilia, Lofgren, Monika, Needs and requests--patients and physicians voices about improving the management of spinal cord injury neuropathic pain, Disability and Rehabilitation, 38, 151–8, 2016 [PubMed: 25918963] | No qualitative data on phenomena of interest. |
| Nunnerley, J. L., Hay-Smith, E. J., Dean, S. G., Leaving a spinal unit and returning to the wider community: an interpretative phenomenological analysis, Disability and Rehabilitation, 35, 1164–1173, 2013 [PubMed: 23035858] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| O’Callaghan, A., McNamara, B., Cocks, E., ‘What am I supposed to do? Cartwheels down the passageway?’ Perspectives on the rehabilitation journey from people with ABI, Brain Injury, 28, 577–578, 2014 | Conference abstract. |
| O’Callaghan, Anna, McAllister, Lindy, Wilson, Linda, Insight vs readiness: factors affecting engagement in therapy from the perspectives of adults with TBI and their significant others, Brain Injury, 26, 1599–610, 2012 [PubMed: 22738228] | Population not in PICO: People over 18 years old. |
| O’Callaghan, Anna, McAllister, Lindy, Wilson, Linda, Blight, Brookshire Brown Cicerone Denzin Fleming Foster Gentleman Goranson Grbich Hickson Hughes Humphreys Humphreys Josselson Katz Keleher LeFebvre Mackay MacPhail Malec McNaughton Minichiello Morse Morton Muus O’Callaghan O’Callaghan O’Callaghan O’Callaghan Penchansky Rankin Sandelowski Schmidt Schwandt Seale Sherer Stringer Tuel Turner-Stokes Youse, Healthcare consumers’ need for brain-injury services: The critical importance of timing in planning future services, Brain Impairment, 13, 316–332, 2012 | Analysis methods not appropriate (data reduced into case vignettes) |
| Odumuyiwa, Tolu, Improving access to social care services following acquired brain injury: a needs analysis, Journal of Long-Term Care, 164–175, 2019 | Population not in PICO: People over 18 years old. |
| Ogilvie, Rebekah, Foster, Kim, McCloughen, Andrea, Curtis, Kate, The injury trajectory for young people 16-24 years in the six months following injury: A mixed methods study, Injury, 47, 1966–74, 2016 [PubMed: 27282687] | Study did not examine phenomena of interest. |
| Ogilvie, Rebekah, Foster, Kim, McCloughen, Andrea, Curtis, Kate, Young peoples’ experience and self-management in the six months following major injury: A qualitative study, Injury, 46, 1841–7, 2015 [PubMed: 26036963] | No qualitative data on phenomena of interest. |
| Oster, Caisa, Kildal, Morten, Ekselius, Lisa, Return to work after burn injury: burn-injured individuals’ perception of barriers and facilitators, Journal of burn care & research : official publication of the American Burn Association, 31, 540–50, 2010 [PubMed: 20616648] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Oyesanya, Tolu O., Bowers, Barbara J., Royer, Heather R., Turkstra, Lyn S., Nurses’ concerns about caring for patients with acute and chronic traumatic brain injury, Journal of Clinical Nursing, 27, 1408–1419, 2018 [PMC free article: PMC5918200] [PubMed: 29399908] | Study not conducted in one of the countries included in the review protocol. |
| Palimaru, Alina, Cunningham, William E., Dillistone, Marcus, Vargas-Bustamante, Arturo, Liu, Honghu, Hays, Ron D., A comparison of perceptions of quality of life among adults with spinal cord injury in the United States versus the United Kingdom, Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation, 26, 3143–3155, 2017 [PubMed: 28712004] | Study did not examine phenomena of interest. |
| Pallesen, H., Buhl, I., Interdisciplinary facilitation of the minimal participation of patients with severe brain injury in early rehabilitation, European Journal of Physiotherapy, 19, 13–23, 2017 | Study includes 5 participants with acquired brain injury but only 2 (40%) are from trauma |
| Patterson, F., Fleming, J., Doig, E., Patient experiences of occupational therapy groups in traumatic brain injury rehabilitation, Brain Impairment, 19, 281, 2018 | Conference abstract. |
| Patton, Desmond, Sodhi, Aparna, Affinati, Steven, Lee, Jooyoung, Crandall, Marie, Post-Discharge Needs of Victims of Gun Violence in Chicago: A Qualitative Study, Journal of interpersonal violence, 34, 135–155, 2019 [PubMed: 27638688] | Study not conducted in one of the countries included in the review protocol. |
| Pekmezaris, Renee, Kozikowski, Andrzej, Pascarelli, Briana, Handrakis, John P., Chory, Ashley, Griffin, Doug, Bloom, Ona, Participant-reported priorities and preferences for developing a home-based physical activity telemonitoring program for persons with tetraplegia: a qualitative analysis, Spinal cord series and cases, 5, 48, 2019 [PMC free article: PMC6786286] [PubMed: 31666989] | Study not conducted in one of the countries included in the review protocol. |
| Phillips, J., Holmes, J., Auton, M., Radford, K., What are the most important outcomes of traumatic brain injury vocational rehabilitation? People with TBI, service provider and employer perspectives, Brain Injury, 30, 494–495, 2016 | Conference abstract. |
| Piccenna, Loretta, Lannin, Natasha A., Gruen, Russell, Pattuwage, Loyal, Bragge, Peter, The experience of discharge for patients with an acquired brain injury from the inpatient to the community setting: A qualitative review, Brain Injury, 30, 241–51, 2016 [PubMed: 26890803] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Plant, Sarah E., Tyson, Sarah F., Kirk, Susan, Parsons, John, What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis, Clinical rehabilitation, 30, 921–30, 2016 [PMC free article: PMC4978164] [PubMed: 27496701] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Pol, M., Peek, S., Van Nes, F., Van Hartingsveldt, M., Buurman, B., Krose, B., Everyday life after a hip fracture: What community-living older adults perceive as most beneficial for their recovery, Age and Ageing, 48, 440–447, 2019 [PMC free article: PMC6503934] [PubMed: 30806451] | No qualitative data on phenomena of interest. |
| Poncet, F., Pradat-Diehl, P., Lamontagne, M. E., Alifax, A., Barette, M., Fradelizi, P., Swaine, B., A mixed-methods approach to evaluate participants’ and service providers’ perceptions of an outpatient rehabilitation programme for persons with acquired brain injury, Brain Injury, 31, 816, 2017 [PubMed: 28716537] | Conference abstract. |
| Poncet, F., Pradat-Diehl, P., Lamontagne, M. E., Alifax, A., Fradelizi, P., Barette, M., Swaine, B., Participant and service provider perceptions of an outpatient rehabilitation program for people with acquired brain injury, Annals of Physical and Rehabilitation Medicine, 60, 334–340, 2017 [PubMed: 28716537] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Popejoy, Lori L., Dorman Marek, Karen, Scott-Cawiezell, Jill, Patterns and problems associated with transitions after hip fracture in older adults, Journal of gerontological nursing, 39, 43–52, 2013 [PubMed: 23799788] | Study not conducted in one of the countries included in the review protocol. |
| Porto, A., Anderson, L., Vogel, L., Zebracki, K., Barriers in accessing adult healthcare for transitioning youth with spinal cord injury, Developmental Medicine and Child Neurology, 60, 116, 2018 | Conference abstract. |
| Poulin, V., Lamontagne, M. E., Ouellet, M. C., Pellerin, M. A., Jean, A., Implementing best practices in cognitive rehabilitation: What are rehabilitation teams’ priorities and why?, Archives of Physical Medicine and Rehabilitation, 98, e157, 2017 | Conference abstract. |
| Prescott, Sarah, Fleming, Jennifer, Doig, Emmah, Refining a clinical practice framework to engage clients with brain injury in goal setting, Australian Occupational Therapy Journal, 66, 313–325, 2019 [PubMed: 30699467] | Study did not examine phenomena of interest. |
| Ramakrishnan, Kumaran, Johnston, Deborah, Garth, Belinda, Murphy, Gregory, Middleton, James, Cameron, Ian, Early Access to Vocational Rehabilitation for Inpatients with Spinal Cord Injury: A Qualitative Study of Patients’ Perceptions, Topics in Spinal Cord Injury Rehabilitation, 22, 183–191, 2016 [PMC free article: PMC4981013] [PubMed: 29339860] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Rashid, M., Caine, V., Newton, A. S., Goez, H. R., Healthcare professionals’ perspective on the delivery of care to children with Acquired Brain Injury (ABI) and communication with their parents, Journal of Pediatric Rehabilitation Medicine, 11, 125–131, 2018 [PubMed: 30010150] | No qualitative data on phenomena of interest. |
| Roberts, J. L., Pritchard, A. W., Williams, M., Totton, N., Morrison, V., D. In N.U, Williams, N. H., Mixed methods process evaluation of an enhanced community-based rehabilitation intervention for elderly patients with hip fracture, BMJ Open, 8 (8) (no pagination), 2018 [PMC free article: PMC6089270] [PubMed: 30093516] | No qualitative data on phenomena of interest. |
| Roberts, Jessica Louise, Din, Nafees Ud, Williams, Michelle, Hawkes, Claire A., Charles, Joanna M., Hoare, Zoe, Morrison, Val, Alexander, Swapna, Lemmey, Andrew, Sackley, Catherine, Logan, Phillipa, Wilkinson, Clare, Rycroft-Malone, Jo, Williams, Nefyn H., Development of an evidence-based complex intervention for community rehabilitation of patients with hip fracture using realist review, survey and focus groups, BMJ Open, 7, e014362, 2017 [PMC free article: PMC5652569] [PubMed: 29025824] | No qualitative data on phenomena of interest. |
| Rongen, A., Bakx, W., Nijhuis, F., Follow-up study of patients with an acquired Brain Injury after early focus on return to work during post-acute rehabilitation, Brain Injury, 24, 450–451, 2010 | Conference abstract. |
