NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Breast radiotherapy
This evidence report contains information on 4 reviews relating to breast radiotherapy.
- Review question 8.1 What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
- Review question 8.2 Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
- Review question 8.3 Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
- Review question 8.4 What are the indications for radiotherapy to internal mammary nodes?
Review question 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Introduction
The number of early breast cancer survivors is increasing. This is the result of a combination of increased incidence of the disease, widespread availability of breast screening and the development of more effective treatment strategies. As a consequence, more women cured of breast cancer will live with the late effects of their treatment.
Breast radiotherapy is associated with a 1–2% excess of non-breast cancer mortality, the majority of which is attributable to cardiac disease. There is a linear, no-threshold relationship between mean heart dose and the risk of subsequent major coronary events. Excluding the heart from the radiotherapy field reduces mean heart dose and therefore the risk of longer term cardiac side effects
The objective of this review is to determine which heart-sparing breast radiotherapy techniques are effective without compromising the treatment of the whole breast volume, and to identify which techniques should be offered to spare the heart during radiotherapy.
PICO table
See Table 1 for a summary of the population, intervention, comparison and outcome (PICO) characteristics of this review.
For full details see review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual; see the methods chapter for further information.
Declarations of interest were recorded according to NICE’s 2014 conflicts of interest policy.
Clinical evidence
Included studies
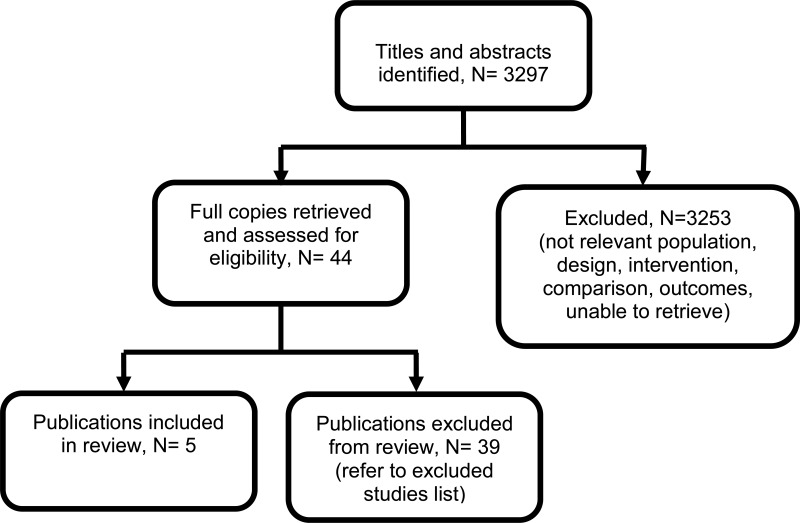
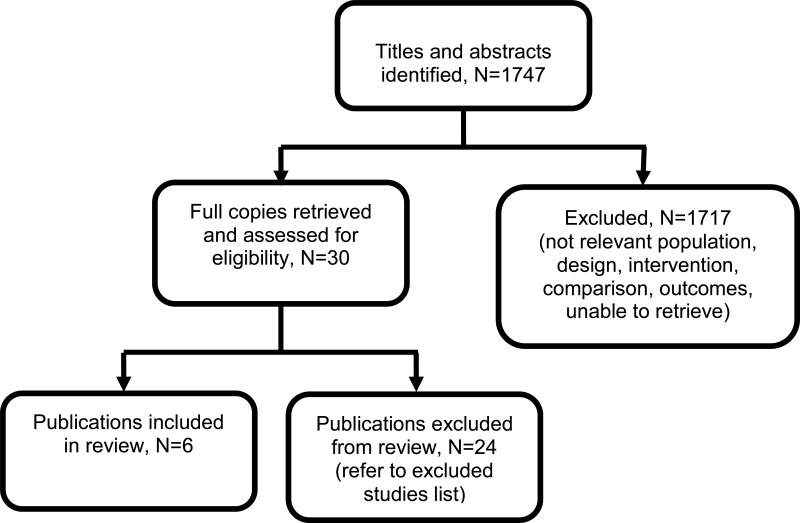
Four observational studies (number of participants, N=236) and 1 randomized cross over study (N=28) were included in the review (Barlett 2017; Barlett 2015; Chi 2015; Czeremszynska 2017; Eldredge Hindy 2015). All 5 studies reported on the mean heart dose. One study (Eldredge Hindy 2015) reported on the target coverage. No studies reported data on local recurrence rate, treatment related morbidity or mortality.
There was no evidence available for shielding and proton beam radiotherapy.
See also the study selection flow chart in appendix C, forest plots in appendix E and study evidence tables in appendix D.
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K.
Summary of clinical studies included in the evidence review
Table 2 provides a brief summary of the included studies
See appendix D for full evidence tables.
Quality assessment of clinical studies included in the evidence review
The clinical evidence profile for this review question (heart sparing radiotherapy) is presented in Table 3 and Table 4. The evidence was very low quality because of the observational nature of the included studies and small sample size.
See appendix F for full GRADE tables.
Economic evidence
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question. Economic modelling was not undertaken for this question because other topics were agreed as higher priorities for economic evaluation.
Evidence statements
Comparison 1. Deep inspiration breath-hold versus free breathing
Critical outcomes
Mean heart dose
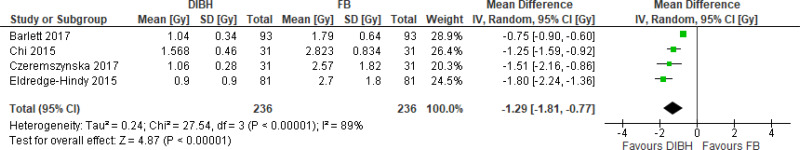
- There is very low quality evidence from four prospective cohort studies (N=236) that deep inhalation breath hold produces clinically meaningful reduction in mean heart dose compared with free breathing at radiotherapy for people with invasive breast cancer and/or ductal carcinoma in situ (DCIS) receiving whole breast radiotherapy.
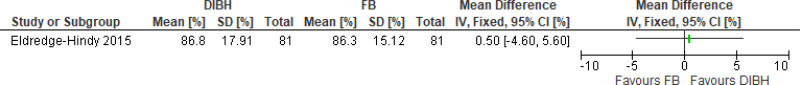
Target coverage
- There is very low quality evidence from one prospective cohort study (N=81) that deep inspiration breath-hold does not produce clinically meaningful change in target coverage compared to free breathing at radiotherapy for people with invasive breast cancer and/or DCIS receiving whole breast radiotherapy.
Important Outcomes
Local recurrence rate
- No evidence was found for this outcome.
Treatment-related morbidity
- No evidence was found for this outcome.
Treatment-related mortality
- No evidence was found for this outcome.
Comparison 2. Deep inspiration breath-hold versus prone radiotherapy
Critical outcomes
Mean heart dose
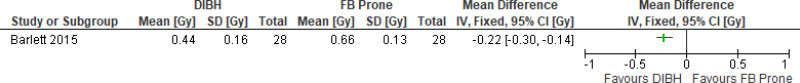
- There is low quality evidence from one randomized cross over study (N=28) that deep inhalation breath hold produces clinically meaningful reduction in mean heart dose compared with prone radiotherapy for people with invasive breast cancer and/or DCIS receiving whole breast radiotherapy.
Target coverage
- No evidence was found for this outcome.
Important Outcomes
Local recurrence rate
- No evidence was found for this outcome.
Treatment-related morbidity
- No evidence was found for this outcome.
Treatment-related mortality
- No evidence was found for this outcome.
Other interventions
- There was no evidence available on shielding or on proton beam radiotherapy
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
As this review question is considering a heart sparing radiotherapy technique, mean heart dose and target coverage were selected as critical outcomes by the committee. The inclusion of treatment-related morbidities and treatment-related mortality as important outcomes was to allow a balance of the benefits and harms of treatments to be made. Local recurrence rate was identified as other important outcome.
No evidence was available for treatment-related morbidities, treatment-related mortality and local recurrence rate.
The quality of the evidence
The quality of the evidence for this review was assessed using GRADE. For comparison of mean heart dose using deep inspiratory breath-hold technique compared to free breathing, the evidence was of a very low quality, and was downgraded due to observational study design and imprecision due to small sample size. For target coverage, the evidence was of very low quality due to observational study design and small sample size.
The quality of evidence for mean heart dose using deep inspiratory breath-hold technique compared to prone radiotherapy was low quality. The evidence quality was downgraded mainly due to uncertainty around the estimate due to small sample size and indirectness due to the inclusion of only women with large breasts.
Benefits and harms
The use of deep inspiratory breath-hold technique during whole breast radiotherapy leads to reduction in mean heart dose without compromising the target coverage. Specifically, it leads to a reduction in mean heart dose by 1.29 Gy, which is almost a 50% reduction in the mean heart dose. The committee discussed that this may potentially lead to reduction in late cardiovascular morbidity/mortality and will be particularly beneficial for people with cardiovascular risk factors. The committee were aware of estimates that a decrease in 1 Gy led to a 7% reduction in cardiovascular morbidity (Darby 2013). The committee noted that reduction in cardiovascular morbidity may also lead to cost reduction to the NHS. The committee also discussed that heart sparing radiotherapy techniques may reduce treatment related anxiety for people undergoing radiotherapy and improve quality of life due to decreased cardiovascular effects.
There was no evidence available regarding treatment related morbidity or mortality and local recurrence rate for deep inspiratory breath hold technique. Based on their experience and expertise, the committee discussed that deep inspiratory breath hold technique only requires a change in position during radiotherapy and is not known to be associated with serious harms. However, the committee discussed that deep inspiratory breath-hold technique may be more demanding for people who may struggle to do this exercise. The committee also discussed that people with disabilities, particularly respiratory compromise, may be unable to perform the breathing exercises required and therefore unable to access the technique.
The committee agreed that although many centres were already offering the breath-hold technique, some centres did not use it routinely and therefore this recommendation would reduce variation in practice across the country.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee discussed that the use of deep inspiratory breath-hold technique will require increased resource use within some radiotherapy departments. This will include a coaching session of up to 45 minutes to train the person to use the technique, an extension to the radiotherapy treatment time of approximately 10 to 15 minutes (as the treatment is paused between breath-holds), and possibly some initial training time for the radiotherapy team to implement the use of routine breath-hold technique. The extended treatment time will also impact on the utilisation of equipment, which may already be used to capacity.
However, these costs may be offset in the longer term by the expected reduction in cardiac events and therefore a reduction in the costs to the NHS of managing these events. Therefore, it is likely that the technique would be cost-effective in cost per QALY terms.
While there may be resource implications for those centres not currently using the technique, the overall resource impact of implementing the recommendation across the NHS was not thought to be significant because the technique is already being used in many centres.
Other factors the committee took into account
The committee noted that deep inspiratory breath-hold technique may also benefit people with right sided breast cancer, particularly when the target volume extends over the midline, but had not looked at evidence for this so were unable to make a specific recommendation for this group of people.
References
Bartlett 2015
Bartlett, F. R., Colgan, R. M., Donovan, E. M., McNair, H. A., Carr, K., Evans, P. M., Griffin, C., Locke, I., Haviland, J. S., Yarnold, J. R., Kirby, A. M. (2015) The UK HeartSpare Study (Stage IB): Randomised comparison of a voluntary breath-hold technique and prone radiotherapy after breast conserving surgery. Radiotherapy and Oncology, 114, 66–72. [PubMed: 25739317]Bartlett 2017
Bartlett, F. R., Donovan, E. M., McNair, H. A., Corsini, L. A., Colgan, R. M., Evans, P. M., Maynard, L., Griffin, C., Haviland, J. S., Yarnold, J. R., Kirby, A. M. (2017) The UK HeartSpare Study (Stage II): Multicentre Evaluation of a Voluntary Breath-hold Technique in Patients Receiving Breast Radiotherapy. Clinical Oncology, 29, e51–e56. [PubMed: 27890346]Chi 2015
Chi, F., Wu, S., Zhou, J., Li, F., Sun, J., Lin, Q., Lin, H., Guan, X., He, Z. (2015) Dosimetric comparison of moderate deep inspiration breath-hold and free-breathing intensity-modulated radiotherapy for left-sided breast cancer. Cancer/Radiotherapie, 19, 180–186. [PubMed: 25921618]Czeremszynska 2017
Czeremszynska, B., Drozda, S., Gorzynski, M., Kepka, L. (2017) Selection of patients with left breast cancer for deep-inspiration breath-hold radiotherapy technique: Results of a prospective study. Reports of Practical Oncology and Radiotherapy, 22, 341–348. [PMC free article: PMC5496478] [PubMed: 28701900]Darby 2013
Darby, S.C., Ewertz M., McGale, P, Bennet A.M., Blom-Goldman, U., Bronnum, D., Correa, C., Cutter, D., Gagliardi, G., Gigante, B., Jensen, M.B., Nisbet, A., Peto, R., Rahimi, K., Taylor, C., Hall, P.(2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. New England Journal of Medicine, 368(11),987–98. [PubMed: 23484825]Eldredge-Hindy 2015
Eldredge-Hindy, H., Lockamy, V., Crawford, A., Nettleton, V., Werner-Wasik, M., Siglin, J., Simone, N. L., Sidhu, K., Anne, P. R. (2015) Active Breathing Coordinator reduces radiation dose to the heart and preserves local control in patients with left breast cancer: Report of a prospective trial. Practical Radiation Oncology, 5, 4–10. [PMC free article: PMC4289538] [PubMed: 25567159]
Review question 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Introduction
Adjuvant whole breast radiotherapy is the current standard treatment option for most people with stage 1 and 2 breast cancer after breast-conserving surgery (BCS). Multiple retrospective studies and an overview of randomized trials have established the equivalence of this treatment approach compared with mastectomy in terms of both disease-free and overall survival. Whole breast radiotherapy halves the risk of local recurrence. However, local recurrence rates have fallen dramatically over the last 30 years, so that the absolute benefit of radiotherapy for some individuals may not outweigh the potential risks (for example, normal tissue toxicity, cardiac morbidity, second cancers). For many women, increasingly diagnosed with small screen-detected cancers, it is the late complications of radiotherapy, rather than the risk of local recurrence, that is their predominant concern.
Whilst the proportional benefit of radiotherapy is similar across all subgroups of women with breast cancer, the absolute benefit for women with good prognosis tumours is small. The aim of this review is to determine if specific groups of women can be identified in whom breast radiotherapy does not have a favourable risk/benefit ratio and so can be omitted.
PICO table
See Table 5 for a summary of the population, intervention, comparison and outcome (PICO) characteristics of this review.
For full details see review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual; see the methods chapter for further information.
Declarations of interest were recorded according to NICE’s 2014 conflicts of interest policy.
Clinical evidence
Included studies
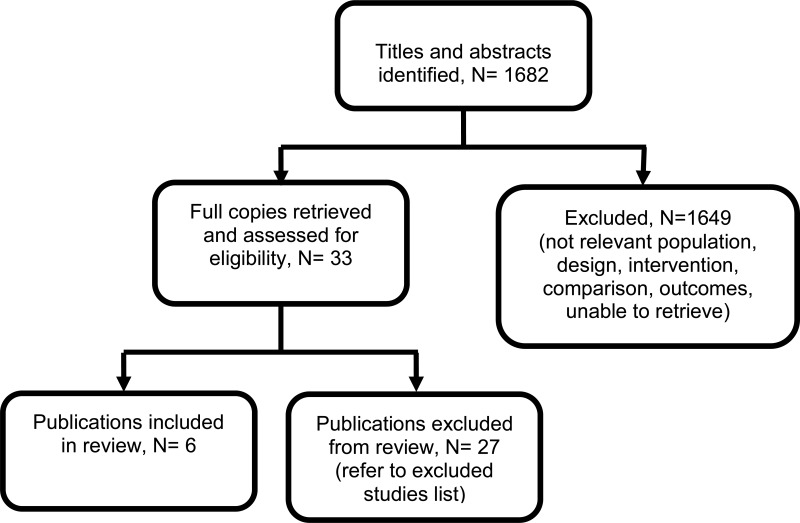
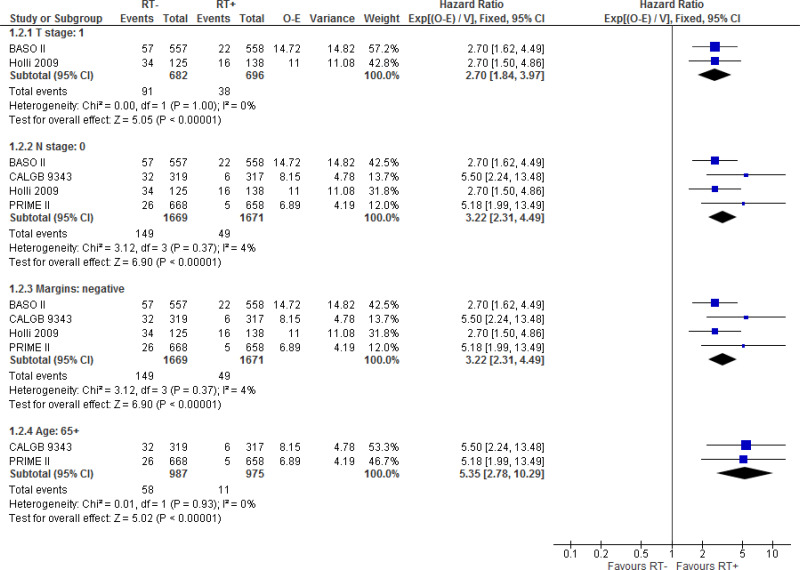
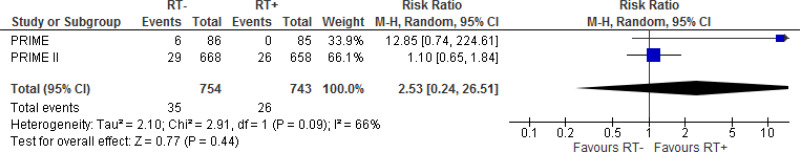
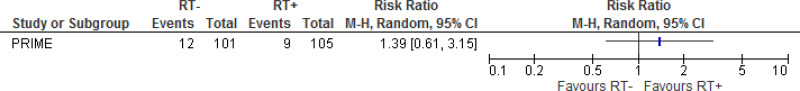
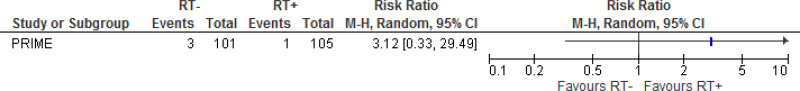
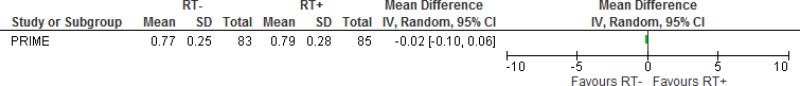
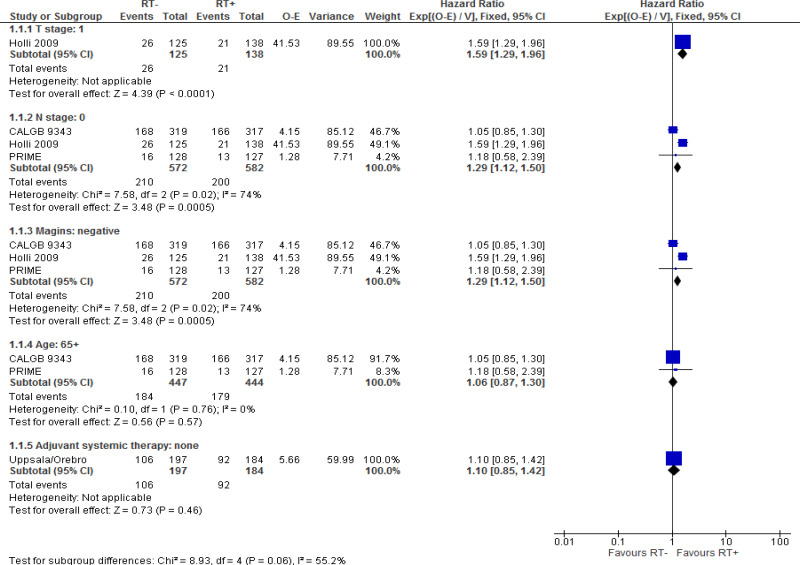
Six studies (N=3977) were included in the review (Blamey 1990; Holli 2009; Hughes 2013; Kunkler 2013; Wickberg 2014; Williams 2011). These studies report data from 6 trials: British Association of Surgical Oncologists (BASO) II trial (number of publications, k=1), Cancer and Leukemia Group B (CALGB) 9434 trial (k=1), Holli 2009 (k=1), Postoperative Radiotherapy in Minimum-Risk Elderly (PRIME; k=1), PRIME II (k=1), and Uppsala/Orebro trial (k=1). The BASO II, CALGB, and PRIME II trials compared BCS and endocrine therapy with or without whole breast radiotherapy, Holli 2009 and Uppsala/Orebro trial compared BCS and dissection of the axilla with or without whole breast radiotherapy, and the PRIME trial compared BCS alone with or without whole breast radiotherapy.