| Roscigno, Cecelia I., Parent Perceptions of How Nurse Encounters Can Provide Caring Support for the Family in Early Acute Care After Children’s Severe Traumatic Brain Injury, Journal of Neuroscience Nursing, 48, E2–E15, 2016 [PMC free article: PMC4862592] [PubMed: 26871242] | Study not conducted in one of the countries included in the review protocol. |
| Roth, Karin, Mueller, Gabi, Wyss, Adrian, Experiences of peer counselling during inpatient rehabilitation of patients with spinal cord injuries, Spinal cord series and cases, 5, 1, 2019 [PMC free article: PMC6333824] [PubMed: 30675385] | The majority of participants had not experienced traumatic injury and the results not presented separately for target population. |
| Rothlisberger, Fabian, Boes, Stefan, Rubinelli, Sara, Schmitt, Klaus, Scheel-Sailer, Anke, Challenges and potential improvements in the admission process of patients with spinal cord injury in a specialized rehabilitation clinic - an interview based qualitative study of an interdisciplinary team, BMC health services research, 17, 443, 2017 [PMC free article: PMC5485498] [PubMed: 28651583] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Ryerson Espino, S., Kelly, E., Riordan, A., Zebracki, K., Vogel, L., Personal and family experiences of caregivers of children with SCI, Developmental Medicine and Child Neurology, 58, 107–108, 2016 | Conference abstract. |
| Ryerson Espino, Susan L., Kelly, Erin H., Rivelli, Anne, Zebracki, Kathy, Vogel, Lawrence C., It is a marathon rather than a sprint: an initial exploration of unmet needs and support preferences of caregivers of children with SCI, Spinal Cord, 56, 284–294, 2018 [PubMed: 29187744] | Study not conducted in one of the countries included in the review protocol. |
| Sale, J. E. M., Bogoch, E., Hawker, G., Gignac, M., Beaton, D., Jaglal, S., Frankel, L., Patient perceptions of provider barriers to post-fracture secondary prevention, Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 25, 2581–9, 2014 [PubMed: 25082555] | No qualitative data on phenomena of interest. |
| Salsbury, Stacie A., Vining, Robert D., Gosselin, Donna, Goertz, Christine M., Be good, communicate, and collaborate: a qualitative analysis of stakeholder perspectives on adding a chiropractor to the multidisciplinary rehabilitation team, Chiropractic & manual therapies, 26, 29, 2018 [PMC free article: PMC6014012] [PubMed: 29977521] | Study not conducted in one of the countries included in the review protocol. |
| Samoborec, Stella, Ayton, Darshini, Ruseckaite, Rasa, Winbolt, Gary, Evans, Sue M., System complexities affecting recovery after a minor transport-related injury: The need for a person-centred approach, Journal of Rehabilitation Medicine, 51, 120–126, 2019 [PubMed: 30426136] | Population described as people that sustained predominantly minor injuries; study does not report any results separately for target population. |
| Sandstrom, Linda, Engstrom, Asa, Nilsson, Carina, Juuso, Paivi, Experiences of suffering multiple trauma: A qualitative study, Intensive & critical care nursing, 2019 [PubMed: 31351691] | Setting not in PICO: Intensive care unit |
| Sashika, Hironobu, Takada, Kaoruko, Kikuchi, Naohisa, Rehabilitation needs and participation restriction in patients with cognitive disorder in the chronic phase of traumatic brain injury, Medicine, 96, e5968, 2017 [PMC free article: PMC5287971] [PubMed: 28121947] | Study not conducted in one of the countries included in the review protocol. |
| Schiller, Claire, Franke, Thea, Belle, Jessica, Sims-Gould, Joanie, Sale, Joanna, Ashe, Maureen C., Words of wisdom - patient perspectives to guide recovery for older adults after hip fracture: a qualitative study, Patient preference and adherence, 9, 57–64, 2015 [PMC free article: PMC4298293] [PubMed: 25609927] | Study did not examine rehabilitation. |
| Segevall, Cecilia, Soderberg, Siv, Bjorkman Randstrom, Kerstin, The Journey Toward Taking the Day for Granted Again: The Experiences of Rural Older People’s Recovery From Hip Fracture Surgery, Orthopedic nursing, 38, 359–366, 2019 [PubMed: 31764899] | Study did not examine rehabilitation while an inpatient, when transferring, or seeking to access rehabilitation following discharge. |
| Self, Megan, Driver, Simon, Stevens, Laurel, Warren, Ann Marie, Physical activity experiences of individuals living with a traumatic brain injury: a qualitative research exploration, Adapted physical activity quarterly : APAQ, 30, 20–39, 2013 [PubMed: 23283024] | Study not conducted in one of the countries included in the review protocol. |
| Sena Martins, Bruno, Fontes, Fernando, Hespanha, Pedro, Barnes, Barnes Davis Fontes Fontes Goffman Guion Hahn Henriques Hughes Klein Leder Martins Martins Oliver Oliver Oliver Santos Somers Stiker Stone Turner Wall, Spinal cord injury in Portugal: Institutional and personal challenges, Journal of Disability Policy Studies, 28, 119–128, 2017 | No qualitative data on phenomena of interest. |
| Sharp, K., Richards, S., Client’s perspectives of smartphone technology in acquired brain injury rehabilitation, Brain Impairment, 14, 167, 2013 | Conference abstract. |
| Silver, Jeremy, Ljungberg, Inger, Libin, Alexander, Groah, Suzanne, Barriers for individuals with spinal cord injury returning to the community: a preliminary classification, Disability and Health Journal, 5, 190–6, 2012 [PubMed: 22726860] | Study not conducted in one of the countries included in the review protocol. |
| Silver, Samuel A., Saragosa, Marianne, Adhikari, Neill K., Bell, Chaim M., Harel, Ziv, Harvey, Andrea, Kitchlu, Abhijat, Neyra, Javier A., Wald, Ron, Jeffs, Lianne, What insights do patients and caregivers have on acute kidney injury and posthospitalisation care? A single-centre qualitative study from Toronto, Canada, BMJ Open, 8, e021418, 2018 [PMC free article: PMC6009618] [PubMed: 29909373] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Sims-Gould, Joanie, Byrne, Kerry, Hicks, Elisabeth, Khan, Karim, Stolee, Paul, Examining “success” in post-hip fracture care transitions: a strengths-based approach, Journal of Interprofessional Care, 26, 205–11, 2012 [PubMed: 22251369] | Population not in PICO: People over 18 years old. |
| Singh, Gurkaran, MacGillivray, Megan, Mills, Patricia, Adams, Jared, Sawatzky, Bonita, Mortenson, W. Ben, Patients’ Perspectives on the Usability of a Mobile App for Self-Management following Spinal Cord Injury, Journal of Medical Systems, 44, 26, 2019 [PubMed: 31828440] | No qualitative data on phenomena of interest. |
| Singh, Hardeep, Shah, Meeral, Flett, Heather M., Craven, B. Catherine, Verrier, Mary C., Musselman, Kristin E., Perspectives of individuals with sub-acute spinal cord injury after personalized adapted locomotor training, Disability and Rehabilitation, 40, 820–828, 2018 [PubMed: 28084843] | Population not in PICO: People over 18 years old. |
| Slomic, M., Christiansen, B., Sveen, U., Soberg, H. L., Users’ experiential knowledge as a base for evidence-based practice in inter-professional rehabilitation, Brain Injury, 30, 580–581, 2016 | Conference abstract. |
| Slomic, M., Soberg, H. L., Sveen, U., Christiansen, B., Transitions of patients with traumatic brain injury and multiple trauma between specialized and municipal rehabilitation services-Professionals’ perspectives, Cogent Medicine, 4, 1320849, 2017 | Population not in PICO: People over 18 years old. |
| Slomic, Mirela, Christiansen, Bjorg, Soberg, Helene L., Sveen, Unni, User involvement and experiential knowledge in interprofessional rehabilitation: a grounded theory study, BMC health services research, 16, 547, 2016 [PMC free article: PMC5051024] [PubMed: 27716269] | No qualitative data on phenomena of interest. |
| Smith, Bridget M., Martinez, Rachael N., Evans, Charlesnika T., Saban, Karen L., Balbale, Salva, Proescher, Eric J., Stroupe, Kevin, Hogan, Timothy P., Barriers and strategies for coordinating care among veterans with traumatic brain injury: a mixed methods study of VA polytrauma care team members, Brain Injury, 32, 755–762, 2018 [PubMed: 29537883] | Study not conducted in one of the countries included in the review protocol. |
| Smith, E. M., Boucher, N., Miller, W. C., Caregiving services in spinal cord injury: A systematic review of the literature, Spinal Cord, 54, 562–569, 2016 [PubMed: 26902459] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Smith, M., Hada, E., Long, C., Bushnik, T., Examining language preference and acculturation and implications for the continuum of care of patients with traumatic brain injury (TBI), Journal of Head Trauma Rehabilitation, 30, E107, 2015 | Conference abstract. |
| Snell, Deborah L., Martin, Rachelle, Surgenor, Lois J., Siegert, Richard J., Hay-Smith, E. Jean C., What’s wrong with me? seeking a coherent understanding of recovery after mild traumatic brain injury, Disability and Rehabilitation, 39, 1968–1975, 2017 [PubMed: 27626509] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Soong, Christine, Kurabi, Bochra, Exconde, Kathleen, Tajammal, Faiqa, Bell, Chaim M., Design of an orthopaedic-specific discharge summary, BMC Health Services Research, 16, 545, 2016 [PMC free article: PMC5050605] [PubMed: 27716194] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Sorli, H., Bach, B., Haarberg, D., Hjort-Larsen, G., Anette Hansen, S., Kristiansen, G., Hansen, H., Telerehabilitation in Norway, Brain Injury, 24, 284–285, 2010 | Conference abstract. |