All studies reported data for subgroups of interest: T stage 1, (k=2), N stage 0 (k=5), age ≥65 years (k=3), no adjuvant systemic therapy received (k=1), and negative surgical margins (k=5).
The clinical studies included in this evidence review are summarised in Table 6 and evidence from these are summarised in the clinical GRADE evidence profile below (Table 7). See also the study selection flow chart in appendix C, forest plots in appendix E and study evidence tables in appendix D.
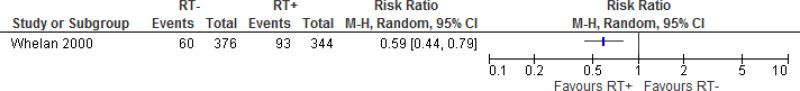
This review updates a question from the previous guideline CG80 (NICE 2009). Therefore, studies for this topic identified by the previous guideline are incorporated into forest plots, GRADE evidence profiles, and evidence statements. However, studies are not incorporated where there is more recent data available from the same trial, unless different outcomes are reported, or where a change in protocol from the previous guideline means that studies no longer meet inclusion criteria. Therefore, 21 articles included in the previous guideline were not incorporated into the current results for the following reasons: did not meet current inclusion criteria outlined in review protocol (k=16), more recent data available (k=2), insufficient presentation of results in original article to include in analysis (k=2), does not report data for any subgroups of interest so cannot inform current question (k=1). This resulted in only one article (Whelan 2000) from CG80 being added to the current evidence.
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K.
Summary of clinical studies included in the evidence review
See appendix D for full evidence tables.
Quality assessment of clinical studies included in the evidence review
The clinical evidence profile for this review question (breast radiotherapy after breast-conserving surgery) is presented in Table 7. The majority of the evidence is moderate or low quality. This is primarily due to small number of events of interest occurring.
See appendix F for full GRADE tables.
Economic evidence
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question. Economic modelling was not undertaken for this question because other topics were agreed as higher priorities for economic evaluation.
Evidence statements
Comparison 1. No whole breast radiotherapy versus whole breast radiotherapy
Critical outcomes
Local recurrence rate
- There is moderate quality evidence from 2 RCTs (N=1378) that whole breast radiotherapy produces clinically meaningful reductions in local recurrence at 10 to 12 year follow-up compared with no whole breast radiotherapy for women with T stage 1 invasive breast cancer.
- There is moderate quality evidence from 4 RCTs (N=3340) that whole breast radiotherapy produces clinically meaningful reductions in local recurrence at 5 to 12 year follow-up compared with no whole breast radiotherapy for women with N stage 0 invasive breast cancer.
- There is moderate quality evidence from 4 RCTs (N=3340) that whole breast radiotherapy produces clinically meaningful reductions in local recurrence at 5 to 12 year follow-up compared with no whole breast radiotherapy for women with invasive breast cancer and negative surgical margins following breast-conserving surgery.
- There is low quality evidence from 2 RCTs (N=1962) that whole breast radiotherapy produces clinically meaningful reductions in local recurrence at 5 to 10 year follow-up compared with no whole breast radiotherapy for women with invasive breast cancer aged 65 years and over.
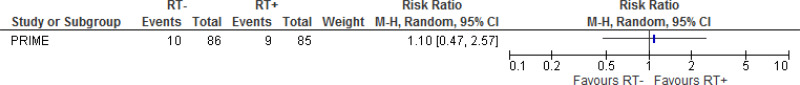
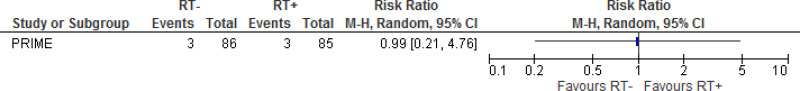
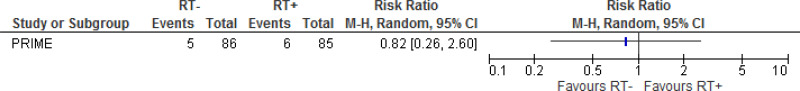
Treatment-related morbidity
- There is low quality evidence from 1 RCT (N=171) that whole breast radiotherapy reduces fractures (cause unspecified) at 5 year follow-up compared with no whole breast radiotherapy for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery. However, this was not statistically or clinically significant.
- There is moderate quality evidence from 1 RCT (N=171) that there is no effect of whole breast radiotherapy on congestive cardiac failure at 5 year follow-up for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery.
- There is low quality evidence from 1 RCT (N=171) that there was no effect of whole breast radiotherapy following breast-conserving surgery on myocardial infarction at 5 year follow-up for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins.
- There is low quality evidence from 2 RCTs (N=1497) that there was no effect of whole breast radiotherapy following breast-conserving surgery on secondary cancer (cause unspecified) at 5 year follow-up for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins.
Health-realted quality of life
- There is low quality evidence from 1 RCT (N=206) that whole breast radiotherapy produces clinically significant reductions in depression at 5 year follow-up compared with no whole breast radiotherapy for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery. However, this was not statistically significant.
- There is low quality evidence from 1 RCT (N=206) that whole breast radiotherapy produces clinically significant reductions in anxiety at 5 year follow-up compared with no whole breast radiotherapy for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery. However, this was not statistically significant.
- There is low quality evidence from 1 RCT (N=168) that there is no effect of radiation on HRQoL, as measured by EQ5D at 5 year follow-up, for women aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery.
- There is evidence from 1 RCT (N=720) that that whole breast radiotherapy produces clinically significant improvements in HRQoL, as measured by Breast Cancer Chemotherapy Questionnaire at 2 month follow-up, compared with no whole breast radiotherapy in women with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery. It was not possible to judge the overall quality of this evidence as it was included from the previous NICE guideline (CG80).
Important outcomes
Overall survival
- There is moderate quality evidence from 1 RCT (N=263) that whole breast radiotherapy produces clinically meaningful increases in overall survival at 12 year follow-up compared with no whole breast radiotherapy for women with T stage 1 invasive breast cancer.
- There is moderate quality evidence from 3 RCTs (N=1154) that whole breast radiotherapy produces clinically meaningful increases in overall survival at 5 to 12 year follow-up compared with no whole breast radiotherapy for women with N stage 0 invasive breast cancer.
- There is moderate quality evidence from 3 RCTs (N=1154) that whole breast radiotherapy produces clinically meaningful increases in overall survival at 5 to 12 year follow-up compared with no whole breast radiotherapy for women with invasive breast cancer and negative surgical margins following breast-conserving surgery.
- There is high quality evidence from 2 RCTs (N=891) that there was no effect of whole breast radiotherapy following breast-conserving surgery on overall survival at 5 to 10 year follow-up for women with invasive breast cancer aged 65 years and over.
- There is moderate quality evidence from 1 RCT (N=381) that there was no effect of whole breast radiotherapy on overall survival at 20 year follow-up for women with invasive breast cancer not receiving adjuvant systemic therapy.
Disease-free survival
- No evidence was found for this outcome.
Treatment-related mortality
- No evidence was found for this outcome.
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
As the purpose of this review was to determine if the use of radiotherapy could lead to a clinically meaningful reduction in recurrence of breast cancer after surgery in low risk people, and the risks and benefits of this approach were thought to be finely balanced, the committee prioritised local recurrence rate, treatment-related morbidity and health related quality of life as critical outcomes. Overall survival, disease-free survival and treatment-related mortality were selected as important outcomes.
There was no evidence available for disease-free survival and treatment-related mortality. There was also no evidence available for several of the subgroups of interest, specifically positive margins, oestrogen receptor (ER) status, human epidermal growth factor receptor 2 (HER2) status, grade, younger age, women who received adjuvant systemic therapy, T stage 2 and above and N stage 1 and above.
The quality of the evidence
The quality of the evidence for this review was assessed using GRADE. The evidence for local recurrence rate ranged from moderate to high across the different subgroups. The evidence for treatment-related morbidity and HRQoL was low quality. The evidence for overall survival across the different subgroups of interest ranged from moderate to high quality (with most of it being moderate quality).
The committee noted that there were high rates of performance bias in the studies due to the inability to blind for whole breast radiotherapy. However they considered this was unlikely to have a significant impact due to the objective nature of the outcomes. There were also high rates of imprecision due to small number of events of interest and small sample sizes.
The evidence showed that whole breast radiotherapy produces clinically meaningful reductions in local recurrence compared with no breast radiotherapy for people with T1 breast cancer, N0 breast cancer, people with invasive breast cancer and negative surgical margins following breast-conserving surgery, and people with invasive breast cancer aged 65 years and over. The committee noted that radiotherapy reduces recurrence rates for all women, but it was important to discuss the benefits and risks with individual patients. Some patients may be very anxious about recurrence, and want everything possible to reduce risk. However, some patients interpret risk more rationally and would rather avoid potential side effects when the risk of recurrence is small.
The evidence showed that whole breast radiotherapy produces clinically significant reductions in anxiety and depression compared with no whole breast radiotherapy for individuals aged 65 years and over with N stage 0 invasive breast cancer and negative surgical margins following breast-conserving surgery. However these data had low event rates and the symptoms of anxiety and depression were only measured at a single time point, not over a period of time. Therefore the Committee were uncertain about the actual effect size for this outcome.
The evidence showed that whole breast radiotherapy produces clinically meaningful increases in overall survival compared with no whole breast radiotherapy for individuals with T stage 1 invasive breast cancer, N stage 0 invasive breast cancer, and in individuals with invasive breast cancer and negative surgical margins following breast-conserving surgery. No clinically meaningful differences in overall survival were found in people aged 65 and over and individuals not receiving adjuvant systemic therapy
Benefits and harms
Given that the evidence showed clinically meaningful reductions in local recurrence, anxiety and depression and increases in overall survival with whole breast radiotherapy for people with invasive breast cancer who have had breast conserving surgery with clear margins, the Committee agreed to offer this treatment to this group.
The absolute risk of local recurrence at 5 years is very low, based on the evidence. There are harms associated with the use of radiotherapy and the benefits on overall survival are only realised in the longer term (5 and 10 year survival is the same with or without radiotherapy). Therefore the benefits of giving radiotherapy to those with a very low absolute risk of recurrence are less certain, particularly if they are willing to take endocrine therapy. Consequently the committee recommended there should be a discussion about the benefits and harms of whole breast radiotherapy with this group of people so that they can make an informed choice about their treatment. Important factors to include in the discussion are the local recurrence rates with and without radiotherapy, that overall survival is the same and that there is no increase in serious late effects with radiotherapy.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee discussed the potential costs and savings of recommendations and agreed that an increase in resources would not be required as the use of whole breast radiotherapy after breast-conserving surgery is already standard practice. Therefore it is possible that the recommendations could lead to cost savings if radiotherapy is omitted in low risk patients (following a discussion with the patient).
References
Blamey 2013
Blamey, R.W., Bates, T., Chetty, U., Duffy, S.W., Ellis, I.O., George, D., Mallon, E., Mitchell, M.J., Monypenny, I., Morgan, D.A., Macmillan, R.D., Patnick, J., Pinder, S.E., (2013) Radiotherapy or tamoxifen after conserving surgery for breast cancers of excellent prognosis: British Association of Surgical Oncology (BASO) II trial. European journal of cancer, 49, 2294–302. [PubMed: 23523089]Holli 2009
Holli, K., Hietanen, P., Saaristo, R., Huhtala, H., Hakama, M., Joensuu, H., (2009) Radiotherapy after segmental resection of breast cancer with favorable prognostic features: 12-year follow-up results of a randomized trial. Journal of Clinical Oncology, 27, 927–32. [PubMed: 19114687]Hughes 2013
Hughes, K.S., Schnaper, L.A., Bellon, J.R., Cirrincione, C.T., Berry, D.A., McCormick, B., Muss, H.B., Smith, B.L., Hudis, C.A., Winer, E.P., Wood, W.C., (2013) Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. Journal of Clinical Oncology, 31, 2382–7. [PMC free article: PMC3691356] [PubMed: 23690420]Kunkler 2015
Kunkler, I.H., Williams, L.J., Jack, W.J., Cameron, D.A., Dixon, J.M., (2015) Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. The Lancet. Oncology, 16, 266–73. [PubMed: 25637340]NICE 2009
National Institute for Health and Clinical Excellence. (2009) Early and locally advanced breast cancer: diagnosis and treatment. NICE guideline (CG80). [PubMed: 19167201]Whelan 2000
Whelan, T. J., Levine, M., Julian, J., Kirkbride, P., Skingley, P. (2000). The effects of radiation therapy on quality of life of women with breast carcinoma: Results of a randomized trial. Cancer, 88, 2260–2266. [PubMed: 10820347]Wickberg 2014
Wickberg, A., Holmberg, L., Adami, H.O., Magnuson, A., Villman, K., Liljegren, G., (2014) Sector resection with or without postoperative radiotherapy for stage I breast cancer: 20-year results of a randomized trial. Journal of Clinical Oncology, 32, 791–7. [PubMed: 24493730]Williams 2011
Williams, L.J., Kunkler, I.H., King, C.C., Jack, W., Pol, M., (2011) A randomised controlled trial of post-operative radiotherapy following breast-conserving surgery in a minimum-risk population. Quality of life at 5 years in the PRIME trial. Health technology assessment (Winchester, England), 15, i–xi, 1–57. [PubMed: 21366974]
Review question 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Introduction
Whole breast radiotherapy (WBRT) is the current standard adjuvant treatment option for most women with early invasive breast cancer after breast conserving surgery (BCS). Multiple retrospective studies and an overview of randomized trials have established the equivalence of this treatment approach compared with mastectomy in terms of both disease-free and overall survival.
WBRT halves the risk of local recurrence. However, local recurrence rates have fallen dramatically over the last 30 years, so that the absolute benefit of WBRT for some women may not outweigh the potential risks (normal tissue toxicity, cardiac morbidity, second cancers). For many women, increasingly diagnosed with small screen-detected cancers, it is the late complications of radiotherapy (RT), rather than the risk of local recurrence, that is their predominant concern. Whilst the proportional benefit of radiotherapy is similar across all subgroups of women with breast cancer, the absolute benefit for women with good prognosis tumours is small. The risk of true local recurrence is highest in the area of the breast close to the site of the original tumour raising the possibility that there are women at low risk of local recurrence for whom treatment of the whole breast volume and surrounding tissue is not necessary.
The aim of this review is to determine if there is a group of women in whom partial breast radiotherapy (PBR) would offer a better risk-benefit approach than whole breast radiotherapy.
PICO table
See Table 8 for a summary of the population, intervention, comparison and outcome (PICO) characteristics of this review.
For full details see review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual; see the methods chapter for further information.
Declarations of interest were recorded according to NICE’s 2014 conflicts of interest policy.
Clinical evidence
Included studies
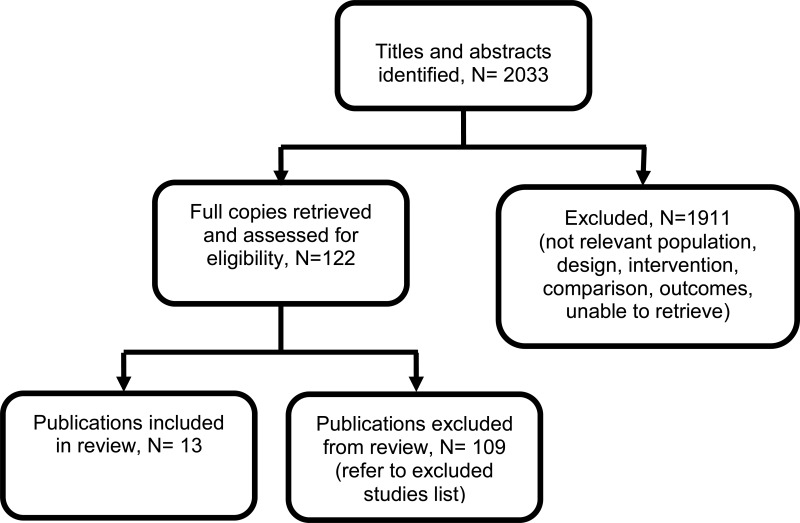
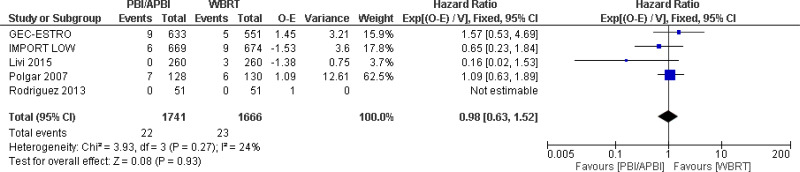
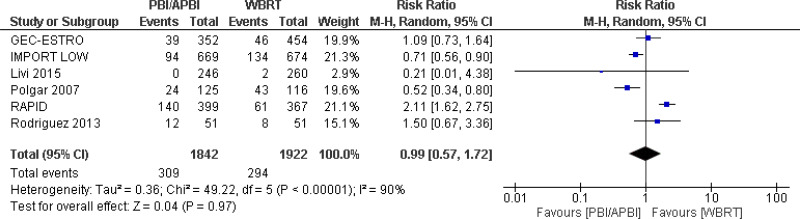
Six randomised trials (N=6215), reported on in 12 publications (The Groupe Européen de Curiethérapie and the European SocieTy for Radiotherapy & Oncology [GEC-ESTRO; Ott 2016; Polgar 2017; Strnad 2016]; Intensity Modulated and Partial Organ Radiotherapy [IMPORT-LOW; Coles 2017] Livi 2015 [Livi 2010; Livi 2015]; Polgár 2007 [Lovey 2007; Polgar 2007; Polgar 2013]; Randomized Trial of Accelerated Partial Breast Irradiation [RAPID; Olivotto 2013]; Rodriguez 2013 [Rodriguez 2013]), and 1 systematic review (Hickey 2016) were included in the review.
Evidence from these are summarised in Table 9 and the clinical GRADE evidence profile in Table 10.
See also the study selection flow chart in appendix C, forest plots in appendix E and study evidence tables in appendix D.
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K.
Summary of clinical studies included in the evidence review
See appendix D for full evidence tables.
Quality assessment of clinical studies included in the evidence review
The clinical evidence profile for this review question (partial-breast radiotherapy versus whole-breast radiotherapy after breast-conserving surgery) is presented in Table 10. The majority of the evidence is moderate or low quality. This is primarily due to small number of events of interest occurring.
See appendix F for full GRADE tables.
Economic evidence
Included studies
One relevant study was identified in a literature review of published cost-effectiveness analyses on this topic; Shah 2013 (see appendix H and appendix I for summary and full evidence tables). The study considered the cost-effectiveness of accelerated partial breast radiotherapy (APBRT) techniques in comparison to whole beam radiotherapy (WBRT) techniques. The analysis was a cost-utility analysis measuring effectiveness in terms of quality adjusted life years (QALYs).
Excluded studies
See supplement 1: Health economics for the list of excluded studies.
Summary of studies included in the economic evidence review
The base case results of Shah 2013 showed that all APBRT techniques were cost-effective and indeed dominant in comparison to whole beam intensity modulated radiotherapy (IMRT) techniques (i.e. less costly and more effective). In comparison to WBRT with 3D conformal radiotherapy (CRT), APBRT techniques with IMRT or 3DCRT were again found to be dominant. However, other forms of APBRT were found to be more costly and more effective with ICERs of $12,514, $67,329 and $557 per QALY for single lumen, multi lumen and interstitial APBRT techniques, respectively.
The analysis was deemed to be only partially applicable to the decision problem in the UK setting as it was conducted from the perspective of the US health care system. Furthermore, serious limitations were identified in the analysis. Most notably, uncertainty around the base case estimates was not assessed as no deterministic or probabilistic sensitivity analyses were conducted.
Overall, the analysis appears to suggest that accelerated partial breast radiotherapy may be cost-effective in comparison to whole beam radiotherapy. However, further research would be required before drawing decisive conclusions around the cost-effectiveness of accelerated partial breast radiotherapy in the UK context.
Evidence statements
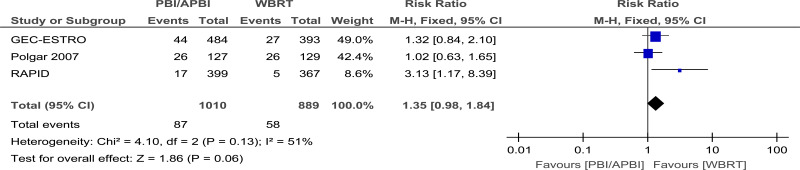
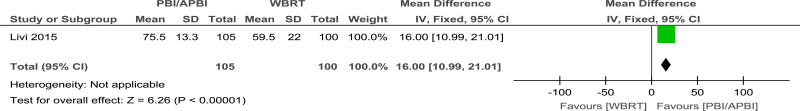
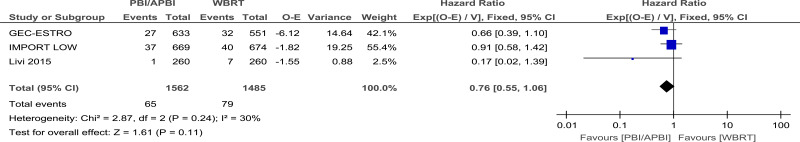
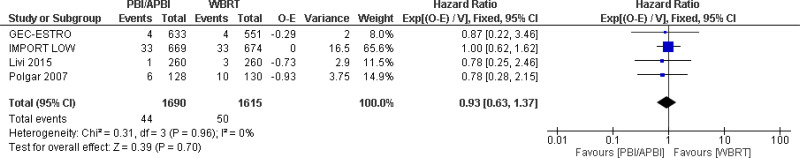
Comparison 1. Partial breast radiotherapy versus whole breast radiotherapy
Critical outcomes
Local recurrence
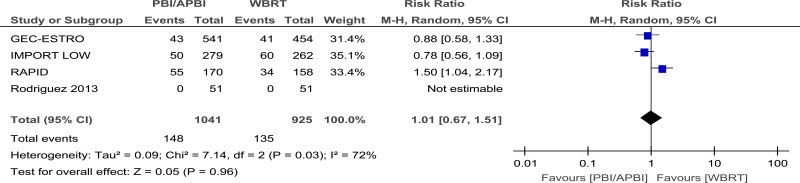
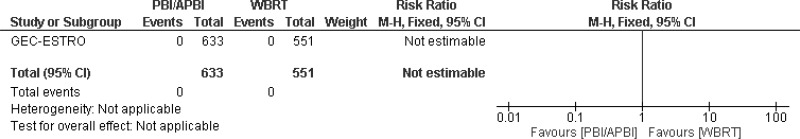
- There is low quality evidence from 5 RCTs (N=3407) that there is no effect of a difference on local recurrence free survival at 5 to 10 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
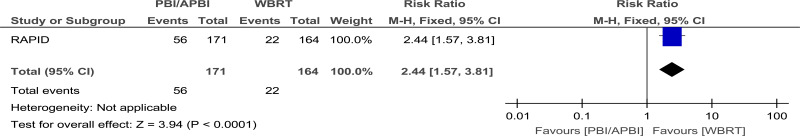
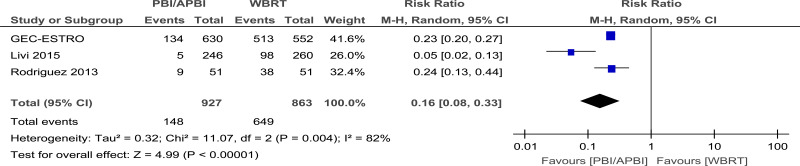
Treatment-related morbidity
- There is very low quality evidence from 6 RCTs (N=3764) that there is no clinically important difference in physician-reported cosmesis at 5 years follow-up between women with invasive breast cancer who received partial breast radiotherapy compared with those who received whole breast radiotherapy.
- There is very low quality evidence from 4 RCTs (N=1966) that there is no clinically important difference in patient-reported cosmesis at 5 years follow-up between women with invasive breast cancer who received partial breast radiotherapy compared with those who received whole breast radiotherapy.
- There is low quality evidence from 1 RCT (N=335) that partial breast radiotherapy produces clinically meaningful reductions in nurse-reported cosmesis at 5 years follow-up compared with whole breast radiotherapy for women with invasive breast cancer.
- There is low quality evidence from 3 RCTs (N=1790) that partial breast radiotherapy produces clinically meaningful reductions in acute radiotherapy skin toxicity at 0 to 90 days follow-up compared with whole breast radiotherapy for women with invasive breast cancer.
- There is very low quality evidence from 5 RCTs (N=3175) that there is no clinically important difference in late radiotherapy skin toxicity at 3 to 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
- There is very low quality evidence from 3 RCTs (N=2475) that there is no clinically important difference in breast pain at 3 to 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
- There is low quality evidence from 3 RCTs (N=1899) that there is no clinically important difference in fat necrosis at 3 to 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
Health-realted quality of life
- There is low quality evidence from 1 RCT (N=205) that that partial breast radiotherapy produces clinically important improvements in HRQoL, as measured using EORTC QLQC30 and BR23 module at 2 year follow-up, compared with whole breast radiotherapy for women with invasive breast cancer.
Important outcomes
Overall survival
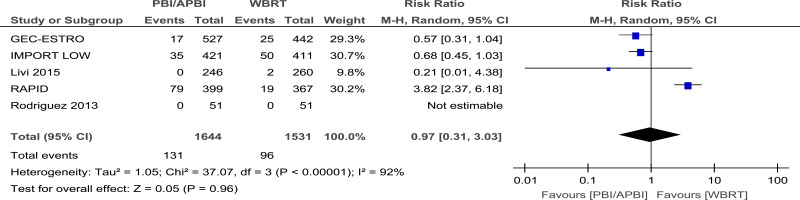
- There is moderate quality evidence from 3 RCTs (N=3047) that there is no clinically important difference in overall survival at 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
Disease-free survival
- There is moderate quality evidence from 4 RCTs (N=3305) that there is no clinically important difference in disease-free survival at 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
- There is moderate quality evidence from 4 RCTs (N=3305) that there is no clinically important difference in distant metastasis-free survival at 5 years follow-up for women with invasive breast cancer when comparing partial breast radiotherapy with whole breast radiotherapy.
Treatment-related mortality
- There is moderate quality evidence from 1 RCT (N=1184) of no clinically important difference in treatment-related mortality at 5 year follow-up for women with invasive breast cancer, but no treatment related deaths were observed in this study.
Economic evidence statement
- Evidence from one cost-utility analysis) showed that all APBRT techniques were dominant in comparison to WBRT with IMRT. APBRT using IMRT or 3DCRT were found to be dominant in comparison to WBRT with CRT while other APBRT techniques were found to be more costly and more effective with ICERs of $12,514, $67,329 and $557 per QALY for single lumen, multi lumen and interstitial APBRT techniques, respectively. The analysis was partially applicable with serious limitations.
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
The critical outcomes were local recurrence, treatment-related morbidity and health related quality of life. This is because breast radiotherapy following surgery is done to reduce the risk of local recurrence and by irradiating less of the breast there is a potential impact on treatment-related morbidity and health related quality of life. Overall survival, disease-free survival and treatment related mortality were considered important outcomes, because the group offered partial breast radiotherapy are typically at low risk of disease recurrence and even lower risk of death from breast cancer.
The quality of the evidence
The evidence came from randomised trials and ranged from very low to high quality. The major issue was heterogeneity in treatment-related morbidity with some trials favouring partial breast RT but others favouring whole breast RT. This was most likely due to the different surgical and partial breast radiotherapy techniques used in the trials, for example the use of accelerated partial breast radiotherapy. For this reason the committee based their recommendations on the trials with surgical techniques, radiotherapy regimens and adjuvant endocrine therapy most applicable to the UK.
The evidence review aimed to identify a group with a particularly low absolute risk of local recurrence who would be best suited to partial breast radiotherapy. The inclusion criteria of the trials meant that only low risk patients were included and there were too few cases of local recurrence to define such a group. For this reason the committee used the trial entry criteria of the most relevant trial (IMPORT-LOW) in their recommendation: women aged 50 and over with tumours that are less than or equal to 3 cm, N0, oestrogen receptor (ER)-positive, human epidermal growth factor receptor 2 (HER2)-negative and grade 1 to 2.
The committee acknowledged that follow-up in the trial most relevant to the UK setting had not yet reached 10 years and that differences in local recurrence may become evident with longer follow-up. For this reason they did not make a strong recommendation in favour of partial breast radiotherapy
Benefits and harms
The benefits of partial breast radiotherapy accrue from irradiating less tissue. This results in fewer acute adverse effects like skin toxicity and potentially fewer late adverse effects involving the heart and lungs. The potential harm of partial breast radiotherapy, as opposed to whole breast radiotherapy, is there may be an increased rate of local recurrence requiring further treatment. The evidence, however, suggests the absolute rates of local recurrence are very low in this selected patient group and are equivalent between partial breast and whole breast radiotherapy, at least up to five years.
The committee were also aware of the Royal College of Radiologists 2016 consensus statement on partial breast radiotherapy after breast-conserving surgery which recommended its use in women aged 50 and over with tumours that are less than or equal to 3 cm, N0, ER-positive, HER2-negative and grade 1 to 2.
Cost effectiveness and resource use
The committee considered the results of the cost-utility study (Shah 2013) identified in the literature review conducted for this topic. The analysis was thought to have demonstrated the potential cost-effectivenes of accelerated partial breast radiotherapy in comparison to whole beam therapy. However, as the analysis was not directly applicable to the UK context, it was not thought to give a reliable estimate of cost-effectiveness in the UK context.
In terms of the potential resource impact, the committee considered there would be a potential reduction in costs of treating late effects if partial breast radiotherapy were used but there may also be increased costs in treating local recurrence beyond five years, the balance of these is as yet unknown. The use of partial breast radiotherapy delivered as external beam radiotherapy would not have any implications on planning time, delivery time or patient counselling time, and is already used in most centres in the UK.
Other factors the committee took into account
The committee excluded those people with lobular carcinoma from the recommendation for partial breast radiotherapy due to the increased risk of multicentricity and therefore local recurrence in this group.
The committee were aware that NICE were in the process of developing separate guidance on the use of the intrabeam radiotherapy system in early breast cancer and so intrabeam radiotherapy was not considered in this review.
References
Coles 2017
Coles, C.E., Griffin, C.L., Kirby, A.M., Titley, J., Agrawal, R.K., Alhasso, A., Bhattacharya, I.S., Brunt, A.M., Ciurlionis, L., Chan, C., Donovan, E.M., Emson, M.A., Harnett, A.N., Haviland, J.S., Hopwood, P., Jefford, M.L., Kaggwa, R., Sawyer, E.J., Syndikus, I., Tsang, Y.M., Wheatley, D.A., Wilcox, M., Yarnold, J.R., Bliss, J.M. et al (2017) Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. The Lancet, 390, 1048–1060. [PMC free article: PMC5594247] [PubMed: 28779963]Hickey 2016
Hickey, B.E., Lehman, M., Francis, D.P., See, A.M., Partial breast irradiation for early breast cancer. (2016) Cochrane Database of Systematic Reviews [PMC free article: PMC6457864] [PubMed: 27425375]Livi 2010
Livi, L., Buonamici, F. B., Simontacchi, G., Scotti, V., Fambrini, M., Compagnucci, A., Paiar, F., Scoccianti, S., Pallotta, S., Detti, B., Agresti, B., Talamonti, C., Mangoni, M., Bianchi, S., Cataliotti, L., Marrazzo, L., Bucciolini, M., Biti, G. (2010) Accelerated Partial Breast Irradiation With IMRT: New Technical Approach and Interim Analysis of Acute Toxicity in a Phase III Randomized Clinical Trial. International Journal of Radiation Oncology Biology Physics, 77, 509–515. [PubMed: 19700248]Livi 2015
Livi, L., Meattini, I., Marrazzo, L., Simontacchi, G., Pallotta, S., Saieva, C., Paiar, F., Scotti, V., De Luca Cardillo, C., Bastiani, P., Orzalesi, L., Casella, D., Sanchez, L., Nori, J., Fambrini, M., Bianchi, S. (2015) Accelerated partial breast irradiation using intensity-modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomised controlled trial. European Journal of Cancer, 51, 451–463. [PubMed: 25605582]Lovey 2007
Lovey, K., Fodor, J., Major, T., Szabo, E., Orosz, Z., Sulyok, Z., Janvary, L., Frohlich, G., Kasler, M., Polgar, C. (2007) Fat Necrosis After Partial-Breast Irradiation With Brachytherapy or Electron Irradiation Versus Standard Whole-Breast Radiotherapy-4-Year Results of a Randomized Trial. International Journal of Radiation Oncology Biology Physics, 69, 724–731. [PubMed: 17524571]Meattini 2017
Meattini, I., Saieva, C., Miccinesi, G., Desideri, I., Francolini, G., Scotti, V., Marrazzo, L., Pallotta, S., Meacci, F., Muntoni, C., Bendinelli, B., Sanchez, L. J., Bernini, M., Orzalesi, L., Nori, J., Bianchi, S., Livi, L. (2017) Accelerated partial breast irradiation using intensity modulated radiotherapy versus whole breast irradiation: Health-related quality of life final analysis from the Florence phase 3 trial. European Journal of Cancer, 76, 17–26. [PubMed: 28262584]Olivotto 2013
Olivotto, I. A., Whelan, T. J., Parpia, S., Kim, D. H., Berrang, T., Truong, P. T., Kong, I., Cochrane, B., Nichol, A., Roy, I., Germain, I., Akra, M., Reed, M., Fyles, A., Trotter, T., Perera, F., Beckham, W., Levine, M. N., Julian, J. A. (2013) Interim cosmetic and toxicity results from RAPID: A randomized trial of accelerated partial breast irradiation using three-dimensional conformal external beam radiation therapy. Journal of Clinical Oncology, 31, 4038–4045. [PubMed: 23835717]Ott 2016
Ott, O. J., Strnad, V., Hildebrandt, G., Kauer-Dorner, D., Knauerhase, H., Major, T., Lyczek, J., Guinot, J. L., Dunst, J., Miguelez, C. G., Slampa, P., Allgauer, M., Lossl, K., Polat, B., Kovacs, G., Fischedick, A. R., Wendt, T. G., Fietkau, R., Kortmann, R. D., Resch, A., Kulik, A., Arribas, L., Niehoff, P., Guedea, F., Schlamann, A., Potter, R., Gall, C., Malzer, M., Uter, W., Polgar, C. (2016) GEC-ESTRO multicenter phase 3-trial: Accelerated partial breast irradiation with interstitial multicatheter brachytherapy versus external beam whole breast irradiation: Early toxicity and patient compliance. Radiotherapy and Oncology, 120, 119–123. [PubMed: 27422584]Polgar 2007
Polgar, C., Fodor, J., Major, T., Nemeth, G., Lovey, K., Orosz, Z., Sulyok, Z., Takacsi-Nagy, Z., Kasler, M. (2007) Breast-Conserving Treatment With Partial or Whole Breast Irradiation for Low-Risk Invasive Breast Carcinoma-5-Year Results of a Randomized Trial. International Journal of Radiation Oncology Biology Physics, 69, 694–702. [PubMed: 17531400]Polgar 2013
Polgar, C., Fodor, J., Major, T., Sulyok, Z., Kasler, M. (2013) Breast-conserving therapy with partial or whole breast irradiation: Ten-year results of the Budapest randomized trial. Radiotherapy and Oncology, 108, 197–202. [PubMed: 23742961]Polgar 2017
Polgar, C., Ott, O. J., Hildebrandt, G., Kauer-Dorner, D., Knauerhase, H., Major, T., Lyczek, J., Guinot, J. L., Dunst, J., Miguelez, C. G., Slampa, P., Allgauer, M., Lossl, K., Polat, B., Kovacs, G., Fischedick, A. R., Fietkau, R., Resch, A., Kulik, A., Arribas, L., Niehoff, P., Guedea, F., Schlamann, A., Potter, R., Gall, C., Uter, W., Strnad, V. (2017) Late side-effects and cosmetic results of accelerated partial breast irradiation with interstitial brachytherapy versus whole-breast irradiation after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: 5-year results of a randomised, controlled, phase 3 trial. The Lancet Oncology, 18, 259–268. [PubMed: 28094198]Rodriguez 2013
Rodriguez, N., Sanz, X., Dengra, J., Foro, P., Membrive, I., Reig, A., Quera, J., Fernandez-Velilla, E., Pera, O., Lio, J., Lozano, J., Algara, M. (2013) Five-year outcomes, cosmesis, and toxicity with 3-dimensional conformal external beam radiation therapy to deliver accelerated partial breast irradiation. International Journal of Radiation Oncology Biology Physics, 87, 1051–1057. [PubMed: 24161420]Shah 2013
Shah, C. Cost-efficacy of acceleration partial-breast irradiation compared with whole-breast irradiation. Breast Cancer Research & Treatment, 2013. 138(1): p. 127–35. [PubMed: 23329353]Strnad 2016
Strnad, V., Ott, O. J., Hildebrandt, G., Kauer-Dorner, D., Knauerhase, H., Major, T., Lyczek, J., Guinot, J. L., Dunst, J., Miguelez, C. G., Slampa, P., Allgauer, M., Lossl, K., Polat, B., Kovacs, G., Fischedick, A. R., Wendt, T. G., Fietkau, R., Hindemith, M., Resch, A., Kulik, A., Arribas, L., Niehoff, P., Guedea, F., Schlamann, A., Potter, R., Gall, C., Malzer, M., Uter, W., Polgar, C. (2016) 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: A randomised, phase 3, non-inferiority trial. The Lancet, 387, 229–238. [PubMed: 26494415]
Review question 8.4. What are the indications for radiotherapy to internal mammary nodes?