| Speck, Rebecca M., Jones, Gabrielle, Barg, Frances K., McCunn, Maureen, Team composition and perceived roles of team members in the trauma bay, Journal of trauma nursing : the official journal of the Society of Trauma Nurses, 19, 133–8, 2012 [PubMed: 22955707] | Study not conducted in one of the countries included in the review protocol. |
| Starnes, C. L., Bailey, E. A., Calvert, C. T., Gusler, J., Cairns, B. A., Development of a pediatric educational tool: Helping burns heal-an adventure for kids with burns, Journal of Burn Care and Research, 37, S172, 2016 | Conference abstract. |
| Stergiou-Kita, M., Bottari, C., Dawson, D., Hebert, D., Grigorovich, A., Inter-professional approaches to vocational evaluation following traumatic brain injury, Brain Injury, 28, 774–775, 2014 | Conference abstract. |
| Stolee, Paul, Elliott, Jacobi, Byrne, Kerry, Sims-Gould, Joanie, Tong, Catherine, Chesworth, Bert, Egan, Mary, Ceci, Christine, Forbes, Dorothy, A Framework for Supporting Post-acute Care Transitions of Older Patients With Hip Fracture, Journal of the American Medical Directors Association, 20, 414–419.e1, 2019 [PubMed: 30852166] | Population not in PICO: People over 18 years old. |
| Stott-Eveneshen, Sarah, Sims-Gould, Joanie, McAllister, Megan M., Fleig, Lena, Hanson, Heather M., Cook, Wendy L., Ashe, Maureen C., Reflections on Hip Fracture Recovery From Older Adults Enrolled in a Clinical Trial, Gerontology & geriatric medicine, 3, 2333721417697663, 2017 [PMC free article: PMC5433673] [PubMed: 28540341] | No qualitative data on phenomena of interest. |
| Strandberg, T., Materne, M., Returning to working life after acquired brain injury-The rehabilitation-process, possibilities and hindrance for participation, Brain Injury, 28, 754, 2014 | Conference abstract. |
| Sullivan, Martin, Paul, Charlotte E., Herbison, G. Peter, Tamou, Peina, Derrett, Sarah, Crawford, Maureen, A longitudinal study of the life histories of people with spinal cord injury, Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention, 16, e3, 2010 [PubMed: 20876766] | A study protocol only. No data presented. |
| Sveen, Unni, Ostensjo, Sigrid, Laxe, Sara, Soberg, Helene L., Problems in functioning after a mild traumatic brain injury within the ICF framework: the patient perspective using focus groups, Disability and Rehabilitation, 35, 749–57, 2013 [PubMed: 22897238] | No qualitative data on phenomena of interest. |
| Swaine, B., Cullen, N., Bayley, M., Lavoie, A., Marshall, S., Turgeon, A., Sirois, M. J., Messier, F., Trempe, C., Who goes where and why? An environmental scan of rehab referral, admission and discharge of persons with brain injury in two canadian provinces, Brain Injury, 24, 362, 2010 | Conference abstract. |
| Takada, Kaoruko, Sashika, Hironobu, Wakabayashi, Hidetaka, Hirayasu, Yoshio, Social participation and quality-of-life of patients with traumatic brain injury living in the community: A mixed methods study, Brain Injury, 30, 1590–1598, 2016 [PubMed: 27630033] | Study not conducted in one of the countries included in the review protocol. |
| Talbot, Lise R., Levesque, Annie, Trottier, Josee, Process of implementing collaborative care and its impacts on the provision of care and rehabilitation services to patients with a moderate or severe traumatic brain injury, Journal of multidisciplinary healthcare, 7, 313–20, 2014 [PMC free article: PMC4122558] [PubMed: 25114538] | No qualitative data on phenomena of interest. |
| Thrussell, Helen, Coggrave, Maureen, Graham, Allison, Gall, Angela, Donald, Michelle, Kulshrestha, Richa, Geddis, Tracey, Women’s experiences of sexuality after spinal cord injury: a UK perspective, Spinal Cord, 56, 1084–1094, 2018 [PubMed: 30140048] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Todis, Bonnie, McCart, Melissa, Glang, Ann, Hospital to school transition following traumatic brain injury: A qualitative longitudinal study, NeuroRehabilitation, 42, 269–276, 2018 [PubMed: 29660964] | Study not conducted in one of the countries included in the review protocol. |
| Torjussen, I., In sickness and in health? The effect of ABI on couples’ relationships, Brain Impairment, 13, 160–161, 2012 | Conference abstract. |
| Toscan, Justine, Manderson, Brooke, Santi, Selena M., Stolee, Paul, “Just another fish in the pond”: the transitional care experience of a hip fracture patient, International journal of integrated care, 13, e023, 2013 [PMC free article: PMC3718274] [PubMed: 23882170] | Case report. |
| Turner, B., Fleming, J., Ownsworth, T., Cornwell, P., From hospital to home: A new conceptual framework for transition-based service delivery following acquired brain injury, Neurorehabilitation and Neural Repair, 26, 686, 2012 | Conference abstract. |
| Turner, Benjamin, Fleming, Jennifer, Ownsworth, Tamara, Cornwell, Petrea, Perceptions of recovery during the early transition phase from hospital to home following acquired brain injury: a journey of discovery, Neuropsychological rehabilitation, 21, 64–91, 2011 [PubMed: 21132603] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Turner, Benjamin James, Fleming, Jennifer, Ownsworth, Tamara, Cornwell, Petrea, Perceived service and support needs during transition from hospital to home following acquired brain injury, Disability and Rehabilitation, 33, 818–29, 2011 [PubMed: 20812814] | No qualitative data on phenomena of interest. |
| Tverdal, Cathrine Buaas, Howe, Emilie Isager, Roe, Cecilie, Helseth, Eirik, Lu, Juan, Tenovuo, Olli, Andelic, Nada, Traumatic brain injury: Patient experience and satisfaction with discharge from trauma hospital, Journal of Rehabilitation Medicine, 50, 505–513, 2018 [PubMed: 29620136] | Not a qualitative study. |
| Tyerman, Emma, Eccles, Fiona J. R., Gray, Victoria, The experiences of parenting a child with an acquired brain injury: A meta-synthesis of the qualitative literature, Brain Injury, 31, 1553–1563, 2017 [PubMed: 28750173] | Study did not examine rehabilitation. |
| Tyerman, Emma, Eccles, Fiona J. R., Gray, Victoria, Murray, Craig D., Siblings’ experiences of their relationship with a brother or sister with a pediatric acquired brain injury, Disability and Rehabilitation, 41, 2940–2948, 2019 [PubMed: 29987955] | The majority of participants’ siblings had not experienced traumatic injury and results not presented separately for target population. |
| Umeasiegbu, Veronica I., Waletich, Brittany, Whitten, Laura A., Bishop, Malachy, Abreu, Bartlett Berg Bishop Corrigan Cott Creswell Degeneffe Degeneffe deGuise Elbogen Gontkovsky Heinemann Jennekens Kreutzer Lefebvre Lehan Man Murphy O’Callaghan O’Callaghan Pickelsimer Ponsford Rotondi Sinnakaruppan Spearman Turner Vaughn, Community-based rehabilitation needs: Perceptions of individuals with brain injury and their families in the Midwestern United States, Special Issue: Family support and adjustment following acquired brain injury: An international perspective., 19, 155–163, 2013 | Study not conducted in one of the countries included in the review protocol. |
| Unger, Janelle, Singh, Hardeep, Mansfield, Avril, Hitzig, Sander L., Lenton, Erica, Musselman, Kristin E., The experiences of physical rehabilitation in individuals with spinal cord injuries: a qualitative thematic synthesis, Disability and Rehabilitation, 41, 1367–1383, 2019 [PubMed: 29334811] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Valizadeh, Sousan, Dadkhah, Behrouz, Mohammadi, Eissa, Hassankhani, Hadi, The perception of trauma patients from social support in adjustment to lower-limb amputation: a qualitative study, Indian journal of palliative care, 20, 229–38, 2014 [PMC free article: PMC4154173] [PubMed: 25191013] | Study not conducted in one of the countries included in the review protocol. |
| Van de Velde, Dominique, Bracke, Piet, Van Hove, Geert, Josephsson, Staffan, Devisch, Ignaas, Vanderstraeten, Guy, The illusion and the paradox of being autonomous, experiences from persons with spinal cord injury in their transition period from hospital to home, Disability and Rehabilitation, 34, 491–502, 2012 [PubMed: 21978173] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Van de Veldea, Dominique, Bracke, Piet, Van Hove, Geert, Josephsson, Staffan, Vanderstraeten, Guy, Perceived participation, experiences from persons with spinal cord injury in their transition period from hospital to home, International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation, 33, 346–55, 2010 [PubMed: 20679902] | Population not in PICO: Study did not mention that the patients were transferred to outpatient or community services following discharge. |
| Vassallo, G., Robinson, G., Fraser, C., Fallon, D., Kirk, S., A qualitative study to investigate families’ information and support needs following severe traumatic brain injury in childhood, Developmental Medicine and Child Neurology, 1), 34, 2014 | Conference abstract. |
| Wade, S. L., Moscato, E. L., Raj, S. P., Narad, M. E., Clinician perspectives delivering telehealth interventions to children/families impacted by pediatric traumatic brain injury, Rehabilitation Psychology, 64, 298–306, 2019 [PubMed: 30816734] | Study not conducted in one of the countries included in the review protocol. |
| Waring, Justin, Marshall, Fiona, Bishop, Simon, Understanding the occupational and organizational boundaries to safe hospital discharge, Journal of health services research & policy, 20, 35–44, 2015 [PubMed: 25472988] | It was not clear how many participants had experienced a traumatic injury; results not presented separately for target population. |
| Weatherhead, S., Calvert, P., Newby, G., Three models of group therapy in community brain injury rehabilitation, Brain Injury, 26, 430–431, 2012 | Conference abstract. |
| Weir, N., Prescott, S., Fleming, J., Doig, E., Exploration of structured communication during client-centred goal setting with people with acquired brain injury, Brain Impairment, 19, 347–348, 2018 | Conference abstract. |
| Wharewera-Mika, Julie, Cooper, Erana, Kool, Bridget, Pereira, Susana, Kelly, Patrick, Caregivers’ voices: The experiences of caregivers of children who sustained serious accidental and non-accidental head injury in early childhood, Clinical child psychology and psychiatry, 21, 268–86, 2016 [PubMed: 26088208] | No qualitative data on phenomena of interest. |
| Wheatley, Alison, Bamford, Claire, Shaw, Caroline, Flynn, Elizabeth, Smith, Amy, Beyer, Fiona, Fox, Chris, Barber, Robert, Parry, Steve W., Howel, Denise, Homer, Tara, Robinson, Louise, Allan, Louise M., Developing an Intervention for Fall-Related Injuries in Dementia (DIFRID): an integrated, mixed-methods approach, BMC Geriatrics, 19, 57, 2019 [PMC free article: PMC6394022] [PubMed: 30819097] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Whiteneck, G., Gassaway, J., Dijkers, M., Balance of spinal cord injury rehabilitation services provided in inpatient and postdischarge settings, Archives of Physical Medicine and Rehabilitation, 91, e19, 2010 [PubMed: 21353820] | Conference abstract. |
| Whiteneck, G., Gassaway, J., Dijkers, M., Lammertse, D., Hammond, F., Heinemann, A., Backus, D., Charlifue, S., Ballard, P., Zanca, J., Inpatient and post-discharge rehabilitation services provided in the first year after spinal cord injury: Findings from the SCI rehab study, Topics in Spinal Cord Injury Rehabilitation, 16, 28–29, 2011 [PubMed: 21353820] | Conference abstract. |
| Whiteneck, Gale G., Gassaway, Julie, Dijkers, Marcel P., Lammertse, Daniel P., Hammond, Flora, Heinemann, Allen W., Backus, Deborah, Charlifue, Susan, Ballard, Pamela H., Zanca, Jeanne M., Inpatient and postdischarge rehabilitation services provided in the first year after spinal cord injury: findings from the SCIRehab Study, Archives of Physical Medicine and Rehabilitation, 92, 361–8, 2011 [PubMed: 21353820] | Study not conducted in one of the countries included in the review protocol. |
| Wilbanks, Susan R., Ivankova, Nataliya V., Exploring factors facilitating adults with spinal cord injury rejoining the workforce: a pilot study, Disability and Rehabilitation, 37, 739–49, 2015 [PubMed: 25003483] | Study not conducted in one of the countries included in the review protocol. |
| Williams, L. M., Douglas, J. M., It takes 2 to tango: The therapeutic alliance in community brain injury rehabilitation, Brain Impairment, 18, 362, 2017 | Conference abstract. |
| Wong, A., Papadimitriou, C., Whiteneck, G., Deutsch, A., Heinemann, A., Goldsmith, A., Christopher, K., Focht, C., Lenze, E., Patient engagement in spinal cord injury rehabilitation: Patient and provider perspectives, Archives of Physical Medicine and Rehabilitation, 97, e71, 2016 | Conference abstract. |
| Wright, Courtney J., Zeeman, Heidi, Biezaitis, Valda, Holistic Practice in Traumatic Brain Injury Rehabilitation: Perspectives of Health Practitioners, PLoS ONE, 11, e0156826, 2016 [PMC free article: PMC4894634] [PubMed: 27270604] | No qualitative data on phenomena of interest. |
| Yenikomshian, Haig A., Lerew, Tara L., Tam, Melvin, Mandell, Sam P., Honari, Shari E., Pham, Tam N., Evaluation of Burn Rounds Using Telemedicine: Perspectives from Patients, Families, and Burn Center Staff, Telemedicine journal and e-health : the official journal of the American Telemedicine Association, 25, 25–30, 2019 [PubMed: 29733269] | The focus was not specific to participants who had experienced traumatic injury and the results not presented separately for target population. |
| Yoshida, Karen K., Self, Hazel M., Renwick, Rebecca M., Forma, Laura L., King, Audrey J., Fell, Leslie A., A value-based practice model of rehabilitation: consumers’ recommendations in action, Disability and Rehabilitation, 37, 1825–33, 2015 [PubMed: 25427892] | No qualitative data on phenomena of interest. |
Economic studies
Table 44Excluded economic studies and reasons for their exclusion
| Study | Reason for Exclusion |
|---|---|
| Bandyopadhyay, S., Wilkinson, I., Giokarinin-Royal, T., How incorporating ‘lean’ approach led to improved delivery of care and reduction in length of hospital stay, Age and Ageing, 48, 2019 | Conference abstract. |
| Bhowaneedin, A., Smith, H., Deeley, H., Reyes Payeras, C., Keating, O., Smallbone, T., Wright, I., Sharples, P. M., What evidence is available to support the development of a regional specialist neurorehabilitation outreach service, Archives of Disease in Childhood, 104, A26–A27, 2019 | Conference abstract. |
| Cheung, W. H., Shen, W. Y., Dai, D. L. K., Lee, K. B., Zhu, T. Y., Wong, R. M. Y., Leung, K. S., Evaluation of a multidisciplinary rehabilitation programme for elderly patients with hip fracture: A prospective cohort study, Journal of Rehabilitation Medicine, 50, 285–291, 2018 [PubMed: 29260234] | Intervention not in PICO: Intervention group included geriatrician care in an acute hospital and a multidisciplinary rehabilitation programme after discharge from the convalescence hospital (rehabilitation service coordination was not in an inpatient setting). |
| Closa, Conxita, Mas, Miquel A., Santaeugenia, Sebastia J., Inzitari, Marco, Ribera, Aida, Gallofre, Miquel, Hospital-at-home Integrated Care Program for Older Patients With Orthopedic Processes: An Efficient Alternative to Usual Hospital-Based Care, Journal of the American Medical Directors Association, 18, 780–784, 2017 [PubMed: 28578883] | Comparison not in PICO: Control group are in-patients and the experimental group are out-patients. |
| Collins, Nina, Miller, Richard, Kapu, April, Martin, Rita, Morton, Melissa, Forrester, Mary, Atkinson, Shelley, Evans, Bethany, Wilkinson, Linda, Outcomes of adding acute care nurse practitioners to a Level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction, The journal of trauma and acute care surgery, 76, 353–7, 2014 [PubMed: 24398767] | Intervention not in PICO: Acute care nurse practitioner (ACPN) who coordinated acute/ clinical care; only mention of “rehabilitation” was “The ACNP attended the daily discharge huddle, a team meeting that encompasses T2 [step-down care from ICU] and T3 [trauma nurse practitioner satellite service] NPs [nurse practitioner], case managers, social worker, liaisons to rehabilitation and nursing home facilities, and home health agency staff to facilitate communication and the discharge process.” Only outcome reported is length of stay. |
| Cooper, M., Ganda, K., Palmer, A., Seibel, M. J., Cost effectiveness of a targeted intervention to reduce refracture rates: Analysis of a four year prospective controlled study, Journal of Bone and Mineral Research, 26, 2011 | Conference abstract. |
| Farquhar, M., Lannin, N. A., Morarty, J., Functional outcomes from a specialised acquired brain injury community rehabilitation service - Evaluating a new model of care, Brain Impairment, 18, 344, 2017 | Conference abstract. |
| Fukuda, Haruhisa, Shimizu, Sayuri, Ishizaki, Tatsuro, Has the Reform of the Japanese Healthcare Provision System Improved the Value in Healthcare? A Cost-Consequence Analysis of Organized Care for Hip Fracture Patients, PLoS ONE, 10, e0133694, 2015 [PMC free article: PMC4514762] [PubMed: 26208322] | Comparison not in PICO: Hip fracture care in hospitals autonomously providing integrated care across specialties versus in acute care hospitals and rehabilitative care hospitals providing organized care across separate facilities (the organisation of the care not further described). |
| Kapu, A., Jones, P., Financial impact of adding acute care nurse practitioners (ACNPs) to inpatient models of care, Critical Care Medicine, 40, 27, 2012 | Conference abstract. |
| Leung, C. K., Mok, H. W., Shen, W. Y., Cheung, W. H., Leung, K. S., Evaluation of cost-effectiveness of a multidisciplinary hip fracture management program in Hong Kong, Osteoporosis International, 24, S597–S598, 2013 | Conference abstract. |
| Ling, Shi-Neng James, Kleimeyer, Christopher, Lynch, Genni, Burmeister, Elizabeth, Kennedy, Diana, Bell, Kate, Watkins, Leith, Cooke, Cameron, Can geriatric hip fractures be managed effectively within a level 1 trauma center?, Journal of Orthopaedic Trauma, 29, 160–4, 2015 [PubMed: 25699541] | Intervention not in PICO: Acute hip fracture care and not coordination of rehabilitation. |
| Pogoda, Terri K., Levy, Charles E., Helmick, Katherine, Pugh, Mary Jo, Health services and rehabilitation for active duty service members and veterans with mild TBI, Brain Injury, 31, 1220–1234, 2017 [PubMed: 28981342] | Narrative overview including cost considerations; not an economic evaluation. |
| Soong, C., Cram, P., Chezar, K., Tajammal, F., Exconde, K., Matelski, J., Sinha, S.K., Abrams, H.B., Fan-Lun, C., Fabbruzzo-Cota, C. and Backstein, D., Impact of an integrated hip fracture inpatient program on length of stay and costs, Journal of orthopaedic trauma, 30, 647–652, 2016 [PubMed: 27875490] | Population not in PICO: Hip fracture in adults. |
Appendix L. Research recommendations
Research recommendations for review question: D.2a What are the best methods to deliver and coordinate rehabilitation services and social services for adults with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No research recommendations were made for this review question.