Introduction
Targeting clinically negative internal mammary nodes (IMN) with radiotherapy as part of the post-operative treatment of breast cancer is not commonly recommended in the UK. Notwithstanding the high rates of subclinical IMN involvement and a prior meta-analysis which demonstrated that regional node irradiation in conjunction with chest wall radiotherapy improved outcomes, there remains uncertainty about the benefits of this approach as isolated parasternal relapses are rare. Furthermore, until recently it has proven difficult to encompass the IMN using the available radiotherapy technologies whilst respecting safe dose limits to the heart and lungs.
The previous guideline CG80 (NICE 2009) recommended that radiotherapy to the IMN chain should not be offered after breast surgery. Recent randomised controlled trials (RCTs) and 1 large case controlled study have led to a reappraisal of this approach, and this review aims to revisit the potential indications for the inclusion of IMN in the radiation treatment volume
PICO table
See Table 11 for a summary of the population, intervention, comparison and outcome (PICO) characteristics of this review.
For full details see review protocol in appendix A.
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual; see the methods chapter for further information.
Declarations of interest were recorded according to NICE’s 2014 conflicts of interest policy.
Clinical evidence
Included studies
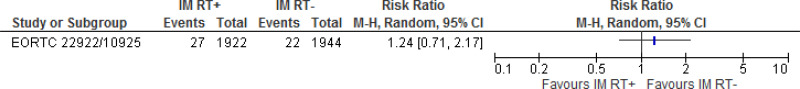
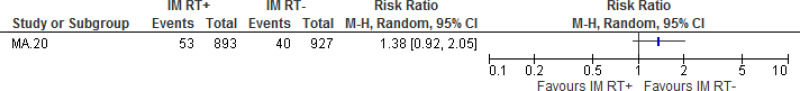
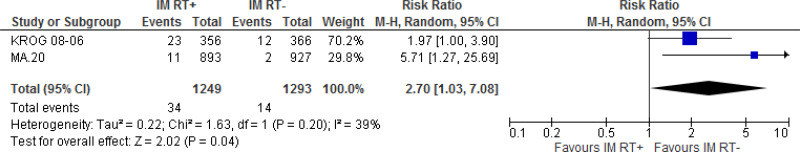
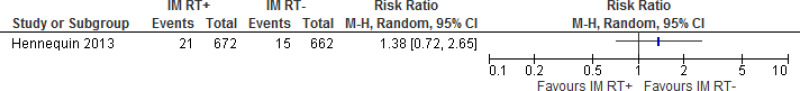
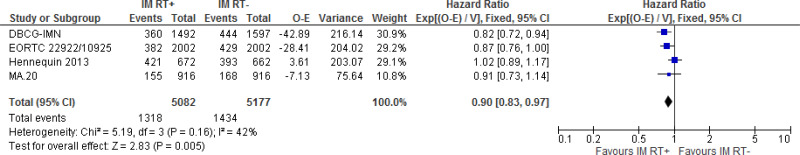
Six studies (n=10,981) were included in the review (Choi 2016; Hennequin 2013; Matzinger 2010; Poortmans 2015; Thorsen 2016; Whelan 2015), which report data from 5 trials: Danish Breast Cancer Group – Internal Mammary Node (DBCG-IMN) trial (k=1), European Organisation for Research and Treatment of Cancer (EORTC) trial 22922/10925 (k=2), Hennequin, Bossard 2013 (k=1), Korean Radiation Oncology Group (KROG) 08-06 trial (k=1), MA.20 trial (k=1).
The DBCG-IMN trial compared radiotherapy to the breast/chest wall, scar, and the supraclavicular, infraclavicular and axially lymph nodes with or without internal mammary (IM) lymph nodes, the EORTC trial 22922/10925 compared radiotherapy to the IM and medial supraclavicular (MS) lymph nodes with no radiation to the IM and MS lymph nodes, Hennequin 2013 compared radiotherapy to the chest wall, supraclavicular nodes, and apical axillary nodes (for pN+ cases) with or without radiotherapy to the IM lymph nodes, KROG-08-06 trial compared radiotherapy to the breast, IM and supraclavicular lymph nodes with radiotherapy to the breast and supraclavicular lymph nodes only, and MA.20 compared whole breast radiation with or without radiation to the IM, supraclavicular and axillary lymph nodes.
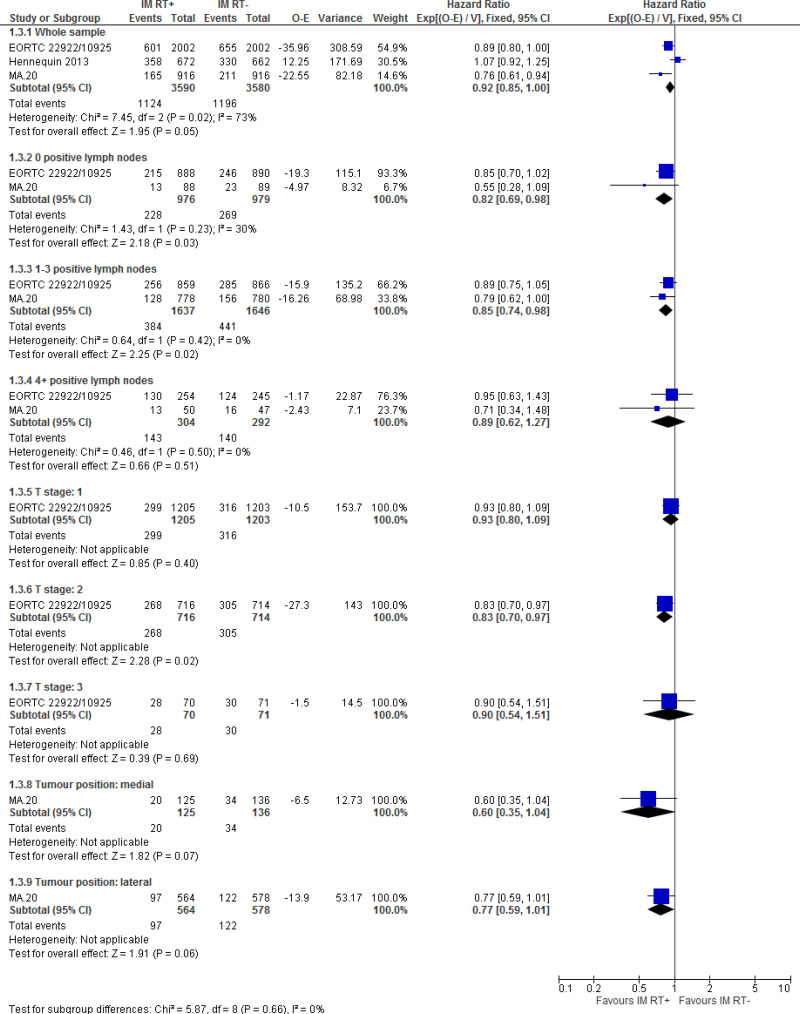
Only 2 studies (Poortmans 2015; Whelan 2015) reported data for critical outcomes by subgroups of interest: 0 lymph node metastases (k=2), 1–3 lymph node metastases (k=2), 4+ lymph node metastases (k=2), T stage 1 (k=1), T stage 2 (k=1), T stage 3 (k=1), medial tumour position (k=1), and lateral tumour position (k=1).
The clinical studies included in this evidence review are summarised in Table 12 and evidence from these are summarised in the clinical GRADE evidence profile below (Table 13). See also the study selection flow chart in appendix C, forest plots in appendix E, and study evidence tables in appendix D.
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K.
Summary of clinical studies included in the evidence review
Quality assessment of clinical studies included in the evidence review
The clinical evidence profile for this review is presented in Table 13. The majority of the evidence is moderate or low quality. This is primarily due to imprecision around the estimates due to a small number of events of interest and wide confidence intervals.
See appendix F for full GRADE tables.
Economic evidence
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question. Economic modelling was not undertaken for this question because other topics were agreed as higher priorities for economic evaluation.
Evidence statements
Comparison 1. Radiotherapy to the internal mammary nodes versus no radiotherapy to the internal mammary nodes
Critical outcomes
Locoregional recurrence rate
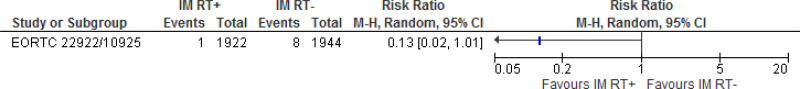
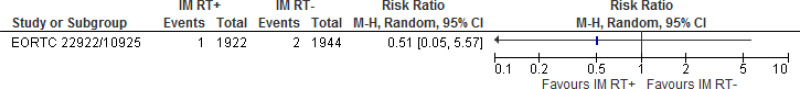
- There is moderate quality evidence from 1 RCT (N=1832) that radiotherapy to the internal mammary nodes produces clinically meaningful reductions in locoregional recurrence following surgery for early invasive breast cancer compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
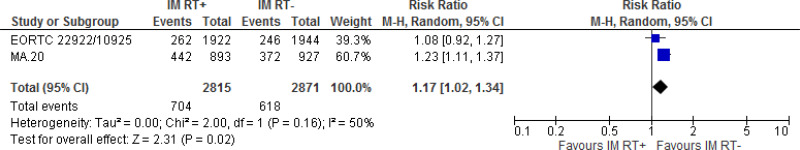
Disease-free survival
- There is moderate quality evidence from 3 RCTs (N=7170) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in disease-free survival following surgery for early invasive breast cancer compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
- There is high quality evidence from 2 RCTs (N=1955) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in disease-free survival following surgery for individuals with 0 positive lymph nodes compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
- There is high quality evidence from 2 RCTs (N=3283) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in disease-free survival following surgery for individuals with 1–3 positive lymph nodes compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
- There is moderate quality evidence from 2 RCTs (N=596) that there is no clinically important effect of radiotherapy to the internal mammary nodes on disease-free survival at 10 year follow-up for individuals with 4 or more positive lymph nodes.
- There is high quality evidence from 1 RCT (N=2408) that there is no clinically important effect of radiotherapy to the internal mammary nodes on disease-free survival at 10 year follow-up for individuals with T stage 1 invasive breast cancer.
- There is high quality evidence from 1 RCT (N=1430) that radiotherapy to the internal mammary nodes produces clinically significant increases in disease-free survival following surgery for individuals with T stage 2 invasive breast cancer compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
- There is low quality evidence from 1 RCT (N=141) that there is no clinically important effect of radiotherapy to the internal mammary nodes on disease-free survival at 10 year follow-up for individuals with T stage 3 invasive breast cancer.
- There is low quality evidence from 1 RCT (N=261) that there is no clinically important effect of radiotherapy to the internal mammary nodes on disease-free survival at 10 year follow-up for individuals with medially located invasive breast cancer.
- There is moderate quality evidence from 1 RCT (N=1142) that there is no clinically important effect of radiotherapy to the internal mammary nodes on disease-free survival at 10 year follow-up for individuals with laterally located invasive breast cancer.
Treatment-related morbidity
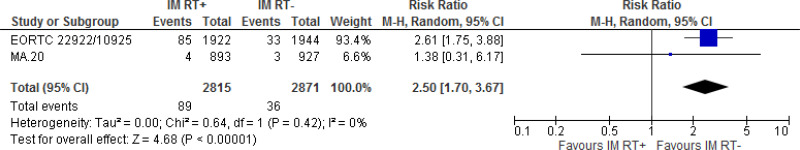
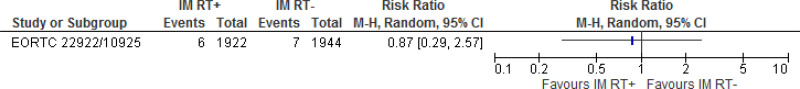
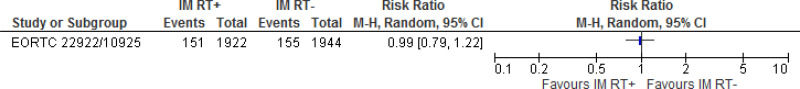
- There is moderate quality evidence from 2 RCTs (N=2542) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in acute radiation pneumonitis (within 3 to 6 months of completing radiotherapy) for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
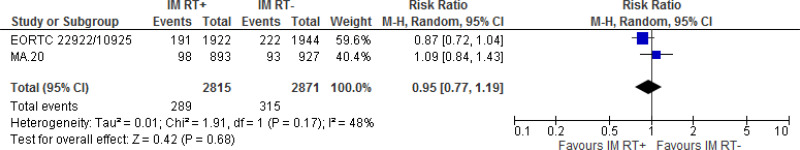
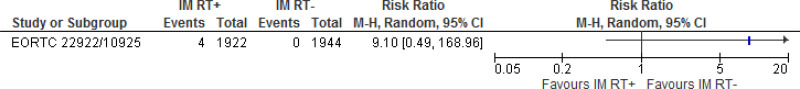
- There is high quality evidence from 2 RCTs (N=5686) that there is no effect of radiotherapy to the internal mammary nodes on secondary cancer (potentially radiation-induced) at 10 year follow-up for individuals with invasive breast cancer.
- There is low quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful reductions in arm/shoulder function impairment at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is moderate quality evidence from 2 RCTs (N=5686) that there is no effect of radiotherapy to the internal mammary nodes on fatigue at 3 month to 3 year follow-up for individuals with invasive breast cancer.
- There is low quality evidence from 1 RCT (N=1820) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in grade 2+ acute pain (site not specified; within 3 months of completing radiotherapy) for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is high quality evidence from 2 RCTs (N=5686) that there is no effect of radiotherapy to the internal mammary nodes on skin toxicity at 3 month to 3 year follow-up for individuals with invasive breast cancer.
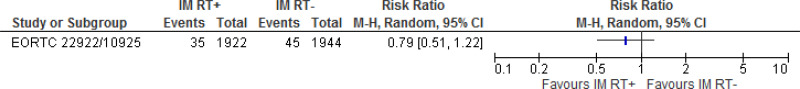
- There is moderate quality evidence from 2 RCTs (N=5686) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in lung toxicity at 3 to 10 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes.
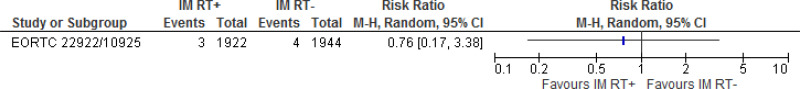
- There is low quality evidence from 3 RCTs (N=7020) that there is no effect of radiotherapy to the internal mammary nodes on cardiac toxicity at 10 year follow-up for individuals with invasive breast cancer.
- There is moderate quality evidence from 1 RCT (N=1820) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in grade 2+ lymphoedema at 10 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes.
- There is low quality evidence from 1 RCT (N=1334) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in grade 3+ morbidity as measured by the SOMA-LENT scale at 10 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is moderate quality evidence from 1 RCT (N=3866) that there is no effect of radiotherapy to the internal mammary nodes on mastitis at 3 year follow-up for individuals with invasive breast cancer.
- There is moderate quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful reductions in breast infection at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is moderate quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful reductions in radionecrosis at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is low quality evidence from 1 RCT (N=3866) that there is no effect of radiotherapy to the internal mammary nodes on osteonecrosis at 3 year follow-up for individuals with invasive breast cancer.
- There is moderate quality evidence from 1 RCT (N=3866) that there is no effect of radiotherapy to the internal mammary nodes on oedema at 3 year follow-up for individuals with invasive breast cancer.
- There is low quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful reductions in breast/chest wall pain at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is moderate quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in retrosternal pain at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
- There is moderate quality evidence from 1 RCT (N=3866) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in dysphagia at 3 year follow-up for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes. However, this was not statistically significant.
Important outcomes
Overall survival
- There is high quality evidence from 4 RCTs (N=10,259) that radiotherapy to the internal mammary nodes produces clinically meaningful increases in overall survival following surgery for individuals with invasive breast cancer compared with no radiotherapy to the internal mammary nodes at 10 year follow-up.
Health-related quality of life
- No evidence was found for this outcome.
The committee’s discussion of the evidence
Interpreting the evidence
The outcomes that matter most
The committee prioritised locoregional recurrence rate, disease-free survival and treatment-related morbidity as critical outcomes. Locoregional recurrence and disease-free survival were prioritised ahead of overall survival as the time taken for overall survival events to occur means there is less data available and it is less commonly examined by trials. Overall survival and health-related quality of life were selected as important outcomes.
There was no evidence available for health-related quality of life.
The quality of the evidence
The quality of the evidence for this review was assessed using GRADE. The evidence for locoregional recurrence was moderate quality. For disease-free survival the evidence was moderate quality for the sample as a whole, but the data for different subgroups ranged from low to high quality (with most of it being either moderate or high). The evidence for treatment related morbidity ranged from low to high quality with most of it being either low or moderate quality. Overall survival evidence was high quality.
It was noted that there were high rates of performance bias due to no blinding in studies. However it was agreed that this was unlikely to have a significant impact on the results due to the objective nature of the outcomes for which there was evidence available. It was also noted that there were high rates of imprecision for locoregional recurrence and treatment-related morbidities due to small number of events of interest and wide confidence intervals.
The committee noted that only two studies (Poortmans 2015; Whelan 2015) reported data for critical outcomes by the subgroups of interest. There was also no subgroup data based on laterality which could impact on toxicity.
The committee also noted that most of the studies had used internal mammary chain radiotherapy in conjunction with radiotherapy to the supraclavicular fossa. As a result it was difficult to determine the relative benefit of treatment solely to the internal mammary chain from these studies. Therefore the committee based their recommendations on the evidence from the one study that only irradiated the internal mammary nodes (rather than also irradiating the supraclavicular fossa). As this study reported overall survival, which was an important, not a critical outcome, the committee made a weaker recommendation.
Only one study included node negative patients and this gave radiotherapy to both trial arms. Therefore the committee agreed not to make any recommendations based on these data or for this group of people. The committee also noted the data on disease free survival for different T-stage had very wide confidence intervals and agreed not to make any recommendations based on this.
Benefits and harms
The evidence showed clinically meaningful reductions in locoregional recurrence and clinically meaningful increases in disease-free survival and overall survival with radiotherapy to the internal mammary nodes. The evidence also showed clinically meaningful increases in disease free survival for people with 0 and 1–3 positive lymph nodes. Whilst no clinically meaningful effect was found on this outcome for people with 4 or more positive nodes, the committee noted that the sample size was small and the magnitude of the effect was similar. They therefore agreed to recommend radiotherapy to the internal mammary chain for all node positive patients.
The committee noted that the evidence showed there was clinically meaningful increases in lung toxicity associated with radiotherapy to the internal mammary nodes. Therefore, based on their knowledge and experience, they recommended that a radiotherapy technique should be used that minimises the dose to the lung. Although the evidence review here did not demonstrate increased cardiac toxicity the committee were aware that radiotherapy to avoid cardiac toxicity was a separate question and that a heart-sparing technique should be used.
The committee noted that the potential benefits of giving radiotherapy to the internal mammary chain were likely to be reductions in locoregional recurrence and improvements in overall survival and disease-free survival. The potential harms would be increased treatment-related morbidity, but the committee noted that the evidence had not shown a clinically meaningful effect for anything except lung toxicity and grade 2+ lymphoedema. For lung toxicity a recommendation had been made to minimise the potential harm, but the risk of lymphoedema could not, unfortunately, be minimised.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee carefully considered the economic implications in this topic area as they were aware that including the internal mammary chain in the radiotherapy field may increase costs as it would increase planning time. It should be noted however that these potential cost increases cannot be captured when employing standard costing methodology for radiotherapy using NHS reference costs. This reflects the manner in which radiotherapy costs are estimated in NHS Reference costs whereby radiotherapy planning and delivery costs are stratified according to the type of radiotherapy delivered (and this category would not change when including the internal mammary chain). There is also no change in the overall dosage or number of fractions when including the internal mammary chain and so again there is no change in costs according to NHS Reference cost methodology.
While it is not possible to estimate the cost impact, the committee agreed that any increased cost would be minor as including the internal mammary chain does not impact delivery time or the number of sessions required. Further, any expenditure was considered to be worthwhile because of a decrease in locoregional recurrence and improved disease-free survival.
Other factors the committee took into account
The committee discussed the fact that including the internal mammary chain within the nodal radiotherapy target and using a radiotherapy technique that minimises the dose to the lung and heart is not currently standard practice and will require additional training, technique development and implementation. There will be an increase to both the planning, dosimetry and treatment times to deliver this, and this will need to be done on a centre basis to ensure tolerance doses can be achieved, with respect to each centres specific equipment, set-up and imaging protocols.
With regard to nodal voluming, current guidelines recommend that if nodal volumes are to be treated, then these sites should be volumed to assist in field placement. If looking purely at the time it takes to volume the IMC, then the estimated additional time is approximately an extra 30 minutes per patient. Delineating the supraclavicular fossa (SCF) target volume may add a further 20–30 minutes. A number of patients may also require axillary radiotherapy as a treatment alternative to surgical clearance and this will have further voluming time increases of about 30 minutes.
References
Choi 2016
Choi, J., Kim, Y. B., Shin, K. H., Ahn, S. J., Lee, H. S., Park, W., Kim, S. S., Kim, J. H., Lee, K. C., Kim, D. W., Suh, H. S., Park, K. R., Shin, H. S., Suh, C. O., (2016) Radiation Pneumonitis in Association with Internal Mammary Node Irradiation in Breast Cancer Patients: An Ancillary Result from the KROG 08-06 Study. Journal of Breast Cancer, 19, 275–282. [PMC free article: PMC5053312] [PubMed: 27721877]Hennequin 2013
Hennequin, C., Bossard, N., Servagi-Vernat, S., Maingon, P., Dubois, J. B., Datchary, J., Carrie, C., Roullet, B., Suchaud, J. P., Teissier, E., Lucardi, A., Gerard, J. P., Belot, A., Iwaz, J., Ecochard, R., Romestaing, P., (2013) Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy. [Erratum appears in Int J Radiat Oncol Biol Phys. 2014 Aug 1;89(5):1145]. International journal of radiation oncology, biology, physics, 86, 860–6. [PubMed: 23664327]Matzinger 2010
Matzinger, O., Heimsoth, I., Poortmans, P., Collette, L., Struikmans, H., Van den Bogaert, W., Fourquet, A., Bartelink, H., Ataman, F., Gulyban, A., Pierart, M., Van Tienhoven, G., EORTC Radiation Oncology & Breast Cancer Groups (2010) Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage I to III breast cancer (EORTC trial 22922/10925). Acta oncologica, 49, 24–34. [PubMed: 20100142]NICE 2009
National Institute for Health and Clinical Excellence. (2009). Early and locally advanced breast cancer: diagnosis and treatment. NICE guideline (CG80). [PubMed: 19167201]Poortmans 2015
Poortmans, P. M., Collette, S., Kirkove, C., Van Limbergen, E., Budach, V., Struikmans, H., Collette, L., Fourquet, A., Maingon, P., Valli, M., De Winter, K., Marnitz, S., Barillot, I., Scandolaro, L., Vonk, E., Rodenhuis, C., Marsiglia, H., Weidner, N., van Tienhoven, G., Glanzmann, C., Kuten, A., Arriagada, R., Bartelink, H., Van den Bogaert, W., EORTC Radiation Oncology & Breast Cancer Groups (2015) Internal Mammary and Medial Supraclavicular Irradiation in Breast Cancer. New England Journal of Medicine, 373, 317–27. [PubMed: 26200978]Thorsen 2016
Thorsen, L. B., Offersen, B. V., Dano, H., Berg, M., Jensen, I., Pedersen, A. N., Zimmermann, S. J., Brodersen, H. J., Overgaard, M., Overgaard, J., (2016) DBCG-IMN: A Population-Based Cohort Study on the Effect of Internal Mammary Node Irradiation in Early Node-Positive Breast Cancer. Journal of Clinical Oncology, 34, 314–20. [PubMed: 26598752]Whelan 2015
Whelan, T. J., Olivotto, I. A., Parulekar, W. R., Ackerman, I., Chua, B. H., Nabid, A., Vallis, K. A., White, J. R., Rousseau, P., Fortin, A., Pierce, L. J., Manchul, L., Chafe, S., Nolan, M. C., Craighead, P., Bowen, J., McCready, D. R., Pritchard, K. I., Gelmon, K., Murray, Y., Chapman, J. A., Chen, B. E., Levine, M. N., M. A. Study Investigators (2015) Regional Nodal Irradiation in Early-Stage Breast Cancer. New England Journal of Medicine, 373, 307–16. [PMC free article: PMC4556358] [PubMed: 26200977]
Appendices
Appendix A. Review protocols
Review protocol for 8.4. What are the indications for radiotherapy to internal mammary nodes? (PDF, 299K)
Appendix B. Literature search strategies
Literature search strategies for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Database: Medline & Embase (Multifile)
Last searched on Embase 1974 to 2017 July 10, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) 1946 to Present.
Date of last search: 11 July 2017
| # | Searches |
|---|---|
| 1 | exp breast cancer/ use oemezd |
| 2 | exp breast carcinoma/ use oemezd |
| 3 | exp medullary carcinoma/ use oemezd |
| 4 | exp intraductal carcinoma/ use oemezd |
| 5 | exp breast tumor/ use oemezd |
| 6 | exp Breast Neoplasms/ use prmz |
| 7 | exp “Neoplasms, Ductal, Lobular, and Medullary”/ use prmz |
| 8 | Carcinoma, Intraductal, Noninfiltrating/ use prmz |
| 9 | Carcinoma, Lobular/ use prmz |
| 10 | Carcinoma, Medullary/ use prmz |
| 11 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 |
| 12 | exp breast/ use oemezd |
| 13 | exp Breast/ use prmz |
| 14 | breast.tw. |
| 15 | 12 or 13 or 14 |
| 16 | (breast adj milk).tw. |
| 17 | (breast adj tender$).tw. |
| 18 | 16 or 17 |
| 19 | 15 not 18 |
| 20 | exp neoplasm/ use oemezd |
| 21 | exp Neoplasms/ use prmz |
| 22 | 20 or 21 |
| 23 | 19 and 22 |
| 24 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. use oemezd |
| 25 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. use oemezd |
| 26 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. use prmz |
| 27 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. use prmz |
| 28 | exp Paget nipple disease/ use oemezd |
| 29 | Paget’s Disease, Mammary/ use prmz |
| 30 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 31 | 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 |
| 32 | 11 or 31 |
| 33 | exp Radiotherapy/ use prmz |
| 34 | exp radiotherapy/ use oemezd |
| 35 | radiotherapy.fs. |
| 36 | (radiotherap$ or radiat$ or irradiat$ or brachytherap$ or tomotherap$).mp. |
| 37 | (fractionat$ or hyperfractionat$ or hypofractionat$).mp. |
| 38 | 33 or 34 or 35 or 36 or 37 |
| 39 | (deep adj3 (inspirat$ or inhal$) adj3 breath$).mp. |
| 40 | DIBH.mp. |
| 41 | (breath$ adj hold$).mp. |
| 42 | (deep adj (inspirat$ or inhal$)).mp. |
| 43 | ((inspirat$ or inhal$) adj breath$).mp. |
| 44 | ((respirat$ or inspirat$) adj3 (gated or gating)).mp. |
| 45 | ((respirat$ or inspirat$) adj3 (manoeuv$ or motion$ or synchron$)).mp. |
| 46 | ((free or active) adj3 breath$).mp. |
| 47 | Breath-Holding/ use prmz |
| 48 | breath-holding/ use oemezd |
| 49 | *Respiration/ use prmz |
| 50 | *breathing/ use oemezd |
| 51 | (prone adj4 (position$ or radiotherap$ or radiation$ or irradiation$ or planning or set-up or setup)).mp. |
| 52 | Prone Position/ use prmz |
| 53 | prone position/ use oemezd |
| 54 | shielding.mp. |
| 55 | Radiation Protection/ use prmz |
| 56 | radiation shield/ use oemezd |
| 57 | ((proton$ or photon$) adj3 (therap$ or treatment$ or radiotherap$ or radiation$ or irradiation$ or RT or beam$ or field$)).tw. |
| 58 | Proton Therapy/ use prmz |
| 59 | proton therapy/ use oemezd |
| 60 | 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 |
| 61 | 32 and 38 and 60 |
| 62 | Heart/ use prmz |
| 63 | heart/ use oemezd |
| 64 | ((heart$ or cardiac$ or cardio$) adj3 (morbidity or mortality or toxicity or event$ or effect$ or sequelae$)).mp. |
| 65 | 62 or 63 or 64 |
| 66 | 32 and 38 and 65 |
| 67 | Heart/re use prmz |
| 68 | ((heart$ or cardiac$) adj3 (sparing or protect$ or avoid$ or displac$ or dose)).mp. [mp=ti, ab, hw, tn, ot, dm, mf, dv, kw, fx, nm, kf, px, rx, ui, sy] |
| 69 | 67 or 68 |
| 70 | 32 and 38 and 69 |
| 71 | 61 or 66 or 70 |
| 72 | (left adj side$).ti. |
| 73 | 32 and 38 and 72 |
| 74 | 71 or 73 |
| 75 | limit 74 to yr=“1996 -Current” |
| 76 | remove duplicates from 75 [Then general exclusions filter applied] |
Database: Cochrane Library via Wiley Online
Date of last search: 11 July 2017
| # | Searches |
|---|---|
| #1 | MeSH descriptor: [Breast Neoplasms] explode all trees |
| #2 | MeSH descriptor: [Neoplasms, Ductal, Lobular, and Medullary] explode all trees |
| #3 | MeSH descriptor: [Carcinoma, Intraductal, Noninfiltrating] explode all trees |
| #4 | MeSH descriptor: [Carcinoma, Lobular] this term only |
| #5 | MeSH descriptor: [Carcinoma, Medullary] this term only |
| #6 | #1 or #2 or #3 or #4 or #5 |
| #7 | MeSH descriptor: [Breast] explode all trees |
| #8 | breast:ti,ab,kw (Word variations have been searched) |
| #9 | #7 or #8 |
| #10 | (breast next milk):ti,ab,kw (Word variations have been searched) |
| #11 | (breast next tender*):ti,ab,kw (Word variations have been searched) |
| #12 | #10 or #11 |
| #13 | #9 not #12 |
| #14 | MeSH descriptor: [Neoplasms] explode all trees |
| #15 | #13 and #14 |
| #16 | (breast* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #17 | (mammar* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #18 | MeSH descriptor: [Paget’s Disease, Mammary] this term only |
| #19 | (paget* and (breast* or mammary or nipple*)):ti,ab,kw (Word variations have been searched) |
| #20 | #15 or #16 or #17 or #18 or #19 |
| #21 | #6 or #20 |
| #22 | (deep near/3 (inspirat* or inhal*) near/3 breath*):ti,ab,kw (Word variations have been searched) |
| #23 | DIBH:ti,ab,kw (Word variations have been searched) |
| #24 | (breath* next hold*):ti,ab,kw (Word variations have been searched) |
| #25 | (deep next (inspirat* or inhal*)):ti,ab,kw (Word variations have been searched) |
| #26 | ((inspirat* or inhal*) next breath*):ti,ab,kw (Word variations have been searched) |
| #27 | ((respirat* or inspirat*) near/3 (gated or gating or manoeuv* or motion* or synchron*)):ti,ab,kw (Word variations have been searched) |
| #28 | ((free or active) near/3 breath*):ti,ab,kw (Word variations have been searched) |
| #29 | MeSH descriptor: [Breath-Holding] explode all trees |
| #30 | MeSH descriptor: [Respiration] this term only |
| #31 | (prone near/4 (position* or radiotherap* or radiation* or irradiation* or planning or set-up or setup)):ti,ab,kw (Word variations have been searched) |
| #32 | MeSH descriptor: [Prone Position] explode all trees |
| #33 | shielding:ti,ab,kw (Word variations have been searched) |
| #34 | MeSH descriptor: [Radiation Protection] explode all trees |
| #35 | ((proton* or photon*) near/3 (therap* or treatment* or radiotherap* or radiation* or irradiation* or RT or beam* or field*)):ti,ab,kw (Word variations have been searched) |
| #36 | MeSH descriptor: [Proton Therapy] explode all trees |
| #37 | #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 |
| #38 | #21 and #37 |
| #39 | MeSH descriptor: [Radiotherapy] explode all trees |
| #40 | (radiotherap* or radiat* or irradiat* or brachytherap* or tomotherap* or fractionat* or hyperfractionat* or hypofractionat*):ti,ab,kw (Word variations have been searched) |
| #41 | #39 or #40 |
| #42 | MeSH descriptor: [Heart] explode all trees |
| #43 | ((heart* or cardiac* or cardio*) near/3 (morbidity or mortality or toxicity or event* or effect* or sequelae*)):ti,ab,kw (Word variations have been searched) |
| #44 | #42 or #43 |
| #45 | #21 and #41 and #44 |
| #46 | MeSH descriptor: [Heart] explode all trees and with qualifier(s): [Radiation effects - RE] |
| #47 | ((heart* or cardiac*) near/3 (sparing or protect* or avoid* or displac* or dose)):ti,ab,kw (Word variations have been searched) |
| #48 | #46 or #47 |
| #49 | #21 and #48 |
| #50 | #38 or #45 or #49 |
| #51 | (left next side*):ti,ab,kw (Word variations have been searched) |
| #52 | #21 and #41 and #51 |
| #53 | #50 or #52 Publication Year from 1996 to 2017 |
Literature search strategies for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Database: Medline
Database: Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present.
Date of last search: 18 November 2016
| # | Searches |
|---|---|
| 1 | exp Breast Neoplasms/ |
| 2 | exp “Neoplasms, Ductal, Lobular, and Medullary”/ |
| 3 | Carcinoma, Intraductal, Noninfiltrating/ |
| 4 | Carcinoma, Lobular/ |
| 5 | Carcinoma, Medullary/ |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | exp Breast/ |
| 8 | breast.tw. |
| 9 | 7 or 8 |
| 10 | (breast adj milk).tw. |
| 11 | (breast adj tender$).tw. |
| 12 | 10 or 11 |
| 13 | 9 not 12 |
| 14 | exp Neoplasms/ |
| 15 | 13 and 14 |
| 16 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. |
| 17 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. |
| 18 | Paget’s Disease, Mammary/ |
| 19 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 20 | 15 or 16 or 17 or 18 or 19 |
| 21 | 6 or 20 |
| 22 | Mastectomy, Segmental/ |
| 23 | (segmentectom$ or post?segmentectom$).tw. |
| 24 | (lumpectom$ or post?lumpectom$).tw. |
| 25 | (quadrectom$ or post?quadrectom$).tw. |
| 26 | ((local or limited) adj2 (excision or resection)).tw. |
| 27 | ((partial or segment$) adj2 (mammectom$ or mastectomy$)).tw. |
| 28 | (breast adj conserv$).mp. |
| 29 | breast?conserv$.mp. |
| 30 | (conserv$ adj2 (surgery or therapy)).tw. |
| 31 | 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 |
| 32 | exp Radiotherapy/ |
| 33 | radiotherapy.fs. |
| 34 | (radiotherap$ or radiat$ or irradiat$ or brachytherap$ or tomotherap$).mp. |
| 35 | (fractionat$ or hyperfractionat$ or hypofractionat$).mp. |
| 36 | 32 or 33 or 34 or 35 |
| 37 | 21 and 31 and 36 |
| 38 | limit 37 to yr=“2008 -Current” |
| 39 | Limit 38 to RCTs and SRs, and general exclusions filter applied |
Database: Embase
Database: Embase Classic+Embase 1947 to 2016 Week 45.