Research recommendations for review question: D.2b What are the best methods to deliver and coordinate rehabilitation services and social services for children and young people with complex rehabilitation needs after traumatic injury when they transfer from inpatient to outpatient rehabilitation services?
No research recommendations were made for this review question.
Tables
Table 1Summary of the adult protocol (PICO/PPC table)
| Population | Quantitative |
|
|---|---|---|
| Qualitative |
| |
| Intervention/Phenomenonof interest | Quantitative |
|
| Qualitative | Methods to coordinate and deliver rehabilitation services (including in combination with social services) for adults when transferring from inpatient to outpatient rehabilitation services. Themes will be identified from the literature, but may include:
| |
| Comparison | Quantitative |
|
| Qualitative | Not applicable. | |
| Outcomes | Quantitative |
|
| Qualitative |
Themes will be identified from the literature pertaining to methods to coordinate and deliver rehabilitation services themselves and rehabilitation and social services in combination for adults, when transferring from inpatient to outpatient rehabilitation services, regarded by the population as optimal/not optimal or effective/non-effective. Themes will be identified from the literature but may include:
| |
| Context | Quantitative |
Rehabilitation and social care settings for patients with complex rehabilitation needs after traumatic injury Exclusion:
|
| Qualitative |
ADL: Activities of daily living; COPM: Canadian occupational performance measure; E-ADL-Test: Erlangen Activities of Daily Living test; EURO-QoL 5D 3L; EuroQol 5 dimensions and 3 levels; FIMFAM: Functional independence measure and functional assessment measure; GAS: Goal attainment scaling; GP: General practitioner; MDT: Multi-disciplinary team; NHS: National Health Service; OARS: Older American resources and services scale; PAT: Performance ADL test; SFMA; Selective functional movement assessment; SF-12: 12 item short-form survey; SF-36: 36 item short-form survey; SF-6D: 6-dimension short-form
Table 2Summary of the children and young people protocol (PICO/PPC table)
| Population | Quantitative |
|
|---|---|---|
| Qualitative |
| |
| Intervention/Phenomenonof interest | Quantitative |
|
| Qualitative |
Methods to coordinate and deliver rehabilitation services themselves and rehabilitation and social services in combination for children and young people when transferring from inpatient to outpatient rehabilitation services, regarded by the population as optimal/not optimal or effective/non-effective. Themes will be identified from the literature but may include:
| |
| Comparison | Quantitative |
|
| Qualitative | Not applicable. | |
| Outcomes | Quantitative |
|
| Qualitative | Themes will be identified from the literature but may include:
| |
| Context | Quantitative |
Rehabilitation and social care settings for patients with complex rehabilitation needs after traumatic injury Exclusion:
|
| Qualitative |
ADL: Activities of daily living; CHQ-CF80: Child Health Questionnaire self-report (adolescents aged 12-18 years); CHQ-PF-50: Child Health Questionnaire parent-report (children aged 5-18 years); COPM: Canadian occupational performance measure; E-ADL-Test: Erlangen Activities of Daily Living test; EURO-QoL 5D 3L; EuroQol 5 dimensions and 3 levels; FIMFAM: Functional independence measure and functional assessment measure; GAS: Goal attainment scaling; GP: General practitioner; MDT: Multi-disciplinary team; NHS: National Health Service; OARS: Older American resources and services scale; PAT: Performance ADL test; PEDS-QL: Pediatric Quality of Life Inventory; SENCO: Special Educational Needs Co-ordinator; SFMA; Selective functional movement assessment; SF-12: 12 item short-form survey; SF-36: 36 item short-form survey; SF-6D: 6-dimension shortform; TARN; Trauma Audit and Research Network
Table 3Summary of included quantitative studies
| Study | Population | Interventiona | Controla | Outcomes |
|---|---|---|---|---|
|
RCT Australia |
N = 142 General trauma Age in years [Mean (SD)]:
Gender (M/F): 106/36 NB. Only reported for whole study rather than by group. Time since injury in years: not reported. |
Multidisciplinary care Patients were invited to a MDT outpatient clinic at 1-month, 3-months postdischarge and 6-month post-discharge assessment. Visits lasted for 2-4 hours and included consultations with rehabilitation doctors, a physiotherapist, an occupational therapist and clinical psychologist. |
Usual care Overseen by a GP, with patients attending outpatients for surgical reviews or allied health therapies depending on need, prior to discharge. Invited for assessment and treatment at 6-months post-discharge only. |
|
|
RCT Singapore |
N = 162 Hip fracture Age in years [Mean (SD)]:
|
MDT care + structured assessments and checklists Patients had medical assessment on admission, followed by a protocol for early detection and management of complications. 5-week physiotherapy and occupational therapy were applied by therapists, complete with recommended milestones. Hip precaution advice was also given. |
MDT care only 2 × 30 minutes’ therapy sessions per day, 5 × per week (10 sessions total per week). Medical ward rounds occureed 3 × per week, with an MDT round every 2 weeks. |
|
|
Prospective and retrospective cohort study The Netherlands |
N = 401 Hip fracture Age in years [Mean (SD)]:
|
Multidisciplinary care pathway A 6 months MDT hip fracture pathway that spanned from admission to discharge from nursing home rehabilitation units. The pathway had a strict discharge protocol, beginning upon admission to the medical centre when they were registered to nursing homes that had beds specifically reserved for hip fracture patients. Doctors at these nursing homes were able to view medical records of participants who would be discharged to them. Post-discharge, patients had 6-week, 3-months and 6-months visits outpatient clinics. |
Standard care As per the participating medical centres hip fracture protocol prior to the intervention. No further details reported. |
|
|
Retrospective cohort study USA |
N = 21,682 General trauma Age in years [Mean (SD)]:
|
Traumatic clinical care coordination A full-time healthcare professional supervised and coordinated care, including a phone call to patient within 72 hours after discharge. |
No traumatic clinical care coordination No further details reported. |
|
|
RCT Taiwan |
N = 126 Hip fracture Age in years [Mean (SD)]:
|
Discharge planning with gerontological nurse Hospital discharge was provided by qualified gerontological nurse and included hard copies of an individualised discharge plan, goals, progression and ongoing concerns. Pariticpants received a nurse visit within 48 hours of hospital admission (and at least every 2 days during their stay) with a home visit scheduled 3-7 days’ post-discharge. |
Routine discharge planning Routine discharge planning provided by nurses. No information, discharge summary, home visit or telephone contact was given. |
|
|
RCT Taiwan |
N = 50 Hip fracture Characteristics only reported for whole study population rather than by arm. Age in years [Mean (SD)]: 78.75 (6.99) Gender (M/F): 32/18 Time since injury: not reported |
Comprehensive discharge planning Comprehensive discharge-planning was delivered by trained nurses using structured discharge instructions. 2 × home visits were also provided post-discharge, 1 at 2-weeks post-discharge and the other at 3-months post-dicharge. |
Routine discharge planning Discharge service with non-structured discharge instructions. |
|
|
RCT New Zealand |
N = 403 General trauma Age in years [Mean (SD)]:
|
Supported discharge team care Rehabilitation programme delivered by a MDT (including healthcare assistants, registered nurses, allied health professionals) for a maximum of 6 weeks. Consultant geriatricians were consulted weekly via case conferencing, with healthcare assistance visiting ≤ 4 × visits per day, 7 × per week. The team discussed patient’s progress weekly. On discharge, advance care planning was passed to the patient’s GP. |
Usual care Hospital-based discharge planning with subsequent community-based services (to include allied health, district nursing and home care). |
|
|
RCT UK |
N = 71 Hip fracture Age in years [Mean (SD)]:
Time since injury in years [Mean (SD)]:
|
More intensive MDT care ≥6 × face-to-face contacts per week with a member of the rehabilitation MDT, for a maximum of 12 weeks. |
Less intensive MDT care ≤ 3 × face-to-face contacts per week with a member of the rehabilitation MDT, for a maximum of 12 weeks. |
|
|
RCT UK | See Ryan 2006a | Seen Ryan 2006a | See Ryan 2006a |
|
|
RCT Sweden |
N = 199 Hip fracture Age in years [Mean (SD)]:
|
MDT post-operative rehabilitation Implemented in a geriatric orthopaedic ward. Areas of the pathway that were related to coordination of rehabilitation were:
|
Conventional post-operative rehabilitation Implemented in general orthopaedic ward (or general geriatric unit if patient required longer rehabilitation). Differences included ward layout, staffing levels, no staff education, no specific team structure, and less individual care planning. Additionally, there was no routine examination for post-operative complications, no nutritionally enriched food. Regarding rehabilitation, functional retraining for daily tasks was not always performed and no follow-up was scheduled after discharge. |
|
|
RCT Norway |
N = 151 TBI Age in years [Median (range)]:
|