Date of last search: 18 November 2016
| # | Searches |
|---|---|
| 1 | exp breast cancer/ |
| 2 | exp breast carcinoma/ |
| 3 | exp medullary carcinoma/ |
| 4 | exp intraductal carcinoma/ |
| 5 | exp breast tumor/ |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | exp breast/ |
| 8 | breast.tw. |
| 9 | 7 or 8 |
| 10 | (breast adj milk).tw. |
| 11 | (breast adj tender$).tw. |
| 12 | 10 or 11 |
| 13 | 9 not 12 |
| 14 | exp neoplasm/ |
| 15 | 13 and 14 |
| 16 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. |
| 17 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. |
| 18 | exp Paget nipple disease/ |
| 19 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 20 | 15 or 16 or 17 or 18 or 19 |
| 21 | 6 or 20 |
| 22 | partial mastectomy/ |
| 23 | segmental mastectomy/ |
| 24 | (segmentectom$ or post?segmentectom$).tw. |
| 25 | (lumpectom$ or post?lumpectom$).tw. |
| 26 | (quadrectom$ or post?quadrectom$).tw. |
| 27 | ((local or limited) adj2 (excision or resection)).tw. |
| 28 | ((partial or segment$) adj2 (mammectom$ or mastectomy$)).tw. |
| 29 | (breast adj conserv$).mp. |
| 30 | breast?conserv$.mp. |
| 31 | (conserv$ adj2 (surgery or therapy)).tw. |
| 32 | 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 |
| 33 | exp radiotherapy/ |
| 34 | radiotherapy.fs. |
| 35 | (radiotherap$ or radiat$ or irradiat$ or brachytherap$ or tomotherap$).mp. |
| 36 | (fractionat$ or hyperfractionat$ or hypofractionat$).mp. |
| 37 | 33 or 34 or 35 or 36 |
| 38 | 21 and 32 and 37 |
| 39 | limit 38 to yr=“2008 -Current” |
| 40 | Limit 38 to RCTs and SRs, and general exclusions filter applied |
Database: Cochrane Library via Wiley Online
Date of last search: 18 November 2016
| # | Searches |
|---|---|
| #1 | MeSH descriptor: [Breast Neoplasms] explode all trees |
| #2 | MeSH descriptor: [Neoplasms, Ductal, Lobular, and Medullary] explode all trees |
| #3 | MeSH descriptor: [Carcinoma, Intraductal, Noninfiltrating] explode all trees |
| #4 | MeSH descriptor: [Carcinoma, Lobular] this term only |
| #5 | MeSH descriptor: [Carcinoma, Medullary] this term only |
| #6 | #1 or #2 or #3 or #4 or #5 |
| #7 | MeSH descriptor: [Breast] explode all trees |
| #8 | breast:ti,ab,kw (Word variations have been searched) |
| #9 | #7 or #8 |
| #10 | (breast next milk):ti,ab,kw (Word variations have been searched) |
| #11 | (breast next tender*):ti,ab,kw (Word variations have been searched) |
| #12 | #10 or #11 |
| #13 | #9 not #12 |
| #14 | MeSH descriptor: [Neoplasms] explode all trees |
| #15 | #13 and #14 |
| #16 | (breast* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #17 | (mammar* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #18 | MeSH descriptor: [Paget’s Disease, Mammary] this term only |
| #19 | (paget* and (breast* or mammary or nipple*)):ti,ab,kw (Word variations have been searched) |
| #20 | #15 or #16 or #17 or #18 or #19 |
| #21 | #6 or #20 |
| #22 | MeSH descriptor: [Mastectomy, Segmental] this term only |
| #23 | (segmentectom* or post segmentectom* or post-segmentectom* or postsegmentectom*):ti,ab,kw (Word variations have been searched) |
| #24 | (lumpectom* or post lumpectom* or post-lumpectom* or postlumpectom*):ti,ab,kw (Word variations have been searched) |
| #25 | (quadrectom* or post quadrectom* or post-quadrectom* or postquadrectom*):ti,ab,kw (Word variations have been searched) |
| #26 | ((local or limited) near/2 (excision or resection)):ti,ab,kw (Word variations have been searched) |
| #27 | ((partial or segment*) near/2 (mammectom* or mastectomy*)):ti,ab,kw (Word variations have been searched) |
| #28 | (breast next conserv*):ti,ab,kw (Word variations have been searched) |
| #29 | (conserv* near/2 (surgery or therapy)):ti,ab,kw (Word variations have been searched) |
| #30 | #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 |
| #31 | MeSH descriptor: [Radiotherapy] explode all trees |
| #32 | (radiotherap* or radiat* or irradiat* or brachytherap* or tomotherap*):ti,ab,kw (Word variations have been searched) |
| #33 | (fractionat* or hyperfractionat* or hypofractionat*):ti,ab,kw (Word variations have been searched) |
| #34 | #31 or #32 or #33 |
| #35 | #21 and #30 and #34 Publication Year from 2008 to 2016 |
Literature search strategies for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Database: Medline & Embase (Multifile)
Database: Last searched on Embase 1974 to 2017 August 03, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) 1946 to Present
Date of last search: 4 August 2017
| # | Searches |
|---|---|
| 1 | exp breast cancer/ use oemezd |
| 2 | exp breast carcinoma/ use oemezd |
| 3 | exp medullary carcinoma/ use oemezd |
| 4 | exp intraductal carcinoma/ use oemezd |
| 5 | exp breast tumor/ use oemezd |
| 6 | exp Breast Neoplasms/ use prmz |
| 7 | exp “Neoplasms, Ductal, Lobular, and Medullary”/ use prmz |
| 8 | Carcinoma, Intraductal, Noninfiltrating/ use prmz |
| 9 | Carcinoma, Lobular/ use prmz |
| 10 | Carcinoma, Medullary/ use prmz |
| 11 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 |
| 12 | exp breast/ use oemezd |
| 13 | exp Breast/ use prmz |
| 14 | breast.tw. |
| 15 | 12 or 13 or 14 |
| 16 | (breast adj milk).tw. |
| 17 | (breast adj tender$).tw. |
| 18 | 16 or 17 |
| 19 | 15 not 18 |
| 20 | exp neoplasm/ use oemezd |
| 21 | exp Neoplasms/ use prmz |
| 22 | 20 or 21 |
| 23 | 19 and 22 |
| 24 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. use oemezd |
| 25 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. use oemezd |
| 26 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. use prmz |
| 27 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. use prmz |
| 28 | exp Paget nipple disease/ use oemezd |
| 29 | Paget’s Disease, Mammary/ use prmz |
| 30 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 31 | 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 |
| 32 | 11 or 31 |
| 33 | Brachytherapy/ use prmz |
| 34 | *brachytherapy/ use oemezd |
| 35 | Radiotherapy, Conformal/ use prmz |
| 36 | conformal radiotherapy/ use oemezd |
| 37 | Radiotherapy, Intensity-Modulated/ use prmz |
| 38 | *intensity modulated radiation therapy/ use oemezd |
| 39 | ((partial$ or whole$) adj breast$).tw. |
| 40 | ((accelerat$ or target$) adj3 (radiat$ or irradiat$ or radiotherap$ or radiosurg$ or brachytherap$)).tw. |
| 41 | (APBI$ or PBI$ or WBI$).tw. |
| 42 | ((intraoperativ$ or intra-operativ$) adj3 (radiat$ or irradiat$ or radiotherap$ or radiosurg$ or brachytherap$)).tw. |
| 43 | IORT$.tw. |
| 44 | mammosite.tw. |
| 45 | brachytherap$.tw. |
| 46 | (intensit$ adj modulat$).tw. |
| 47 | IMRT$.tw. |
| 48 | (“3D conformal” or “3-D conformal”).tw. |
| 49 | 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 |
| 50 | 32 and 49 |
| 51 | limit 50 to yr=“1996 -Current” |
| 52 | remove duplicates from 51 |
| 53 | Limit 52 to RCTs and SRs, and general exclusions filter applied |
Database: Cochrane Library via Wiley Online
Date of last search: 4 August 2017
| # | Searches |
|---|---|
| #1 | MeSH descriptor: [Breast Neoplasms] explode all trees |
| #2 | MeSH descriptor: [Neoplasms, Ductal, Lobular, and Medullary] explode all trees |
| #3 | MeSH descriptor: [Carcinoma, Intraductal, Noninfiltrating] explode all trees |
| #4 | MeSH descriptor: [Carcinoma, Lobular] this term only |
| #5 | MeSH descriptor: [Carcinoma, Medullary] this term only |
| #6 | #1 or #2 or #3 or #4 or #5 |
| #7 | MeSH descriptor: [Breast] explode all trees |
| #8 | breast:ti,ab,kw (Word variations have been searched) |
| #9 | #7 or #8 |
| #10 | (breast next milk):ti,ab,kw (Word variations have been searched) |
| #11 | (breast next tender*):ti,ab,kw (Word variations have been searched) |
| #12 | #10 or #11 |
| #13 | #9 not #12 |
| #14 | MeSH descriptor: [Neoplasms] explode all trees |
| #15 | #13 and #14 |
| #16 | (breast* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #17 | (mammar* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #18 | MeSH descriptor: [Paget’s Disease, Mammary] this term only |
| #19 | (paget* and (breast* or mammary or nipple*)):ti,ab,kw (Word variations have been searched) |
| #20 | #15 or #16 or #17 or #18 or #19 |
| #21 | #6 or #20 |
| #22 | MeSH descriptor: [Brachytherapy] explode all trees |
| #23 | MeSH descriptor: [Radiotherapy, Conformal] explode all trees |
| #24 | MeSH descriptor: [Radiotherapy, Intensity-Modulated] explode all trees |
| #25 | ((partial* or whole*) next breast*):ti,ab,kw (Word variations have been searched) |
| #26 | ((accelerat* or target*) near/3 (radiat* or irradiat* or radiotherap* or radiosurg* or brachytherap*)):ti,ab,kw (Word variations have been searched) |
| #27 | (APBI* or PBI* or WBI*):ti,ab,kw (Word variations have been searched) |
| #28 | ((intraoperativ* or intra-operativ*) near/3 (radiat* or irradiat* or radiotherap* or radiosurg* or brachytherap*)):ti,ab,kw (Word variations have been searched) |
| #29 | IORT*:ti,ab,kw (Word variations have been searched) |
| #30 | mammosite:ti,ab,kw (Word variations have been searched) |
| #31 | brachytherap*:ti,ab,kw (Word variations have been searched) |
| #32 | (intensit* next modulat*):ti,ab,kw (Word variations have been searched) |
| #33 | IMRT$*:ti,ab,kw (Word variations have been searched) |
| #34 | ((3D* or 3-D*) next conformal):ti,ab,kw (Word variations have been searched) |
| #35 | #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 |
| #36 | #21 and #35 |
Literature search strategies for 8.4. What are the indications for radiotherapy to internal mammary nodes?
Database: Medline
Last searched on Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present.
Date of last search: 5 January 2017
| # | Searches |
|---|---|
| 1 | exp Breast Neoplasms/ |
| 2 | exp “Neoplasms, Ductal, Lobular, and Medullary”/ |
| 3 | Carcinoma, Intraductal, Noninfiltrating/ |
| 4 | Carcinoma, Lobular/ |
| 5 | Carcinoma, Medullary/ |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | exp Breast/ |
| 8 | breast.tw. |
| 9 | 7 or 8 |
| 10 | (breast adj milk).tw. |
| 11 | (breast adj tender$).tw. |
| 12 | 10 or 11 |
| 13 | 9 not 12 |
| 14 | exp Neoplasms/ |
| 15 | 13 and 14 |
| 16 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. |
| 17 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).mp. |
| 18 | Paget’s Disease, Mammary/ |
| 19 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 20 | 15 or 16 or 17 or 18 or 19 |
| 21 | 6 or 20 |
| 22 | exp Radiotherapy/ |
| 23 | radiotherapy.fs. |
| 24 | (radiotherap$ or radiat$ or irradiat$ or brachytherap$ or tomotherap$).mp. |
| 25 | (fractionat$ or hyperfractionat$ or hypofractionat$).mp. |
| 26 | 22 or 23 or 24 or 25 |
| 27 | 21 and 26 |
| 28 | Axilla/ |
| 29 | Lymph Nodes/ |
| 30 | Lymphatic Metastasis/ |
| 31 | internal mammary.mp. |
| 32 | (supraclavicular or supraclavicule).mp. |
| 33 | 28 or 29 or 30 or 31 or 32 |
| 34 | 27 and 33 |
| 35 | ((regional or node or nodal or lymph$ or axill$ or supraclavicul$ or internal mammary or IMN) adj3 (radiotherap$ or radiat$ or irradiat$ or RT or brachytherap$ or tomotherap$ or fractionat$ or hyperfractionat$ or hypofractionat$)).tw. |
| 36 | Lymphatic Metastasis/rt [Radiotherapy] |
| 37 | 35 or 36 |
| 38 | 21 and 37 |
| 39 | 34 or 38 |
| 40 | limit 39 to yr=“2006 -Current” |
| 41 | Limit 40 to RCTs and SRs, and general exclusions filter applied |
Database: Embase
Last searched on Embase Classic+Embase 1947 to 2017 January 04.
Date of last search: 5 January 2017
| # | Searches |
|---|---|
| 1 | exp breast cancer/ |
| 2 | exp breast carcinoma/ |
| 3 | exp medullary carcinoma/ |
| 4 | exp intraductal carcinoma/ |
| 5 | exp breast tumor/ |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | exp breast/ |
| 8 | breast.tw. |
| 9 | 7 or 8 |
| 10 | (breast adj milk).tw. |
| 11 | (breast adj tender$).tw. |
| 12 | 10 or 11 |
| 13 | 9 not 12 |
| 14 | exp neoplasm/ |
| 15 | 13 and 14 |
| 16 | (breast$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. |
| 17 | (mammar$ adj5 (neoplasm$ or cancer$ or tumo?r$ or carcinoma$ or adenocarcinoma$ or sarcoma$ or leiomyosarcoma$ or dcis or duct$ or infiltrat$ or intraduct$ or lobul$ or medullary or tubular)).tw. |
| 18 | exp Paget nipple disease/ |
| 19 | (paget$ and (breast$ or mammary or nipple$)).tw. |
| 20 | 15 or 16 or 17 or 18 or 19 |
| 21 | 6 or 20 |
| 22 | exp radiotherapy/ |
| 23 | radiotherapy.fs. |
| 24 | (radiotherap$ or radiat$ or irradiat$ or brachytherap$ or tomotherap$).mp. |
| 25 | (fractionat$ or hyperfractionat$ or hypofractionat$).mp. |
| 26 | 22 or 23 or 24 or 25 |
| 27 | 21 and 26 |
| 28 | axilla/ |
| 29 | lymph node/ |
| 30 | lymph node metastasis/ |
| 31 | internal mammary.mp. |
| 32 | (supraclavicular or supraclavicule).mp. |
| 33 | 28 or 29 or 30 or 31 or 32 |
| 34 | 27 and 33 |
| 35 | ((regional or node or nodal or lymph$ or axill$ or supraclavicul$ or internal mammary or IMN) adj3 (radiotherap$ or radiat$ or irradiat$ or RT or brachytherap$ or tomotherap$ or fractionat$ or hyperfractionat$ or hypofractionat$)).tw. |
| 36 | lymph node metastasis/rt [Radiotherapy] |
| 37 | 35 or 36 |
| 38 | 21 and 37 |
| 39 | 34 or 38 |
| 40 | limit 39 to yr=“2006 -Current” |
| 41 | Limit 40 to RCTs and SRs, and general exclusions filter applied |
Database: Cochrane Library via Wiley Online
Date of last search: 5 January 2017
| # | Searches |
|---|---|
| #1 | MeSH descriptor: [Breast Neoplasms] explode all trees |
| #2 | MeSH descriptor: [Neoplasms, Ductal, Lobular, and Medullary] explode all trees |
| #3 | MeSH descriptor: [Carcinoma, Intraductal, Noninfiltrating] explode all trees |
| #4 | MeSH descriptor: [Carcinoma, Lobular] this term only |
| #5 | MeSH descriptor: [Carcinoma, Medullary] this term only |
| #6 | #1 or #2 or #3 or #4 or #5 |
| #7 | MeSH descriptor: [Breast] explode all trees |
| #8 | breast:ti,ab,kw (Word variations have been searched) |
| #9 | #7 or #8 |
| #10 | (breast next milk):ti,ab,kw (Word variations have been searched) |
| #11 | (breast next tender*):ti,ab,kw (Word variations have been searched) |
| #12 | #10 or #11 |
| #13 | #9 not #12 |
| #14 | MeSH descriptor: [Neoplasms] explode all trees |
| #15 | #13 and #14 |
| #16 | (breast* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #17 | (mammar* near/5 (neoplasm* or cancer* or tumo?r* or carcinoma* or adenocarcinoma* or sarcoma* or leiomyosarcoma* or dcis or duct* or infiltrat* or intraduct* or lobul* or medullary or tubular)):ti,ab,kw (Word variations have been searched) |
| #18 | MeSH descriptor: [Paget’s Disease, Mammary] this term only |
| #19 | (paget* and (breast* or mammary or nipple*)):ti,ab,kw (Word variations have been searched) |
| #20 | #15 or #16 or #17 or #18 or #19 |
| #21 | #6 or #20 |
| #22 | MeSH descriptor: [Radiotherapy] explode all trees |
| #23 | (radiotherap* or radiat* or irradiat* or brachytherap* or tomotherap*):ti,ab,kw (Word variations have been searched) |
| #24 | (fractionat* or hyperfractionat* or hypofractionat*):ti,ab,kw (Word variations have been searched) |
| #25 | #22 or #23 or #24 |
| #26 | #21 and #25 |
| #27 | MeSH descriptor: [Axilla] this term only |
| #28 | MeSH descriptor: [Lymph Nodes] this term only |
| #29 | MeSH descriptor: [Lymphatic Metastasis] this term only |
| #30 | internal mammary:ti,ab,kw (Word variations have been searched) |
| #31 | (supraclavicular or supraclavicule):ti,ab,kw (Word variations have been searched) |
| #32 | #27 or #28 or #29 or #30 or #31 |
| #33 | #26 and #32 |
| #34 | ((regional or node or nodal or lymph* or axill* or supraclavicul* or internal mammary or IMN) near/3 (radiotherap* or radiat* or irradiat* or RT or brachytherap* or tomotherap* or fractionat* or hyperfractionat* or hypofractionat*)):ti,ab,kw (Word variations have been searched) |
| #35 | MeSH descriptor: [Lymphatic Metastasis] explode all trees and with qualifier(s): [Radiotherapy - RT] |
| #36 | #34 or #35 |
| #37 | #21 and #36 |
| #38 | #33 or #37 Publication Year from 2006 to 2017 |
Appendix C. Clinical evidence study selection
Clinical evidence study selection for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Clinical evidence study selection for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Clinical evidence study selection for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Appendix D. Clinical evidence tables
Clinical evidence tables for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Table 14. Studies included in the evidence review for heart sparing radiotherapy (PDF, 349K)
Clinical evidence tables for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Table 15. studies included in the evidence review for breast radiotherapy after breast-conserving surgery (PDF, 458K)
Clinical evidence tables for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Table 16. Studies included in the evidence review for partial breast radiotherapy (PDF, 673K)
Clinical evidence tables for 8.4. What are the indications for radiotherapy to internal mammary nodes?
Table 17. Studies included in the evidence review for radiotherapy to the internal mammary nodes (PDF, 457K)
Appendix E. Forest plots
Forest plots for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Comparison 1. Deep inspiration breat-hold versus free breathing
Figure 5Mean heart dose
CI: Confidence Interval; DIBH: Deep inhalation breath-hold; FB: Free breathing; Gy: Gray
Forest plots for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Comparison 1. No whole breast radiotherapy versus whole breast radiotherapy
Figure 9Treatment-related morbidity: fractures (cause unspecified) at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 10Treatment-related morbidity: congestive cardiac failure at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 11Treatment-related morbidity: myocardial infarction at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 12Treatment-related morbidity: secondary cancer (cause unspecified) at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 13Treatment-related morbidity: score 10+ on HADS anxiety scale at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 14Treatment-related morbidity: score 10+ on HADS depression scale at 5 year follow-up (all patients N stage 0, 65+, negative margins)
Figure 16HRQoL: reduction in scores on Breast Cancer Chemotherapy Questionnaire at 2 month follow-up (all patients N stage 0, negative margins)
Forest plots for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Comparison 1. Whole breast radiotherapy versus partial breast radiotherapy
Forest plots for 8.4. What are the indications for radiotherapy to internal mammary nodes?
Comparison 1. Radiotherapy to the internal mammary nodes versus no radiotherapy to the internal mammary nodes
Figure 33Treatment related morbidity: secondary cancer (potentially radiation-induced) at 10 year follow-up
Figure 48Treatment related morbidity: Grade 2+ acute (within 3 months of the completion of treatment) pain (site not specified)
Figure 49Treatment related morbidity: acute (within 3 to 6 months of the completion of treatment) radiation pneumonitis
Appendix F. GRADE tables
GRADE tables for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Table 5. Clinical evidence profile: Comparison 1. Deep inspiration breath-hold versus free breathing (PDF, 260K)
Table 6. Clinical evidence profile: Comparison 2. Deep inspiration breath-hold versus prone radiotherapy (PDF, 237K)
GRADE tables for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
GRADE tables for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
GRADE tables for 8.4. What are the indications for radiotherapy to internal mammary nodes?
Appendix G. Economic evidence study selection
Economic evidence study selection for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
See Supplement 1: Health economics literature review for details of economic study selection.
Economic evidence study selection for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
See Supplement 1: Health economics literature review for details of economic study selection.
Economic evidence study selection for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
See Supplement 1: Health economics literature review for details of economic study selection.
Economic evidence study selection for 8.4. What are the indications for radiotherapy to internal mammary nodes?
See Supplement 1: Health economics literature review for details of economic study selection.
Appendix H. Economic evidence tables
Economic evidence tables for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
No economic evidence was identified for this review question.