Multidisciplinary outpatient treatment 1 × individual contact with a rehabilitation MDT and a psycho-educational group per week for 4-weeks. A schedule for return to work and other activities was developed, with individualised follow-ups in the first year. The MDT included a rehabilitation specialist, a neuropsychologist, a physician, a social worker, an occupational therapist and a nurse. |
Usual care by GP Follow-up by a GP after multidisciplinary examination, who could refer patients to other rehabilitation professionals. |
|
|
RCT USA |
N = 81 Burn injury Age in years [Mean (SD)]:
|
Extended care practitioner + telephone calls Standard care as per control group plus a reminder of telephone call schedule. Particpiants received semi-structure telephone calls from extended care coordinator at 24-48 hours post-discharge, as well as 2-, 4-, 8- and 12-weeks and 5-, 7- and 9-months post-discharge. The care coordinator assisted with local support groups, worker’s compensation and return to work. MDT were available to assist care coordinator with any other medical issues. |
Standard outpatient care Consisted of pre-discharge advice and a follow-up phone call 24h post-discharge. Participants attended outpatient clinic visits every 2 week by a MDT. |
|
ADL: Activities of daily linving; F: Female; GP: General practitioner; M: Male; MDT: Multidisciplinary team; N/n: Number; RCT: Randomised controlled trials; SD: Standard deviation; TBI: Traumatic brain injury
- (a)
For full details about the intervention/comparison, please see the evidence tables in Appendix D
Table 4Summary of included qualitative studies
| Study and aim of study | Population | Methods | Themes |
|---|---|---|---|
|
Aim of study To describe and compare service delivery approaches that aim to support re-integration into the community following SCI in-patient discharge. |
N = 10 spinal service centres
Country (N):
|
Recruitment period: July 2018 – January 2019 Data collection and analysis:
|
|
|
Aim of study To explore major trauma patient’s experiences of communication with healthcare professionals in the initial 3 years post-injury, in hospital, rehabilitation and community settings. |
N = 65 adults with major trauma Setting: Victorian State Trauma System Age [mean (SD)]: 50.7 (15.5) years Gender (M/F): 42/23 Length of hospital stay [median (IQR)]: 11 (5.4 - 26.5) days Injury cause (N):
|
Recruitment period: July 2014 – July 2015 Data collection and analysis:
|
|
|
Aim of study To explore the continuity of care between in-patient and outpatient rehabilitation services for Danish veterans with lower-limb amputees. |
N = 6 adults with lower-limb amputation Setting: in the community Age [median (range)]: 32 (25-46) years Gender (M/F): 6/0 Time since amputation [median (range)]: 5.7 (2-17) years Injury cause (N):
|
Recruitment period: November 2014 – February 2015 Data collection and analysis:
|
|
|
Aim of study To explore the rehabilitation and aftercare experiences of severe burn patients and the views of allied healthcare professionals. |
N = 57
Characteristics of individuals with burn injuries (and their parents) Burn patients and parents (N): 29
Time since injury: not reported Injury cause: not reported Characteristics of healthcare professionals Profession (N):
|
Recruitment period: January – April 2013 Data collection and analysis:
|
|
|
Aim of study To explore the communication experiences of caregivers and healthcare professionals during transitional care of elderly hip fracture patients from inpatient to community rehabilitation. |
N = 35
Characteristics of healthcare professionals only Profession (N):
|
Recruitment period: January – December 2010 Data collection and analysis:
|
|
|
Aim of study To explore the rehabilitation experiences of adults with TBI up to 4 years post injury, including facilitators and barriers. |
N = 20 adults with TBI Setting: In the community Age at recruitment [median (range)]: 39 (25-63) years Gender (M/F): 12/8 Time since injury: not reported. Injury cause: not reported. |
Recruitment period: December 2014 – May 2015 Data collection and analysis:
|
|
|
Aim of study To explore the experiences and opinions of healthcare professionals regarding how dementia affects rehabilitation care after hip fracture. |
N = 12 healthcare professionals working in hip fracture rehabilitation and dementia Setting: range of rehabilitation hospitals (urban and rural). Profession (N):
|
Recruitment period: Not reported. Data collection and analysis methods:
|
|
|
Aim of study To explore healthcare professionals views on which rehabilitation factors affect complexity TBI outpatient rehabilitation. |
N = 12 healthcare professionals working in TBI rehabilitation Setting: TBI rehabilitation outpatient clinic No demographic information reported. |
Recruitment period: Not reported. Data collection and analysis:
|
|
|
Aim of study To compare TBI care pathways and explore the views of healthcare professionals on TBI care provision in Varsinais-Suomi, Finland and Ile-de-France, France. |
N = 10 healthcare professionals working in TBI rehabilitation
Profession (N):
|
Recruitment period: Not reported. Data collection and analysis methods:
|
|
|
Aim of study To explore the views of healthcare professionals on the design, implementation and acceptability of a new comprehensive rehabilitation case management (CRCM) model. |
N = 32 healthcare professionals working in TBI rehabilitation Setting: Specialised TBI rehabilitation unit Profession (N):
|
Recruitment period: May 2011 – September 2012 Data collection and analysis:
|
|
|
Aim of study To explore healthcare professional’s experiences of acute care and rehabilitation in patients with burn injuries. |
N = 22 healthcare professionals working in burn rehabilitation Setting: range of burn rehabilitation settings (acute, rehabilitation and community). Profession (N):
|
Recruitment period: 2016 Data collection and analysis methods:
|
|
|
Aim of study To explore the experiences of orthopaedic trauma patients when transferring between acute hospital care and community settings. |
N = 7 adults with orthopaedic trauma Age [median (range)]: 51 (32-60) years Gender (M/F): 5/2 Time since injury (range): 2-24 months Injury cause: not reported |
Recruitment period: January – March 2009 Data collection and analysis:
|
|
|
Aim of study To explore the concept of engagement throughout the TBI rehabilitation care continuum and the factors that affect engagement. |
N = 23
Characteristics of adults with TBI only Age (N):
Time since injury: not reported Injury cause: not reported |
Recruitment period: Not reported. Data collection and analysis:
|
|
|
Aim of study To identify the long-term rehabilitation needs of patients with acquired brain injury and their families, and explore their experiences with accessing community services. |
Setting: Community ABI rehabilitation services. Stage 1 N = 76
Age [mean (range)]: 44.6 (29-72) years Gender (M/F): 10/9 Combined characteristics of adults with ABI and family members Injury cause (N):
Characteristics of healthcare professionals Profession: not reported Experience working in rehabilitation: not reported Stage 2 N = 21
Age [mean (range)]: 45 (36-72) years Gender (M/F): 10/2 Time since injury: not reported Injury cause: not reported Characteristics of healthcare professionals Profession: not reported Experience working in rehabilitation: not reported |
Recruitment period: Not reported. Data collection and analysis methods:
|
|
|
Aim of study To explore the experiences and views of patients undergoing SCI rehabilitation in Portugal. |
N = 93
No demographic information reported. |
Recruitment period: Not reported. Data collection and analysis methods:
|
|
|
Aim of study To explore the views of healthcare professionals on which factors are needed for a successful transition of care in patients after hip fracture. |
N = 17 healthcare professionals working in hip fracture rehabilitation Setting: Multiple healthcare settings (community, hospitals and rehabilitation centres) Profession (N):
|
Recruitment period: March – July 2010 Data collection and analysis:
|
|
|
Aim of study To explore the acceptability of a novel mobile phone application designed to facilitate self-management skills in adults with SCI, and their experiences using the application in both inpatient to outpatient settings. |
N = 20 adults with SCI Setting: SCI inpatient rehabilitation centre Age [mean (SD)]: 41 (18) years Gender (M/F): 17/3 Time since injury: not reported Injury cause (N):
|
Recruitment period: Spring 2015 – Winter 2016 Data collection and analysis:
|
|
|
Aim of study To explore the experiences of rehabilitation healthcare professionals while transferring TBI and general major trauma patients between specialised and local rehabilitation services. |
N = 85 healthcare professionals working in TBI rehabilitation
NB. No demographic information reported for observations of professional meetings. Profession (N):
|
Recruitment period: April 2014 – March 2016 Data collection and analysis:
|
|
|
Aim of study To identify factors to improve healthcare transitions in elderly adults with hip fracture and future healthcare transition interventions. |
N = 134
No demographic information reported. |
Recruitment period: 2010 Data collection and analysis:
|
|
|
Aim of study To explore the service and support needs of adults with ABI (and their family carers), and identify factors that night affect these needs, when transitioning between the hospital and home. |
N = 38