Economic evidence tables for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
No economic evidence was identified for this review question.
Economic evidence tables for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Economic evidence tables for 8.4. What are the indications for radiotherapy to internal mammary nodes?
No economic evidence was identified for this review question.
Appendix I. Health economic evidence profiles
Health economic evidence profiles for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
No economic evidence was identified for this review question.
Health economic evidence profiles for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
No economic evidence was identified for this review question.
Health economic evidence profiles for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Table 22Summary table showing the included health economic evidence for the cost-effectiveness of partial breast radiotherapy after breast-conserving surgery
| Study | Population | Comparators | Costs | Effects | Incr costs | Incr effects | ICER | Uncertainty | Applicability and limitations |
|---|---|---|---|---|---|---|---|---|---|
| Shah et al. 2013 | Patients with invasive early stage breast cancer. | APBRT techniques compared against WBRT - 3D CRT | No deterministic or probabilistic sensitivity analyses were conducted. | The analysis was only partially applicable to the UK context since it considered the US health care system. Serious limitations were identified in the analysis. Most notably, uncertainty around the base case estimates was not assessed as no deterministic or probabilistic sensitivity analyses were conducted. | |||||
| WBRT - 3D CRT | $11,726 | 10.84 | Reference | ||||||
| APBRT - 3D CRT | $6,578 | 10.91 | -$5,148 | 0.07 | Dominant | ||||
| APBRT - IMRT | $10,547 | 10.91 | -$1,179 | 0.07 | Dominant | ||||
| APBRT - SL | $12,602 | 10.91 | $876 | 0.07 | $12,514 per QALY | ||||
| APBRT - ML | $16,439 | 10.91 | $4,713 | 0.07 | $67,329 per QALY | ||||
| APBRT - Interstitial | $11,765 | 10.91 | $39 | 0.07 | $557 per QALY | ||||
| APBI techniques compared against WBRT - IMRT | |||||||||
| WBRT - IMRT | $20,637 | 10.84 | Reference | ||||||
| APBRT - 3D CRT | $6,578 | 10.91 | -$14,059 | 0.07 | Dominant | ||||
| APBRT - IMRT | $10,547 | 10.91 | -$10,090 | 0.07 | Dominant | ||||
| APBRT - SL | $12,602 | 10.91 | -$8,035 | 0.07 | Dominant | ||||
| APBRT - ML | $16,439 | 10.91 | -$4,198 | 0.07 | Dominant | ||||
| APBRT - Interstitial | $11,765 | 10.91 | -$8,872 | 0.07 | Dominant | ||||
|
Comments: Incremental costs and QALYs were not reported in the study. Incremental values above have therefore been estimated as the difference between the absolute values reported in the study. Note also that the study presents costs under numerous scenarios. The costs presented above are for reimbursement costs only as it was thought to best reflect the third party perspective (other scenarios reported in the analysis included ‘non-medical’ costs which possibly include costs more applicable to the societal perspective). | |||||||||
Health economic evidence profiles for 8.4. What are the indications for radiotherapy to internal mammary nodes?
No economic evidence was identified for this review question.
Appendix J. Health economic analysis
Health economic analysis for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
No health economic analysis was conducted for this review question.
Health economic analysis for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
No health economic analysis was conducted for this review question.
Health economic analysis for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
No health economic analysis was conducted for this review question.
Health economic analysis for 8.4. What are the indications for radiotherapy to internal mammary nodes?
No health economic analysis was conducted for this review question
Appendix K. Excluded studies
Excluded studies for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
Clinical studies
Download PDF (257K)
Economic studies
See Supplement 1: Health economics literature review for list of excluded economic studies.
Excluded studies for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
Clinical studies
Download PDF (242K)
Economic studies
See Supplement 1: Health economics literature review for list of excluded economic studies.
Excluded studies for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
Clinical studies
Download PDF (443K)
Economic studies
See Supplement 1: Health economics literature review for list of excluded economic studies.
Excluded studies for 8.4. What are the indications for radiotherapy to internal mammary nodes?
Clinical studies
Download PDF (282K)
Economic studies
See Supplement 1: Health economics literature review for list of excluded economic studies.
Appendix L. Research recommendations
Research recommendations for 8.1. What radiotherapy techniques are effective for excluding the heart from the radiation field without compromising coverage of the whole breast target volume for people with early or locally advanced breast cancer?
No research recommendations were made for this review question.
Research recommendations for 8.2. Is there a subgroup of people with early invasive breast cancer who do not need breast radiotherapy after breast-conserving surgery?
No research recommendations were made for this review question.
Research recommendations for 8.3. Is there a subgroup of women with early invasive breast cancer for whom partial breast radiotherapy is an equally effective alternative to whole breast radiotherapy after breast-conserving surgery?
No research recommendations were made for this review question.
Research recommendations for 8.4. What are the indications for radiotherapy to internal mammary nodes?
No research recommendations were made for this review question.
Tables
Table 1Summary of the protocol (PICO table)
| Population | Adults (18 or over) with invasive breast cancer (M0) and/or DCIS receiving whole breast radiotherapy |
|---|---|
| Intervention | Heart sparing techniques:
|
| Comparison |
|
| Outcome | Critical
|
DCIS: Ductal carcinoma in-situ; M0 no distant metastases
Table 2Summary of included studies
| Study | Additional inclusion/exclusion criteria | Intervention/Comparison |
|---|---|---|
| Bartlett 2017 | Left sided breast cancer |
Intervention arm: Deep inspiration breath-hold Control arm: Free breathing |
| Bartlett 2015 | Left sided breast cancer |
Intervention arm: Deep inspiration breath hold Control arm: Prone radiotherapy |
| Chi 2015 | Left sided breast cancer |
Intervention arm: Moderate deep inspiration breath-hold Control arm: Free breathing |
| Czeremszynska 2017 |
Age <70 years Left sided breast cancer |
Intervention arm: Deep inspiration breath-hold Control arm: Free breathing |
| Eldredge-Hindy 2015 | Left sided breast cancer |
Intervention arm: Moderate deep inspiration breath-hold with ABC device Control arm: Free breathing |
ABC: Active breathing coordinator
Table 3Summary clinical evidence profile: Comparison 1. Deep inspiration breathhold versus free breathing
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | ||||
| Free Breathing | Deep Inspiration Breath-Hold | ||||
| Mean Heart Dose at RT (Gy) |
The mean heart dose at RT in the control groups was 2.4 Gy |
The mean mean heart dose at RT in the intervention groups was 1.29 lower (1.81 to 0.77 lower) | - |
236 | Very low5,6,7 |
|
Target Coverage at RT Scale from: 0 to 100. |
The mean target coverage at RT in the control groups was 86.3 % |
The mean target coverage at RT in the intervention groups was 0.5 higher (4.6 lower to 5.6 higher) | - |
81 (1 study1) | Very low7 |
CI: confidence interval; Gy: gray: RT: radiotherapy
- 1
- 2
- 3
- 4
- 5
Downgraded by 2 levels for very serious inconsistency as I square=89%
- 6
Downgraded by 1 level for indirectness due to inclusion of women with only larger breast volumes (estimated volume>750cm3)
- 7
Downgraded by 1 level for serious imprecision, as number of events <400
Table 4Summary clinical evidence profile: Comparison 2. Deep inspiration breathhold versus prone radiotherapy
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | ||||
| Prone RT | Deep Inspiration Breath-Hold | ||||
| Mean Heart Dose at RT (Gy) |
The mean heart NTD dose at RT in the control groups was 0.66 Gy |
The mean heart dose at RT in the intervention groups was 0.22 lower (0.30 to 0.14 lower) | - |
28 (1 study1) | Low2,3 |
CI: Confidence interval; Gy: Gray; NTD: normalized total dose; RT: Radiotherapy;
- 1
- 2
Downgraded by 1 level for serious indirectness as only women with larger breasts included
- 3
Downgraded by 1 level for serious imprecision, as number of events <400
Table 5Summary of the protocol (PICO table)
| Population | Women (18 or over) with invasive breast cancer (M0) who have undergone breast conserving surgery |
|---|---|
| Intervention |
|
| Comparison | Whole breast radiotherapy |
| Outcome | Critical
|
HRQoL, Health related quality of life; M0, no distant metastases
Table 6Summary of included studies
| Study | Trial | Additional inclusion/exclusion criteria | Interventions/comparison |
|---|---|---|---|
| Blamey 2013 | BASO II |
Aged <70 with primary operable unilateral invasive breast cancer (N0, M0) Histological grade 1 or specific good prognosis tumours Maximum tumour size 20mm No previous cancer except adequately treated basal cell carcinoma of the skin Excluded if pregnant or lactating Excluded if other diseases precluded adequate surgery, adjuvant therapy, or follow-up |
|
| Holli 2009 |
Age >40 years Tumour 20mm or less, grade 1 or 2. PR status positive. Low cell proliferation rate Excluded if extensive intraductal component or axillary node metastases |
Intervention arm (RT-): segmental breast resection (1 cm margins) and levels I and II dissection of ipsilateral axilla. Control arm (RT+): segmental breast resection (1 cm margins) and levels I and II dissection of ipsilateral axilla. Whole breast radiotherapy total 50 Gy within 5 weeks using 2 Gy daily fractions. | |
| Hughes 2013 | CALGB 9343 |
≥70 years with stage I, N0, ER+ breast cancer No history of cancer other than in situ cervical or non-melanoma skin cancer within 5 years Initially included tumours up to 4cm but reduced to 2cm |
Intervention arm (RT-): lumpectomy with a clear margin (no ink on tumour). 20 mg tamoxifen per day for 5 years initiated during or after irradiation. Control arm (RT+): lumpectomy with a clear margin (no ink on tumour). 20 mg tamoxifen per day for 5 years initiated during or after irradiation. RT included tangential fields to the entire breast followed by an electron boost to the lumpectomy site. |
| Kunkler 2015 | PRIME II |
≥65 years with T1-T2, N0 hormone receptor positive breast cancer Receiving neoadjuvant hormonal treatment Excluded if history of in-situ or invasive breast cancer of either breast or previous malignant disease in the past year, other than non-melanomatous skin cancer or carcinoma in situ of the cervix |
Intervention arm (RT-): No details for breast conserving surgery procedures provided (except ≥1mm margins). Tamoxifen (20 mg daily for 5 years) as the standard adjuvant endocrine treatment but other forms allowed. Control arm (RT+): No details for breast conserving surgery procedures provided (except ≥1mm margins). Tamoxifen (20 mg daily for 5 years) as the standard adjuvant endocrine treatment but other forms allowed. RT total dose 40–50Gy in 15–25 fractions over 3–5 weeks. Boost permitted but not required. |
| Wickberg 2014 | Uppsala/Orebro |
≤80 years with unifocal stage 1 invasive breast cancer |
Intervention arm (RT-): sector resection and axilla dissected to levels I and II Control arm (RT-): sector resection and axilla dissected to levels I and II. Radiotherapy total dose of 54Gy in 27 fractions |
| Williams 2011 | PRIME |
≥ 65 years with T0–2, N0 unilateral breast cancer Receiving adjuvant endocrine therapy. Medically suitable to attend for all treatments and follow-up. Excluded if pure in situ carcinoma or previous/concurrent malignancy within 5 years other than non-melanomatous skin cancer or carcinoma in situ of cervix Excluded if grade 3 cancer | BCS complete excision – further details not reported |
BASO, British Association of Surgical Oncologists; BCS, Breast conservation surgery; CALGB, Cancer and Leukemia Group B; ER, oestrogen receptor; Gy, gray; PRIME, Postoperative Radiotherapy in Minimum-Risk Elderly; RT, radiotherapy; WLE, wide local excision
Table 7Summary clinical evidence profile: Comparison 1. No whole breast radiotherapy versus whole breast radiotherapy
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
|---|---|---|---|---|---|
| Assumed risk: RT+ | Corresponding risk: RT− | ||||
| Overall survival - T stage: 1 (12 year follow-up) | 12 yr OS 85% | 12 yr OS 77% (73% to 81%) |
HR 1.59 (1.29 to 1.96) |
263 (1 study) | Moderate1 |
| Overall survival - N stage: 0 (5 to 12 year follow-up) | 5 yr OS 88% | 5 yr OS 85% (83% to 87%) |
HR 1.29 (1.12 to 1.5) |
1154 (3 studies) | Moderate2 |
| Overall survival - Margins: negative (5 to 12 year follow-up) | 5 yr OS 88% | 5 yr OS 85% (83% to 87%) |
HR 1.29 (1.12 to 1.5) |
1154 (3 studies) | Moderate2 |
| Overall survival - Age: 65+ (5 to 10 year follow-up) | 5 yr OS 88% | 5 yr OS 87% (85% to 90%) |
HR 1.06 (0.87 to 1.3) |
891 (2 studies) | High |
|
Overall survival - Adjuvant systemic therapy: none (20 year follow-up) | 20 yr OS 50% | 20 yr OS 47% (37% to 56%) |
HR 1.1 (0.85 to 1.42) |
381 (1 study) | Moderate3 |
| Local recurrence - T stage: 1 (10 to 12 year follow-up) | 90% free from local recurrence at 10 yrs | 75% free from local recurrence at 10 yrs (66% to 82%) |
HR 2.7 (1.84 to 3.97) |
1378 (2 studies) | Moderate3 |
| Local recurrence - N stage: 0 (5 to 12 year follow-up) | 96% free from local recurrence at 5 yrs | 88% free from local recurrence at 5 yrs (83% to 91%) |
HR 3.22 (2.31 to 4.49) |
3340 (4 studies) | Moderate3 |
| Local recurrence - Margins: negative (5 to 12 year follow-up) | 96% free from local recurrence at 5 yrs | 88% free from local recurrence at 5 yrs (83% to 91%) |
HR 3.22 (2.31 to 4.49) |
3340 (4 studies) | Moderate3 |
| Local recurrence - Age: 65+ (5 to 10 year follow-up) | 99% free from local recurrence at 5 yrs | 95% free from local recurrence at 5 yrs (90% to 97%) |
HR 5.35 (2.78 to 10.29) |
1962 (2 studies) | Low1 |
| Treatment-related morbidity – fractures (cause unspecified; all patients N stage 0, 65+, negative margins; 5 year follow-up) | 106 per 1000 | 116 per 1000 (50 to 272) |
RR 1.10 (0.47 to 2.57) | 171 (1 study) | Low4 |
| Treatment-related morbidity - congestive cardiac failure (all patients N stage 0, 65+, negative margins; 5 year follow-up) | 35 per 1000 |
35 per 1000 (7 to 168) |
RR 0.99 (0.21 to 4.76) |
171 (1 study) | Low6 |
| Treatment-related morbidity - myocardial infarction (all patients N stage 0, 65+, negative margins; 5 year follow-up) | 71 per 1000 |
58 per 1000 (18 to 184) |
RR 0.82 (0.26 to 2.6) |
171 (1 study) | Low4 |
| Treatment-related morbidity - secondary cancer (cause unspecified; all patients N stage 0, 65+, negative margins; 5 year follow-up) | 35 per 1000 | 89 per 1000 (8 to 928) |
RR 2.53 (0.24 to 26.51) |
1497 (2 studies) | Low1 |
| Treatment-related morbidity - score 10+ on HADS depression scale (all patients N stage 0, 65+, negative margins; 5 year follow-up) | 10 per 1000 |
30 per 1000 (3 to 281) |
RR 3.12 (0.33 to 29.49) |
206 (1 study) | Low4 |
| Treatment-related morbidity - score 10+ on HADS anxiety scale (all patients N stage 0, 65+, negative margins; 5 year follow-up) | 86 per 1000 |
119 per 1000 (52 to 270) |
RR 1.39 (0.61 to 3.15) |
206 (1 study) | Low4 |
| HRQoL - EQ5D scale (all patients N stage 0, 65+, negative margins; 5 year follow-up) |
The mean HRQoL – EQ5D scale (all patients N stage 0, 65+, negative margins) in the intervention groups was 0.02 lower (0.1 lower to 0.06 higher) |
168 (1 study) | Low5 | ||
| HRQoL - reduction in scores on Breast Cancer Chemotherapy Questionnaire (all patients N stage 0, negative margins; 2 month follow-up) | 270 per 1000 |
160 per 1000 (119 to 214) |
RR 0.59 (0.44 to 0.79) | 720 (1 study) | Not possible to GRADE this outcome due to study included from previous guideline |
Rates of overall survival and local recurrence in the control group correspond to the weighted average across included trials or the trial with the shortest follow-up period where these differ across included trials
CI: Confidence interval; EQ5D, EuroQol Research Foundation measure of general health status; HADS: Hospital Anxiety and Depression Scale; HR: Hazard ratio; HRQoL: Health related quality of life; OS: overall survival; RR: Risk ratio;
- 1
<300 events
- 2
Random effects model with significant heterogeneity - I squared value 74% - not possible to investigate heterogeneity as additional subgroups of interest identified by the GC were not reported for the trials that contributed to this estimate. All estimated effects were in the same direction
- 3
Total events <300
- 4
<300 events and 95% CI crosses both thresholds for minimally important difference based on GRADE default values (0.80 and 1.25)
- 5
N<400
- 6
total events<300; not downgraded based on 95% CI due to very small differences in absolute risk
Table 8Summary of the protocol (PICO table)
| Population | Women (18 or over) with invasive breast cancer (M0) who have undergone breast conserving surgery |
|---|---|
| Intervention | Partial breast radiotherapy |
| Comparison | Whole breast radiotherapy |
| Outcome | Critical
|
HRQoL, health-related quality of lfie; M0, no distant metasases
Table 9Summary of included studies
| Study | Trial | Additional inclusion/exclusion criteria | Interventions/comparison |
|---|---|---|---|
| Ott 2016, Polgar 2017, Strnad 2016 | GEC-ESTRO |
Inclusion criteria: Women aged ≥ 40 years; histologically confirmed invasive breast cancer or ductal carcinoma in situ (DCIS) UICC stage 0–IIA, a maximum tumour diameter < 3 cm, complete resection with clear margins ≥2 mm (in case of invasive lobular cancer or pure DCISP5 mm), at least six negative axillary lymph nodes (pN0), or singular nodal micro-metastasis (pN1mi), or negative sentinel node biopsy (pN0sn), or a clinically negative axilla in case of DCIS (cN0), no distant metastasis or contralateral breast cancer. Exclusion criteria: Any signs of a multifocal growth pattern in mammography, had residual micro-calcifications post-operatively, an extensive intraductal component (EIC), vessel invasion (L1, V1), involved, close (<2 mm) or unknown margins (R1/Rx), or were pregnant. |
1) APBI Interstitial brachytherapy; HDR 32 Gy/8 fractions or 30.3 Gy/7 fractions; PDR 50 Gy at 0.6–0.8 Gy/fractions given hourly. 2) External beam WBRT 50.0–50.4 Gy/1.8–2.0 Gy fractions (5–28) plus 10 Gy/5 fraction boost. |
| Coles 2017 | IMPORT LOW |
Inclusion criteria: Women ≥ 50 years undergoing breast conserving surgery for unifocal invasive ductal adenocarcinoma of any grade (1–3); pathological tumour size ≤ 3 cm (pT1–2), axillary node negative or one to three positive nodes (pN0–1), microscopic margins of non-cancerous tissue ≥ 2 mm. Exclusion criteria: Women < 50 years; Invasive carcinoma of classical lobular type; distant metastases; previous malignancy of any kind (unless non-melanomatous skin cancer); undergone a mastectomy; received neoadjuvant chemotherapy or concurrent adjuvant chemoradiotherapy. |
|
| Livi 2010, Livi 2015, Meattini 2017 | Livi 2015 |
Inclusion criteria: Age at presentation >40 years; Tumour size ≤25 mm; Wide excision or quadrantectomy with clear margins (≤5 mm); Clips placed in tumour bed; Full informed consent from patient; Follow-up at the radiotherapy department of Florence University. Exclusion criteria: Women ≤ 40 years; Cardiac dysfunction (Left ventricular ejection fraction <50% as measured by echocardiography or history of active angina, myocardial infarction, or other cardiovascular disease); Forced expiratory volume <1 L/m; Extensive intraductal carcinoma; Multifocal cancer; Psychiatric problems; Follow-up at centre other than the radiotherapy department of Florence University. |
1) Partial breast irradiation or accelerated partial breast irradiation using intensity-modulated radiotherapy (IMRT). 2) Whole breast radiotherapy (WBRT); used 50 Gy/25 fractions plus 10 Gy boost. |
| Lovey 2007, Polgar 2007, Polgar 2013 | Polgar 2007 |
Inclusion criteria: Women > 40 years; Wide excision with microscopically negative surgical margins; unifocal tumour; primary tumour size ≤20 mm (pT1); cN0, pN0, or pN1mi (single nodal micrometastasis >0.2mmand≤2.0 mm) axillary status; and histologic Grade 2 or less. Exclusion criteria: Women ≤ 40 years; bilateral breast carcinoma; prior uni- or contralateral breast cancer; concomitant or previous other malignancies (except basal cell carcinoma of the skin); pure ductal or lobular carcinoma in situ (pTis); invasive lobular carcinoma; or the presence of an extensive intraductal component. |
1) PBI; 7 × 5.2GyHDRmulti-catheter brachytherapy (88/128 women). Those unsuitable for HDR (40/1280 women) had 50 Gy/25 fractions electron beam RT to partial breast. 2) Control arm: 50 Gy/25 fractions WBRT (130 women) |
| Olivotto 2013 | RAPID |
Inclusion criteria: Women ≥ 40 years with invasive ductal carcinoma or ductal carcinoma in situ (DCIS) treated with BCS with microscopically clear margins and negative axillary nodes by sentinel node biopsy, or axillary dissection for those with invasive disease, or by clinical examination for those with DCIS alone. Exclusion criteria: Women < 40 years; combined tumour size (DCIS and/or invasive carcinoma)>3 cm, lobular carcinoma, > one primary tumour in different quadrants of the breast, or an RT plan that did not meet protocol-defined dose-volume constraints for APBI. |
1) APBI using three-dimensional conformal radiotherapy (3D-CRT): 38.5 Gy in 10 fractions, bd over 5–8 days. 6–8 hour gap between doses. 2) WBRT; 42.5 Gy in 16 fractions daily over 22 days. Women with large breast size: 50 Gy in 25 fractions over 25 days. Boost 10 Gy in 4 or 5 fractions over 4–7 days was permitted women who were deemed at moderate to high risk of LR according to local cancer centre guidelines. |
| Rodriguez 2013 | Rodriguez 2013 |
Inclusion criteria: Women age ≥60 years; invasive ductal carcinoma; unifocal tumour; primary tumour size ≤30 mm (pT2); cN0, pN0 axillary status; and histologic grade 2 or less. Exclusion criteria: Women age <60 years; Bilateral breast carcinoma; prior unilateral or contralateral breast cancer; concomitant or other previous malignancies; pure ductal or lobular carcinoma in situ (pTis); invasive lobular carcinoma; presence of an extensive intraductal component; excision with microscopically positive or close (3 mm) surgical margins; multicentric disease; nodepositive disease; concomitant or neoadjuvant chemotherapy; and postsurgical hematoma >2 cm, or seroma fluid that required multiple aspirations. |
1) PBI/APBI delivered by 3D-CRT at 48Gy/24 fractions ± 10 Gy boost (according to risk factors for local recurrence) in 51 women. 2) Conventional WBRT at 48 Gy/24 fractions ± 10 Gy boost in 51 women. |
3D-CRT: 3 dimensional conformal radiotherapy; APBI: Accelerated partial breast irradiation; BCS: breast conserving surgery; DCIS: ductal carcinoma in situ; EIC: extensive intraductal component; GEC-ESTRO: The Groupe Européen de Curiethérapie and the European SocieTy for Radiotherapy & Oncology; Gy: Gray; HDR: High dose rate; IMPORT: Intensity Modulated and Partial Organ Radiotherapy; IMRT: intensity modulated radiotherapy; PBI: Partial breast irradiation; PDR: Pulsed dose rate; RAPID: Randomized Trial of Accelerated Partial Breast Irradiation; UICC: Union for International Cancer Control; WBRT: Whole breast radiotherapy
Table 10Summary clinical evidence profile: Comparison 1. Partial-breast radiotherapy versus whole-breast radiotherapy after breast-conserving surgery
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk: WBRT | Corresponding risk: PBI/APBI | |||||
|
Local recurrence free survival: local recurrence in the ipsilateral breast as a discrete outcome Follow-up: 5 to 10 years1 | 14 per 1000 |
14 per 1000 (9 to 21) |
HR 0.98 (0.63 to 1.52) |
3407 (5 studies) | Low1,2 | |
|
Cosmesis, physician reported Assessed with four-point scales Follow-up: 3 to 5 years | 153 per 1000 |
151 per 1000 (87 to 263) |
RR 0.99 (0.57 to 1.72) |
3764 (6 studies) | Very low3,4,6 | Four-point scales were used to assess cosmesis as poor/worse, fair/normal, good, or excellent. These results represent those with poor/worse or fair/normal cosmesis. |
|
Cosmesis, patient reported at 5 years follow-up Assessed with four-point scales Follow-up: mean 5 years | 146 per 1000 |
147 per 1000 (98 to 220) |
RR 1.01 (0.67 to 1.51) |
1966 (4 studies) | Very low3,5,6 | Four-point scales were used to assess cosmesis as poor, fair, good, or excellent. These results represent those with poor or fair cosmesis. |
|
Cosmesis, nurse reported at 5 year follow-up Assessed with four-point scale Follow-up: mean 5 years | 134 per 1000 |
327 per 1000 (211 to 511) |
RR 2.44 (1.57 to 3.81) |
335 (1 study) | Low2,3 | Cosmesis characteristics were graded on a four-point scale: poor, fair, good, excellent. Results are for those with poor or fair cosmesis. |
|
Acute radiotherapy (RT) skin toxicity Assessed with the Radiation Therapy Oncology Group Common Toxicity Criteria Follow-up: 0 to 90 days | 752 per 1000 |
120 per 1000 (60 to 248) |
RR 0.16 (0.08 to 0.33) |
1790 (3 studies) | Low4 | Treatment tolerance was assessed using the acute radiation morbidity scoring criteria. |
|
Late RT skin toxicity Assessed with the Radiation Therapy Oncology Group Common (RTOG CTC) 5-point scale10 Follow-up: 3 to 5 years | 63 per 1000 |
61 per 1000 (19 to 190) |
RR 0.97 (0.31 to 3.03) |
3175 (5 studies) | Very low4,6 | |
|
Breast Pain Self-reported Follow-up: 3 to 5 years | 67 per 1000 |
61 per 1000 (45 to 81) |
RR 0.9 (0.67 to 1.2) |
2475 (3 studies) | Very low2,7,8 | Self-reported using the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-BR23 breast cancer module, and NCI CTC criteria. |
|
Fat necrosis Assessed with EORTC and NCI 5-point scale Follow-up: 3 to 5 years | 65 per 1000 |
89 per 1000 (64 to 122) |
OR 1.4 (0.98 to 2) |
1899 (3 studies) | Low2,8 | Defined as grade 1 to 3 on EORTC and NCI CTC. |
|
Health related quality of life Assessed using EORTC QLQ-C30 and BR23 module Follow-up: mean 2 years | - |
The mean health related quality of life in the intervention groups was 16 higher (10.99 to 21.01 higher) | - |
205 (1 study) | Low2,9 | |
|
Overall survival Follow-up: mean 5 years | 53 per 1000 |
41 per 1000 (30 to 56) |
HR 0.76 (0.55 to 1.06) |
3047 (3 studies) | Moderate2 | |
|
Disease-free survival Follow-up: mean 5 years | 31 per 1000 |
29 per 1000 (20 to 42) |
HR 0.93 (0.63 to 1.37) |
3305 (4 studies) | Moderate2 | |
|
Distant metastasis-free survival Follow-up: mean 5 years | 22 per 1000 |
20 per 1000 (13 to 32) |
HR 0.9 (0.56 to 1.46) |
3305 (4 studies) | Moderate2 | |
| Treatment-related mortality | No treatment related deaths | No treatment related deaths | Not estimable |
1184 (1 study) | Moderate2 | |
APBI: accelerated partial breast irradiation; CI: Confidence interval; CTC, Common Toxicity Criteria; EORTC QLQ-30: European Organisation for Research and Treatment of Cancer Quality of Life Questionairre; HR: Hazard ratio; NCI, National Cancer Institute; PBI: partial breast irradiation; RR: Risk ratio; RT: radiotherapy; RTOG: Radiation Therapy Oncology Group; WBRT: whole breast radiotherapy
- 1
Clinical heterogeneity was substantial relating to radiotherapy dose, technique and use of quality assurance procedures.
- 2
< 300 events.
- 3
Five of 6 studies were at high risk of bias for blinding of outcome assessors for subjective outcomes.
- 4
Very serious heterogeneity (I2>80%); random effects model used, no subgroup analysis accounted for heterogeneity.
- 5
Serious heterogeneity (I2>50% but <80%); random effects model used, no subgroup analysis accounted for heterogeneity.
- 6
Effect estimate includes both default MID thresholds and the null effect (1).
- 7
Blinding of participants to treatment group not possible for self-reported breast pain.
- 8
Effect estimate includes one default MID threshold and the null effect (1).
- 9
Blinding of outcome assessors was not reported.
Table 11Summary of the protocol (PICO table)
| Population | Adults (18 or over) with invasive breast cancer but no distant metastases (M0) treated with breast conserving surgery or mastectomy (including modified radical mastectomy). |
|---|---|
| Intervention | Radiotherapy to internal mammary nodes (± other nodes) |
| Comparison | No internal mammary node radiotherapy (± other nodes) |
| Outcome | Critical
|
HRQoL, health-related quality of lfie; M0, no distant metasases
Table 12Summary of included studies
| Study | Trial | Additional inclusion/exclusion criteria | Interventions/comparison |
|---|---|---|---|
| Choi 2016 | KROG 08–06 |
|
|
| Hennequin 2013 | No trial name |
|
|
| Matzinger 2010 | EORTC 22922/10925 |
|
|
| Poortmans 2015 | EORTC 22922/10925 |
|
|
| Thorsen 2016 | DBCG-IMN |
|
|
| Whelan 2015 | MA.20 |
|
|
DBCG, Danish Breast Cancer Group; EORTC, European Organisation for Research and Treatment of Cancer; Gy, gray; IM, internal mammary; IMN, internal mammary nodes; KROG, Korean Radiation Oncology Group MeV, megaelectronvolt; MS, medial supraclavicular; RT, radiotherapy
Table 13Summary clinical evidence profile: Comparison 1. Radiotherapy to the internal mammary nodes versus no radiotherapy to the internal mammary nodes
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
|---|---|---|---|---|---|
| Assumed risk: IM RT− | Corresponding risk: IM RT+ | ||||
| Overall survival (10 year follow-up) | 8 yr OS 76% | 8 yr OS 78% (77% to 80%) |
HR 0.9 (0.83 to 0.97) | 10259 (4 studies) | High |
| Treatment-related morbidity - acute radiation pneumonitis (within 3 to 6 months of completing radiotherapy) | 11 per 1000 | 29 per 1000 (11 to 77) |
RR 2.7 (1.03 to 7.08) |
2542 (2 studies) | Moderate1 |
| Disease-free survival - Whole sample (10 year follow-up) | 10 yr DFS 67% | 10 yr DFS 69% (67% to 71%) |
HR 0.92 (0.85 to 1) |
7170 (3 studies) | Moderate2 |
| Disease-free survival - 0 positive lymph nodes (10 year follow-up) | 10 yr DFS 73% | 10 yr DFS 77% (73% to 80%) |
HR 0.82 (0.69 to 0.98) |
1955 (2 studies) | High |
| Disease-free survival - 1–3 positive lymph nodes (10 year follow-up) | 10 yr DFS 73% | 10 yr DFS 77% (74% to 80%) |
HR 0.85 (0.74 to 0.98) |
3283 (2 studies) | High |
| Disease-free survival - 4+ positive lymph nodes (10 year follow-up) | 10 yr DFS 52% | 10 yr DFS 56% (44% to 67%) |
HR 0.89 (0.62 to 1.27) |
596 (2 studies) | Moderate1 |
| Disease-free survival - T stage: 1 (10 year follow-up) | 10 yr DFS 74% | 10 yr DFS 75% (72% to 78%) |
HR 0.93 (0.8 to 1.09) |
2408 (1 study) | High |
| Disease-free survival - T stage: 2 (10 year follow-up) | 10 yr DFS 57% | 10 yr DFS 63% (58% to 68%) |
HR 0.83 (0.7 to 0.97) |
1430 (1 study) | High |
| Disease-free survival - T stage: 3 (10 year follow-up) | 10 yr DFS 58% | 10 yr DFS 61% (44% to 74%) |
HR 0.9 (0.54 to 1.51) |
141 (1 study) | Moderate1 |
| Disease-free survival - Tumour position: medial (10 year follow-up) | 10 yr DFS 75% | 10 yr DFS 84% (74% to 90%) |
HR 0.6 (0.35 to 1.04) |
261 (1 study) | Moderate1 |
| Disease-free survival - Tumour position: lateral (10 year follow-up) | 10 yr DFS 79% | 10 yr DFS 83% (79% to 87%) |
HR 0.77 (0.59 to 1.01) |
1142 (1 study) | Moderate1 |
| Treatment-related morbidity - secondary cancer (potentially radiation-induced; 10 year follow-up) | 110 per 1000 | 104 per 1000 (84 to 131) |
RR 0.95 (0.77 to 1.19) |
5686 (2 studies) | High |
| Locoregional recurrence (10 year follow-up) | 10 yr free from LRR 92% | 10 yr free from LRR 95% (93% to 97%) |
HR 0.59 (0.39 to 0.89) |
1832 (1 study) | Moderate1 |
| Treatment-related morbidity - arm/shoulder function impairment (3 year follow-up) | 4 per 1000 | 1 per 1000 |
RR 0.13 (0.02 to 1.01) |
3866 (1 study) | Low3 |
| Treatment-related morbidity – fatigue (3 month to 3 year follow-up) | 66 per 1000 | 69 per 1000 (57 to 83) |
RR 1.05 (0.87 to 1.26) |
5686 (2 studies) | Moderate4 |
| Treatment-related morbidity - Grade 2+ acute pain (site not specified; within 3 months of completing radiotherapy) | 43 per 1000 | 60 per 1000 (40 to 88 |
RR 1.38 (0.92 to 2.05) |
1820 (1 study) | Low5 |
| Treatment-related morbidity - skin toxicity (3 month to 3 year follow-up) | 215 per 1000 | 252 per 1000 (220 to 288) |
RR 1.17 (1.02 to 1.34) |
5686 (2 studies) | High |
| Treatment-related morbidity - lung toxicity (3 to 10 year follow-up) | 13 per 1000 | 31 per 1000 (21 to 46) |
RR 2.5 (1.7 to 3.67) |
5686 (2 studies) | Moderate1 |
| Treatment-related morbidity - cardiac toxicity (10 year follow-up) | 35 per 1000 | 42 per 1000 (33 to 53) |
RR 1.2 (0.95 to 1.52) |
7020 (3 studies) | Low5 |
| Treatment-related morbidity - Grade 2+ lymphoedema (10 year follow-up) | 45 per 1000 | 84 per 1000 (58 to 121) |
RR 1.85 (1.29 to 2.67) |
1820 (1 study) | Moderate1 |
| Treatment-related morbidity - Grade 3+ morbidity on SOMALENT scale (10 year follow-up) | 23 per 1000 | 31 per 1000 (16 to 60) |
RR 1.38 (0.72 to 2.65) |
1334 (1 study) | Low6 |
| Treatment-related morbidity - mastitis (3 year follow-up) | 4 per 1000 | 3 per 1000 (1 to 9) |
RR 0.87 (0.29 to 2.57) |
3866 (1 study) | Moderate8 |
| Treatment-related morbidity - breast infection (3 year follow-up) | 2 per 1000 | 2 per 1000 (0 to 7) |
RR 0.76 (0.17 to 3.38) |
3866 (1 study) | Moderate8 |
| Treatment-related morbidity - radionecrosis (3 year follow-up) | 1 per 1000 | 1 per 1000 (0 to 6) |
RR 0.51 (0.05 to 5.57) |
3866 (1 study) | Moderate8 |
| Treatment-related morbidity - osteonecrosis (3 year follow-up) | 11 per 1000 | 14 per 1000 (8 to 25) |
RR 1.24 (0.71 to 2.17) |
3866 (1 study) | Low6 |
| Treatment-related morbidity - oedema (3 year follow-up) | 80 per 1000 | 79 per 1000 (63 to 97) |
RR 0.99 (0.79 to 1.22) |
3866 (1 study) | Moderate7 |
| Treatment-related morbidity - breast/chest wall pain (3 year follow-up) | 23 per 1000 | 18 per 1000 (12 to 28) |
RR 0.79 (0.51 to 1.22) |
3866 (1 study) | Low3 |
| Treatment-related morbidity - retrosternal pain (3 year follow-up) | 1 per 1000 | 1 per 1000 (0 to 11) |
RR 2.02 (0.18 to 22.29) |
3866 (1 study) | Moderate8 |
| Treatment-related morbidity - dysphagia (3 year follow-up) | 0 per 1000 | 0 per 1000 (0 to 0) |
RR 9.1 (0.49 to 168.96) |
3866 (1 study) | Moderate8 |
Rates of disease-free survival and locoregional recurrence in the control group correspond to the weighted average across included trials; rates of overall survival correspond to the trial with the shortest follow-up period (DBCG-IMN)
CI: Confidence interval; DFS: dsease-free survival; HR: hazard ratio; IM: internal mammary; OS: overall survival; RR: Risk ratio; RT: radiotherapy; SOMA-LENT: Subjective, Objective, Management, Analytic-Late Effects of Normal Tissues
- 1
total events <300
- 2
Significant heterogeneity (I2 = 73%) - not present in subsequent subgroup analysis
- 3
total events <300 and 95% CI crosses both no effect (1) and minimally important difference based on GRADE default value (0.8)
- 4
95% CI crosses no effect (1) and minimally important difference based on GRADE default value (1.25)
- 5
total events <300 and 95% CI crosses no effect (1) and minimally important difference based on GRADE default value (1.25)
- 6
total events <300 and 95% CI crosses no effect (1) and minimally important differences based on GRADE default values (0.8 and 1.25)
- 7
95% CI crosses both no effect (1) and minimally important difference based on GRADE default value (0.8)
- 8
total events<300; not downgraded based on 95% CI due to very small differences in absolute risk
Final
Evidence reviews
developed by the National Guideline Alliance, hosted by the Royal College of Obstetricians and Gynaecologists
Disclaimer: The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. All NICE guidance is subject to regular review and may be updated or withdrawn.