Characteristics of adults with ABI only Age [mean (range)]: 40.2 (17-63) years Gender (M/F): 15/5 Length of stay in inpatient rehabilitation (N):
|
Recruitment period: Not reported Data collection and analysis:
|
|
ABI: Acquired brain injury; ICU: Intensive care unit; F: Female; M: Male; N: Number; SCI: Spinal cord injury: SD: Standard deviation; TBI: Traumatic brain injury
Table 5Summary of themes and subthemes
| Themes and subthemes | CERQual Quality | No. of studies | Populations covered | ||
|---|---|---|---|---|---|
| Contribution by injury type (number of studies) | Sub-groups as specified in the protocol (number of studies) | ||||
| 1 Service commissioning | |||||
| 1.1 |
Commission a full service Services need to be funded and available for the entire journey of a service user - along with guidelines and a clear vision for how these services should co-ordinate, communicate and standardise in order to meet the needs of their local population | Moderate | 5 | Brain injury (1), Burns (2), Hip-fracture (1), Fractures (1) | Frail adults aged 65+ (1) |
| 1.2 |
Community services and facilities The availability and accessibility of community and social services (for example, social care and housing services) is just as important for overall rehabilitation as medical services are. These services should be properly funded and promoted. | High | 7 | Brain injury (4), Burns (1), Spinal cord injury (1), Brain injury and multiple trauma (1) | None |
| 1.3 |
Workload and demand Rehabiltation healthcare staff report being overworked and underfunded, leading to long waiting lists and poor healthcare provision. | High | 3 | Brain injury (2), Hip-fracture (1) | Frail adults aged 65+ (1) |
| 1.4 |
Rural services People living in rural areas are often underserved. Additional effort will be needed to ensure that the rehabilitation needs after traumatic injuries of these people are met. | High | 5 | Brain injury (4), Burns (1) | None |
| 2 Integrating multiple services | |||||
| 2.1 |
Integrated multidisciplinary team approach A MDT approach to co-ordinating medical and social support needs is important when transferring from inpatient to outpatient services. | High | 5 | Brain injury (1), Burns (1), Hip-fracture (1), Spinal cord injury (1), Brain injury and multiple trauma (1) | Frail adults aged 65+ (1) |
| 2.2 |
Inter-service awareness and relationships Healthcare staff find it easier for multiple agencies to work together if they know each other’s roles and remits, and have the opportunity to build relationships. | High | 3 | Hip-fracture (1), Fractures (1), Brain injury and multiple trauma (1) | Frail adults aged 65+ (1) |
| 2.3 |
Inter-service communication of information Adults with rehabilitation needs can find it distressing to repeat their injury and medical history to multiple people. Communication between rehabilitation services should be efficient and easy. | Moderate | 6 | Burns (1), Hip-fracture (1), Fractures (1), General trauma (1), Amputations (1), Brain injury and multiple trauma (1) | Frail adults aged 65+ (1) |
| 2.4 |
Case coordinator A case coordinator helps to increase continuity and consistency when transferring between inpatient and outpatient settings. | High | 3 | Brain injury (1), Burns (1), General trauma (1) | None |
| 2.5 |
Interdisciplinary consistency Medical information and instructions from different healthcare professionals should be compatible, complimentary and consistent to prevent confusion. | Moderate | 3 | Brain injury (1), Spinal cord injury (1), General trauma (1) | None |
| 3 Delivery | |||||
| 3.1 |
Continuity of staff Where possible, healthcare professionals and people with rehabilitation needs appreciate continuity of staff, This helps to build trust and rapport while changes in staff can be discouraging, costs time to share history and details, and cause mistakes. | High | 4 | Brain injury (2), Burns (1), Fractures (1) | None |
| 3.2 |
Include family Family play a very significant role in coordination of rehabilitation care when returning to the community. If appropriate, family members should be included in discussions and planning of care, as well as any education needed to provide rehabilitation support. | High | 9 | Brain injury (3), Burns (2), Hip-fracture (3), Spinal cord injury (1) | Frail adults aged 65+ (3) |
| 3.3 |
Point of contact A single, identifiable point of communication for information and support can increase coordination when transferring between inpatient and outpatient rehabilitation services. | High | 5 | Brain injury (3), General trauma (1), Amputations (1) | None |
| 3.4 |
Peer support Peer mentors can encourage people in their ongoing rehabilitation, be a role-model and provide information on their own lived experiences with rehabilitation services in the area. | Very low | 1 | Spinal cord injury (1) | None |
| 3.5 |
Delivery at home Healthcare staff report that delivery of rehabilitation at home is becoming more feasible, meaning people do not have to have such prolonged hospital stays. | Low | 2 | Brain injury (1), Burns (1) | None |
| 3.6 |
Technology Videoconferencing and telemedicine can be useful to reach people who cannot attend in-person consultations for a variety of reasons. Apps can also be useful for alerts or reminders | Low | 3 | Burns (1), Spinal cord injury (2) | None |
| 4 Information | |||||
| 4.1 |
Inform about services and plans Adults with rehabilitation needs report co-ordination being increased when they receive more information on what to expect after discharge, what arrangements are in place and probable timelines. | High | 7 | Brain injury (3), Burns (2), Hip-fracture (1), General trauma (1) | Frail adults aged 65+ (1) |
| 4.2 |
Prognosis Adults with rehabilitation needs want information about the likely long-term prognosis of their injuries and how this will affect their lives going forward. | High | 3 | Brain injury (1), Burns (1), General trauma (1) | None |
| 4.3 |
Format Information should be given information in plain, accessible language. Written information may be helpful for retaining this information. | Very low | 1 | General trauma (1) | None |
| 5 Individual factors | |||||
| 5.1 |
Personalisation Rehabilitation should be delivered in an adaptable fashion, taking into account related to age, and symptoms or comorbidities which may limit mobility. Additional planning may be needed to provide flexible rehabilitation sessions, as well as social vulnerabilities (for example, such as housing and financial situation). | Low | 6 | Brain injury (2), Burns (1), Hip-fracture (1), Spinal cord injury (1), Fractures (1) | Frail adults aged 65+ (1) |
| 5.2 |
Admission criteria Inflexible admission criteria may mean that rehabilitative support is not offered to certain adults (for example, if their difficulties are perceived as less severe). Financial factors or postcode may also limit rehabilitation access. | Low | 3 | Brain injury (2), Hip-fracture (1) | Frail adults aged 65+ (1) |
| 5.3 |
Specialists Upon discharge from inpatient settings, adults with rehabilitation needs report that services become more generic and staff do not have knowledge about their particular conditions or disabilities. It is important for the delivery of an individual’s rehabilitation ongoing care team to include some staff with specialist knowledge. | High | 5 | Brain injury (3), Burns (2) | None |
| 5.4 |
Home adjustments Some adults with rehabilitation needs require physical aids and small adjustments in their home. These adjustments may be vital to the discharge process and progression with rehabilitation. | Low | 1 | Fractures (1) | None |
| 5.5 |
Advocacy Some adults with rehabilitation needs may need support with researching options and initiating conversations. Some might need their family to take the lead healthcare staff about rehabilitation, or in some cases the adult may do it for themselves. | High | 3 | Brain injury (1), Hip-fracture (1), Amputations (1) | Frail adults aged 65+ (1) |
| 6 Timing | |||||
| 6.1 |
Gradual Return to the community should be a gradual and incremental process (for example, using pre-discharge home visits). Abrupt endings or loss of support can be distressing. | High | 8 | Brain injury (2), Burns (2), Hip-fracture (1), Spinal cord injury (1), Fractures (1), Brain injury and multiple trauma (1) | Frail adults aged 65+ (1) |
| 6.2 |
Start early Conversations about discharge planning and any adjustments should start early on to avoid abruptness. Last-minute conversations about needs and rehabilitation close to the time discharge are distressing. | Low | 5 | Brain injury (2), Burns (1), Spinal cord injury (1), General trauma (1) | None |
| 6.3 |
Gap in service Some adults with rehabilitation needs report experiencing gaps in service and long waiting times before starting community rehabilitation, which was confusing and distressing. Some of this distress can be lessened if people were given probably timelines. | Low | 6 | Brain injury (3), Hip-fracture (1), Fractures (1), General trauma (1) | Frail adults aged 65+ (1) |
Table 6Summary of relevant qualitative and quantitative evidence
| Qualitative theme | Quantitative intervention and results | Study IDs |
|---|---|---|
| 1 Service commissioning | ||
| Rehabilitation services should be developed to included the entire patient pathway, ensuring that there is a clear vision of how different areas should coordinate and communicate with each other. (moderate quality) | The multidisciplinary care pathway intervention was designed to span from admission at the emergency room to discharge from nursing home rehabilitation units.
| Quantitative
|
| If rehabilitation services are understaffed, healthcare workers can become overworked which affects the coordination of rehabilitatin services. This may cause long waiting lists, cases to be missed and less patient contact time. (high quality) | The MDT post-operative rehabilitation intervention included increasing staffing levels from 1.07 WTE nurses/aides per bed, plus 2 × 1 WTE physiotherapists, 2 × 1 WTE occupational therapists and 0.2 WTE dietician.
| Quantitative
|
| 2 Integrating multiple services | ||
| Multidisciplinary team approach to medical and social support needs should be integrated and united at transfer from inpatient to outpatient rehabilitation services. (high quality) | The multidisciplinary team care, multidisciplinary care pathway, multidisciplinary outpatient treatment, multidisciplinary post-opertive rehabilitation and support discharge team care involved assessment and care from different professionals such as physiotherapist, psychologist nurses, healthcare assistants etc, depending on the needs of the patients until they were discharged into the community.
| Quantitative
|
| Better communication and information sharing between different services reduce the need for adults with rehabilitation to recount or recall their history or symptoms which may be distressing. (moderate quality) | Within the multidisciplinary care pathway and supported discharge team care, patient information was passed to rehabilitation homes and community primary care services respectively, prior to discharge.
| Quantitative
|
| Having a case manager or coordinator ensures continuity and provides a point of contact for patients’ enquiries. (high quality) | The traumatic clinical care coordination and the extended care practitioner plus telephone calls included a healthcare professional that coordinated care during discharge as well as post-discharge follow-ups and home visits.
| Quantitative
|
| Consistency in the information provided by the different parts of the multidisciplinary team can a build trust between the patients and the team. (moderate quality) | Within the extended care practioner plus telephone calls intervention, the extended care practitioner communication with the multidisciplinary team regulary about progress and concerns. The extended care practitioner then relayed this information to the patient, their families and carers.
| Quantitative
|
| 3 Delivery | ||
| A single point of contact for information, support, and for the coordination of plans is helpful for patients as they transfer from inpatient to outpatient rehabilitation settings. (high quality) | Traumatic Clinical Care Coordination, the discharge planning with a gerontological nurse intervention and extended care practitioner intervention all had a central healthcare professional for patients to contact and help coordinate rehabilitation.
| Quantitative
|
| Peer mentors with lived experience in the delivery of rehabilitation services can support patients, offer encouragement and answer questions. (very low quality) | Patients involved in multidisciplinary outpatient treatment internvention shared their experiences at group sessions.
| Quantitative
|
| 4 Information | ||
| Transitions can be smoothed by increasing information available. Patients need to know about the arrangements that have been made for them and their ongoing treatment plan, or what they will need to arrange themselves. This information is empowering and improves treatment adherence. (high quality) | Both discharge planning interventions, extended care coordinator intervention, and the Traumatic Clinical Care Coordination intervention made sharing information with patients and family a key area to focus on.
| Quantitative
|
| Information should be presented in plain, accessible language. Written information can help rehabilitation patients to understand and retain information. (very low quality) | The discharge planning intervention included hard copies of rehabilitation plans, goals and any concerns given to patient and carers prior to discharge.
| Quantitative
|
| 5 Individual factors | ||
| Rehabilitation should be delivered in a way that is adaptable to the circumstances and needs of individuals. Rehabilitation should take into account needs related to age, working patterns, and symptoms or comorbidities such as chronic pain, or disabilities which may limit mobility. (low quality) | The multidisciplinary care pathway, tramatic clinical care coordination, discharge planning with a gerontological nurse, comprehensive discharge planning, supported discharge team care, multidisciplinary post-operative rehabilitation and multidisciplinary outpatient treatment interventions stressed the important of personalising the rehabilitation pathway for patients, rather than a standard ‘one-size-fits-all’ approach.
| Quantitative
|
| Some adults with rehabilitation needs require physical aids and small adjustments in their home to aid discharge process and rehabilitation progress. (low quality) | The discharge planning intervention and MDT post-operative rehabilitation both involved home visits, where minor home adjustments could be made.
| Quantitative
|
| Some patients (and their families) may not be able to advocate for themselves as strongly as others. Healthcare workers should ensure that these vulnerable service users are properly advocated for in rehabilitation and social service situations. (high quality) |
| Quantitative
|
| 6 Timing | ||
| Conversations about rehabilitation and discharge planning should start early on, allowing needs and preferences to be integrated smoothly into recovery plans. Last-minute conversations and preparations can be distressing for patients. (low quality) | The multidisciplinary care pathway and discharge planning interventions ensured that conversations surrounding discharge were initiated early on.
| Quantitative
|
ADL: Activities of daily living; EQ-5D; Euroqol 5-Domain; EQ-VAS; Euroqol Visual Analogue Scale; GP: General practitioner; P-ADL: Phyiscal actitivies of daily living; SF-12; 12 item short form survey; SF-36: 36 item short-form survey
- *
This outcome measure was reported as statistically significant according to the analysis performed by the authors. As only the median and interquartile ranges/no standard deviations were reported by the study authors, and no published minimally important difference were found, we were unable to determine clinical importance.
Table 7Summary of included quantitative studies
| Study | Population | Interventiona | Controla | Outcomes |
|---|---|---|---|---|
|
RCT Brazil |
N=87 TBI Age in months [Mean (SD)]:
|
Family-supported rehabilitation programme An individualised rehabilitation programme was designed around simple activities that could be done at home. Parents received training and a manual containing illustrations of the exercises in their child’s regimen. Bi-weekly appointments at the rehabilitation centre carried on throughout the 12-month intervention to monitor progress and discuss new rehabilitation objectives. Each child had 2 case managers assigned throughout the programme to teach exercises to family members and coordinate care. |
Clinician-delivered rehabilitation programme 5 × 2 hour conventional rehabilitation sessions per week for 12 months, given directly by rehabilitation healthcare professionals. Clinicians followed conventional rehabilitation procedures and treated children without parental presence. Parents received no training about their child’s rehabilitation but did attend information and support group sessions during the initial 2-week assessment period in order to help their coping of their child’s |
|
ADL: Activities of daily living; N: Number; RCT: Randomised controlled trial; SD: Standard deviation; TBI: Traumatic brain injury
- (a)
For full details about the intervention/comparison, please see the evidence tables in Appendix D
Table 8Summary of included qualitative studies
| Study and aim of study | Population | Methods | Themes |
|---|---|---|---|
|
Canada Aim of study To explore healthcare professional’s experiences and views regarding the needs of families’ rehabilitation needs for children with ABI. |
N = 15 healthcare professionals working in ABI rehabilitation Setting: Brain injury clinic of large urban rehabilitation centre No further details reported |
Recruitment period: Not reported Data collection & analysis methods:
|
|
ABI: Acquired brain injury; N: Number
Table 9Summary of themes
| Themes and subthemes | Quality | No. of studies | Populations covered | ||
|---|---|---|---|---|---|
| Contribution by injury type (no. of studies) | Sub-groups as specified in the protocol (no. of studies) | ||||
| Theme 1: Compatibility across healthcare disciplines | |||||
| 1.1 |
Setting common goals In order to increase coordination between disciplines during discharge, healthcare professionals should endeavour to set goals that are common across healthcare settings. Progress should be monitored using standardised measurements, including quality of life. | Very low | 1 | TBI (1) | [none] |
| Theme 2: Resources | |||||
| 2.1 |
Case workers A designated case worker can act as an additional resource for families during discharge, acting as a knowledgeable intermediary between healthcare staff and families. | Very low | 1 | TBI (1) | [none] |
| 2.2 |
Importance of community support Families who have a child with ABI can help support other families re-integrate into the community after discharge. Social media can facilitate this by building stronger connections between parents/carers or support groups. | Very low | 1 | TBI (1) | [none] |
ABI: Acquired brain injury; TBI: Traumatic brain injury
Table 10Synthesis of qualitative and quantitative evidence
| Qualitative theme | Quantitative intervention and results | Study IDs |
|---|---|---|
| Resources | ||
| A designated case worker can act as an additional resource for families during discharge, acting as a intermediary between rehabilitation MDT and families (very low quality) | Within the family-supported rehabilitation programme, each child was allocated 2 case workers (from different rehabilitation disciplines) to act as a central contact point after discharge.
| Quantitative
|
ADL: Activities of daily living; MDT: Multidisciplinary team;
FINAL
Evidence reviews underpinning recommendations 1.1.1, 1.2.1, 1.2.2, 1.4.1, 1.4.2, 1.5.7, 1.6.6, 1.7.1, 1.7.6, 1.7.9, 1.7.10, 1.8.1, 1.8.3, 1.8.9, 1.8.15, 1.8.16, 1.8.22 to 1.8.24, 1.9.1, 1.9.2, 1.10.1, 1.10.2, 1.10.6, 1.10.8 to 1.10.10, 1.10.12 and 1.10.14
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer: The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. All NICE guidance is subject to regular review and may be updated or withdrawn.